Abstract
Purpose
To determine whether pre-matriculation characteristics and career-setting preferences of MD–PhD graduates differ according to their schools’ funding from the National Institute of General Medical Sciences’ Medical Scientist Training Program (MSTP).
Method
The Association of American Medical Colleges provided de-identified records for the national cohort of all 1993–2000 U.S. medical school matriculants, 3,180 of whom graduated with dual MD–PhD degrees by March 2, 2009. The authors examined prematriculation characteristics, educational outcomes, and career-setting preferences at graduation in association with MD–PhD program graduation from schools with long-standing MSTP-funded, recent MSTP-funded, and non-MSTP-funded programs.
Results
Of 3,142 MD–PhD graduates with prematriculation data, 30% were women and 36% were non-white. Graduates from long-standing MSTP-funded schools (63% of all graduates) composed a more highly selective group academically (based on MCAT scores) than did graduates from recent MSTP-funded (6%) and non-MSTP-funded schools (31%). Women and non-white graduates were more likely to have graduated from long-standing MSTP-funded schools. Controlling for MSTP funding and other variables, graduates with total debt of $100,000 or more were more likely to indicate non-research-related career-setting preferences (non-university clinical practice: odds ratio [OR] 3.58, 95% confidence interval [CI] 1.86–6.87; undecided/other: OR 2.15, 95% CI 1.29–3.60). Neither gender nor race/ethnicity was independently associated with graduates’ career-setting preferences.
Conclusions
Women and non-white MD–PhD graduates more likely graduated from long-standing MSTP than non-MSTP-funded schools. Controlling for institutional MSTP funding, MD–PhD graduates with high debt were more likely to indicate non-research-related career-setting preferences.
The National Institute of General Medical Sciences’ (NIGMS) Medical Scientist Training Program (MSTP) began in 1964 with funding to three medical schools that offered joint MD–PhD programs; by 1998, the number of MSTP-funded programs had increased to 32. A 1998 study of MD–PhD graduates from 1971 to 1990 reported differences in graduates’ career paths by the MSTP support they had received; compared with graduates from institutions with MSTP funding, those from institutions without MSTP funding were less likely to have research support and academic appointments and more likely to be engaged in clinical practice.1 Since 1998, the number of medical schools with MSTP funding has continued to grow; as of 2010, there were 42 medical schools with MSTP funding .2,3 However, because over 100 medical schools in the U.S. offer MD–PhD programs,2,3 the majority of MD–PhD programs do not receive MSTP funding.
The extent to which differences in educational outcomes and career plans exist among MD–PhD program graduates of medical schools with or without MSTP-funding has not been examined. Thus, we sought to examine pre-matriculation characteristics of a national cohort of contemporary MD–PhD program graduates to determine whether graduates who matriculated at medical schools with long-standing MSTP funding differed from those who matriculated at medical schools with recent MSTP funding and schools that received no MSTP funding. We hypothesized that the graduates’ pre-matriculation characteristics would differ according to their school’s receipt of MSTP funding and that schools’ receipt of MSTP funding would be associated with MD–PhD graduates’ educational outcomes and career plans.
Method
Cohort
Our sample was part of a larger study database of individualized, de-identified records for all 1993–2000 Liaison Committee on Medical Education (LCME)-accredited U.S. medical school matriculants. Our study sample included all those matriculants who had graduated with MD–PhD degrees by March 2, 2009, the date we received the data from the Association of American Medical Colleges (AAMC). Our study sample included graduates who had enrolled in MD–PhD programs either at the time of or sometime after matriculation to medical school and were enrolled in MD–PhD programs at graduation. We based each matriculant’s most recent degree-program enrollment on information reported to the AAMC by institutional registrars. Because it reportedly takes about eight years to complete MD–PhD dual degree requirements,4 we chose 2000 as the last year of matriculation to allow sufficient time for MD–PhD program enrollees to obtain their MD–PhD degrees.
Measures
The AAMC Student Record System’s variables we used included matriculation date, graduation date, sex, and race/ethnicity. For our analysis, we categorized race/ethnicity as Asian/Pacific Islander, other/unknown (i.e., self-identified as other or multiple races or did not respond), underrepresented minority in medicine (including Black, Hispanic, and American Indian/Alaska Native), and white (which we used as the reference category). We also obtained the Carnegie classifications for the MD–PhD graduates’ undergraduate degree-granting institutions. There were 12 Carnegie Classifications,5 from which we created a six-category variable: 1) baccalaureate colleges–arts and sciences; 2) research universities (high research activity) and doctoral/research universities; 3) master’s colleges/universities; 4) other institutions (all other Carnegie Classifications of non-research-oriented undergraduate institutions); 5) Carnegie Classification not specified; and 6) research universities (very high research activity) as the reference category. Medical school duration was calculated as the number of years from matriculation to graduation.
The AAMC provided matriculants’ Medical College Admission Test (MCAT) results and first-attempt, three-digit United States Medical Licensing Examination (USMLE) Step 1 scores (the latter with permission from the National Board of Medical Examiners). We calculated a composite MCAT score as the sum of verbal reasoning, physical science, and biological science scores. We then categorized composite MCAT scores by quartiles (<31, 31–33, 34–35, and ≥36 as the reference) and included graduates without MCAT scores as a fifth category.
The AAMC provided responses to selected items on the AAMC Graduation Questionnaire (GQ) for all GQ respondents in our study sample. The GQ, administered on a confidential and voluntary basis to graduating students during the spring of their final year of medical school, covers a broad range of topics.6 Our analysis included two variables regarding career plans (specialty choice and career-setting preference) and one variable for total debt at graduation. Based on responses to GQ items pertaining to intended specialty for board certification and intent to sub-specialize in that specialty, we created 11 specialty-choice categories: pediatrics (including pediatrics subspecialties), dermatology, pathology, neurology, radiology, surgical specialties, psychiatry, surgery, all other non-surgical specialties, no specialty chosen (for graduates who responded “no” or “undecided” to the question about plans to become specialty board certified), and internal medicine (including internal medicine/pediatrics and internal medicine subspecialties). We selected internal medicine as the reference group based on a recent survey of graduates of 24 MD–PhD programs, which indicated that internal medicine was the specialty they most frequently chose for residency training and was also the most frequently cited departmental affiliation by MD–PhD program alumni who held full-time academic appointments.4 We created three categories from the career-setting preference choices listed on the GQ: full-time (non-university) clinical practice, undecided/other (including state/federal or medical/healthcare administration and other), and—as the reference group—research-related careers, including full-time university faculty in basic science teaching/research, full-time university faculty in clinical teaching/research, and non-university research scientist (hereafter, full-time faculty/research scientist). The predictive validity of the career-setting preference GQ item for full-time faculty appointments has been established.7 Based on responses to the GQ question about total debt (including both premedical and medical-school debt), we created a four-category variable: ≥$100,000, $50,000–$99,999, $1–$49,999, and no debt as the reference group.
In addition, the AAMC provided a three-category variable for medical school receipt of MSTP funding based on rosters of MSTP-funded institutions,1 updated annually by the NIGMS.2 Of the 129 U.S. LCME-accredited medical schools to which students had matriculated between 1993 and 2000, 33 medical schools (26%) had been receiving MSTP funding for at least six of these eight years.2 These schools were categorized as long-standing MSTP-funded schools. Six schools (5%) began receiving funding in 1998 or 1999; they were categorized as recent MSTP-funded schools. The remaining 90 schools (69%) had received no MSTP funding from 1993 to 2000 and were categorized as non-MSTP-funded schools.
Records for each student were linked using a unique, AAMC-generated identification number and merged into a single file for analysis. The Institutional Review Board at Washington University School of Medicine approved this study.
Statistical analysis
To test the first hypothesis, we ran three separate multivariate logistic regression models to identify pre-matriculation characteristics of the MD–PhD graduates that were associated with enrollment at 1) long-standing MSTP-funded vs. non-MSTP-funded schools (reference), 2) recent MSTP-funded vs. non-MSTP-funded schools (reference), and 3) long-standing MSTP-funded vs. recent MSTP-funded schools (reference). To test the second hypothesis, we ran separate multivariate logistic regression models to identify independent predictors of full-time, non-university clinical practice and undecided/other career-setting preferences, each compared with full-time faculty/research scientist. We report adjusted odds ratios (OR) and 95% confidence intervals (CI) to show the associations between each predictor variable of interest and the dependent variables of interest. Tests were performed using SPSS 17.0.3 (SPSS, Inc., Chicago, IL, 2009). Two-sided P < .05 was considered significant.
Results
From 1993 to 2000, there were 129,867 matriculants in U.S. LCME-accredited medical schools. Of these, 124,896 had graduated by March 2, 2009, including 3,180 (2.5%) MD–PhD program enrollees. We excluded 38 of those graduates for lack of information regarding their race/ethnicity. Our final study sample of 3,142 graduates included 1,978 (63%) who graduated from long-standing MSTP-funded schools, 176 (5.6%) who graduated from recent MSTP-funded schools, and 988 (31.4%) who graduated from non-MSTP-funded schools. Descriptive statistics of our study sample are shown in Table l.
Table 1.
Characteristics of 3,142 U.S. MD-PhD Program Graduates Who Matriculated in Medical School in 1993–2000, by Medical Scientist Training Program (MSTP) Funding* of Their Medical Schools
| Variable | All schools | Long-standing MSTP-funded schools |
Recent MSTP- funded schools |
Non-MSTP- funded schools |
|---|---|---|---|---|
| Characteristics at matriculation | No. (%) | No. (%) | No. (%) | No. (%) |
| Total | 3,142 (100) | 1,978 (100) | 176 (100) | 988 (100) |
| Gender | ||||
| Men | 2,194 (69.8) | 1,394 (70.5) | 116 (65.9) | 684 (69.2) |
|
| ||||
| Women | 948 (30.2) | 584 (29.5) | 60 (34.1) | 304 (30.8) |
|
| ||||
| Race/ethnicity | ||||
| White | 2,026 (64.5) | 1,194 (60.4) | 129 (73.3) | 703 (71.2) |
|
| ||||
| Asian/Pacific Islander | 817 (26.0) | 573 (29.0) | 36 (20.5) | 208 (21.1) |
|
| ||||
| Underrepresented minority | 299 (9.5) | 211 (10.7) | 11 (6.3) | 77 (7.8) |
|
| ||||
| Undergraduate institution Carnegie Classification | ||||
| Research universities (very high research activity) |
2,061 (65.6) | 1,435 (72.5) | 101 (57.4) | 525 (53.1) |
|
| ||||
| Other institutions | 27 (0.9) | 6 (0.3) | 3 (1.7) | 18 (1.8) |
|
| ||||
| Baccalaureate colleges–arts and sciences | 392 (12.5) | 216 (10.9) | 31 (17.6) | 145 (14.7) |
|
| ||||
| Master’s colleges and universities | 206 (6.6) | 85 (4.3) | 21 (11.9) | 100 (10.1) |
|
| ||||
| Research universities (high research activity) and doctoral/research universities |
260 (8.3) | 118 (6.0) | 10 (5.7) | 132 (13.4) |
|
| ||||
| Not specified | 196 (6.2) | 118 (6.0) | 10 (5.7) | 68 (6.9) |
|
| ||||
| MCAT score categories | ||||
| ≥ 36 | 907 (28.9) | 770 (38.9) | 33 (18.8) | 104 (10.5) |
|
| ||||
| 34–35 | 622 (19.8) | 430 (21.7) | 44 (25.0) | 148 (15.0) |
|
| ||||
| 31–33 | 843 (26.8) | 486 (24.6) | 59 (33.5) | 298 (30.2) |
|
| ||||
| < 31 | 723 (23.0) | 277 (14.0) | 36 (20.5) | 410 (41.5) |
|
| ||||
| Not available | 47 (1.5) | 15 (0.8) | 4 (2.3) | 28 (2.8) |
|
| ||||
| No.; Mean (SD) | No.; Mean (SD) | No.; Mean (SD) | No.; Mean (SD) | |
|
|
||||
| MCAT scores | 3,095; 33.3 (3.9) | 1,963; 34.3 (3.6) | 172; 32.8 (3.3) | 960; 31.1 (3.7) |
| Characteristics at graduation | No. (%) | No. (%) | No. (%) | No. (%) |
|---|---|---|---|---|
| Total† | 2,028 (100) | 1,217 (100) | 120 (100) | 691 (100) |
| Specialty choice † | ||||
| Internal medicine | 415 (20.5) | 277 (22.8) | 21 (17.5) | 117 (16.9) |
|
| ||||
| No specialty selected | 138 (6.8) | 85 (7.0) | 10 (8.3) | 43 (6.2) |
|
| ||||
| Other specialties | 266 (13.1) | 134 (11.0) | 18 (15.0) | 114 (16.5) |
|
| ||||
| Psychiatry | 96 (4.7) | 57 (4.7) | 9 (7.5) | 30 (4.3) |
|
| ||||
| Radiology | 176 (8.7) | 104 (8.5) | 13 (10.8) | 59 (8.5) |
|
| ||||
| Dermatology | 123 (6.1) | 81 (6.7) | 9 (7.5) | 33 (4.8) |
|
| ||||
| Ophthalmology | 84 (4.1) | 53 (4.4) | 5 (4.2) | 26 (3.8) |
|
| ||||
| Surgical specialties | 240 (11.8) | 133 (10.9) | 7 (5.8) | 100 (14.5) |
|
| ||||
| Neurology | 136 (6.7) | 86 (7.1) | 9 (7.5) | 41 (5.9) |
|
| ||||
| Pathology | 152 (7.5) | 97 (8.0) | 9 (7.5) | 46 (6.7) |
|
| ||||
| Pediatrics | 202 (10.0) | 110 (9.0) | 10 (8.3) | 82 (11.9) |
|
| ||||
| Total debt at graduation † | ||||
| No debt | 712 (35.1) | 519 (42.6) | 49 (40.8) | 144 (20.8) |
|
| ||||
| $1–$49,999 | 723 (35.7) | 466 (38.3) | 44 (36.7) | 213 (30.8) |
|
| ||||
| $50,000–$99,999 | 362 (17.9) | 159 (13.1) | 12 (10.0) | 191 (27.6) |
|
| ||||
| ≥$100,000 | 231 (11.4) | 73 (6.0) | 15 (12.5) | 143 (20.7) |
|
| ||||
| No.; Mean (SD) | No.; Mean (SD) | No.; Mean (SD) | No.; Mean (SD) | |
|
|
||||
| First-attempt USMLE Step 1 scores | 3,136; 227.0 (19.1) | 1,972; 229.4 (18.3) | 176; 226.9 (18.2) | 988; 222.3 (19.8) |
|
| ||||
| Medical school duration, years | 3,116; 7.8 (1.4) | 1,970; 8.0 (1.3) | 176; 7.8 (1.2) | 970; 7.3 (1.5) |
Long-standing MSTP-funded schools had received MSTP funding in at least six of the eight years from 1993 through 2000; recent MSTP-funded schools had begun receiving MSTP funding in 1998 or 1999; non-MSTP-funded schools had received no MSTP funding in those eight years.
Reported on the AAMC Graduation Questionnaire.
Table 2 shows the results of the multivariate regression models of pre-matriculation variables associated with MSTP-funding category. The Hosmer and Lemeshow test indicated that each model was a good fit to the data (P > .05). Women were more likely than men to have enrolled in long-standing or recent MSTP-funded schools compared with non-MSTP-funded schools. Underrepresented minorities and Asian/Pacific Islanders were more likely than white graduates to have enrolled at long-standing MSTP-funded compared with either recent MSTP-funded or non-MSTP-funded schools. Graduates with MCAT scores <36 or without MCAT scores and those who had obtained undergraduate degrees at institutions other than research universities (very high research activity) were less likely to have enrolled at long-standing MSTP-funded medical schools than at either recent MSTP-funded or non-MSTP-funded schools. Only graduates in the lower two quartiles of MCAT scores and those who obtained undergraduate degrees at research universities (high research activity) and doctoral/research universities were significantly less likely to have enrolled at recent MSTP-funded schools compared with non-MSTP-funded schools.
Table 2.
Multivariate Logistic Regression Models of Pre-matriculation Characteristics of 3,142 U.S. MD–PhD Program Graduates Who Matriculated in Medical School in 1993–2000 in Association with the Medical Scientist Training Program (MSTP) Funding* of Their Medical Schools
| Long-standing MSTP vs. non-MSTP (reference) |
Recent MSTP vs. non-MSTP (reference) |
Long-standing MSTP vs. recent MSTP (reference) |
||||
|---|---|---|---|---|---|---|
| Variable | Adjusted OR (95% CI) | P value† | Adjusted OR (95% CI) | P value† | Adjusted OR (95% CI) | P value† |
| Gender | ||||||
| Men (reference) | 1.00 | 1.00 | 1.00 | |||
|
| ||||||
| Women | 1.40 (1.16–1.70) | .001 | 1.44 (1.01–2.06) | .046 | 1.01 (0.72–1.43) | .944 |
|
| ||||||
| Race/ethnicity | ||||||
| White (reference) | 1.00 | 1.00 | 1.00 | |||
|
| ||||||
| Asian/Pacific Islander | 1.34 (1.09–1.65) | .006 | 0.95 (0.62–1.44) | .804 | 1.49 (1.00–2.21) | .047 |
|
| ||||||
| Underrepresented minority | 4.20 (3.06–5.78) | <.001 | 1.13 (0.57–2.24) | .731 | 3.47 (1.75–6.85) | <.001 |
|
| ||||||
|
Undergraduate institution Carnegie
Classification |
||||||
| Research universities (very high research activity) |
1.00 | 1.00 | 1.00 | |||
|
| ||||||
| Other institutions | 0.13 (0.05–0.35) | <.001 | 1.01 (0.28–3.59) | .987 | 0.17 (0.04–0.70) | .014 |
|
| ||||||
| Baccalaureate colleges–arts and sciences |
0.78 (0.60–1.02) | .068 | 1.25 (0.79–1.99) | .342 | 0.59 (0.38–0.92) | .019 |
|
| ||||||
| Master’s colleges and universities | 0.47 (0.33–0.66) | <.001 | 1.51 (0.88–2.62) | .137 | 0.30 (0.18–0.53) | <.001 |
|
| ||||||
| Research universities (high research activity) and doctoral/research universities |
0.41 (0.30–0.55) | .001 | 0.43 (0.22–0.85) | .016 | 0.92 (0.46–1.84) | .817 |
|
| ||||||
| Not specified | 0.68 (0.48–0.96) | .028 | 0.80 (0.39–1.64) | .545 | 0.89 (0.45–1.77) | .738 |
|
| ||||||
| MCAT score | ||||||
| ≥36 (reference) | 1.00 | 1.00 | 1.00 | |||
|
| ||||||
| 34–35 | 0.37 (0.28–0.49) | <.001 | 0.90 (0.53–1.52) | .691 | 0.42 (0.26–0.68) | <.001 |
|
| ||||||
| 31–33 | 0.21 (0.16–0.27) | <.001 | 0.59 (0.36–0.96) | .035 | 0.36 (0.23–0.57) | <.001 |
|
| ||||||
| <31 | 0.07 (0.05–0.09) | <.001 | 0.23 (0.13–0.40) | <.001 | 0.30 (0.18–0.51) | <.001 |
|
| ||||||
| Not available | 0.06 (0.03–0.13) | <.001 | 0.43 (0.14–1.34) | .147 | 0.16 (0.05–0.53) | .002 |
Long-standing MSTP-funded schools had received MSTP funding in at least six of the eight years from 1993 through 2000; recent MSTP-funded schools had begun receiving MSTP funding in 1998 or 1999; non-MSTP-funded schools had received no MSTP funding in those eight years.
P values are adjusted for other variables in the logistic regression model.
MD–PhD graduates’ educational outcomes and career plans also differed on the basis of their medical schools’ MSTP funding. As shown in Table 1, mean first-attempt USMLE Step l scores were higher and mean duration in medical school was longer among graduates of long-standing MSTP-funded and recent MSTP-funded schools than among graduates of non-MSTP-funded schools. Of the 3,142 MD–PhD graduates in our sample, 2,028 (64.5%) completed the GQ items of interest relating to total debt, specialty choice, and career-setting preference at graduation. These GQ respondents included 61.5% of our sample’s graduates of long-standing MSTP-funded schools, 68.2% of graduates of recent MSTP-funded schools, and 69.9% of graduates of non-MSTP-funded schools. Graduates’ total debt and specialty choices also varied by medical school MSTP funding. The proportion of graduates from non-MSTP-funded schools who reported debt of $50,000 or more was more than twice that of graduates from schools with either long-standing or recent MSTP funding (Table 1). Of the 1,890 respondents who made specialty choices, 905 (47.9%) chose either neurology, internal medicine, pediatrics, or pathology. Internal medicine was the single most frequently chosen specialty, particularly among graduates of long-standing MSTP-funded schools.
Table 3 shows the descriptive statistics for GQ respondents included in the regression analysis, grouped by career-setting preference category. Table 4 shows the results of the multivariate regression model of variables associated with career-setting preference. The Hosmer and Lemeshow test indicated that each model was a good fit to the data (each P > .05). Graduates who had a total debt of ≥$50,000, did not make a specialty choice, or made a specialty choice of radiology, pathology, pediatrics, and other non-surgical specialties were each more likely, whereas graduates with a lengthier medical-school duration were less likely, to indicate a career-setting preference of full-time, non-university clinical practice compared with full-time faculty/research scientist. Graduates with a total debt of ≥$100,000 and those who did not make a specialty choice or chose psychiatry or radiology were each more likely, whereas graduates with a lengthier medical-school duration were less likely, to indicate their career-setting preference as undecided/other compared with full-time faculty/research scientist. Gender, race/ethnicity, and MSTP-funding category were not independently associated with career-setting preference in either model.
Table 3.
Characteristics of 2,010 U.S. MD–PhD Program Graduates Who Matriculated in Medical School in 1993–2000, by Career-setting Preference as Reported on the AAMC Graduation Questionnaire
| Variable | Total | Full-time faculty/research scientist |
Non-university clinical practice |
Undecided/other |
|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | |
| Total | 2,010 (100) | 1,695 (100) | 121 (100) | 194 (100) |
| Gender | ||||
| Men | 1,363 (67.8) | 1,159 (68.4) | 81 (66.9) | 123 (63.4) |
|
| ||||
| Women | 647 (32.2) | 536 (31.6) | 40 (33.1) | 71 (36.6) |
|
| ||||
| Race/ethnicity | ||||
| White | 1,317 (65.5) | 1,101 (65.0) | 81 (66.9) | 135 (69.6) |
|
| ||||
| Asian/Pacific Islander | 521 (25.9) | 457 (27.0) | 24 (19.8) | 40 (20.6) |
|
| ||||
| Underrepresented minority | 172 (8.6) | 137 (8.1) | 16 (13.2) | 19 (9.8) |
|
| ||||
|
Medical school Medical Scientist
Training Program (MSTP) funding * |
||||
| Non-MSTP-funded | 680 (33.8) | 538 (31.7) | 60 (49.6) | 82 (42.3) |
|
| ||||
| Recent MSTP-funded | 120 (6.0) | 102 (6.0) | 5 (4.1) | 13 (6.7) |
|
| ||||
| Long-standing MSTP-funded | 1,210 (60.2) | 1,055 (62.2) | 56 (46.3) | 99 (51.0) |
|
| ||||
| Total educational debt | ||||
| No debt | 708 (35.2) | 631 (37.2) | 20 (16.5) | 57 (29.4) |
|
| ||||
| $1–$49,999 | 717 (35.7) | 627 (37.0) | 37 (30.6) | 53 (27.3) |
|
| ||||
| $50,000–$99,999 | 357 (17.8) | 286 (16.9) | 27 (22.3) | 44 (22.7) |
|
| ||||
| ≥$100,000 | 228 (11.3) | 151 (8.9) | 37 (30.6) | 40 (20.6) |
|
| ||||
| Specialty choice | ||||
|
| ||||
| Internal medicine | 413 (20.5) | 375 (22.1) | 13 (10.7) | 25 (12.9) |
|
| ||||
| No specialty selected | 134 (6.7) | 75 (4.4) | 11 (9.1) | 48 (24.7) |
|
| ||||
| Other specialties | 266 (13.2) | 211 (12.4) | 28 (23.1) | 27 (13.9) |
|
| ||||
| Psychiatry | 95 (4.7) | 77 (4.5) | 6 (5.0) | 12 (6.2) |
|
| ||||
| Radiology | 173 (8.6) | 137 (8.1) | 13 (10.7) | 23 (11.9) |
|
| ||||
| Dermatology | 122 (6.1) | 107 (6.3) | 7 (5.8) | 8 (4.1) |
|
| ||||
| Ophthalmology | 84 (4.2) | 76 (4.5) | 2 (1.7) | 6 (3.1) |
|
| ||||
| Surgery specialties | 236 (11.7) | 210 (12.4) | 13 (10.7) | 13 (6.7) |
|
| ||||
| Neurology | 134 (6.7) | 123 (7.3) | 3 (2.5) | 8 (4.1) |
|
| ||||
| Pathology | 152 (7.6) | 132 (7.8) | 9 (7.4) | 11 (5.7) |
|
| ||||
| Pediatrics | 201 (10.0) | 172 (10.1) | 16 (13.2) | 13 (6.7) |
|
| ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
|
|
||||
| First-attempt USMLE Step l scores | 227.3 (18.9) | 228.3 (18.5) | 220.5 (20.2) | 222.6 (20.5) |
|
| ||||
| Medical school duration, years | 7.6 (1.4) | 7.8 (1.3) | 6.3 (1.9) | 7.0 (1.8) |
Long-standing MSTP-funded schools had received MSTP funding in at least six of the eight years from 1993 through 2000; recent MSTP-funded schools had begun receiving MSTP funding in 1998 or 1999; non-MSTP-funded schools had received no MSTP funding in those eight years.
Table 4.
Predictors of Non-University Clinical Practice and Undecided/Other Career-Setting Preferences of 2,010 U.S. MD–PhD Program Graduates Who Matriculated in Medical School in 1993–2000, Each Compared with Full-Time Faculty/Research Scientist Career-Setting Preference*
| Non-university clinical practice |
Undecided/other | |||
|---|---|---|---|---|
| Variable | Adjusted OR (95% CI) |
P value† | Adjusted OR (95% CI) |
P value† |
| Gender | ||||
| Men (reference) | 1.00 | 1.00 | ||
|
| ||||
| Women | 0.78 (0.50–1.21) | .263 | 1.10 (0.78–1.54) | .598 |
|
| ||||
| Race/ethnicity | ||||
| White (reference) | 1.00 | 1.00 | ||
|
| ||||
| Asian/Pacific Islander | 1.02 (0.60–1.70) | .953 | 0.77 (0.51–1.16) | .210 |
|
| ||||
| Underrepresented minority | 1.39 (0.73–2.65) | .318 | 0.87 (0.48–1.56) | .635 |
|
| ||||
|
Institutional Medical Scientist Training Program (MSTP) funding ‡ |
||||
| Non-MSTP-funded (reference) | 1.00 | 1.00 | ||
|
| ||||
| Recent MSTP-funded | 0.66 (0.24–1.84) | .426 | 1.09 (0.56–2.12) | .804 |
|
| ||||
| Long-standing MSTP-funded | 0.99 (0.64–1.52) | .950 | 0.93 (0.65–1.33) | .693 |
|
| ||||
| First-attempt USMLE Step l scores | 0.99 (0.98–1.00) | .059 | 0.99 (0.98–1.00) | .054 |
|
| ||||
| Medical school duration | 0.57 (0.50–0.65) | <.001 | 0.74 (0.66–0.82) | <.001 |
|
| ||||
| Total educational debt | ||||
| No debt (reference) | 1.00 | 1.00 | ||
|
| ||||
| $1–$49,999 | 1.70 (0.96–3.03) | .071 | 0.87 (0.57–1.31) | .497 |
|
| ||||
| $50,000–$99,999 | 1.99 (1.05–3.77) | .036 | 1.38 (0.87–2.21) | .173 |
|
| ||||
| ≥$100,000 | 3.58 (1.86–6.87) | <.001 | 2.15 (1.29–3.60) | .003 |
|
| ||||
| Specialty choice | ||||
| Internal medicine (reference) | 1.00 | 1.00 | ||
|
| ||||
| No specialty selected | 5.05 (2.03–12.55) | <.001 | 9.83 (5.58–17.33) | <.001 |
|
| ||||
| Other specialties | 2.63 (1.26–5.48) | .010 | 1.36 (0.75–2.48) | .309 |
|
| ||||
| Psychiatry | 2.46 (0.84–7.19) | .101 | 2.32 (1.09–4.92) | .029 |
|
| ||||
| Radiology | 2.84 (1.22–6.62) | .015 | 2.54 (1.37–4.70) | .003 |
|
| ||||
| Dermatology | 2.34 (0.87–6.25) | .091 | 1.21 (0.52–2.79) | .661 |
|
| ||||
| Ophthalmology | 0.81 (0.17–3.78) | .787 | 1.14 (0.44–2.94) | .783 |
|
| ||||
| Surgery specialties | 1.22 (0.53–2.82) | .643 | 0.75 (0.37–1.53) | .426 |
|
| ||||
| Neurology | 0.84 (0.22–3.11) | .787 | 1.09 (0.47–2.51) | .842 |
|
| ||||
| Pathology | 3.20 (1.26–8.09) | .014 | 1.32 (0.62–2.80) | .475 |
|
| ||||
| Pediatrics | 2.36 (1.05–5.30) | .037 | 0.93 (0.45–1.90) | .839 |
As indicated on the AAMC Graduation Questionnaire.
P values are adjusted for other variables in the logistic regression model.
Long-standing MSTP-funded schools had received MSTP funding in at least six of the eight years from 1993 through 2000; recent MSTP-funded schools had begun receiving MSTP funding in 1998 or 1999; non-MSTP-funded schools had received no MSTP funding in those eight years.
Discussion
Overall, the MD–PhD graduates in our study were high achievers academically. Those who had graduated from long-standing MSTP-funded schools were particularly likely to have received undergraduate degrees from research universities with very high research activity and to have matriculated with MCAT scores of >36, and most graduates, regardless of their medical schools’ MSTP funding, planned to pursue research-related careers . But the graduates’ pre-matriculation characteristics, educational outcomes, and career plans differed among the three MSTP-funding groups. Our results should be considered in the context of financial support of MD–PhD program enrollees, the range of contemporary MD–PhD graduates’ specialty choices, and ongoing concerns about physician-scientist workforce diversity.8
Financial support for MD-PhD program enrollees
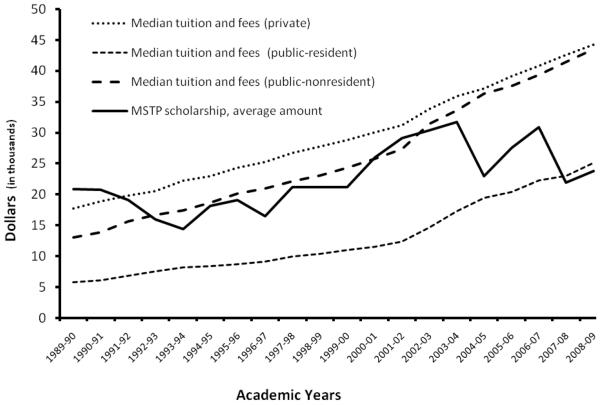
Financial support for MD–PhD program enrollees, particularly for those enrolled in MSTP-funded programs, has changed substantially in recent years. In the 1989–1990 academic year, the average MSTP award per position exceeded the median annual private school tuition, so MD–PhD enrollees at MSTP-funded schools could be supported largely by MSTP funding alone (Figure 1). However, by 2007–2008, the average MSTP award had decreased relative to tuition costs to slightly less than the median annual public school tuition. MD–PhD enrollees at both MSTP-funded and non-MSTP-funded schools now receive funding from numerous NIH institutes as well as from non-federal funding organizations, such as the American Cancer Society and the American Diabetes Association, among others.9 In 2007–2008, non-need-based MSTP funding accounted for $33.6 million in grants/scholarships awarded without a service commitment. Medical schools themselves supported their MD–PhD program enrollees in the substantial amount of $69.4 million in non-need-based MD–PhD support awarded without a service commitment. This total of $103 million accounted for over 20% of all medical school grants/scholarships awarded without a service commitment (both need-based and non-need-base), both school-funded and outside-funded support.10
Figure 1.
Trends in Medical Scientist Training Program (MSTP) awards relative to increasing medical school tuition costs, 1989–2008.24-26
In these economic hard times, MD–PhD programs may be challenged to financially support the steadily increasing numbers of enrollees.11 Furthermore, these enrollees may require support for lengthier periods; our findings, and those of another recent study,4 indicate that MD–PhD program enrollees now take longer than did earlier cohorts to complete the dual-degree program.1 Graduates of MSTP-funded schools in our sample took longer than graduates of non-MSTP funded schools to complete the dual-degree requirements. However, not surprisingly, we observed greater levels of debt among graduates of non-MSTP-funded schools, which likely reflects the typically fully funded status of MD–PhD positions at MSTP-funded, but not necessarily at non-MSTP-funded, schools.12 Despite the fully funded nature of MD–PhD positions at MSTP-funded schools, 19.1% (232/1217) of graduates from long-standing MSTP-funded schools and 22.5% (27/120) of graduates from recent MSTP-funded schools reported at least $50,000 in debt at graduation (Table 1). Since indebted graduates are more likely to prefer full-time clinical practice, strategies to minimize debt among MD-PhD graduates at both MSTP-funded and non-MSTP-funded schools could help MD–PhD programs satisfy their missions to train physician-scientists who go on to research-related careers. These strategies might include programmatic financial counseling/planning support for all MD–PhD enrollees13 and loan repayment programs such as those offered by the NIH.8,14
The issue of debt, in particular, speaks directly to recently published perspectives as to whether federal institutional funding of MSTPs should be eliminated in favor of individual training grants to selected young physician-scientists15 or more heavily supported.16 Our findings suggest that minimizing educational debt, regardless of how it is done, is warranted as a means of maximizing the likelihood that MD–PhD program graduates pursue careers as full-time faculty/research scientists. Notably, when we controlled for level of debt, we found that the longer it took program enrollees to complete the dual degree, the more likely they were to indicate a preference for a career as full-time faculty/research scientist.
Specialty choice
In a 1965–1978 cohort of MD–PhD program graduates, more than 70% chose neurology, pathology, internal medicine, and pediatrics specialties for residency; in a 1999–2007 cohort, this percentage steadily declined to less than 60%.4 Findings from our sample, in which only 48% of MD–PhD graduates choosing any specialty chose these specialties, also indicated that differences in specialty choices were associated with medical school MSTP funding. Thus, observations about specialty choices among graduates of MSTP-funded schools cannot necessarily be generalized to all MD–PhD graduates.17
Similar to a recent report of MD–PhD graduates who chose private practice careers after residency training,4 we observed associations between career-setting preferences and specialty choices. Only 6% of graduates in our sample had not committed to a specialty choice, but this group was more likely to indicate that they preferred clinical practice, were undecided, or had other career plans than they were to indicate a preference for full-time faculty/research scientist careers. Efforts to expose enrollees to a broad range of specialties and MD–PhD role models in these specialties13 seem warranted, especially since MD–PhD enrollees have reported low levels of satisfaction with the career planning information they receive compared with other aspects of their training.13 They also should be made aware of residency-training programs tailored to the needs and concerns of physician-scientists.18-20 Such a program—in internal medicine, for example—could maximize the retention in biomedical research of MD–PhD graduates who are interested in specializing in internal medicine while pursuing research-based careers.18 Enrollees also should be made aware of the research pathway options for graduate medical education that fulfill training requirements for eligibility offered by member boards of the American Board of Medical Specialties, such as the American Board of Internal Medicine,21 among others.
Physician-scientist workforce diversity
Finally, our results should be considered in the context of recent efforts to increase biomedical research workforce diversity. In our sample, 30% of the MD–PhD graduates were women, an improvement over a previous report of less than 20%.1 Furthermore, in a recent survey, directors of 24 MD–PhD programs indicated that, in 2008, 37% of their trainees were women.4 Thus, the proportion of women among MD–PhD graduates will likely continue to increase. Nevertheless, women’s representation among MD–PhD graduates remains well below their representation among all recent medical graduates, which is 49%.10
Our findings regarding race/ethnicity also merit discussion. In the earlier NIGMS study,1 81% of MSTP-supported MD–PhD graduates and 93% of non-MSTP-supported graduates were white. Racial/ethnic diversity among all MD–PhD graduates has since increased (64.5% of the graduates in our sample were white). However, like women, graduates of minority groups underrepresented in medicine remain disproportionately underrepresented among MD–PhD graduates compared to their representation among all medical school graduates.22
Thus continuing efforts are needed to promote greater physician-scientist workforce diversity.8,23 Interestingly, women, underrepresented minorities, and Asian/Pacific Islanders were all more likely to matriculate at long-standing MSTP-funded medical schools than at non-MSTP-funded medical schools (Table 2), suggesting that MSTP funding is likely important for increasing the diversity of the nation’s physician-scientist workforce.
Further considerations
Our study drew from multiple sources: a database of individualized, longitudinal data for a national cohort of all 1993–2000 U.S. LCME-accredited medical school matriculants who graduated with MD–PhD degrees as well as survey and objective data provided by the AAMC and the NBME. However, our results cannot be generalized to graduates from other degree programs or non-LCME-accredited medical schools. In addition, the proportion of graduates of long-standing MSTP-funded schools who completed the GQ items of interest was lower than that of graduates of recent MSTP-funded and non-MSTP-funded schools. Another limitation of our study was that we lacked information about the graduates’ PhD-degree fields of study, which undoubtedly covered a broad range of disciplines; their educational outcomes and career plans may have varied on the basis of their PhD disciplines.
Despite these limitations, our results can further inform the understanding of the characteristics and career plan determinants of MD–PhD graduates. Our observations of differences among MD–PhD graduates and the MSTP funding of their medical schools (including duration of that funding) suggest that future studies of MD–PhD program graduates should include consideration of their medical schools’ MSTP-funding status. Finally, the increase we have observed in the proportions of women and non-white MD–PhD graduates since the 1998 NIGMS report1 is particularly relevant to ongoing efforts to increase the diversity of our nation’s biomedical research workforce.
Acknowledgments
The authors thank Paul Jolly, PhD, Gwen Garrison, PhD, David Matthew, PhD, and Franc J. Slapar, MA, at the Association of American Medical Colleges, Washington, D.C., for provision of the data and assistance with coding; Robert M. Galbraith MD, MBA, and Ms. Jillian Ketterer at the National Board of Medical Examiners and Bert Shapiro, PhD, at the National Institutes of General Medical Sciences for assistance with data from their respective agencies; and Mr. Jim Struthers in the Division of Health Behavior Research at Washington University School of Medicine for assistance with data management.
Funding/Support: By grant R01 GM085350 from the National Institutes of General Medical Sciences (Dr. Jeffe and Dr. Andriole).
Ethical approval: The study was approved by the Institutional Review Board at Washington University School of Medicine.
Footnotes
Other disclosures: None.
Disclaimer: The conclusions of the authors are not necessarily those of the Association of American Medical Colleges, National Board of Medical Examiners, National Institutes of General Medical Sciences or their respective staff members. The funding source was not involved in the design or conduct of the study, in collection, management, analysis, or interpretation of the data, or in the preparation, review or approval of the manuscript.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Donna B. Jeffe, Division of Health Behavior Research, Department of Medicine, Washington University School of Medicine, and director of the health behavior, communication, and outreach core, Alvin J. Siteman Cancer Center, Barnes-Jewish Hospital and Washington University School of Medicine, St. Louis, Missouri..
Dorothy A. Andriole, Washington University School of Medicine, St. Louis, Missouri..
References
- 1.National Institute of General Medical Sciences . MSTP study: The careers and professional activities of graduates of the NIGMS medical scientist training program. National Institutes of Health; Bethesda, MD: [Accessed April 21, 2011]. Sep, 1998. http://publications.nigms.nih.gov/reports/mstpstudy/ [Google Scholar]
- 2.National Institute of General Medical Sciences . Medical Scientist Training Program (MSTP) institutions. National Institutes of Health; Bethesda, MD: [Accessed April 17, 2011]. http://www.nigms.nih.gov/Training/InstPredoc/PredocInst-MSTP.htm. [Google Scholar]
- 3.Barzansky B, Etzel SI. Medical schools in the United States, 2007-2008. JAMA. 2008;300(10):1221–1227. doi: 10.1001/jama.300.10.1221. [DOI] [PubMed] [Google Scholar]
- 4.Brass LF, Akabas MH, Burnley LD, et al. [Accessed April 12, 2011];Are MD–PhD programs meeting their goals?: An analysis of career choices made by graduates of 24 MD–PhD programs. Acad Med. 2010 85:692–701. doi: 10.1097/ACM.0b013e3181d3ca17. http://journals.lww.com/academicmedicine/Abstract/2010/04000/Are_MD_PhD_Programs_Meeting_Their_Goals__An.35.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Carnegie Foundation for Advancement of Teaching [Accessed April 17, 2011];Classification description. http://www.carnegiefoundation.org/classifications/index.asp?key-791.
- 6.Association of the American Medical Colleges . Graduation Questionnaire (GQ) all-school reports. Association of the American Medical Colleges; Washington, DC: [Accessed April 17, 2011]. https://www.aamc.org/data/gq/allschoolsreports/ [Google Scholar]
- 7.Andriole DA, Jeffe DB, Hageman H, et al. [Accessed April 12, 2011];Variables associated with full-time faculty appointment among contemporary U.S. medical graduates: implications for academic medicine workforce diversity. Acad Med. 2010 85:1250–1257. doi: 10.1097/ACM.0b013e3181e10159. http://journals.lww.com/academicmedicine/Abstract/2010/07000/Variables_Associated_With_Full_Time_Faculty.33.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Association of Professors of Medicine Physician-Scientist Initiative [Accessed April 17, 2011];Recommendations for revitalizing the nation’s physician-scientist workforce. http://www.im.org/PolicyAndAdvocacy/PSI/Documents/APM%20PSI%20Report.pdf.pdf.
- 9.Association of American Medical Colleges [Accessed April 17, 2011];Potential funding sources for MD–PhD students. https://www.aamc.org/students/download/62756/data/fundingformdphd.pdf.
- 10.Association of American Medical Colleges . AAMC data book: Medical schools and teaching hospitals by the numbers. Association of American Medical Colleges; Washington, DC: 2009. [Google Scholar]
- 11.Garrison G. AAMC data and MD–PhD students: 2007 MD–PhD Keystone Meeting. Association of American Medical Colleges; Washington, DC: [Accessed April 17, 2011]. 2007. https://www.aamc.org/download/103200/data/garrisonhandout.pdf. [Google Scholar]
- 12.Association of American Medical Colleges . FAQ table: Summary of MD–PhD programs and policies. Association of American Medical Colleges; [Accessed April 17, 2011]. Web Site. https://www.aamc.org/students/download/62760/data/faqtable.pdf. [Google Scholar]
- 13.Ahn J, Watt CD, Man L, Greeley SAW, Shea JA. [Accessed April 12, 2011];Educating future leaders of medical research: Analysis of student opinions and goals from the MD–PhD SAGE (Students’ Attitudes, Goals, and Education) survey. Acad Med. 2007 82(7):633–645. doi: 10.1097/ACM.0b013e318065b907. http://journals.lww.com/academicmedicine/Abstract/2007/07000/Educating_Future_Leaders_of_Medical_Research_.3.aspx. [DOI] [PubMed] [Google Scholar]
- 14.Ley TJ, Rosenberg LE. Removing career obstacles for young physician-scientists - loan-repayment programs. N Engl J Med. 2002;346(5):368–371. doi: 10.1056/NEJM200201313460515. [DOI] [PubMed] [Google Scholar]
- 15.Wiley CA. [Accessed April 12, 2011];Medical scientist training programs: A modest proposal to eliminate federal funding in favor of individual fellowships. Acad Med. 2010 85(10):1558. doi: 10.1097/ACM.0b013e3181f119ad. http://journals.lww.com/academicmedicine/Citation/2010/10000/Medical_Scientist_Training_Programs__A_Modest.9.aspx. [DOI] [PubMed] [Google Scholar]
- 16.Andersen OS, O’Banion MK. [Accessed April 12, 2011];Medical scientist training programs: Federal funding offers support and drives innovation. Acad Med. 2010 85(10):1559. doi: 10.1097/ACM.0b013e3181f1195d. http://journals.lww.com/academicmedicine/Citation/2010/10000/Medical_Scientist_Training_Programs__Federal.10.aspx. [DOI] [PubMed] [Google Scholar]
- 17.Paik JC, Howard G, Lorenz RG. Postgraduate choices of graduates from medical scientist training programs, 2004-2008. JAMA. 2009;302(12):1271–1273. doi: 10.1001/jama.2009.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muslin AJ, Kornfeld S, Polonsky KS. The physician scientist training program in internal medicine at Washington University School of Medicine. Acad Med. 2009;84:468–471. doi: 10.1097/ACM.0b013e31819a8158. [DOI] [PubMed] [Google Scholar]
- 19.Northwestern University Clinical and Translational Sciences Institute [Accessed April 17, 2011];Physician scientist training program. http://www.nucats.northwestern.edu/education-career-development/grants-awards-funded-opportunities/pstp/index.html.
- 20.University of California, San Diego – Department of Medicine [Accessed April 17, 2011];From the Chairman of the Department of Medicine: UCSD physician-scientist training pathway. http://pstp.ucsd.edu/index.shtml.
- 21.American Board of Internal Medicine [Accessed April 17, 2011];Research pathway policy & requirements. http://www.abim.org/certification/policies/research/requirements.aspx.
- 22.Andriole DA, Whelan A, Jeffe DB. Characteristics and career intentions of the emerging MD–PhD workforce. JAMA. 2008;300(10):1165–1173. doi: 10.1001/jama.300.10.1165. [DOI] [PubMed] [Google Scholar]
- 23.National Research Council of the National Academies . Assessment of NIH minority research and training programs, Phase 3. National Academies Press; Washington DC: [Accessed April 17, 2011]. 2005. http://www.nap.edu/catalog/11329.html. [PubMed] [Google Scholar]
- 24.Association of American Medical Colleges . AAMC data book statistical information related to medical education (annual editions) Association of American Medical Colleges; Washington DC: 1991-1998. [Google Scholar]
- 25.Association of American Medical Colleges . AAMC data book statistical information related to medical schools and teaching hospitals (annual editions) Association of American Medical Colleges; Washington DC: 1999-2000. [Google Scholar]
- 26.Association of American Medical Colleges . AAMC data book: medical schools and teaching hospitals by the numbers (annual editions) Association of American Medical Colleges; Washington DC: 2001-2010. [Google Scholar]