Abstract
Background
The Hip & Knee Book: Helping you cope with osteoarthritis was developed to change disadvantageous beliefs and encourage physical activity in people with hip or knee osteoarthritis.
Aim
To assess the feasibility of conducting a definitive randomised controlled trial (RCT) of this evidence-based booklet in people with hip or knee osteoarthritis.
Design
Phase II feasibility randomised controlled trial (RCT).
Method
Computerised searches of patients' record databases identified people with osteoarthritis of the hip or knee, who were invited to participate in the RCT comparing the new booklet with a control booklet. Outcomes were measured at baseline, 1 month, and 3 months, and included: beliefs about hip and knee pain, exercise, and fear avoidance; level of physical activity; and health service use.
Results
The trial methods were feasible in terms of recruitment, randomisation, and follow-up, but most participants recruited had longstanding established symptoms. After one and 3 months, there was a small relative improvement in illness, exercise, and fear-avoidance beliefs and physical activity level in The Hip & Knee Book group (n = 59) compared with the control group (n = 60), which provides some proof of principle for using these outcomes in future trials.
Conclusion
This feasibility study provided proof of principle for testing The Hip & Knee Book in a larger definitive RCT.
Keywords: osteoarthritis, hip; osteoarthritis, knee; patient education handout; primary health care; randomised controlled trial
INTRODUCTION
Systematic reviews have highlighted the effectiveness of exercise in reducing pain and disability in hip and knee osteoarthritis,1-4 and guidelines have emphasised the central role of exercise in the management of osteoarthritis.5,6 Both aerobic walking and muscle-strengthening exercise have been shown to be effective; however, the optimal type, dose, and setting for such physical activity is uncertain.3,7 Despite these benefits, long-term adherence to exercise regimes is disappointing, and if exercise is not maintained its beneficial effects decline over time and finally disappear.8 The level of physical activity in older adults in the UK is low,9-12 and reduced further by pain-related fear of movement in those with osteoarthritis.13,14 Indeed, there is a culturally conditioned response to pain that encourages rest, which is inappropriate for most people with osteoarthritis. How can people with osteoarthritis be encouraged to increase their physical activity?
The authors have developed The Hip & Knee Book: Helping you cope with osteoarthritis, which is an evidence-based advice booklet encouraging increased activity in people with hip or knee osteoarthritis.15 The theoretical framework underpinning this new booklet was an extension of Leventhal's theory of self-regulation, concerning illness16 and treatment beliefs.17 The development of this booklet has been described previously.18The objectives of this phase II randomised controlled trial (RCT) were to assess the feasibility of conducting a larger definitive RCT of this new booklet and to measure change in health beliefs and exercise behaviour for patients with hip and knee osteoarthritis.19
METHOD
Inclusion and exclusion criteria
The protocol for this phase II RCT has been fully described elsewhere.20 Participants were recruited from four general medical practices in North East Wales in the UK. Patients aged over 50 years presenting in primary care with hip or knee osteoarthritis within the previous 12 months were identified by searching the practices' computerised patient record database for relevant diagnostic codes. Exclusion criteria were inflammatory joint disease, fractures, arthroplasty referral, and prescription of potent opioid analgesia.
How this fits in
The Hip & Knee Book: Helping you cope with osteoarthritis has been developed to change disadvantageous beliefs and encourage physical activity in people with hip or knee osteoarthritis. A phase II feasibility randomised controlled trial (RCT) was performed comparing this new booklet with a control booklet. The trial methods were feasible and the results provide proof of principle for testing The Hip & Knee Book in a larger definitive RCT.
Randomisation
Randomisation balanced the two groups by site of pain, age, sex, and duration of symptoms, using an optimal allocation approach.21,22 Patients were recruited from each practice and then randomised as a block by an independent statistician.
Study interventions
Participants randomised to the intervention arm were sent the new advice booklet by mail. This booklet, The Hip & Knee Book: Helping you cope with osteoarthritis,15 emphasised the beneficial effects of physical activity for arthritic joints, and stressed that a substantial degree of control over their condition was possible and within each individual's capability. Participants randomised to the control arm were sent a patient information booklet about osteoarthritis produced by the Arthritis Research UK (ARUK),23 which did not address the same exercise-related beliefs. Clinical care of patients was not affected in any other manner by participation in the RCT.
Outcome measures
Outcomes were measured by postal questionnaire at baseline, 1, and 3 months. The primary outcomes were illness and treatment beliefs. Illness beliefs regarding the progressive nature of osteoarthritis were measured with the Hip and Knee Beliefs Questionnaire (HKBQ) modified from the Back Beliefs Questionnaire.24 Treatment beliefs were measured with a modified Exercise Attitude Questionnaire-18 (EAQ-18).25 Secondary outcomes included: physical activity over the previous seven days measured with the International Physical Activity Questionnaire (IPAQ);26 fear-avoidance beliefs using the Tampa Scale for Kinesiophobia (TSK);27 and health service activity collected from a NHS perspective from responses to an adapted Client Service Receipt Inventory (CSRI).28
Any adverse effects were collected as written comments. All data were anonymised and coded so that data collection and statistical analysis were blinded to treatment allocation.
Trial analysis
Feasibility was assessed by measuring recruitment and retention rates. Statistical analysis of the primary and secondary outcome measures was based on an intention-to-treat analysis using repeated measures analysis of covariance (ANCOVA), adjusting each patient's follow-up score with baseline. Data with a skewed distribution were transformed to normality so that missing data could be imputed, then transcribed back to the skewed distribution of the original data. Missing results were imputed using Imputation by Chained Equations in Stata,29 which used an iterative procedure to allow for multiple missing values. The imputed datasets were analysed separately, and then the separate estimates were combined according to Rubin's rules.30
Telephone interviews
As an additional process evaluation, participants were contacted by telephone in August 2010, several months after participating in the trial, and asked whether they could remember receiving the booklet and whether it had changed what they thought about their osteoarthritis and about physical activity or exercise.
RESULTS
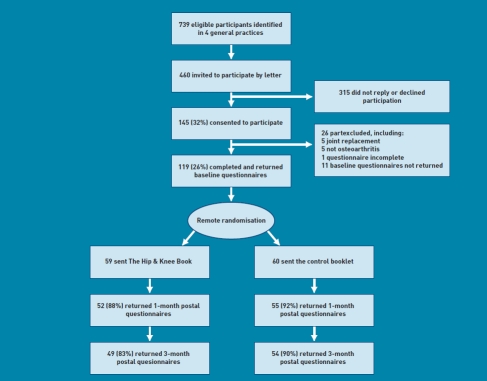
Four practices were recruited between July 2008 and August 2009 after sending letters of invitation to 16 practices. Between January and March 2009, 460 letters were sent to potential participants; 145 (32%) consented to take part and were sent baseline questionnaires, of which 119 (89%) were returned (Figure 1). The numbers eligible to participate varied between the four practices. Practices one, two, and three identified 1.5-1.8% of their practice population in a search of diagnostic codes in their computerised patient record database, whereas practice four identified 6.7%. From some of the written comments on the forms of patients who declined to participate, there was evidence of inappropriate diagnostic labelling in patients from practice four The recruitment rate varied from 24% of invited patients in practice two to 33% in practices three and four. The follow-up questionnaire response rate was 90% at 1 month and 89% at 3 months. Individual scale response rates were sometimes lower due to missing items, or, specifically in the IPAQ, if the box marked ‘Don't know’ was ticked.
Figure 1.
Trial flow chart.
Baseline results
Demographic factors and variables such as age, sex, employment status, educational attainment, and ethnicity were similar between the two groups at baseline, as was the duration of symptoms and the joints affected (Table 1). Data from 32 IPAQ and one HKBQ questionnaire were missing at baseline and had to be imputed. The mean values of all baseline outcome measures were similar, apart from IPAQ. There was an imbalance in this outcome, with the control group more active than the intervention group, but also with large interquartile ranges.
Table 1.
Baseline trial results
| Demographic or outcome variable | The Hip & Knee Book (n = 59) | Control book(n = 60) |
|---|---|---|
| Sex | ||
| Male | 21 | 22 |
| Female | 38 | 38 |
| Mean age, years (SD) | 68.2(8.1) | 68.6(8.5) |
| Ethnicity | ||
| White British | 59 | 59 |
| White and Black African | 0 | 1 |
| Educational qualification | ||
| None | 24 | 21 |
| GCSE/A-level | 19 | 16 |
| Professional/vocational | 3 | 11 |
| Degree/diploma | 13 | 12 |
| Occupation | ||
| Unemployed/sickness | 2 | 3 |
| Full-time/part-time employment | 14 | 15 |
| Retired | 43 | 42 |
| Median duration of symptoms years (IQR) | 6(2,11.8) | 6 (3, 10) |
| Osteoarthritis location | ||
| Knee only | 8 | 7 |
| Hip only | 24 | 22 |
| Knee and hip | 27 | 31 |
| HKBQ, mean(SD) | 29.9(8.5), n= 59 | 31.0(8.6), n = 59 |
| EAQ-18, mean (SD) | 38.8 (13.8), n= 59 | 37.6 (11.4), n = 60 |
| TSK, mean (SD) | 33.3 (9.3), n= 59 | 34.5 (10.1), n = 60 |
| IPAQ, median (IQR) METs min/week | 2439 (0 to 6 560), n = 43 | 1442 (99 to 3 944), n = 44 |
EAQ = Exercise Attitude Questionnaire. HKBQ = Hip and Knee Beliefs Questionnaire. IPAQ = International Physical Activity Questionnaire. IQR = interquartile range. MET = metabolic equivalent. SD = standard deviation. TSK = Tampa Scale of Kinesiophobia.
Outcomes at 1 and 3 months
Data from the following numbers of questionnaires were missing at follow-up and had to be imputed: 1 month 35 IPAQ, 13 TSK, 15 HKBQ, 13 EAQ-18; 3 months 50 IPAQ, 16 TSK, 17 HKBQ, 16 EAQ-18. All outcome measures had some missing data at all three time points. Missing values were imputed using multiple regression with variables at all three time points, with sex, age, and duration as auxiliary variables. The final ANCOVA regression estimates reflected the difference in mean change scores after 1 and 3 months using the control as a reference group. There were small improvements in all outcome measures at both follow-up points. There were relative improvements in favour of The Hip & Knee Book in all outcome measures at both time points (Tables 2 and 3). Standardised differences of mean change score were of the order of 0.1 or 0.2 (Table 3).
Table 2.
Follow-up results at 1 month with imputed missing values
| Outcome measure | The Hip & Knee book 1-month mean score (SD) | Control book 1-month mean score (SD) | Difference in adjusted mean change from baseline (SE) | 95% CI |
|---|---|---|---|---|
| HKBQ | 26.8 (8.4), n = 59 | 28.5(8.3), n = 59 | -1.1 (1.3) | -3.7 to 1.6 |
| EAQ-18 | 36.5(13.1), n = 59 | 36.9(10.6), n = 60 | -1.4(1.3) | -4.0 to 1.2 |
| TSK | 30.7 (8.2), n = 59 | 34.2(9.0), n = 60 | -2.8(1.3) | -5.4 to-0.2 |
| IPAQ, METs min/week | 5411 (5780), n = 43 | 4821 (4657), n = 44 | 871 (907) | -941 to 2683 |
EAQ = Exercise Attitude Questionnaire. HKBQ = Hip and Knee Beliefs Questionnaire. IPAQ = International Physical Activity Questionnaire. MET = metabolic equivalent. SE = standard error. TSK = Tampa Scale of Kinesiophobia.
Table 3.
Follow-up results at 3 months, with imputed missing values
| Outcome measure | The Hip & Knee book 3-month mean score (SD) | Control book 3-month mean score (SD) | Difference in adjusted mean change from baseline (SE) | 95% CI |
|---|---|---|---|---|
| HKBQ | 25.7(7.9), n = 59 | 27.4(8.6), n = 59 | -1.1 (1.3) | -3.8 to 1.5 |
| EAQ-18 | 36.4(12.9), n = 59 | 38.0(11.2), n = 60 | -2.6(1.4) | -5.4 to 0.2 |
| TSK | 31.2(8.8), n = 59 | 32.1 (10.7), n = 60 | -0.1(1.5) | -3.0 to 2.9 |
| IPAQ, METsmin/week | 4859 (6763), n = 43 | 3904 (4285), n = 44 | 1263(1174) | -1099 to 3624 |
EAQ = Exercise Attitude Questionnaire. HKBQ = Hip and Knee Beliefs Questionnaire. IPAQ = International Physical Activity Questionnaire. MET = metabolic equivalent. SD = standard deviation. SE = standard error TSK = Tampa Scale of Kinesiophobia.
Resource data were available for 103 participants and demonstrated the feasibility of including an economic evaluation in a future definitive RCT. Resource use was similar for both groups in terms of primary care consultations, secondary care outpatient visits, and accident and emergency department attendances. Inpatient days were greater in the control group, but none of these admissions were directly related to osteoarthritis (Table 4).
Table 4.
Resource use over 3 months per patient
| Mean, median (min, max) | ||
|---|---|---|
| The Hip and Knee Book group (n = 49) | Control group (n = 54) | |
| Primary care sector | ||
| GP consultations | 0.94, 1 (0, 6) | 1.22, 1 (0, 9) |
| Practice nurse consultations | 0.31, 0 (0, 2) | 0.46, 0 (0, 3) |
| Other health professionals | 0.58, 0 (0, 4) | 0.65, 0 (0, 10) |
| Secondary care sector | ||
| Outpatient visits/day surgery | 1.16, 0 (0, 13) | 1.2, 0 (0, 13) |
| Accident and emergency attendances | 0.04, 0 (0, 1) | 0.07, 0 (0,2) |
| Inpatient days | 0.04, 0 (0, 1) | 0.78, 0 (0, 30) |
| Investigations | ||
| Blood tests/ECG/lung function | 1.02, 0 (0, 8) | 1.26, 1 (0, 11) |
| Endoscopy/arthroscopy | 0.16, 0 (0, 2) | 0.07, 0 (0, 2) |
| Imaging | 0.47, 0 (0, 7) | 0.43, 0 (0, 4) |
ECG = electrocardiogram
To explore the influence of symptom duration, a subgroup analysis was performed comparing shorter and longer duration of symptoms either side of the median duration of 6 years.
There was no significant difference between the groups (n = 59) and no consistent trend across the different outcomes and follow-up intervals.
Written comments
Participants made additional written comments on 45 of the 1-month and 43 of the three-month questionnaires. Most of these gave extra information concerning: comorbid conditions, social circumstances, investigations, and treatment, or explained their symptoms in more detail. Two participants made comments about The Hip & Knee Book at 1 month, and five at 3 months. Most of these comments were positive, stating that the booklet had encouraged them to exercise. One stated that the booklet was unhelpful compared to medical and surgical treatments, and one participant felt that there should be greater emphasis on weight loss. No comments about any harm or other unintended effects were disclosed. There were two neutral comments about the control booklet.
Telephone interviews
Several months after completing the trial, it was possible to contact 92 participants (77%) by telephone, 43 (73%) in The Hip & Knee Book group, and 49 (82%) in the control group. In The Hip & Knee Book group, 13 (30%) had not read or could not remember reading the booklet; 20 (47%) had not increased their physical activity levels, 10 (23%) of whom were already physically active; and 10 (23%) reported that they had increased their level of physical activity after reading The Hip & Knee Book. In the control group, 11 (22%) had not read or could not remember reading the booklet; 31 (63%) had not increased their physical activity levels, 13 (27%) of whom were already physically active; and 7 (14%) reported that they had increased their level of physical activity after reading the control booklet.
DISCUSSION
Summary
The trial methods were feasible in terms of recruitment, randomisation, and follow-up. The small relative improvement in illness, exercise and fear-avoidance beliefs, and physical activity level provided proof of principle for using these outcomes in future trials testing the effectiveness of The Hip & Knee Book.
Strengths and limitations
The intervention booklet was an evidence-based booklet underpinned by a psychological theory of self-regulation concerning illness and treatment beliefs. The control booklet was a respected booklet produced by the ARUK.23 Although physical activity was not stressed, it was mentioned, and might have had a larger effect on outcomes than usual primary care without any booklet. The booklets were delivered by post to the participants and may have had a smaller effect than if given by their GP as part of a consultation about osteoarthritis. The intervention booklet was an evidence-based booklet underpinned by a psychological theory of self-regulation concerning illness and treatment beliefs. There were missing data at follow-up; 11-14% of most outcomes were missing, increasing to 29% of IPAQ at 1 month and 42% at 3 months. This is a possible source of bias, which the study attempted to minimise by imputing missing values.
There are other causes of hip and knee pain apart from osteoarthritis, and the diagnostic code search strategy used for identifying suitable participants was not specific for osteoarthritis and resulted in a variation in recruitment rate between practices, with evidence of inappropriate diagnostic labelling in one practice. Identifying patients with early-stage osteoarthritis of the hip or knee from primary care records is problematic, as people often spend years with joint pain as the diagnostic code before finally getting an osteoarthritis code. A change to inclusion criteria would be beneficial fora future RCT, either an additional check of eligibility prior to trial inclusion, or broadening the criteria to include all patients over 50 years of age with hip or knee pain.
The symptom duration in the participants varied, with a median of 6 years and an interquartile range of 2 to 11 years, which may have diluted the effect of the advice. A subgroup analysis found no consistent or significant effect of symptom duration either side of the median duration; however, very few participants were newly diagnosed. It seems logical to presume that the benefits of increasing activity would have more profound effects in people with a new diagnosis than those with longstanding disease and entrenched behaviours.
Comparison with existing literature
The authors are not aware of any other RCTs evaluating an advice booklet for osteoarthritis. Most of the research on education and self-management for people with osteoarthritis concerns self-management interventions (SMIs), which are problem-focused, action-oriented, patient-generated care plans,31 and are more complex and costly than booklets.32,33 Indeed many RCTs of SMIs have used information booklets as the control intervention, and found some evidence that they are less effective than SMIs, but the nature of the control booklets was very different from the present booklet, which was firmly focused on fostering positive beliefs and attitudes about what to do in the face of osteoarthritis.
In the field of back pain research, a similar booklet The back book (Roland M et al, The Stationery Office, 1996) has been shown, in two RCTs, to improve fear-avoidance beliefs and back pain-related health status.34,35 In these trials, which had positive results, the booklets were given to patients during a consultation or following an educational talk related to the presenting symptoms, whereas in the present trial the booklet was sent by post and most recipients had established symptoms. It may be that demedicalising back pain is easier because osteoarthritis of the hip or knee is perceived as a disease requiring medical intervention, and when all else fails arthroplasty is available as an acceptable treatment. However, the results of focus groups held during the development of The Hip & Knee Book showed that it was well received and conveyed its intended messages concerning beliefs.18
Implications for practice and research
The methods fordelivering a future phase III trial were feasible in terms of the procedures for delivering the intervention and the likely rates of recruitment and retention of participants. A change of inclusion criteria would be beneficial, either an additional check of eligibility, or broadening the criteria to include all patients aged over 50 years, with hip or knee pain. An alternative measure of physical activity would increase response rates for this outcome.
Distributing The Hip & Knee Book in this untargeted mannerto primary care patients with a diagnostic label of osteoarthritis of the hip or knee is an acceptable, inexpensive, and straightforward intervention that has the potential to change beliefs and encourage some people to become more physically active. As such, it is similarto othersimple primary care health-promotion interventions such as smoking cessation. A future definitive RCT using the same methods would need to be much larger (n = 700) to test the small effects found in this pilot RCT with sufficient power Targeting the booklet on the newly diagnosed and the physically inactive during a consultation, and using usual care without a booklet as the control, might increase its effectiveness. Only about a quarter of those that received The Hip & Knee Book increased their physical activity; a telephone reminder or a follow-up booklet might increase the proportion that change their behaviour However, any of these changes would require a more complex distribution strategy, would cost more in terms of administration and consultation time, and would require further pilot testing.
Acknowledgments
We would like to thank all of the patients who participated in the trial; the National Institute forSocial Care and Health Research (NISCHR) Clinical Research Centre North Wales research network; Rachel Gray who conducted the telephone interviews; Glynne Andrew, Betsi Cadwaladr University Health Board; colleagues from the Department of Primary Care and Public Health, Cardiff University for their comments and suggestions; and the South East Wales Trials Unit (SEWTU), which is funded by NISCHR.
Funding
Wales Office of Research and Development for Health and Social Care now called National Institute forSocial Care and Health Research (grant number ReF06/2/234).
Trial registration
Current Controlled Trials ISRCTN24554946.
Ethical approval
Ethical approval was obtained from the North Wales East Research Ethics Committee (REC reference 09/WNo03/5).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Many of the authors previously developed and wrote The Hip & Knee Book: Helping you cope with osteoarthritis, which has been published by The Stationery Office.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.van Baar ME, Assendelft WJ, Dekker J, et al. Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review of randomized clinical trials. Arthritis Rheum. 1999;42(7):1361–1369. doi: 10.1002/1529-0131(199907)42:7<1361::AID-ANR9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy CJ, Oldham JA. The effectiveness of exercise in the treatment of osteoarthritic knees: a critical review. Physical Therapy. 1999;4:241–250. [Google Scholar]
- 3.Brosseau L, MacLeay L, Robinson VA, et al. Intensity of exercise forthe treatment of osteoarthritis. Cochrane Database of Syst Rev. 2003;(2):CD004259. doi: 10.1002/14651858.CD004259. [DOI] [PubMed] [Google Scholar]
- 4.Hernández-Molina G, Reichenbach S, Zhang B, et al. Effect of therapeutic exercise for hip osteoarthritis: results of a meta-analysis. Arthritis Rheum. 2008;59(9):1221–1228. doi: 10.1002/art.24010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roddy E, Zhang W, Doherty M, et al. Evidence based recommendations forthe role of exercise in the management of osteoarthritis of the hip or knee -the MOVE consensus. Rheumatology. 2005;44(1):67–73. doi: 10.1093/rheumatology/keh399. [DOI] [PubMed] [Google Scholar]
- 6.National Collaboration Centre for Chronic Conditions. National Clinical Guideline for the care and management of osteoarthritis in adults. London: Royal College of Physicians; 2008. [PubMed] [Google Scholar]
- 7.Ashworth NL, Chad KE, Harrison EL, et al. Home versus center based physical activity programs in olderadults. Cochrane Database Syst Rev. 2005;(1):CD004017. doi: 10.1002/14651858.CD004017.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Baar ME, Dekker J, Oostendorp RA, et al. Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months follow up. Ann Rheum Dis. 2001;60(12):1123–1130. doi: 10.1136/ard.60.12.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Health and Social Care Information Centre. Health Survey for England — 2008: physical activity and fitness. http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england/health-survey-for-england—2008-physical-activity-and-fitness (accessed 18 May 2011)
- 10. Welsh Assembly Government. Welsh Health Survey 2009: initial headline results. http://new.wales.gov.uk/topics/statistics/headlines/health2010/1005251/?lang=en (accessed 18 May 2011)
- 11. The Scottish Government. The Scottish Health Survey 2008. http://www.scotland.gov.uk/Publications/2009/09/28102003/70 (accessed 18 May 2011)
- 12. Northern Ireland Health and Social Wellbeing Survey 2005/06. Topline results - physical activity. http://www.csu.nisra.gov.uk/Physical%20activity.pdf (accessed 18 May 2011)
- 13.Heuts PHTG, Vlaeyen JWS, Roelofs J, et al. Pain-related fear and daily functioning in patients with osteoarthritis. Pain. 2004;110(1-2):228–235. doi: 10.1016/j.pain.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 14.Hendry MA, Williams NH, Wilkinson C, et al. Motivation to Exercise in Arthritis of the Knee: a qualitative study in primary care patients. Fam Pract. 2006;23(5):558–567. doi: 10.1093/fampra/cml022. [DOI] [PubMed] [Google Scholar]
- 15.Williams NH, Amoakwa E, Burton K, et al. The hip and knee book: helping you cope with osteoarthritis. London: TSO; 2009. [Google Scholar]
- 16.Cameron LD, Leventhal H. The self-regulation of health and illness behaviour. New York: Routledge; 2003. [Google Scholar]
- 17.Horne R. Patients' beliefs about treatment: the hidden determinant of treatment outcome? J Psychosom Res. 1999;47(6):491–495. doi: 10.1016/s0022-3999(99)00058-6. [DOI] [PubMed] [Google Scholar]
- 18.Williams NH, Amoakwa E, Burton K, et al. The Hip and Knee Book: developing an active management booklet for hip and knee osteoarthritis. Br J Gen Pract. 2010;60(571):113–120. doi: 10.3399/bjgp10X483166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craig P, Dieppe P, MacIntyre S, et al. Developing and evaluating complex interventions: new guidance. London: Medical Research Council; 2009. http://www.mrc.ac.uk/complexinterventionsguidance (accessed 18 May 2011) [Google Scholar]
- 20.Williams NH, Amoakwa E, Burton K, et al. Activity Increase Despite Arthritis (AÏDA): design of a phase II randomised controlled trial evaluating an active management booklet for hip and knee osteoarthritis [ISRCTN24554946] BMC Fam Pract. 2009;10:62. doi: 10.1186/1471-2296-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raab GM, Butcher I. Balance in cluster randomized trials. Stat Med. 2001;20(3):351–355. doi: 10.1002/1097-0258(20010215)20:3<351::aid-sim797>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 22.Carter B, Hood K. Balance algorithm for cluster randomized trial. BMC Med Res Methodol. 2008;8:65. doi: 10.1186/1471-2288-8-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arthritis Research UK. Osteoarthritis: an information booklet. Chesterfield: Arthritis Research Campaign; 2004. [Google Scholar]
- 24.Symonds TL, Burton AK, Tillotson KM, Main CJ. Do attitudes and beliefs influence work loss due to low back trouble? Occup Med. 1996;46(1):3–6. doi: 10.1093/occmed/46.1.25. [DOI] [PubMed] [Google Scholar]
- 25.Maningandan C, Charles J, Divya I, et al. Construction of exercise attitude questionnaire-18 to evaluate patients' attitudes toward exercises. Int J Rehab Res. 2004;27(3):229–231. doi: 10.1097/00004356-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Craig C, Marshall AL, Sjostrom M, et al. International Physical Activity Questionnaire (IPAQ): 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 27.Heuts PHTG, Vlaeyen JWS, Roelofs J, et al. Pain-related fearand dailyfunctioning in patients with osteoarthritis. Pain. 2004;110(1-2):228–235. doi: 10.1016/j.pain.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 28.Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. Oxford: Oxford University Press; 2007. [Google Scholar]
- 29.Royston P. Multiple imputation of missing values. Stata J. 2004;4:227–241. [Google Scholar]
- 30.Rubin DB. Multiple imputation for non-response in surveys. New York: Wiley and Sons; 1987. [Google Scholar]
- 31.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 32.Iversen MD, Hammond A, Betteridge N. Self-management of rheumatic diseases: state of the art and future perspectives. Ann Rheum Dis. 2010;69(6):955–963. doi: 10.1136/ard.2010.129270. [DOI] [PubMed] [Google Scholar]
- 33.Patel A, Buszewicz M, Beecham J, et al. Economic evaluation of arthritis self-management in primary care. BMJ. 2009;339:b3532. doi: 10.1136/bmj.b3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burton AK, Waddell G, Tillotson KM, et al. Information and advice to patients with back pain can have a positive effect: a randomised controlled trial of a novel educational booklet. Spine. 1999;24(23):2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 35.Kovacs FM, Abraira V, Santos S, et al. Spanish Back Pain Research Network. A comparison of two short education programs for improving low back pain related disability in the elderly: a cluster randomised controlled clinical trial. Spine. 2007;32(10):1053–1059. doi: 10.1097/01.brs.0000261556.84266.0f. [DOI] [PubMed] [Google Scholar]