Abstract
We evaluated the average 7-year survivorship and clinical results of a newer primary posterior stabilized total knee arthroplasty (TKA). The modifications in this design included a deeper patellar sulcus aimed at reducing contact stresses, improving patellar tracking, and achieving greater maximum flexion. A consecutive group of 137 patients (171 knees) who underwent TKAs using the Optetrak PS knee prosthesis between October 1997 and March 2004 were followed for an average of 6.8 years (range 4.0–11.5 years). Preoperative range of motion (ROM) and Knee Society scores were obtained and compared to that of the patients’ most recent follow-up. Manipulation under anesthesia (MUA) and revision of the implant for any reason were considered endpoints for Kaplan–Meier survival analysis of all knees. Twenty-one knees (12.3%) underwent MUA. Three knees (1.8%) underwent revision, resulting in a 97.2% survival at a mean 10 years follow-up. Pain scores and ROM significantly improved after surgery (from preoperative average of 5.3 and 105° respectively to 44.6 and 120° postoperatively). These findings suggest that this posterior stabilized knee design is both a safe and effective option for patients undergoing primary TKA.
Keywords: total knee arthroplasty, survivorship, outcomes
Introduction
Posterior stabilized (PS) devices provide adequate stability in most patients requiring total knee arthroplasty (TKA). In 1978, the first Insall–Burstein posterior stabilized (IB PS) knee was implanted at our institution [11]. Since then, several modifications in the design have been introduced. In 1994, a newer PS TKA system (Optetrak® Posterior Stabilized Knee System, Exactech®, Inc., Gainesville, FL, USA) was developed. This system incorporated design modifications in the patellofemoral articulation aimed at addressing recurrent problems such as patellar clunk, patellar fractures, and patellofemoral pain in the IB PS lineage [1, 4, 5, 7].
Modifications in implant design have tried to maximize flexion, stability, and survival rates. In posterior stabilized implants, substitution of the posterior cruciate ligament with a spine-cam mechanism allowed for greater range of motion, fewer incidences of patellar subluxation, and more predictable kinematics compared to cruciate-retaining designs [4, 7, 13, 15]. However, differences in design account for variance in stability, rollback, and wear [3, 8, 9]. To address problems seen in the IB PS lineage, the Optetrak PS design modifications included deepening the patellar sulcus and recessing it in the femoral box, truncating the sides of the patellar flange, altering the ML and AP radii of articulation, and increasing the jump height of the femur over the tibia. Because this is a newer implant, to our knowledge, there is only one other published paper with midterm results specifically evaluating the Optetrak Posterior Stabilized total knee system [10].
The purpose of our study was to evaluate the midterm clinical results of a consecutive series of Optetrak® Posterior Stabilized (Exactech®, Inc., Gainesville, FL, USA) TKAs implanted by one surgeon at our institution using preoperative and postoperative ROM and Knee Society scores, the incidence of manipulations, revisions and arthroscopies, survivorship analysis, and radiographic data.
Materials and Methods
The senior author (GF) performed 190 Optetrak® PS TKAs in a consecutive group of 156 patients with degenerative arthritis at our institution between October 1997 and March 2004. Eligible patients underwent primary TKA with this implant during this time and had at least 4 years of follow-up. Exclusion criteria were as follows: revision TKAs, patients with instability who required greater knee constraint and underwent TKAs with a more constrained implant, and patients who failed to meet the minimum 4-year follow-up. Seven patients (seven knees) died before the minimum follow-up while 12 patients (12 knees) were lost to follow-up prior to 4 years. For those who died, their prostheses were verified as intact at the time of death.
This left 171 knees in 137 patients (94 female, 43 male) with a mean age of 67 years (range, 39–88 years) available for retrospective review. Mean follow-up was 6.8 years (range, 4.0–11.5 years). Mean preoperative ROM was 105° (range, 40–135°). Limited preoperative ROM of 90° or less was observed in 35 knees (20%). Preoperative varus deformities were present in 139 knees (81%), valgus deformities in 26 knees (15%), and neutral alignment in six knees (4%). All patients gave informed consent prior to their inclusion in the study, and this study was approved by our institutional review board.
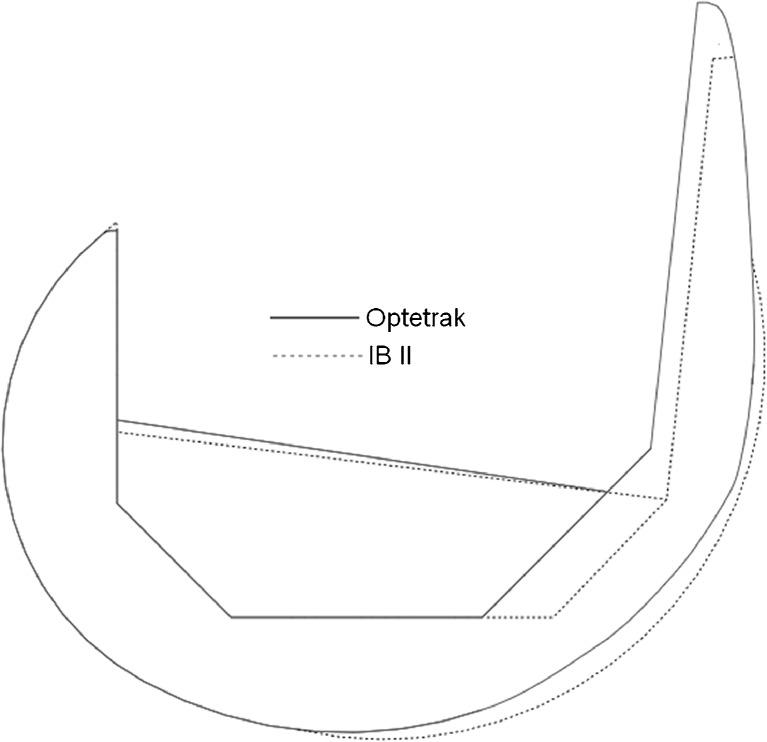
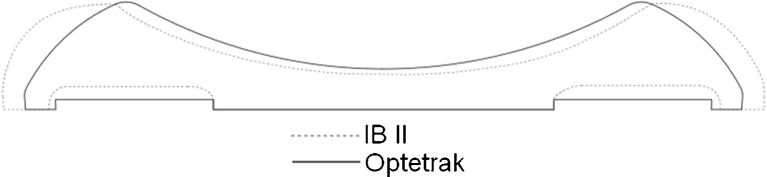
The prosthesis used in all TKAs incorporated the following design modifications: deepening of the patellar sulcus, elongating the sulcus and recessing it in the femoral box to decrease the possibility of soft tissue entrapment, and truncating the sides of the patellar flange to reduce retinacular tension [10] (Figs. 1, 2, and 3).
Fig. 1.

This is a schematic diagram of the Optetrak total knee replacement system showing the patellofemoral articulation
Fig. 2.
This is an overlay schematic diagram of the sagittal view of the Optetrak PS and IB PS II knee replacement systems, showing changes in the trochlea
Fig. 3.
This is an overlay schematic diagram of the axial view of the patellofemoral articulation, demonstrating smoother transition of the trochlea and medial and lateral retinacular region in the Optetrak PS implant compared to the IB PS II implant
The surgical approach involved a standard anterior incision and medial parapatellar arthrotomy in all patients. Alignment was achieved by intramedullary femoral alignment and extramedullary tibial alignment. For knees in varus alignment, the distal femur was cut in 5° of valgus whereas for knees in valgus alignment, it was cut in 2° of valgus. The tibial, femoral, and patellar components were fixated using hand-mixed cement.
All patients received pneumatic compression using VenaFlow and warfarin with a target INR of 2.0 as prophylactic treatment for deep venous thrombosis. All patients received patient controlled epidural regional analgesia and continuous passive range of motion postoperatively (beginning in the recovery room), as well as a standard rehabilitation protocol.
ROM and Knee Society scores were obtained preoperatively and postoperatively at all follow-ups. The scores from the preoperative and most recent follow-up appointments were compared using a Wilcoxon rank sum test. Risk of MUA and revision were compared univariately to sex using a Fisher’s exact test and to age and body mass index (BMI) using a Mann–Whitney U test. Kaplan–Meier survival analysis was used to evaluate the hazard (i.e., risk) of MUA and the survival of the implant with failure defined as revision for any reason. Cox proportional hazards models were created to evaluate the effects of age, BMI, and sex on MUA hazard and implant survival.
In addition to assessment of clinical parameters, all routine postoperative X-rays that included AP/Lat and Merchant’s views at annual follow-up appointments were analyzed.
Results
Clinical Outcomes: Range of Motion and Knee Society Scores
Preoperatively, the mean ROM was 105° (range, 40–135°), which improved to 120° (range, 75–140°) postoperatively (Table 1). The mean Knee Society pain score was 5.3 (range, 0–45) preoperatively, improving to 44.6 postoperatively (range, 10–50). The mean Knee Society function score was 45.1 (range, 20–100 points) preoperatively, improving to 73.2 (range, 0–100) postoperatively. The mean Knee Society total knee score was 39.8 (range, 13–94) preoperatively, improving to 92.8 (range, 49–100) postoperatively. All of these improvements were statistically significant (p < 0.01).
Table 1.
Preoperative and last follow-up outcome measures
| Preoperative | Last follow-up | p value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Range of motion | 104.7 | 17.2 | 119.5 | 11.7 | <0.01 |
| Knee society | |||||
| Pain | 5.3 | 7.3 | 44.6 | 9.1 | <0.01 |
| Total function | 45.1 | 12.1 | 73.2 | 22.9 | <0.01 |
| Total knee score | 39.8 | 13.7 | 92.8 | 9.6 | <0.01 |
| Total score | 86.0 | 21.3 | 166.4 | 29.3 | <0.01 |
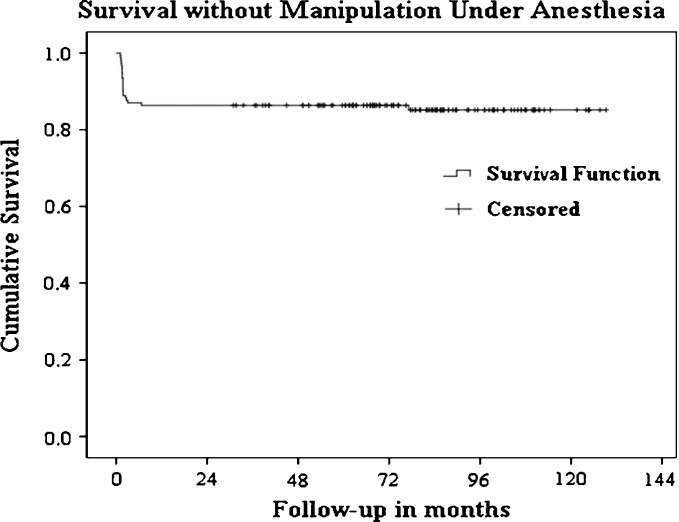
Manipulations
Twenty-one MUAs were performed (12.3%) in patients who failed to achieve 90° of flexion by 6 weeks following surgery. Males were 2.8 times more likely to have MUA (p = 0.04), but age and BMI were not associated. Kaplan–Meier survival analysis demonstrated a hazard of 11.7% (Fig. 4) for MUA within 8 months of surgery. Cox proportional hazards models are not presented since no associations were found, and the results are identical to the Kaplan–Meier with no covariates included in the models.
Fig. 4.
This graph shows a Kaplan–Meier survival curve for time until manipulation under anesthesia
The average preoperative ROM in the MUA group was 106°. Of the knees manipulated, 24% (5 out of 21) had limited preoperative ROM of 90° or less prior to the index TKR which makes this a challenging group of patients with regard to postoperative ROM. In addition, 38% (8 out of 21) of knees had preoperative conditions putting them at risk for lower postoperative ROM necessitating MUA, such as one patient with a systemic disease (rickets) and advanced varus deformity, two patients with osteonecrosis and collapse of the medial femoral condyle, and seven patients with traumatic ligament and/or meniscal injury that required surgical reconstruction. Post-traumatic arthritis with multiple prior surgeries is a diagnosis frequently associated with stiffness post-TKA [12], as prior knee surgery can negatively impact ROM following TKA [6, 16]. Additionally, 14% (3 out of 21) suffered from postoperative complications restricting flexion, including two patients with a hematoma and one patient with a wound dehiscence requiring revision wound treatment in an obese patient.
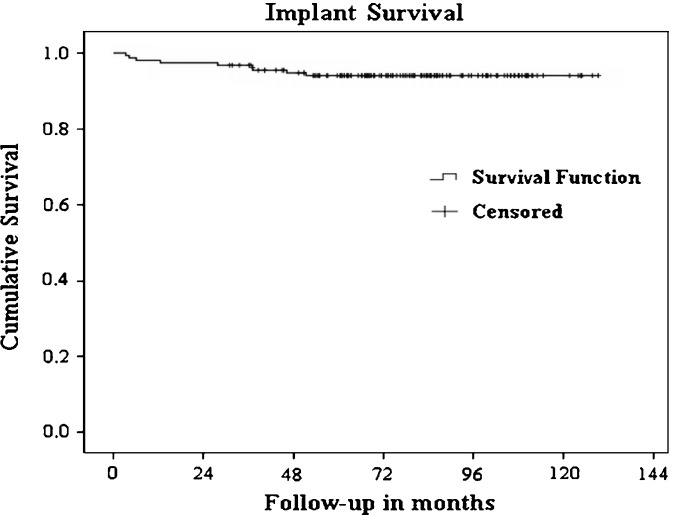
Revisions
Three of the 171 knees (1.8%) required revision surgery, two for stiffness and one for isolated aseptic patellar loosening. There were no infections in any of the revised knees, and no evidence of aseptic loosening was noted in any of the femoral or tibial components. No females underwent revision while three males were revised (p = 0.02). Age and BMI were not associated with risk of revision. Implant survival was 97.2% at 10 years (Fig. 5) with no particular patient demographics being predictive of revision.
Fig. 5.
This graph shows a Kaplan–Meier survival curve for time until revision surgery
Of the two knees revised for stiffness, both were revised after developing postoperative hematomas that led to pain and sustained loss of flexion. Both of these patients received warfarin for thromboembolic disease prophylaxis. The isolated patella revision was performed in a patient who developed patellofemoral pain 4 years postoperatively that did not respond to conservative treatment options. While there was no radiographic evidence of gross loosening, an MRI of the knee revealed early resorption around the pegs suggesting possible loosening. Intraoperatively, the patella was noted to have early loosening, was removed easily, and a new patella component was placed.
Other Complications
One patient exhibited maltracking of the patella and was treated with a lateral retinacular release. Two knees underwent arthroscopic surgery subsequent to total knee replacement. One was due to stiffness and reflex sympathetic dystrophy in a morbidly obese patient (BMI 37) and required debridement of scar tissue. In the other, arthroscopy and debridement of scar tissue of the patella region was necessitated by mild crepitus that was painful and symptomatic, but not consistent with a true patella clunk syndrome. There was no instability or loosening in either of these knees.
Radiographic Findings
At the most recent follow-up, there were no radiolucencies and no indication of femoral or tibial loosening. There was no incidence of osteolysis, patellar dislocation, patellar fracture, or avascular necrosis of the patella in our cohort of patients.
Discussion
The aim of our study was to evaluate the midterm survivorship and clinical results of a newer posterior stabilized knee implant. A limitation of our study was the loss to follow-up of potential study subjects before the minimum follow-up of 4 years. This is often an issue when retrospectively investigating midterm follow-up in an older group of patients. Another limitation was the lack of a specific patellofemoral outcome questionnaire. As previously noted, only one arthroscopy was performed for crepitus in a morbidly obese patient, but no patient was noted to have true patellar clunk syndrome.
Previous posterior stabilized knee implants exhibited complications with the patellofemoral articulation. For example, patellar clunk, patellar fractures, and patellofemoral pain were recurrent problems with the IB PS lineage [1, 4, 5, 7], limiting patient outcomes and implant survivorship.
Our postoperative ROM and Knee Society scores are comparable to those reported in literature. A study by Stern and Insall [15] in 1992 investigated the results of an older posterior stabilized implant and reported an average postoperative ROM of 110°, an average postoperative knee score of 92, and an average postoperative function score of 66 at 9–12 years of follow-up. A study on the IB-II PS knee in 2002 [4] revealed an average postoperative ROM of 116° and average postoperative total knee and function scores of 94 and 79, respectively, at an average of 7.5 years of follow-up. In 2005, the first study on the Optetrak® Posterior Stabilized Knee was conducted. Robinson [10] reviewed 66 primary TKAs utilizing this prosthesis with a minimum 5 years of follow-up, reporting an average ROM of 118° and an average postoperative function score of 78. In our study, average postoperative ROM, knee, and function scores were 120°, 92.8, and 73.2, respectively.
Therefore, our study and that of Robinson [10] reflect the greater ROM offered by the Optetrak posterior stabilized implant at midterm follow-up compared to older designs. While our knee and function scores are similar to those in previous studies, 7.0% (12 out of 171) of patients in our study had very low preoperative Knee Society Function scores (≤20), which could have limited these scores postoperatively. Our results still reflect significant improvement in function within our patient group.
Our MUA data are also similar to that of previous studies. In 1999, Larson and Lachiewicz [7] explored patellofemoral complications with the IB-II PS implant at an average of 4 years following arthroplasty and found that 13% (15 out of 118) knees were manipulated for stiffness. Although the 12.3% (21 out of 117) manipulation rate in our study does not reflect a large improvement in the incidence of MUA, 24% of manipulated knees in our study had limited preoperative ROM (≤90°), and limited preoperative ROM is the most significant predictor of limited postoperative ROM necessitating MUA. Within the same MUA group, 38% suffered from preoperative knee conditions, including trauma and multiple surgeries, that are known to increase risk of stiffness and complications postoperatively and 14% experienced postoperative knee events associated with adverse outcomes following TKA. Of the patients who received MUA, those with the lowest preoperative ROM tended to be males, which lends support to the finding that men had a 2.8 times greater chance of MUA than females.
Our revision data reflect improvements in implant survival. Stern and Insall [15] presented a 94% rate of survival at 9–12 years of follow-up and an 8% (14 out of 180) revision rate due to six tibial loosenings, three femoral loosenings, and five infections in an older posterior stabilized implant. In 2002, Sharkey et al. [14] examined 212 revision total knee arthroplasties in 203 patients and found that instability, malalignment, and component loosening accounted for half of all early revision surgeries. Indelli et al. [4] investigated the IB-II PS knee in 2002, and a 90.9% success rate was predicted at 8 years. In Robinson’s Optetrak PS knee study [10], predicted implant survival was 97% at 7.75 years, and there was one patellar fracture necessitating the only revision surgery in 66 knees.
In our study, predicted survivorship was 97.2% at 10 years, which was better than in previous studies. Our revision rate was low at 1.8% (3 out of 171). Two of these revisions were due to stiffness following hematomas, one in a patient with HIV. The third revision was due to patellar loosening in a patient with gout in the knee. Therefore, the instability, malalignment, and infection necessitating revisions in previous reports no longer hindered survivorship in our data. Although no females required revision, this was probably due to chance, as two of the three revision patients were males who had preexisting health complications (HIV and gout) that could have affected their implant survival.
Two patients in our study required arthroscopy and debridement of scar tissue following surgery. One was for stiffness and reflex sympathetic dystrophy in a morbidly obese patient and the other was for crepitus that was not true patellar clunk syndrome. Aside from the isolated patellar revision, this was the only observed patellofemoral complication, possibly representing the consequence of improvements in implant design as compared to older reports. For example, in a study on the IB-II PS implant, mild patellar clunk was found in three knees and mild crepitation was found in 17 knees [4] while a 2.5% (3 out of 118) incidence of patellar fracture was noted in another study [7]. Only one patellar fracture was found in the other Optetrak study [10], and none was found in ours.
Our radiographic findings at most recent follow-up support our data revealing no implant loosening or patellar fractures in our patient group.
The observed performance of the Optetrak Posterior Stabilized knee reflects improvements in implant design. By moving the patellar track posteriorly, smoothing the transition, and implementing earlier patellar capture (less room for soft tissue to clunk), the patellar tracking was improved. Another change made was based on the research of Bartel et al. who showed that in order to decrease polyethylene stresses, the tibial–femoral congruity had to be increased [2]. The mediolateral (ML) and anteroposterior (AP) radii of the articulation were changed to increase ML conformity between the surfaces of the tibia and femur, thereby reducing contact stress. Additionally, the modular tibial insert locking mechanism was modified in an attempt to decrease polyethylene motion [10]. The consistency of the femoral box was increased. The jump height of the femur over the tibia was also increased to offer greater resistance to posterior subluxation. Greater flexion was built into the prosthesis, increasing maximum flexion to 120°. Design changes also included more consistent kinematics compared to older implants such as the IB-II PS, in which larger implants had less allowable ROM.
Our own study compares favorably with the lineage of posterior stabilized knee systems. Our survival results (97.2% at 10 years) and midterm functional outcomes favorably compare to previous studies. However, further studies are recommended to examine long-term outcomes of this implant system.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aglietti P, Buzzi R. Posteriorly stabilized total-condylar knee replacement. J Bone Joint Surg (B). 1988;70:211–216. doi: 10.1302/0301-620X.70B2.3346290. [DOI] [PubMed] [Google Scholar]
- 2.Bartel DL, Rawlinson JJ, Burnstein AH, et al. Stresses in polyethylene components of contemporary total knee replacements. Clin Orthop. 1995;317:76. [PubMed] [Google Scholar]
- 3.Callaghan J, O’Rourke M, Goetz D, et al. Tibial post impingement in posterior stabilized total knee arthroplasty. Clin Orthop. 2002;404:83. doi: 10.1097/00003086-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Indelli P, Aglietti P, Buzzi R, Baldini A. The Insall–Burstein II prosthesis: A 5- to 9-year follow-up study in osteoarthritic knees. J Arthroplasty. 2002;17:544–549. doi: 10.1054/arth.2002.32186. [DOI] [PubMed] [Google Scholar]
- 5.Insall J, Lachiewicz P, Burstein A. The posterior stabilized condylar prosthesis: A modification of the total condylar design. J Bone Joint Surg (Am). 1982;64:1317–1323. doi: 10.2106/00004623-198264090-00006. [DOI] [PubMed] [Google Scholar]
- 6.Katz MM, Hungerford DS, Krackow KA, Lennox DW. Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1987;69:225–233. doi: 10.2106/00004623-198769020-00009. [DOI] [PubMed] [Google Scholar]
- 7.Larson C, Lachiewicz P. Patellofemoral complications with the Insall–Burstein II posterior-stabilized total knee arthroplasty. J Arthroplasty. 1999;14:288–292. doi: 10.1016/S0883-5403(99)90053-0. [DOI] [PubMed] [Google Scholar]
- 8.Puloski S, McCalden R, MacDonald S, et al. Tibial post wear in posterior stabilized total knee arthroplasty: An unrecognized source of polyethylene debris. J Bone Joint Surg (Am) 2001;83:390. doi: 10.2106/00004623-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Ritter M, Berend M, Meding J, et al. Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop. 2001;388:51. doi: 10.1097/00003086-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Robinson R. Five-year follow-up of primary Optetrak Posterior Stabilized total knee arthroplasties in osteoarthritis. J Arthroplasty. 2005;20:927–931. doi: 10.1016/j.arth.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 11.Robinson R. The early innovators of today’s resurfacing condylar knees. J Arthroplasty. 2005;20(Supplement):2–26. doi: 10.1016/j.arth.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Scott RD. Stiffness associated with total knee arthroplasty. Orthopedics. 2009;32(9):682. doi: 10.3928/01477447-20090728-30. [DOI] [PubMed] [Google Scholar]
- 13.Scuderi G, Clarke H. Cemented posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19(No 4 Suppl 1):17–21. doi: 10.1016/j.arth.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Sharkey Peter F., Hozack William J., Rothman Richard H., Shastri Shani, Jacoby Sidney M. Why Are Total Knee Arthroplasties Failing Today? Clinical Orthopaedics and Related Research. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Stern S, Insall J. Posterior stabilized prosthesis. J Bone Joint Surg (Am). 1992;74:980–986. doi: 10.2106/00004623-199274070-00004. [DOI] [PubMed] [Google Scholar]
- 16.Stiehl JB, Voorhorst PE, Keblish P, Sorrells RB. Comparison of range of motion after posterior cruciate ligament retention or sacrifice with a mobile bearing total knee arthroplasty. Am J Knee Surg. 1997;10:216–220. [PubMed] [Google Scholar]