Abstract
The primary diagnosis of femoroacetabular impingement is based on clinical symptoms, physical exam findings, and radiographic abnormalities. The study objective was to determine the radiographic findings that correlate with and are predictive of hip pain in femoroacetabular impingement (FAI). One hundred prospective patients with unilateral FAI symptoms based on clinical and radiographic findings were included in this study. All patients filled out a WOMAC pain questionnaire. Two independent-blinded surgeons assessed antero-posterior and lateral radiographs for 33 radiographic parameters of FAI. Correlations between pain scores and radiographic findings were calculated. A matched radiographic analysis was performed comparing symptomatic versus asymptomatic hips. Radiograph findings were also compared between males and females. Weak positive correlations were identified between increasing pain scores with radiographic findings of posterior wall dysplasia, presence of a shallow socket, and a more lateral acetabular fossa relative to the Ilioischial line. A symptomatic hip had a lower neck shaft angle, greater distance from Ilioischial line to acetabular fossa and larger distance from cross-over sign to superolateral point of the acetabulum when compared to the asymptomatic hip in the same patient. Symptomatic hips in males had more joint space narrowing, femoral osteophytes, higher alpha angles and larger, more incongruent femoral heads compared to females. Females had more medial acetabular fossa relative to the Ilioischial line and smaller femoral head extrusion index. Similar to other musculoskeletal conditions, radiographic findings of FAI are poor predictors of hip pain.
Keywords: femoroacetabular impingement, hip pain, hip radiographic analysis
Introduction
Femoroacetabular impingement (FAI) is now recognized as a common pathology in young adults potentially leading to osteoarthritis of the hip [2, 7, 13, 14, 18, 19, 21, 27, 29, 31]. Recently, the use of magnetic resonance imaging (MRI) in the evaluation of hip pain has grown increasingly popular [19]. MRI is useful for evaluating the extension of labral tears and particularly for cartilage wear. However, it has been shown that labral tears in up to 87% of cases coexist with radiographic findings consistent with FAI [10, 32]. It is now postulated that these radiographic abnormalities are the causal agents for labral tears and chondral damage [12]. Therefore, plain radiographs are still the first and most important imaging modality in the management and evaluation of patients with FAI [22] and are routinely used to determine the severity of the deformity, the risk of progression and the indications for surgery [1, 6].
Recently, an increased number of radiographic parameters are used to measure and describe cam and pincer pathology such as morphology of the femoral head (Table 1); however, it is unclear which of these findings are considered the most critical and useful in diagnosis of FAI and weather they are clinically relevant or have prognostic value related to hip pain. Our objective was to determine the radiographic findings that correlate with and are predictive of hip pain in FAI.
Table 1.
Radiographic measurements
| Radiographic findings | Abbreviation | Description |
|---|---|---|
| Acetabular/labral ossification | OS | 0—normal, 1—ossified, 2—fractured, 3—true os |
| Acetabular cysts | Ace-SC | 0—none, 1—small (≤2 mm), 2—large (>3 mm) |
| Acetabular fossa relative to ilioischial line | AceF-IIL | 0 is lateral, 1 is touching, 2 is medial |
| Acetabular Length | Ace-L | To Shenton’s line/teardrop in mm |
| Acetabular osteophytes | Ace-Oph | 0—none, 1—small, 2—large |
| Acetabular subchondral sclerosis | Ace-ScS | 0—no, 1—yes |
| Alpha angle | Alpha-A | In degrees |
| AP trochanter-neck offset | AP-TNO | highest of trochanter to piriformis fossa (mm) |
| Center of rotation relative to the tip trochanter | COR-GT | + is valgus, − varus (mm) |
| Congruency of femoral head | Congruency | 0 < or 1 > 2 mm of central |
| Cross-over sign | COS | 0—no, 1—yes |
| Distance from the acetabular edge to COS | Dis-COS | lateral acetabular wall (mm) |
| Femoral cysts | Fem-SC | 0—none, 1—small (≤2 mm), 2—large (>2 mm) |
| Femoral head diameter | FH-Dia | In mm |
| Femoral head extrusion index% | FH-Ex-In | Lateral uncoverage/width |
| Femoral head sphericity, AP and lateral | FH-Sph | 0—yes, 1—no |
| Femoral osteophytes | Fem-Oph | 0—none, 1—small, 2—large |
| Femoral subchondral sclerosis | Fem-ScS | 0—no, 1—yes |
| Head-neck offset, AP and lateral | AP-HNO | In mm |
| Herniation Pits, AP and lateral | HP | 0—no, 1—yes |
| Ilioischial line relative to acetabular fossa | IIL-AceF | (−) medial, (+) lateral (mm) |
| Joint space narrowing | JSN | 0—none,1— < 2 mm, 2— > 2 mm |
| Neck shaft angle | NSA | In degrees |
| Posterior wall relative to center of femoral head (CFH) | PW_CFH | Medial is minus, lateral is positive (mm) |
| Posterior wall sign | PW sign | 0—PW is lateral or through the CFH, 1—medial |
| Prominent ischial spine | PIS | 0—no, 1—yes |
| Sharp’s angle | SA | In degrees |
| Tip of PIS to ilioinguinal line | PIS-Ilio | In mm |
| Tip of PIS to pelvic brim | PIS-BRIM | In mm |
| Tonnis angle | TA | In degrees |
| Tonnis scale | TS | 0–3 |
| Trough, AP and lateral | Tro | 0—no, 1—yes |
| Wiberg’s center edge angle | CEA | In degrees |
Materials and Methods
One hundred consecutive patients with diagnosis of unilateral symptomatic FAI were included in this study following appropriate Institutional Review Board approval for a prospective study. The diagnosis was made by the senior attending surgeon based on the patients’ clinical symptoms such as groin pain, physical exam of the patient including positive impingement test and internal rotation of less than 10°, the radiographic criteria of cam and pincer lesions [3], and MRI findings of FAI, after the exclusion of the extra-articular causes of hip pain. Of the 100 patients, 44 were males and 56 were females (45 left and 55 right hips). Age range was 13–61 years, with a mean of 34.3 (±11.3) years. Body mass index (BMI) range was 16.8–39.4 with mean of 23.1 (±4.1). All patients (200 hips) had two radiographs performed for each hip including antero-posterior pelvis and cross-table lateral. The definition of symptomatic hips was based on the patients’ complains of any discomfort such as pain or stiffness. Inclusion criteria included all patients with unilateral groin pain, a positive impingement test (pain with flexion, adduction, and internal rotation of the hip [7]), internal rotation of less than 10°, and radiographic findings consistent with FAI. Exclusion criteria included prior hip surgery, bilateral hip symptoms and morbid obesity with BMI greater than 40.
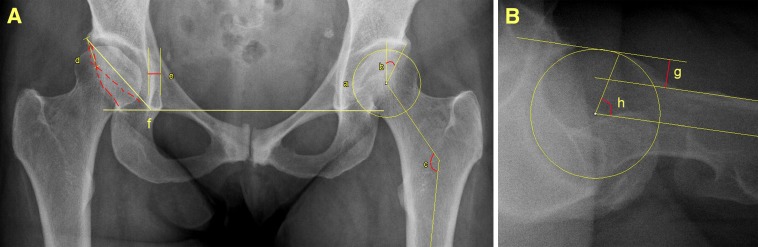
Thirty-three radiographic parameters (Fig. 1a and b) were identified and measured using digital radiograph computer software (Spectra, Linköping, Sweden). These radiographic measurements (Table 1) included the cross-over sign (COS), prominent ischial spine (PIS), posterior wall sign, neck shaft angle (NSA), head neck offset (HNO), distance from ilioischial line to acetabular fossa (IIL_AceF) [5, 8, 9, 15, 16, 21, 23, 26, 30]. Nine of these 33 measurements were considered to be associated with FAI (five for pincer and four for cam lesions). All the measurements were done by two independent surgeons (ASR, BS), whom were blinded as to which side was the symptomatic side or to any other patient identifiers. Intra-observer Cohen’s kappa was calculated. All patients also completed the Western Ontario and McMaster Universities (WOMAC) pain assessment questionnaire. WOMAC has historically been used for osteoarthritis and now recently been validated for the assessment of FAI [25].
Fig. 1.
Sample radiographic measurement of an AP (1A) pelvis and cross table lateral (1B) radiographs (a femoral head sphericity, b center edge angle, c neck shaft angle, red dotted line cross-over sign, d distance from the acetabular edge to the cross-over sign, e acetabular fossa relative to ilioischial line, f Sharp’s angle, g head-neck offset, h alpha angle)
In the first step, correlation between each of the 33 radiographic findings with WOMAC pain scores was calculated using the Pearson’s correlation test. Second, a matched radiographic analysis was performed comparing symptomatic versus asymptomatic hips using Student’s t test or chi-square. Lastly, differences in radiographic presentation of FAI in symptomatic hips were investigated for their relation to gender. All descriptive statistics (mean, SD and mean SE) and calculations (paired Student’s t test, chi-square, Fisher’s exact test and Pearson correlation) were performed with SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
Results
Diagnosis of FAI in symptomatic hips included 43 cam, 37 pincer, and 20 cases of combined lesions. The WOMAC pain score ranged from 2 to 86 with mean of 37.5 (±20.7). Ninety-five percent of n symptomatic hips had at least one element of FAI in radiographic analysis (14% cam, 23% pincer, and 58% combined). Intra-observer Cohen’s kappa was calculated to be 0.8 (range 0.67–1.00, p < 0.001). We found positive correlations between increasing pain scores with more medial posterior wall relative to center of femoral head (PW_CFH), more lateral acetabular fossa relative to the ilioischial line (AceF_IIL), and presence of posterior wall sign (Table 2).
Table 2.
Correlations for pain scores and radiographic findings in symptomatic hips
| Posterior wall relative to center of femoral head (Pearson correlation) | Acetabular fossa relative to ilioischial line (independent t test) | Posterior wall sign (independent t test) | |
|---|---|---|---|
| Pain scores | ρ = 0.023 (r = 0.226) | ρ = 0.01 | ρ = 0.02 |
Several radiographic findings were statistically different between symptomatic and asymptomatic hips. Symptomatic hips present with lower NSA, greater distance from ilioischial line to acetabular fossa and larger distance from the acetabular edge to the cross-over sign compared to the non-symptomatic side (Table 3). Regardless of these differences, none of them was a single strong predictor of pain. Several radiographic findings were significantly present bilaterally, including acetabular sclerosis (75%), joint space narrowing (78%), cyst formation (33%), alpha angle (60%), COS (70%), and PIS (79%).
Table 3.
Symptomatic vs. asymptomatic hips
| Paired t-test | Symptomatic side | Non-symptomatic side | ρ Value |
|---|---|---|---|
| Neck shaft angle (degrees) | 132.18 | 133.07 | 0.005 |
| Ilioischial-line relative to acetabular fossa (mm) | 0.23 | -0.28 | 0.022 |
| Distance from the acetabular edge to COS (mm) | 20.2 | 18.5 | 0.033 |
We found several gender differences in radiographic presentation of symptomatic hips (Table 4). Men presented more frequently with joint space narrowing, femoral osteophytes, non-spherical femoral heads on both anteroposterior and lateral images, larger femoral head diameter, higher alpha angles, and lower center of rotation relative to the tip trochanter compared to females. Femoral osteophytes and herniation pits almost predominantly occurred in male patients. In males, pain scores correlated with more medial PW_CFH and presence of posterior wall sign. Males also reported more pain than females. On the other hand, females presented with smaller Dis_Cos, lower femoral head extrusion index, with more signs of coxa profunda (more medial acetabular fossa relative to the ilioischial line) then males. In females, pain scores correlated with HNO and more lateral AceF_IIL (Table 5).
Table 4.
Radiographic differences in males versus females
| Radiographic findings | Male | Female | ρ Value |
|---|---|---|---|
| Presence of Joint space narrowing | 29% | 11% | 0.02 |
| Presence femoral osteophytes | 22% | 2% | 0.002 |
| Number of patients with non-sphericity femoral head in AP or lateral images | 25 | 16 | 0.006 |
| Femoral head diameter (mm) | 58 | 52 | <0.001 |
| Alpha angle (degree) | 88° | 68.1° | <0.001 |
| Center of rotation relative to the tip of greater trochanter (mm) | −2.0 | 0.45 | 0.046 |
| Ilioischial-line relative to acetabular fossa (mm) | 1.53 | −0.86 | 0.001 |
| Presence herniation pits in AP or lateral images | 18% | 2% | 0.01 |
| Distance from the acetabular edge to COS (mm) | 21.9 | 17.2 | 0.039 |
| Femoral head extrusion index | 0.17 | 0.14 | 0.022 |
| Acetabular length (mm) | 75.37 | 66.64 | <0.001 |
| Mean WOMAC pain scores | 31.6 | 42.3 | 0.009 |
Table 5.
Correlations with pain scores in males and females
| Males | |
| Posterior wall relative to center of femoral head (Pearson correlation) | ρ = 0.001 (r =−0.48) |
| Posterior wall sign (independent t test) | ρ = 0.03 |
| Females | |
| Head–neck offset (Pearson Correlation) | ρ = 0.012 (r =−0.33) |
| Acetabular fossa relative to ilioischial line (Independent t test) | 0.03 |
Discussion
FAI has become recognized as a common patho-anatomical process [2, 7, 13, 14, 18, 23, 28]. While numerous studies document the abnormal radiographic features associated with FAI, it is unclear which of these findings are most important and correlate with pain. There is limited data investigating any radiographic differences between symptomatic and asymptomatic hips in a same patient and any gender-specific findings. This prompted our present radiographic analysis to investigate these questions in unilateral FAI patients, compared to their asymptomatic side.
Our data showed weak correlation between pain scores and two findings of posterior wall dysplasia and a relative shallower socket (more lateral acetabular fossa relative to the ilioischial line). These are interesting findings since they are associated with dysplasia and not impingement. It has been documented that patients with symptomatic hips have radiographic findings of both impingement and dysplasia [19]. A potential explanation of this phenomenon may be due to edge loading. Interestingly, our findings suggest that patients with more coxa profunda had less pain. This is different than Reynolds et al. [24] which showed that radiographic evidence of impingement between the femoral neck and anterior acetabular edge, such as a retroverted orientation of the acetabulum, are associated with pain. Another explanation for the lack of a strong correlation is that radiographic abnormalities often do not correlate with symptom severity. This has been shown in hip and knee arthritis and spinal deformities [17, 20]. Djurasovic et al. [4] reported that in the patients who had not undergone prior surgery for spine abnormalities, clinical presentation of symptoms did not correlate with radiographic findings.
Although we found several radiographic findings of FAI that were more frequently present in symptomatic hips, all were small differences and none was a single strong predictor for pain. The distance from ilioischial line to acetabular fossa and from the acetabular edge to COS between symptomatic and non-symptomatic hips was 0.51 and 1.7 mm, respectively, which was not clinically significant. The difference in NSA between symptomatic and asymptomatic hips was small and may not seem clinically significant; however, in the setting of a matched pair, this may explain the unilateral nature of symptoms in these patients. Although radiographic findings of bilateral hips may seem similar, we found that symptomatic hips were in more relative varus. In addition, the symptomatic hips had a larger distance from the acetabular edge to the cross-over sign which is potentially indicative of more pincer pathology. Another finding in symptomatic hips was that the acetabular fossa was more lateral to the ilioischial line, which is indicative of releative shallower sockets
In our patient cohort, several radiographic findings were present bilaterally despite unilateral symptoms. These are mostly osteoarthritic finding which includes acetabular sclerosis, joint space narrowing, alpha angle, and cyst formation. Similar to our findings, Allen et al. [1] recently reported 77.8% bilateral radiographic finding of cam-type deformity in a retrospective study of 113 patients, while only 26% had bilateral hip pain. His data showed that most cam lesion although present bilaterally, have unilateral symptoms.
Lastly, we also found several differences in radiographic findings based on gender. Men exhibit more signs of cam characteristics (non-spherical femoral head with larger diameter and higher alpha angle) and females show more signs of pincer (smaller HNO, IIL_AceF and Ace_L). Our findings corroborate with prior studies about gender and FAI [2, 11, 13, 22] and confirms the conclusion made by Allen et al. [1] that men have significantly higher alpha angles than females. We found that femoral osteophytes are almost exclusively present in male patients and significantly correlate with pain, similar to the published data [17, 20]. Neogi et al. [20] demonstrated a strong correlation between presence of osteophytes and knee pain.
There are several limitations to this study which include a limited number of cases, lack of follow-up and no outcome measures. However, our major limitation was that since many of these radiographic findings were rare and subtle, this study may have been underpowered and low intra-observer reliability despite our kappa score. On the other hand, the strength of our study was the design of a prospective-matched study comparing symptomatic and asymptomatic hips with two independent observers.
In conclusion, there is a poor correlation between pain and radiographic findings of FAI. We did not find a single strong radiographic predictor of pain. There is a unique gender characteristic in FAI radiographic findings.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Institutional Review Board was obtained. Informed consent was given prior to inclusion in this study by all patients. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA).
Levels of Evidence: III
Contributor Information
Anil S. Ranawat, Phone: +1-646-7978700, FAX: +1-646-7978777, Email: ranawatanil@hss.edu.
Michael Leunig, Phone: +41-44-3857312, FAX: +41-44-3857795.
References
- 1.Allen D, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91(5):589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467(3):666–75. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Djurasovic M, Glassman SD. Correlation of radiographic and clinical findings in spinal deformities. Neurosurg Clin N Am. 2007;18:223–227. doi: 10.1016/j.nec.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88(2):372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgerald RH, Jr. Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res. 1995 (311):60–68. [PubMed]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003(417):263–269. [DOI] [PubMed]
- 9.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79(10):1489–1497. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Guevara CJ, Pietrobon R, Carothers JT, Olson SA, Vail TP. Comprehensive morphologic evaluation of the hip in patients with symptomatic labral tear. Clin Orthop Relat Res. 2006;453:277–285. doi: 10.1097/01.blo.0000246536.90371.12. [DOI] [PubMed] [Google Scholar]
- 11.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986(213):20–33. [PubMed]
- 12.Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodríguez E, Camacho-Galindo J. Arthroscopic treatment of Cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. The Journal of Arthroplasty. 2008;23(2):226–234. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 13.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83(2):171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 14.Jager M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9(3):256–263. doi: 10.1007/s00776-004-0770-y. [DOI] [PubMed] [Google Scholar]
- 15.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25(6):758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 16.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lanyon P, O’Reilly S, Jones A, et al. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis. 1998;57:595–601. doi: 10.1136/ard.57.10.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leunig M, Ganz R. Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis. Unfallchirurg. 2005;108(1):9–10. doi: 10.1007/s00113-004-0902-z. [DOI] [PubMed] [Google Scholar]
- 19.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74–80. doi: 10.1097/00003086-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Neogi T, Felson D, Niu J, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ. 2009;339:b2844. doi: 10.1136/bmj.b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 22.Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. doi: 10.1097/01.blo.0000181147.86058.74. [DOI] [PubMed] [Google Scholar]
- 23.Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 25.Rothenfluh DA, Reedwisch D, Muller U, Ganz R, Tennant A, Leunig M. Construct validity of a 12-item WOMAC for assessment of femoroacetabular impingement and osteoarthritis of the hip. Osteoarthritis Cartilage. 2008;16(9):1032–1038. doi: 10.1016/j.joca.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Shindle MK, Voos JE, Heyworth BE, Mintz DN, Moya LE, Buly RL, Kelly BT. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am. 2007;89(Suppl 3):29–43. doi: 10.2106/JBJS.G.00603. [DOI] [PubMed] [Google Scholar]
- 27.Siebenrock K. A., Kalbermatten D. F., Ganz R. Effect of Pelvic Tilt on Acetabular Retroversion: A Study of Pelves From Cadavers. Clinical Orthopaedics and Related Research. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 28.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466(2):273–280. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25(1):122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 31.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81(12):1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Wenger Doris E, Kendell Kurtis R, Miner Mark R, Trousdale Robert T. Acetabular Labral Tears Rarely Occur in the Absence of Bony Abnormalities. Clinical Orthopaedics and Related Research. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]