Abstract
Background
Treatment acceptance by patients is influenced by the way treatment effects are presented. Presentation of benefits using relative risk increases treatment acceptance compared to the use of absolute risk. It is not known whether this effect is modified by prior presentation of a patient's individualised risk estimate or how presentation of treatment harms by relative or absolute risk affects acceptance.
Aim
To compare acceptance of a hypothetical treatment to prevent hip fracture after presentation of the treatment's benefit in relative or absolute terms in the context of a personal fracture risk estimate, and to reassess acceptance following subsequent presentation of harm in relative orabsolute terms.
Design and setting
Randomised controlled trial of patients recruited from 10 GPs' lists in Christchurch, New Zealand.
Method
Women aged ≥50 years were invited to participate. Participants were given a personal 10-year hip fracture risk estimate and randomised to receive information on a hypothetical treatment's benefit and harm in relative orabsolute terms.
Results
Of the 1140 women invited to participate 393 (34%) took part. Treatment acceptance was greater following presentation of benefit using absolute terms than relative terms after adjustment forage, education, previous osteoporosis diagnosis, and self-reported risk (OR 1.73, 95% confidence interval [CI] = 1.10 to 2.73, P = 0.018). Presentation of the treatment's harmful effect in relative terms led to a greater proportion of participants declining treatment than did presentation in absolute terms (OR 4.89, 95% CI = 2.3 to 11.0, P<0.001).
Conclusion
Presentation of treatment benefit and harm using absolute risk estimates led to greater treatment acceptance than presentation of the same information in relative terms.
Keywords: communication, decision making, hip fracture, osteoporosis, preventive medicine, risk
INTRODUCTION
Disease prevention is a major part of current clinical practice in primary care. This often requires asymptomatic patients to take long-term treatment to reduce their risk of a future adverse event. The immediate inconvenience, cost, and risk of taking medication are balanced against a potential but distant benefit of treatment. When deciding whether to accept such treatment, patients and their doctors must understand the likelihood of the treatment conferring benefit and causing harm.
The way in which likelihood information is presented influences whether patients accept treatment.1 The use of relative risk to describe treatment benefits has been shown to result in greater acceptance of treatment than does presentation in absolute terms. 1-5 The effect of different methods of risk presentation has previously been examined using presentation of a standard population risk scenario to participants rather than using a calculated personal risk estimate. Patients may respond differently to a personalised risk than they do to a hypothetical one, hence this investigation of personalised risk.
Absolute risk estimates are considered to lead to better understanding of the magnitude of treatment effects than relative risk estimates. The use of natural frequencies (numbers rather than percentages or fractions) has been suggested as the clearest means of communicating risk to both doctors and patients.6,7
A gradient of absolute benefit is achieved with long-term prophylactic treatment: those at greatest baseline risk are more likely to benefit from treatment than those at lower risk. However, the adverse effects of treatment are evenly shared regardless of baseline risk. The method used to present a treatment's harms may be therefore as important as that used to present benefits. Different methods of presentation of treatment benefits have been studied; however, there are few studies of the effect of risk presentation methods for describing treatment harms and there is uncertainty about the effect of different methods of communicating this information. Qualitative descriptions of side effects have been found to exaggerate perception of side-effect risk,8,9 while the use of natural frequencies displayed using figure charts has been suggested as a way of reducing side-effect aversion.10 This study investigated the effect of communication methods for both the benefits and harms of treatment on participants' acceptance of fracture prevention treatment in the context of a personalised risk calculation for hip fracture.
A range of preventive treatments is available to reduce the risk of fracture.11-13 The absolute risk reduction achieved with these treatments is determined by the individual's risk of fracture: those at greatest risk of fracture will have the greatest absolute reduction in their fracture risk. Treatments for osteoporosis have been associated with important side effects,13-17 so the decision to use these drugs requires the patient and doctor to balance the likelihood of benefit against the likelihood of harm.
How this fits in
Presentation of treatment benefits in relative risk terms increases treatment acceptance when compared to presentation using absolute risk. In practice, this effect may be modified by prior discussion of an individual's own 5- or 10-year risk of disease (as when considering osteoporosis treatment or cardiovascular disease prevention). The presentation of a treatment's harms may also affect treatment acceptance, but this has received less attention. This study found that, following presentation of a personal hip fracture risk estimate, absolute risk estimates of both the benefit and harm of a hypothetical preventive treatment led to greater treatment acceptance than did presentation using relative risk estimates.
This study was designed to compare the effect of presenting a hypothetical preventive treatment's benefit and adverse effect by relative risk or absolute risk using natural frequencies, on participants' acceptance of preventive treatment for hip fracture. Participants were given this information in the context of their personal hip fracture risk estimate.
METHOD
Ten GPs at four practices in Christchurch, New Zealand, took part in the study. Practices were selected to represent the range of socioeconomic and geographic environments of the city. All women aged >50 years and enrolled with participating GPs were invited to take part in the study and were recruited by invitation letter from their GP. Recruitment was from December 2008 until April 2010. Exclusion criteria were severe cognitive or communication problems, including non-English speakers, and terminal illness.
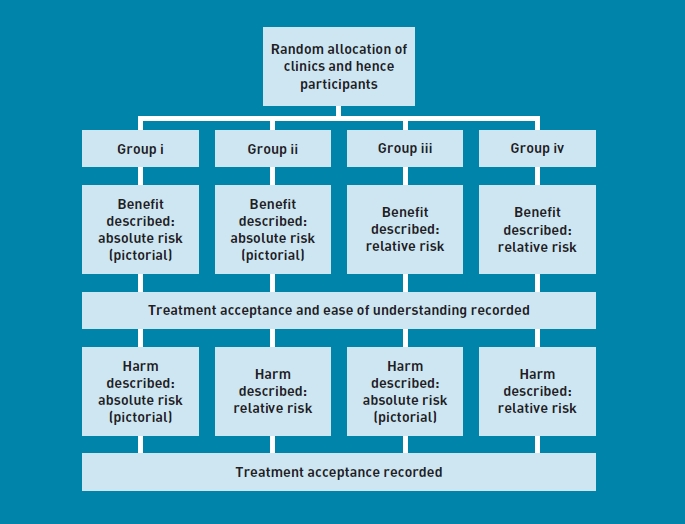
Clinics and hence participants were randomised to one of four groups:
benefit described pictorially in absolute terms, harm described pictorially in absolute terms;
benefit described pictorially in absolute terms, harm described in relative terms;
benefit described in relative terms, harm described pictorially in absolute terms; and
benefit described in relative terms, harm described in relative terms.
Participants were seen at research clinics. Participants were booked to attend a clinic at their convenience. Clinics were randomly allocated to treatment by minimisation of the imbalance overthe four arms, and initial allocation and ties were allocated by a table of random numbers. Enrolment and randomisation of clinics was by a research nurse. Participants and researchers were aware that the purpose of the study was to assess the effect of different methods of description on the acceptance of treatment. Researchers used a standard interview approach and forms for all participants to ensure consistency. Participants were asked to rate their self-reported risk of hip fracture. Demographic and medical data were recorded and used to inform participants of their 10-year hip fracture using the FRAX® software.
Participants were presented with information on treatment benefit either in absolute (pictorial) terms or in relative terms. The following were recorded:
acceptance of treatment; and
ease of understanding of treatment benefit.
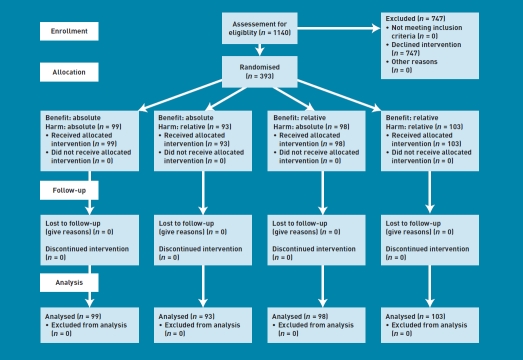
Participants were then presented with information on treatment harm either in absolute (pictorial) terms or in relative terms. Treatment acceptance was recorded again. (Figure 1).
Figure 1.
Participant flow.
Participants allocated to the relative risk group for presentation of benefit were told that treatment would reduce their risk of hip fracture by 40%. Those in the absolute (pictorial) risk group were presented with a chart of 1000 human figures on which the number of women expected to have a hip fracture in the following 10 years was highlighted. The number of fractures avoided by taking treatment was then indicated on the same chart. The number of expected fractures, and hence the number of fractures avoided with treatment, varied between participants according to their calculated 10 year fracture risk (1-200 per 1000 people over 10 years).
After presentation of the treatment's benefit, participants were told that the treatment increased the risk of stroke. Those allocated to the relative risk group were told that stroke risk was increased by 67%. Those in the absolute (pictorial) risk group were shown another chart of 1000 human figures on which was highlighted the number of women expected to have a stroke in the following 10 years without the treatment (12 per 1000) and the additional strokes expected with the treatment (8 per 1000).
Treatment acceptance was measured on a 4-point scale and participants were asked to choose one of ‘very likely’, ‘quite likely’, ‘quite unlikely’, or ‘very unlikely’ to accept treatment. Ease of understanding was also recorded on a 4-point scale and participants were asked how easy it was to understand the effect of the treatment on their risk of hip fracture and to choose one of ‘very easy’, easy’, ‘quite difficult’, and ‘difficult’.
The treatment described to participants was hypothetical, no actual fracture prevention medication was mentioned.
Statistical analysis
Data were recorded in booklets by the interviewer and then entered into an Access® database. Data were analysed in the R language for statistical computing.18 Odds ratios and 95% confidence intervals (CIs) were calculated, results were considered statistically significant at P = 0.05. Descriptive statistics were analysed by ANOVA or Fisher's exact test where appropriate. Multiple logistic regression of main effects was used to adjust for covariates and to estimate the strength of covariate effects. Covariates were eliminated from the final models by forward and backward substitution based on the AIC (Akaike's information criterion) measure of fit. Only significant effects were included in the final models.
Sample size
The proportion accepting treatment given a relative explanation of benefit was expected to be about 80%.2 A sample of 200 was aimed for in both groups by explanation of benefit which using Fisher's exact test at 0.05% significance could detect a drop of 20% in the acceptance proportion with 93.5% power. The sample size achieved was 393 which allowed the detection of a drop of 18.6% in the acceptance proportion with 90% power.
RESULTS
Three hundred and ninety-three women from an eligible population of 1140 responded to invitations to participate. The response rate 34% (Figure 2). Recruitment was carried out over 16 months between December 2008 and April 2010. Participants were similar with respect to personal or family history of fracture, self-reported fracture risk, weight, and height (Table 1). Differences in age, European ethnicity, and calculated 10-year hip fracture risk were statistically significant although small in magnitude.
Figure 2.
CONSORT flow diagram.
Table 1.
Participant characteristics in each arm of the study
| Benefit description | Absolute | Relative | ||||
|---|---|---|---|---|---|---|
| Harm description | Absolute | Relative | Absolute | Relative | Total | |
| n | 99 | 93 | 98 | 103 | 393 | |
| Age, years (SD) | 63.0(9.1) | 61.5(8.7) | 62.1 (8.1) | 65.7(8.3) | 63.1 (8.7) | |
| Weight, kg (SD) | 69.3(12.5) | 72.6(17.6) | 71.9(15) | 73.7(16.1) | 71.9(15.4) | |
| Height, cm (SD) | 160.5(12.3) | 161.5(6.6) | 161.4(7.1) | 161.1 (6.9) | 161.1 (8.5) | |
| Previous diagnosis of osteoporosis (%) | 5(5.1) | 3 (3.2) | 2 (2.0) | 7 (6.8) | 17(4.3) | |
| Fracture history | ||||||
| Personal (%) | 14 (14.1) | 14 (15.1) | 12 (12.2) | 17 (16.5) | 57 (14.5) | |
| Family history of hip fracture (%) | 13 (13.1) | 19 (20.4) | 13 (13.3) | 14 (13.6) | 59 (15.0) | |
| 10-year hip fracture risk, % | 1.2 | 0.7 | 1.7 | 2.6 | 2.6 | |
| Median (interquartile range) | 2.3 (0.4–2.7) | 2.1 (0.4–2.5) | 1.6 (0.5–2.1) | 2.8 (0.7–3.5) | 2.2 (0.5–2.7) | |
| Self-reported risk | ||||||
| Unlikely (%) | 83 (83.8) | 70 (75.3) | 87 (88.8) | 81 (78.6) | 321 (81.7) | |
| Likely (%) | 16 (16.2) | 23 (24.7) | 11 (11.2) | 22 (21.4) | 72 (18.3) | |
| Ethnicity | ||||||
| European (%) | 79 (79.8) | 78 (83.9) | 90 (91.8) | 94 (91.3) | 341 (86.8) | |
| Mãori (%) | 8 (8.1) | 6 (6.5) | 7 (7.1) | 6 (5.8) | 27 (6.9) | |
| Other (%) | 18 (18.2) | 16 (17.2) | 8 (8.2) | 12 (11.7) | 54 (13.7) | |
| Education | ||||||
| School only/none (%) | 45 (45.5) | 48 (51.6) | 52 (53.1) | 49 (47.6) | 194 (49.4) | |
| Tertiary (%) | 35 (35.4) | 28 (30.1) | 32 (32.7) | 38 (36.9) | 133 (33.8) | |
| Degree (%) | 19 (19.2) | 17 (18.3) | 14 (14.3) | 16 (15.5) | 66 (16.8) | |
10-year hip fracture risk is right skewed (skewness 3.2), median, (interquartile range), [Q2–Q3] are reported. Differences in age, European ethnicity, and calculated 10-year hip fracture risk were small but statistically significant.
Acceptance of treatment after presentation of benefit
All participants were allocated to first receive information on the treatment's benefit in either relative or absolute (pictorial) terms. Characteristics of both groups of participants are shown in Table 2.
Table 2.
Participant characteristics for presentation of treatment benefit
| Communication method |
|||
|---|---|---|---|
| Absolute | Relative | Total | |
| n | 192 | 201 | 393 |
| Age, years (SD) | 62.3 (8.9) | 63.9 (8.4) | 63.1 (8.7) |
| Weight, kg (SD) | 70.9(15.3) | 72.9(15.6) | 71.9(15.4) |
| Height, cm (SD) | 161.0(9.9) | 161.3(7) | 161.1 (8.5) |
| Previous diagnosis of osteoporosis (%) | 8 (4.2) | 9 (4.5) | 17(4.3) |
| Fracture history (%) | |||
| Personal | 28 (14.6) | 29 (14.4) | 57 (14.5) |
| Family history of hip fracture | 32 (16.7) | 27 (13.4) | 59 (15.0) |
| 10-year hip fracture risk, % | 1.0 | 1.3 | 2.6 |
| Median (interquartile range) | 2.2 (0.4–2.6) | 2.1 (0.6–2.7) | 2.2 (0.5–2.7) |
| Self-reported risk (%) | |||
| Unlikely | 153 (79.7) | 168 (83.6) | 321 (81.7) |
| Likely | 39 (20.3) | 33 (16.4) | 72 (18.3) |
| Ethnicity (%) | |||
| European | 157 (81.8) | 184 (91.5) | 341 (86.8) |
| Mãori | 14 (7.3) | 13 (6.5) | 27 (6.9) |
| Other | 34 (17.7) | 20 (10.0) | 54 (13.7) |
| Highest qualification (%) | |||
| School only/none | 93 (48.4) | 101 (50.2) | 194 (49.4) |
| Tertiary | 63 (32.8) | 70 (34.8) | 133 (33.8) |
| Degree | 36 (18.8) | 30 (14.9) | 66 (16.8) |
10-year hip fracture risk is right skewed (skewness 3.2), median, (interquartile range), [Q2–Q3] are reported.
A larger proportion of participants in the absolute (pictorial) risk group (43%) than in the relative group (36%) indicated they would be likely to accept treatment (Table 3). Crude odds for acceptance of treatment showed no difference between the absolute and relative risk groups (Table 3). After adjustment for age, education, previous diagnosis and self-reported risk, a significantly higheracceptance of treatment after presentation of treatment effects in absolute terms was detected (OR for acceptance of treatment after presentation of treatment effects in absolute terms 1.73, 95% CI = 1.10 to 2.73, P= 0.018).
Table 3.
Outcomes by presentation of benefit, irrespective of presentation of harm
| Communication method | OR (crude) | 95%CI | P-value | OR (adjusted) | 95% CI | P-value | ||
|---|---|---|---|---|---|---|---|---|
|
Acceptance of treatment |
||||||||
| Likely | Unlikely | |||||||
| Absolute (%) | 82 (43) | 110 (57) | 1.35 | 0.90 to 2.04 | 0.146 | 1.73 | 1.10 to 2.73 | 0.018 |
| Relative (%) | 71 (36) | 129 (65) | ||||||
|
Ease of understanding treatment effect |
||||||||
| Easy | Difficult | |||||||
| Absolute (%) | 180 (94) | 12 (6) | 2.03 | 1.00 to 4.34 | 0.051 | 2.06 | 0.97 to 4.58 | 0.066 |
| Relative (%) | 176 (88) | 24 (12) | ||||||
OR = odds ratio. Risk of taking treatment is adjusted for significant effects of age, previous diagnosis of osteoporosis, education, and self-reported risk. The model also included effects for fracture by trauma and New Zealand ethnicity which improved the fit of the model but were not significant. Understanding treatment effect is adjusted for New Zealand European ethnicity (not significant), working status and self-reported risk.
Difficulty in understanding the effect of treatment was reported by 9% of participants. Twice as many participants given a relative explanation of the treatment's effect reported difficulty than those given an absolute (pictorial) explanation, however this was not statistically significant and the CI was wide (adjusted OR 2.06, 95% CI = 0.97 to 4.58). (Table 3).
Multiple regression was used to investigate the effect of covariates on the likelihood of taking treatment (yes/no) after its benefit had been explained. The initial logistic model containing all main effects was reduced by forward and backward substitution leaving increased age, lower level of education, previous diagnosis of osteoporosis, higher self-reported risk and benefits explained in absolute (pictorial) terms all producing significantly higher likelihood of taking the treatment (Table 4). The strongest of these effects was a previous diagnosis of osteoporosis (OR 5.4, 95% CI = 1.52 to 26.12). History of fracture by trauma and New Zealand ethnicity increased the fit of the final model but were not significant, while there was no evidence for significant main effects due to 10-year hip fracture risk, alcohol, smoking, bone mineral density, weight, height, fracture (spontaneous or family history), employment or ethnicity other than New Zealand. The final model had adequate fit to the data (P<0.001), correctly predicting 65% of responses and had pseudo R2 of 0.14 using maximum likelihood and 0.19 using Cragg and Uhler's method.
Table 4.
Logistic regression predicting likelihood of taking treatment after benefit presented
| OR | 95% CI | P-value | |
|---|---|---|---|
| Age (per decade after 50 years) | 1.4 | (1.05 to 1.78) | 0.020 |
| Education (relative to high school or less) | |||
| Tertiary | 0.6 | (0.38 to 0.99) | 0.046 |
| Degree | 0.2 | (0.09 to 0.44) | <0.001 |
| New Zealand ethnicity | 1.7 | (0.84 to 3.49) | 0.151 |
| Previous diagnosis of osteoporosis | 5.4 | (1.52 to 26.12) | 0.017 |
| Self-reported risk (relative to very unlikely to have a fracture) | |||
| Quite unlikely | 1.8 | (1.1 to 3) | 0.021 |
| Quite/very likely | 1.9 | (1.01 to 3.65) | 0.045 |
| History of trauma fracture | 3.1 | (0.88 to 12.3) | 0.089 |
| Benefit (absolute) | 1.7 | (1.1 to 2.73) | 0.018 |
Influence of presentation of harm on acceptance of treatment
Of the 153 participants who, after presentation of the treatment's beneficial effect had indicated that they would accept treatment, 12 (14%) of those who were then presented harm in relative terms and 32 (46%) of those who were presented harm in absolute (pictorial) terms remained likely to again accept treatment. Thus, 109 (71%) of those who had initially indicated they would accept treatment altered their initial decision after the drug's harmful effect was presented. Participants who received the information on harm in relative terms were more likely to change their minds than those who received the same information in absolute (pictorial) terms (OR 4.89, 95% CI = 2.30 to 11.00, P<0.001) (Table 5). Of the 239 participants who had already declined treatment after the benefit was described, only three changed their minds and opted to take the treatment after presentation of harm.
Table 5.
Likelihood of accepting treatment following presentation of harm
| Take treatment after benefits explained | Method used to describe harm | Take treatment after harm explained | OR | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Unlikely | Likely | |||||
| Likely | Relative | 71 | 12 | 1.0 | ||
| Absolute | 38 | 32 | 4.89 | 2.30 to 11.00 | <0.001 | |
| Unlikely | Relative | 113 | 0 | |||
| Absolute | 123 | 3 | – | – | – | |
Multiple regression was used to investigate the effect of covariates on the likelihood of accepting treatment (yes/no) after its benefit and harm had been explained. The initial logistic model containing all main effects and an interaction term between harm and benefit indicated no evidence of a significant interaction between the presentation methods for harm and benefit. After elimination of covariates by forward and backward substitution only higher self-reported risk (OR 2.7, 95% CI = 1.3 to 5.5, P= 0.007) and harm explained absolute (pictorial) terms (OR 3.8, 95% CI = 1.9 to 8.1, P<0.001) produced significantly higher likelihood of taking the treatment. The final model had a pseudo R2 of 0.05 using maximum likelihood indicating there is considerable unexplained variation.
Given that benefit was explained first followed by presentation of harm in all four arms of the study, the effect of presentation of harm described here is always contingent on prior explanation of benefit. Hence participants' likelihood of accepting treatment after presentation of benefit may be included as an explanatory variable in a multiple regression model with the outcome being the final likelihood of accepting treatment after both benefit and then harm have been explained, along with all interaction terms with method of presentation of harm and benefit and main effects for the other demographic and explanatory variables. There was no evidence of interaction in the full model and after forward and backward substitution the only significant terms were the likelihood of acceptance after benefit was explained (OR 41.6, 95% CI = 14.4 to 176.9, P= 1.7×10−9) and absolute (pictorial) presentation of harm (OR 5.3, 95% CI = 2.6 to 11.8, P= 1.5×10−5). Both were associated with higher likelihood of accepting treatment after presentation of harm following presentation of benefit. The final model had pseudo R2 of 0.21 using maximum likelihood, the higher R2 due to 71.4% of participants not changing their mind after presentation of harm.
DISCUSSION
Summary
After adjustment for age, education, previous diagnosis of osteoporosis, and self-reported risk, presentation of a hypothetical treatment's benefits in absolute (pictorial) terms resulted in greater acceptance of the treatment. For participants who initially accepted treatment, presentation of the treatment's harm in relative terms was more likely to altertheir decision than was presentation of the treatment's harm in absolute (pictorial) terms.
A number of other factors influenced the decision to accept treatment. The strongest effect was a previous diagnosis of osteoporosis (OR 5.4, 95% CI = 1.52 to 26.12). This effect was independent of the calculated 10-year fracture risk, which is a more accurate estimate of fracture risk than a finding of osteoporosis alone.19,20 This may be an important consideration when discussing fracture risk with women who have confirmed osteoporosis but have a low calculated fracture risk.
Participants' level of education was also shown to have an effect on their likelihood of accepting treatment. Participants with a lower level of education were more likely to accept treatment than those with a tertiary level qualification. This may be related to better numeracy, a greater tolerance of risk or greater confidence in declining an offered treatment among better educated participants.
Strengths and limitations
The study was powered to detect a clinically important 18.6% difference in the proportion accepting treatment in the group presented with treatment benefits in relative and absolute terms.
The study's method closely mirrors current clinical practice in which treatment effects are interpreted in a patient-centred context. When long-term preventive treatments are considered, doctors are encouraged to calculate a 5-10 year estimate of risk (for example in fracture and cardiovascular disease prevention) and to use this to inform their discussion and treatment options. Therefore these findings may better reflect patient-centred decision making than previous studies which have used non-personalised baseline disease risk estimates.
Participants were recruited from the lists of 10 GPs at four practices in Christchurch, New Zealand. The participants were largely European and had a high level of education. The results may not be generalisable to other populations.
Differences in mean age and 10-year fracture risk in the four groups of participants were detected which may have introduced a bias to these findings. However, these differences were small in magnitude and it was found that the 10-year fracture risk did not have a significant effect on likelihood of accepting treatment in the model, and differences in age were effectively accounted for in the model.
The power calculation was based on an expected treatment acceptance rate of 80% for participants presented with treatment benefit in relative terms. The acceptance rate was lower than this (36% for relative description and 43% for absolute description) which may have limited the ability to detect smaller differences in treatment acceptance between the two communication methods.
While the presentation of a treatment's effects using different methods of risk communication may result in differing degrees of enthusiasm for treatment, it is not possible to determine from this study whether participants' decisions were congruent with the value they placed on hip fracture and its avoidance. However, participants with a higher level of self-reported fracture risk were more likely to accept treatment.
Comparison with exiting literature
Greater acceptance of treatment after presentation of benefit in absolute terms is an unexpected finding as previous work has found that relative presentation of benefits is associated with greater treatment acceptance.1-5 A difference between this study and previous work is that all participants in this study were given information about the treatment's effects in the context of their own personal risk presented as an estimated 10-year risk in absolute percentage terms. As this risk was low for most participants (mean risk 2.6%; standard deviation 3.9), its disclosure may have mitigated the usual effect of describing treatment benefits in relative terms as participants given information in relative terms in the current study may have made their own calculation of the absolute benefit treatment would offer them. However, this does not explain the increased acceptance of treatment in those participants informed of the treatment's benefit in absolute terms. As this is a novel finding that was significant only after adjustment for demographic and fracture risk factors, further investigation is required.
Presentation of treatment harm in relative terms was significantly more likely to cause participants to decline treatment than was presentation of the same information in absolute terms. This is an area of risk communication that has not been well studied, but this finding is consistent with previous observations of the effect of relative risk on treatment acceptance where this method of communicating risk appears to magnify the perceived effect of treatment.
Implications for research and practice
This study's findings suggest that when discussing preventive treatments with patients in the context of their personalised risk estimate, presentation of a treatment's beneficial effects in absolute terms may increase treatment acceptance compared to presentation of treatment benefits in relative terms. This is an unexpected finding which may have been due to the use of participants' personal fracture risk to set the context for the effect of treatment. This possible effect warrants further study.
The use of absolute estimates to explain treatment effects is considered to convey more meaningful information to patients and health professionals and therefore to allow better informed decision making. If the finding of increased treatment acceptance with absolute (pictorial) presentation of a treatment's beneficial and harmful effects is correct, then this does not undermine the well-established reasons for preferring this communication method. Indeed, it may reassure health professionals that using this method will not necessarily lead to reduced acceptance of valuable treatments by patients and hence encourage its more widespread use.
Presentation of the harmful effect of treatment in relative terms may strongly increase the chance of a patient declining treatment.
Acknowledgments
We are grateful to the participants, participating GPs and health centre staff. We would like to thank Dr Ruth Savage for her helpful comments.
Funding
This study was funded with a University of Otago Research Grant.
Ethical approval
The study protocol was reviewed and approved by the Upper South B Regional Ethics Committee (URB/08/11/052).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Covey J. A meta-analysis of the effects of presenting treatment benefits in different formats. Med Decis Making. 2007;27(5):638–654. doi: 10.1177/0272989X07306783. [DOI] [PubMed] [Google Scholar]
- 2.Hux JE, Naylor CD. Communicating the benefits of chronic preventive therapy: does the format of efficacy data determine patients' acceptance of treatment? Med Decis Making. 1995;15(2):152–157. doi: 10.1177/0272989X9501500208. [DOI] [PubMed] [Google Scholar]
- 3.Sarfati D, Howden-Chapman P, Woodward A, Salmond C. Does the frame affect the picture? A study into how attitudes to screening for cancer are affected by the way benefits are expressed. J Med Screen. 1998;5(3):137–140. doi: 10.1136/jms.5.3.137. [DOI] [PubMed] [Google Scholar]
- 4.Carling CLL, Kristoffersen DT, Montori VM, et al. The effect of alternative summary statistics for communicating risk reduction on decisions about taking statins: a randomized trial. PLoS Med. 2009;6(8):e1000134. doi: 10.1371/journal.pmed.1000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards A, Elwyn G, Covey J, et al. Presenting risk information — a review of the effects of ‘framing’ and other manipulations on patient outcomes. J Health Commun. 2001;6(1):61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- 6.Gigerenzer G. Reckoning with risk. Learning to live with uncertainty. London: Penquin Books; 2002. [Google Scholar]
- 7.Hoffrage U, Gigerenzer G. Using natural frequencies to improve diagnostic inferences. Acad Med. 1998;73(5):538–540. doi: 10.1097/00001888-199805000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Berry DC, Knapp P, Raynor DK. Provision of information about drug side-effects to patients. Lancet. 2002;359(9309):853–854. doi: 10.1016/s0140-6736(02)07923-0. [DOI] [PubMed] [Google Scholar]
- 9.Knapp P, Raynor DK, Berry DC. Comparison of two methods of presenting risk information to patients about the side effects of medicines. Qual Saf Health Care. 2004;13(3):176–180. doi: 10.1136/qshc.2003.009076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waters EA, Weinstein ND, Colditz GA, Emmons KM. Reducing aversion to side effects in preventive medical treatment decisions. J Exp Psychol Appl. 13(1):11–21. doi: 10.1037/1076-898X.13.1.11. [DOI] [PubMed] [Google Scholar]
- 11.Wells G, Cranney A, Peterson J, et al. Alendronate for the primaryand secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;23(1):CD001155. doi: 10.1002/14651858.CD001155.pub2. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women. NICE technology appraisal guidance. London: NICE; 2008. [Google Scholar]
- 13.Black DM, Delmas PD, Eastell R, et al. Once-yearlyzoledronicacidfortreatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 14.Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691. doi: 10.1136/bmj.c3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heckbert SR, Li G, Cummings SR, et al. Use of alendronate and risk of incident atrial fibrillation in women. Arch Intern Med. 2008;168(8):826–831. doi: 10.1001/archinte.168.8.826. [DOI] [PubMed] [Google Scholar]
- 16.Clarita VO, Shiri L, Sudhir R, et al. Unusual mid-shaft fractures during long-term bisphosphonate therapy. Clin Endocrinol (Oxf) 2010;72(2):161–168. doi: 10.1111/j.1365-2265.2009.03581.x. [DOI] [PubMed] [Google Scholar]
- 17.Lenart B, Neviaser A, Lyman S, et al. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporos Int. 2009;20(8):1353–1362. doi: 10.1007/s00198-008-0805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2009. [Google Scholar]
- 19.Kanis JA, Johnell O, et al. Prediction of fracture from low bone mineral density measurements overestimates risk. Bone. 2000;26(4):387–391. doi: 10.1016/S8756-3282(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 20.Kanis J, Oden A, Johnell O, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–1046. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]