Abstract
Background
The majority of research on gait mechanics in knee osteoarthritis has focused on people with medial compartment involvement. As a result, little is known about the gait mechanics of people with the less common, lateral compartment disease.
Objective
The objective of this study was to compare walking mechanics—specifically, differences in frontal-plane lower-extremity kinematics and kinetics—in people with medial knee osteoarthritis, people with lateral knee osteoarthritis, and people who were healthy.
Design
A cross-sectional design was used.
Methods
Fifteen people with medial knee osteoarthritis, 15 people with lateral knee osteoarthritis, and 15 people who were healthy (control group) were recruited for the study. All participants underwent a gait analysis at an intentional walking speed. The variables of interest for the study were peak frontal-plane moments and angles and angular excursions of the lower extremity during the stance phase of gait. Data were statistically analyzed with a one-way analysis of variance.
Results
Participants with lateral knee osteoarthritis exhibited significantly less knee adduction excursion, lower peak knee abduction moment, and lower peak rear-foot eversion compared with the control group and the medial knee osteoarthritis group.
Limitations
Participants in the control group were approximately 10 years younger than participants with knee osteoarthritis. Despite this difference, neither body mass index nor gait speed, each of which is a factor with a stronger influence on gait mechanics, differed among the groups.
Conclusions
Participants with lateral knee osteoarthritis exhibited frontal-plane gait mechanics at the knee and rear foot that were different from those of participants with medial knee osteoarthritis. The results of this study may guide the development of interventions specific to treating people with lateral knee osteoarthritis.
Knee osteoarthritis (OA) is a degenerative joint disease characterized by pain and stiffness.1 These symptoms are related to disruption of the articular surfaces and are associated with significant impairment in functional ability.2 The disease prevalence increases with age, and currently 12% to 16% of people older than 65 years of age in the United States have been diagnosed with knee OA.3,4 It has been estimated that almost 45% of all people in the United States will develop knee OA during their lifetime.5 With the growing prevalence of the disease, a concomitant growth in the cost of treating the disease also has been observed. The cost for end-stage treatment of the disease has been estimated to be $38,000.6 Projections show that the cost will continue to rise as the baby boomer generation enters the age range for typical symptomatic disease presentation.
Tibiofemoral knee OA can develop in either the medial or lateral compartment.7 However, it is 9 times more common in the medial compartment.7 Static lower-extremity alignment has been shown to influence which compartment is involved, with genu valgus being associated with lateral OA and genu varus being associated with medial OA.8–11 Genu valgus alignment often is associated with hip adduction proximally and rear-foot eversion distally.12 Genu varus alignment, however, is associated with decreased hip adduction proximally and increased rear-foot inversion distally.
To date, only one study has compared the gait mechanics of people who have medial knee OA with those of people who have lateral knee OA.13 These researchers reported that, relative to people in a control group, people with medial knee OA exhibited more knee adduction but less hip adduction during gait than people with lateral knee OA.13 Alterations in hip and knee alignment are likely to lead to differences in respective joint loading. Weidow et al13 noted that people with medial knee OA had 52% higher internal knee abduction moments than people who were healthy (control group). People with lateral knee OA had 63% lower internal knee abduction moments than the control group.13 Surprisingly, lower internal peak hip abduction moments were reported in both people with medial knee OA and people with lateral knee OA than in the control group. Mundermann et al14 observed similar reductions in hip abduction moments in people with severe medial knee OA and in the control group. However, they found no difference between people with less severe medial knee OA and the control group. Alterations at the hip and knee are likely to influence mechanics distally and thus can significantly alter gait mechanics. Unfortunately, previous research studies did not include an evaluation of the differences in these distal mechanics, such as peak rear-foot eversion, eversion excursion, and the peak inversion moment.
In summary, knee OA is clearly associated with some malalignment of the lower extremity. The direction of knee malalignment (varus or valgus) influences which knee compartment becomes involved and likely influences gait mechanics. However, only one study has compared the gait mechanics of people who have been diagnosed with medial knee OA and those of people who have been diagnosed with lateral knee OA. In addition, no studies have examined the effect of these differences on rear-foot mechanics during gait. Therefore, the purpose of this study was to compare frontal-plane gait mechanics at the hip, knee, and rear foot in people with medial knee OA, people with lateral knee OA, and people who were healthy (control group). We hypothesized that, compared with people with lateral knee OA or the control group, people with medial knee OA would walk with increased peak knee adduction, increased knee adduction excursion, and an increased peak internal knee abduction moment. We also hypothesized that, compared with people with lateral knee OA or the control group, people with medial knee OA would exhibit decreased hip adduction, decreased hip adduction excursion, and a decreased peak hip abduction moment. Finally, we expected that people with lateral knee OA would exhibit increased rear-foot eversion, increased eversion excursion, and an increased peak inversion moment and that, for all variables of interest, values in the control group would fall between values in people with medial knee OA and values in people with lateral knee OA.
Method
We conducted an a priori power assessment for a one-way analysis of variance (ANOVA) design for the variables peak knee adduction and peak knee abduction moment. Using a β value of .20, an α value of .05, a difference between groups of 10%, and the variability from previously published work, we determined that 14 people per group were needed to adequately power the study.15,16 Therefore, 15 people per group were recruited through local advertisements.
Participants
All participants were 40 to 75 years of age. The participants in the control group were asymptomatic and had no history of knee problems. The participants with OA were diagnosed with unilateral medial or lateral compartment tibiofemoral OA on the basis of a flexed-knee radiograph that was graded by a single rheumatologist. People were excluded if they had any other lower-extremity arthritis. A Kellgren-Lawrence (K-L) grade was assigned to each radiograph to classify disease severity.17 A K-L grade of 2 or higher was required for inclusion in the study. In addition, all participants with OA had to report knee pain of at least 3 of 10 on a verbal analog scale during walking activities to be included in the study. Exclusion criteria included any other pathological condition that could affect ambulation. People with evidence of symptomatic, patellofemoral compartment involvement were excluded. Finally, all participants had to be able to ambulate without an assistive device.
Study Design
People who met the inclusion criteria were invited to a motion analysis laboratory for an instrumented gait analysis. Participants first provided written informed consent. Next, anatomical markers were placed over the following landmarks on the limb that was diagnosed with knee OA: the greater trochanters, the medial and lateral femoral condyles, the medial and lateral malleoli, the heads of the first and fifth metatarsals, and the distal aspect of the laboratory shoe (Nike Air Pegasus*). Tracking markers were placed on the skin over the L5–S1 interspinous space, the ipsilateral anterior superior iliac spine, and the ipsilateral iliac crest. Additionally, clusters of 4 tracking markers were placed on the distal posterior thigh and the posterior lateral shank. A cluster of 3 individual rear-foot markers were placed directly over the calcaneus and projected through holes in the heel counters of the laboratory shoe.15 Marker placement and testing were completed by 2 trained laboratory researchers using a marker set that has been shown to be reliable within and between days.18
The gait analysis was then performed. After a standing calibration, the anatomical markers were removed, leaving the tracking markers for the walking trials. Each participant's intentional walking speed was determined with photocells as the participant traversed a 25-m walkway. Intentional walking speed was defined as the speed that the participants would use to walk to and from a mailbox. Once determined, the speed was maintained within ±5% for all trials on the basis of feedback from the photocells. Data from a minimum of 5 usable trials were collected. A 6-camera motion analysis system† sampling at 120 Hz was used to capture the individual marker. Kinetic data were captured with a force platform‡ sampling at 1,080 Hz. The force platform was located at approximately the midpoint of the participant's gait path during the trials. Kinematic data were filtered with a low-pass filter at 8 Hz and a fourth-order, zero-lag Butterworth filter. Kinetic data were filtered with a low-pass filter at 50 Hz and a fourth-order, zero-lag Butterworth filter. All inverse dynamic and joint kinematic calculations (Euler sequence X-Y-Z)19 were performed with Visual 3D software.§
Outcome Measures
The kinematic variables of interest were the peak angle, angular excursion, and the peak moment in the frontal plane for the rear foot, knee, and hip. Peak angle was defined as the maximum value during the stance phase of gait. Angular excursion was defined as the peak angle during the stance phase subtracted from the initial angle at heel-strike. The kinetic variables of interest were the peak knee abduction moment, the peak inversion moment, and the peak hip abduction moment. Moment data were expressed as internal moments and were normalized to body weight (in kilograms) and height (in meters). Data for the variables of interest were extracted from 5 individual trials and then averaged.
Data Analysis
A one-way ANOVA was used to analyze group differences for the variables of interest. In the case of statistical significance, post hoc tests (Tukey honestly significant difference) were used to further analyze the data (SPSS version 14‖). The ANOVAs were performed with and without age as a covariate. Because age was not a significant covariate, only the results of the ANOVA without age as a covariate are presented to improve clarity. Corrections for multiple tests were made by use of post hoc testing with standard Bonferroni corrections for multiple comparisons. Chi-square analysis was used to examine the equality of the distribution of K-L grades between the medial knee OA and lateral knee OA groups. Statistical significance was set at a P value of <.02. To correlate our results with those of prior studies, we made an a priori plan to compare the peak hip abduction moment for participants who had medial knee OA and a K-L grade of greater than or equal to 3 with that for participants in the control group.14 Only statistical differences that were beyond the error of the measurement are reported in this article.18
Role of the Funding Source
This work was made possible by grant number NIH-RR16548 (Thomas Buchanan, primary investigator) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). The sole role of the funding source was monetary support for the completion of the study. The funding source had no role in data analysis or dissemination of the results of the study.
Results
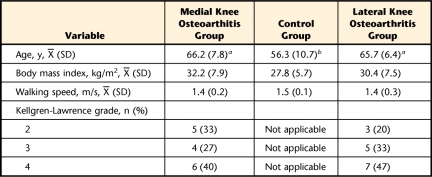
There was no difference in body mass index among the groups. However, participants in the control group were approximately 10 years younger than those in the 2 OA groups (Tab. 1). There was no difference in the proportion of disease severity between participants with medial knee OA and those with lateral knee OA (Tab. 1).
Table 1.
Descriptive Statistics for the Study Participants
a Value was significantly different from that for participants in the control group.
b Value was significantly different from that for participants with lateral knee osteoarthritis.
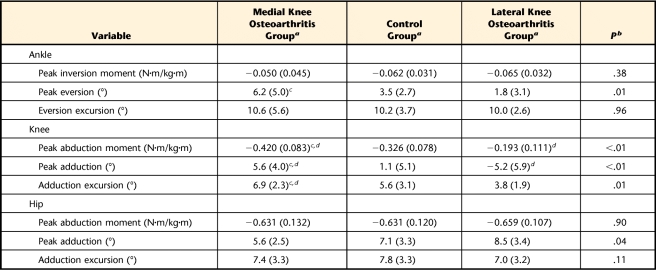
The knee abduction moments for all groups demonstrated a bimodal shape with a larger peak during the first half of the stance phase than during the second half of the stance phase. The peak abduction moment was significantly lower in participants with lateral knee OA than in participants in the control group and significantly lower in participants in the control group than in participants with medial knee OA (Tab. 2, Fig. 1). Similar results were observed for the peak knee adduction angle. The peak knee adduction angle occurred at approximately 25% of the stance phase for all groups (Tab. 2, Fig. 1). Knee adduction excursion in participants with lateral knee OA was significantly lower than that in participants with medial knee OA but was not significantly different from that in participants in the control group (Tab. 2, Fig. 1). In general, there were greater differences in knee joint kinetics and kinematics between the lateral knee OA and control groups than between the medial knee OA and control groups.
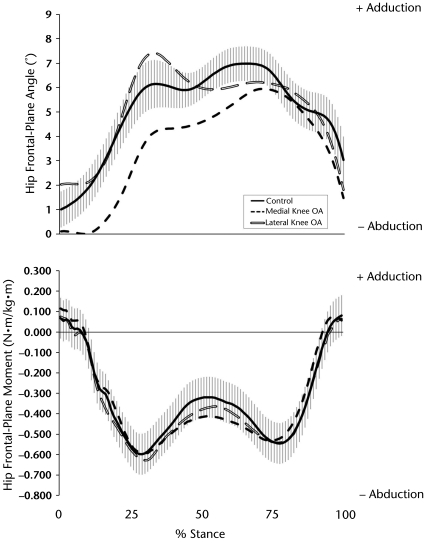
Table 2.
Variables of Interest
a Reported as mean (standard deviation).
b Reported for the one-way analysis of variance.
c Value was significantly different from that for participants with lateral knee osteoarthritis.
d Value was significantly different from that for participants in the control group.
Figure 1.
Knee frontal-plane angle and moment during the stance phase in participants with medial and lateral knee osteoarthritis (OA) and participants in the control group. Means are plotted for all groups; ±1 standard error of the mean bars are plotted for the control group only.
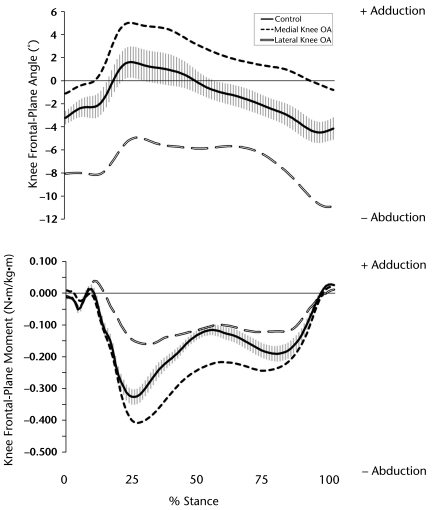
The hip kinematic patterns appeared to differ among the groups upon visual inspection (Fig. 2). Despite an offset between participants with medial knee OA and participants in the control group, their 2 patterns were quite similar; participants in the control group exhibited more hip adduction than participants with medial knee OA throughout the stance phase. However, participants with lateral knee OA demonstrated a more defined and larger peak value during the early stance phase (Tab. 2, Fig. 2). Compared with participants with lateral knee OA, participants with medial knee OA exhibited a reduction in peak hip adduction of 2.9 degrees, although this reduction was not statistically significant (Tab. 2, Fig. 2). No differences were observed in hip kinetics. All groups exhibited similar bimodal curves with no differences in peak hip abduction moments. To make comparisons with previous work examining hip abduction moments in people with more severe knee OA (K-L grade of ≥3), we performed a subset analysis. Similar to the findings for the entire group, no differences in hip abduction moments were observed among the groups when participants with more severe knee OA solely were considered.
Figure 2.
Hip frontal-plane angle and moment during the stance phase in participants with medial and lateral knee osteoarthritis (OA) and participants in the control group. Means are plotted for all groups; ±1 standard error of the mean bars are plotted for the control group only.
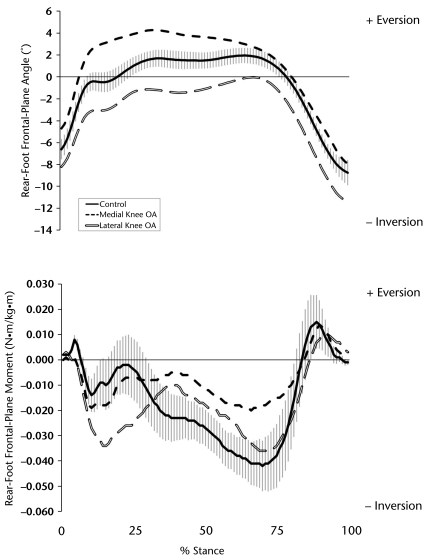
At the ankle, rear-foot eversion patterns were similar among the groups. However, there was an offset in the patterns for all groups. The joint excursions were similar; however, there were significant differences in peak eversion. Participants with lateral knee OA exhibited less peak eversion than those in the control group. Participants in the control group exhibited less peak eversion than those with medial knee OA (Tab. 2, Fig. 3). In terms of frontal-plane kinetics, participants with medial knee OA and participants in the control group exhibited similar patterns during the first 25% of the stance phase, whereas participants with lateral knee OA and those in the control group exhibited similar patterns during the final 75% of the stance phase. However, the peak rear-foot inversion moments during the first half of the stance phase were not statistically different among the groups (Tab. 2, Fig. 3).
Figure 3.
Rear-foot frontal-plane angle and moment during the stance phase in participants with medial and lateral knee osteoarthritis (OA) and participants in the control group. Means are plotted for all groups; ±1 standard error of the mean bars are plotted for the control group only.
Discussion
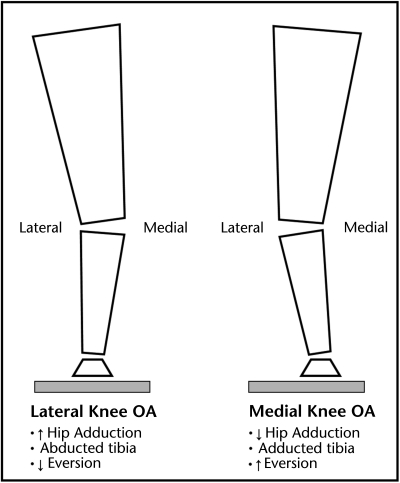
The purpose of the present study was to compare the gait mechanics of people who have medial knee OA and lateral knee OA with those of people in a control group (Fig. 4). The results suggest that people with medial knee OA exhibit gait mechanics at the knee, hip, and ankle that are different from those of people with lateral knee OA. The peak knee abduction moment, peak knee adduction, knee adduction excursion, and peak rear-foot eversion were all higher in participants with medial knee OA than in participants with lateral knee OA. Participants in the control group typically exhibited mechanics that fell between those of participants with lateral knee OA and those of participants with medial knee OA.
Figure 4.
Diagram of the posterior view of the left lower extremity in participants with lateral (left) and medial (right) knee osteoarthritis (OA). Increased rear-foot inversion is needed for the foot to be plantigrade in the participant with lateral knee osteoarthritis (left), and increased rear-foot eversion is needed in the participant with medial knee osteoarthritis (right).
The higher peak knee adduction exhibited by participants with medial knee OA than by participants with lateral knee OA was expected (Figs. 1 and 4). We believe that this result is related to the increased knee adduction associated with the genu varus alignment that is typical of medial knee OA. The difference in peak knee adduction between lateral knee OA and medial knee OA was observed previously.13 Weidow et al13 reported even larger differences (18°) in knee adduction between these groups than we reported in the present study (10.8°). However, these researchers presented the median value for each group, which may yield a larger difference than the mean value reported in the present study.13
The difference in knee adduction excursion between the groups was similar to the difference in peak knee adduction; participants with medial knee OA exhibited more excursion than participants with lateral knee OA. Our findings regarding the knee kinetics were consistent with those of others; the highest knee abduction moments were seen in participants with medial knee OA, and the lowest were seen in participants with lateral knee OA.13,14 Previous research suggested that the peak knee abduction moment is correlated with load in the medial compartment of the knee joint.20 Combined with our findings, this notion suggests that people with medial knee OA exhibit elevated loads in the medial compartment compared with people without the disease. In contrast, people with lateral knee OA likely exhibit reduced loads in the medial compartment; thus, more of the load may be distributed in the lateral compartment in these people.
Differences in rear-foot mechanics between people with medial knee OA and people with lateral knee OA have yet to be reported in the literature. However, alterations in knee mechanics are likely to lead to changes at the foot (Fig. 3). Typically, genu valgus is associated with rear-foot eversion and genu varus is associated with rear-foot inversion.12 However, we found that participants with medial knee OA exhibited more peak eversion than those with lateral knee OA. Because the overall excursions were similar in these groups, the differences in peak values were attributed to differences at the time of heel-strike. These differences remained fairly constant throughout the stance phase. The values for participants in the control group fell between those for participants in the other 2 groups (Fig. 3).
Although the findings were in contrast to our hypothesis, we believe that they indicate a compensatory mechanism of the foot to remain plantigrade. For example, because genu varus is typically associated with medial knee OA, the foot is likely positioned in increased inversion before heel-strike. Therefore, increased eversion is needed to obtain a plantigrade position. The opposite is true for genu valgus, which is associated with lateral knee OA. This conceptual model recently was supported by researchers who observed increased rear-foot eversion in people with genu varum.21 It is interesting that the offsets seen in rear-foot kinematics were not mirrored in the kinetics (Fig. 3). For example, given the increased rear-foot eversion seen in people with medial knee OA, increased inversion moments would be expected. However, people with medial knee OA, on average, exhibited the lowest inversion moments throughout most of the stance phase.
The results of the present study provide valuable information regarding conservative treatments for both medial knee OA and lateral knee OA. The differences in lower-extremity mechanics between people with medial knee OA and those with lateral knee OA support current interventions for knee OA. Treatment of knee OA can be accomplished directly with knee braces or indirectly with wedged foot orthoses.22,23 Our findings for the rear foot suggest that caution is needed in the application of medial and lateral wedging. For example, a lateral wedge is used to indirectly reduce knee adduction associated with medial knee OA.15,24,25 This reduced knee adduction is accomplished by increasing eversion of the foot. Our results suggest that people with medial knee OA already exhibit increased foot eversion as a compensatory measure for knee varus. Further eversion induced by a lateral wedge may increase the risk of foot pathologies that are associated with this motion, such as plantar fasciitis or posterior tibialis tendinitis. People with these preexisting conditions or excessive rear-foot compensation might be better served by other approaches, such as gait retraining or hip strengthening, to address abnormal frontal-plane gait mechanics at the knee.26,27 The typical goal of these types of interventions is to provide a more proximal mechanism to alter loading at the knee. Such interventions would not so aggressively alter plantar loading and thus might be more successful in improving function in people with knee OA and a history of foot-related pathology. Regardless of the intervention, the results of the present study suggest that monitoring changes at the foot should be an important component of any intervention used to alter loading at the knee.
We recognize that participants in the control group were younger than participants in either OA group by approximately 10 years. However, there is currently no evidence to suggest that this age difference would significantly influence our variables of interest. Additionally, our statistical analysis revealed that age was not a significant covariate in the present study. Two variables, body mass index and walking speed, which were controlled in our study, have been established as affecting gait mechanics.28,29 Both of these variables were similar in participants in the control group and those in the OA groups.
The findings of the present study should dovetail into current knee OA research and practice in accounting for the entire kinetic chain of the lower extremity during evaluation or treatment of a patient with medial or lateral knee OA. Because of the nature of the study, extrapolation can be made only with respect to the frontal plane. Few studies have examined sagittal-plane changes, and fewer studies have assessed the transverse plane in patients with differential compartment involvement in knee OA.13 Thus, future studies examining changes in these planes and in different compartments involved in primary knee OA would be beneficial to the rehabilitation literature. Differences between compartments are typically not of concern for surgery, with the exceptions of extreme cases, because the hardware tends to correct malalignments. However, these differences are meaningful to health care providers who aim to improve function in patients with knee OA using a conservative approach. Initial research has suggested that patients with medial knee OA and those with lateral knee OA respond differently to similar interventions aimed at offloading the compartment in which the disease is progressing.15,24,25,30 The specificity of the response suggests that the development of clinical prediction rules may help guide best practices in the conservative treatment of the disease.
In summary, people with medial knee OA and those with lateral knee OA have significantly different frontal-plane gait mechanics at the knee, hip, and ankle. These differences should be taken into account in the development of interventions designed to treat degenerative joint diseases. As health care costs and knee injury rates continue to rise, the focus on conservative treatments for knee OA will continue to increase. We hope that the results of the present study will provide foundational evidence for effective interventions to mitigate the progression of knee OA and lead to healthier and more active lifestyles for patients with knee OA.
The Bottom Line
What do we already know about this topic?
Patients with medial and lateral knee osteoarthritis exhibit different hip and knee mechanics during gait. These differences in mechanics have previously been associated with elevated disease progression.
What new information does this study offer?
The findings from this study suggest that patients with medial and lateral knee osteoarthritis also have different mechanics at the ankle. The observed differences in mechanics are contrary to current clinical beliefs. The difference in presentation may be due to the chronic effects of the disease process.
If you're a patient, what might these findings mean for you?
If you have osteoarthritis on the inside of the knee (medial knee osteoarthritis), the treatments you receive may be different from the treatments that patients with knee osteoarthritis on the outside of the knee (lateral knee osteoarthritis) may receive.
Footnotes
All authors provided concept/idea/research design and project management. Dr Butler, Dr Barrios, and Dr Davis provided writing, data collection, and data analysis. Dr Royer and Dr Davis provided fund procurement.
The authors thank Nike Inc for donating the footwear used for the laboratory experiment and New Balance Inc for donating the footwear used during the accommodation period of the study.
The protocol for this study was reviewed and approved by the Institutional Review Board of the University of Delaware.
A poster presentation of this work was given at the annual meeting of the American Society of Biomechanics; August 2004; Portland, Oregon.
This work was made possible by grant number NIH-RR16548 (Thomas Buchanan, primary investigator) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH).
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NCRR or the NIH.
Nike Inc, One Bowerman Dr, Beaverton, OR 97005.
Vicon-UK, 14 Minns Business Park, West Way, Oxford OX2 0JB, United Kingdom.
Bertec Corp, 6171 Huntley Rd, Suite J, Columbus, OH 43229.
C-Motion Inc, 20030 Century Blvd, Suite 104A, Germantown, MD 20874.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1. Kauppila AM, Kyllonen E, Mikkonen P, et al. Disability in endstage knee osteoarthritis. Disabil Rehabil. 2009;31:370–380 [DOI] [PubMed] [Google Scholar]
- 2. Brandt KD. The pathogenesis of osteoarthritis. Rheumatol Rev. 1991;1:3–11 [Google Scholar]
- 3. Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–2279 [PubMed] [Google Scholar]
- 4. Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–180 [PubMed] [Google Scholar]
- 5. Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59:1207–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Felson DT, Nevitt MC, Zhang Y, et al. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheum. 2002;46:1217–1222 [DOI] [PubMed] [Google Scholar]
- 8. Tanamas S, Hanna FS, Cicuttini FM, et al. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61:459–467 [DOI] [PubMed] [Google Scholar]
- 9. Brouwer GM, van Tol AW, Bergink AP, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204–1211 [DOI] [PubMed] [Google Scholar]
- 10. Cerejo R, Dunlop DD, Cahue S, et al. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–2636 [DOI] [PubMed] [Google Scholar]
- 11. Sharma L, Song J, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195 [DOI] [PubMed] [Google Scholar]
- 12. Gross MT. Lower quarter screening for skeletal malalignment: suggestions for orthotics and shoewear. J Orthop Sports Phys Ther. 1995;21:389–405 [DOI] [PubMed] [Google Scholar]
- 13. Weidow J, Tranberg R, Saari T, Karrholm J. Hip and knee joint rotations differ between patients with medial and lateral knee osteoarthritis: gait analysis of 30 patients and 15 controls. J Orthop Res. 2006;24:1890–1899 [DOI] [PubMed] [Google Scholar]
- 14. Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844 [DOI] [PubMed] [Google Scholar]
- 15. Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res. 2007;25:1121–1127 [DOI] [PubMed] [Google Scholar]
- 16. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- 17. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ferber R, McClay Davis I, Williams DS, III, Laughton C. A comparison of within- and between-day reliability of discrete 3D lower extremity variables in runners. J Orthop Res. 2002;20:1139–1145 [DOI] [PubMed] [Google Scholar]
- 19. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144 [DOI] [PubMed] [Google Scholar]
- 20. Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395–403 [PubMed] [Google Scholar]
- 21. Barrios JA, Davis IS, Higginson JS, Royer TD. Lower extremity walking mechanics of young individuals with asymptomatic varus knee alignment. J Orthop Res. 2009;27:1414–1419 [DOI] [PubMed] [Google Scholar]
- 22. Raja K, Dewan N. Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Am J Phys Med Rehabil. 2011;90:247–262 [DOI] [PubMed] [Google Scholar]
- 23. Pollo FE, Otis JC, Backus SI, et al. Reduction of medial compartment loads with valgus bracing of the osteoarthritic knee. Am J Sports Med. 2002;30:414–421 [DOI] [PubMed] [Google Scholar]
- 24. Kakihana W, Akai M, Yamasaki N, et al. Changes of joint moments in the gait of normal subjects wearing laterally wedged insoles. Am J Phys Med Rehabil. 2004;83:273–278 [DOI] [PubMed] [Google Scholar]
- 25. Hinman RS, Payne C, Metcalf BR, et al. Lateral wedges in knee osteoarthritis: what are their immediate clinical and biomechanical effects and can these predict a three-month clinical outcome? Arthritis Rheum. 2008;59:408–415 [DOI] [PubMed] [Google Scholar]
- 26. Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J Biomech. 2010;43:2208–2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thorp LE, Wimmer MA, Foucher KC, et al. The biomechanical effects of focused muscle training on medial knee loads in OA of the knee: a pilot, proof of concept study. J Musculoskelet Neuronal Interact. 2010;10:166–173 [PubMed] [Google Scholar]
- 28. Lai P, Leung A, Li A, Zhang M. Three-dimensional gait analysis of obese adults. Clin Biomech. 2008;23:S2–S6 [DOI] [PubMed] [Google Scholar]
- 29. Landry SC, McKean KA, Hubley-Kozey CL, et al. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech. 2007;40:1754–1761 [DOI] [PubMed] [Google Scholar]
- 30. Rodrigues PT, Ferreira AF, Pereira RM, et al. Effectiveness of medial-wedge insole treatment for valgus knee osteoarthritis. Arthritis Rheum. 2008;59:603–608 [DOI] [PubMed] [Google Scholar]