Abstract
Periventricular leukomalacia, specifically characterized as white matter injury, in neonates is strongly associated with the damage of pre-myelinating oligodendrocytes. Clinical data suggest that hypoxia-ischemia during delivery and intrauterine or neonatal infection-inflammation are important factors in the etiology of periventricular leukomalacia including cerebral palsy, a serious case exhibiting neurobehavioral deficits of periventricular leukomalacia. In order to explore the pathophysiological mechanisms of white matter injury and to better understand how infectious agents may affect the vulnerability of the immature brain to injury, novel animal models have been developed using hypoperfusion, microbes or bacterial products (lipopolysaccharide) and excitotoxins. Such efforts have developed rat models that produce predominantly white matter lesions by adopting combined hypoxia-ischemia technique on postnatal days 1-7, in which unilateral or bilateral carotid arteries of animals are occluded (ischemia) followed by 1-2 hour exposure to 6-8% oxygen environment (hypoxia). Furthermore, low doses of lipopolysaccharide that by themselves have no adverse-effects in 7-day-old rats, dramatically increase brain injury to hypoxic-ischemic challenge, implying that inflammation sensitizes the immature central nervous system. Therefore, among numerous models of periventricular leukomalacia, combination of hypoxia-ischemia-lipopolysaccharide might be one of the most-acceptable rodent models to induce extensive white matter injury and ensuing neurobehavioral deficits for the evaluation of candidate therapeutics.
Keywords: Periventricular leukomalacia, white matter injury, cerebral palsy, hypoperfusion (hypoxia-ischemia), inflammation (lipopolysaccharide), premyelinating oligodendrocytes
Cerebral palsy (CP), one of the most-devastating neural diseases, results from asphyxia during delivery as well as intrauterine infection [1]. The disease is also called periventricular leukomalacia (PVL), hypoxia-ischemia encephalopathy (HIE), white matter injury/damage (WMI/WMD), and CP in serious cases exhibiting neurobehavioral symptoms. Although asphyxia during delivery is considered an important etiological factor in many cases with PVL, the etiology might be multi-factorial. Infections and inflammation, coagulopathy and genetic background alone or in combination seem to be important [2]. Furthermore, it is well known that respiratory dysfunction is a predominant factor in pre-term infants in which a very-high incidence of CP is produced [3-6]. Motor, perceptual, visual, behavioral and/or cognitive disorders occur in the majority of cases with PVL [7-9]. For a better understanding of the underlying mechanisms of WMI, several animal models of PVL have been developed based on the hypoxia-ischemia (HI) surgery, infection or lipopolysaccharide (LPS) administration, or excitotoxin challenge. In this review, we summarized these models of PVL and analyzed the association between infection/inflammation and cerebral palsy found in human infants [10].
Neuropathology of Infantile PVL
Although infantile WMI was named PVL [11], it seems like that WMI is widespread including periventricular, subcortical and callosal white matters, and internal capsule [12-15]. Injury of white matter usually predominates, however gray matter areas, such as the cerebral cortex, thalamus and basal ganglia, are also affected directly or secondarily due to loss of white matter according to the severity [14,16]. WMI lesions are shown to be focal or diffuse [17]. The focal lesions involve necrosis of all tissue constituents, neurons or axons, astrocytes and oligodendrocytes, which may lead to cavitary lesions with surrounding proliferating astrocytes (so called astrocytosis or hypertrophic astrocytes). In comparison, the diffuse type involves a broad paucity of white matter, thinning of the corpus callosum, and often ventriculomegaly in late stages [18]. Particularly, the diffuse injury is characterized by astrogliosis, loss of oligodendroglial lineage, and impaired myelinogenesis [19]. WMI usually occurs during delivery when the white matter is non-myelinated or in the initial phase of myelination, and populated mainly by late oligodendroglial progenitors (O4+O1-), but with a small proportion of immature oligondendroglia (O4+O1+) [20]. Axons may also be lost in the lesions as demonstrated by axonal retraction balls and clubs [11,21]. Accumulation of amyloid precursor proteins (APP) [22] and axonal transections [21] are seen in the focal lesions [23]. In addition to hypertrophic (activated) astrocytes, microglia and macrophages are also constituents of WMI [14,15,22], and these cells are immunoreactive for the pro-inflammatory cytokines including tumor-necrosis factor-α (TNF-α) and interleukin-6 (IL-6) [24], suggestive of an inflammatory response. These cells may be reactivated residents of the white matter or recruited from the blood, indicating the possible participation of blood-derived inflammatory cells [25].
Etiology of Infantile PVL
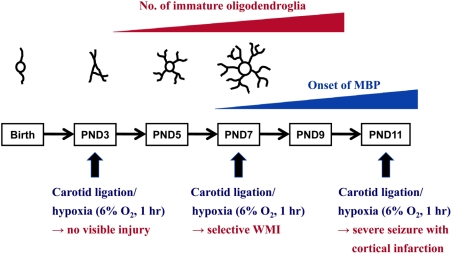
There are two major etiologies of PVL; i.e., ischemia (hypoxia)-reperfusion [26] and infection/inflammation, resulting in fetal inflammatory responses [27]. The ischemia-reperfusion process is confirmed by the presence of arterial end and border zones in the periventricular white matter [28,29], pressure-passive circulation without autoregulatory function [30], and the susceptibility of O4+O1- late oligodendroglial progenitors which are predominating oligodendroglial cells at gestational weeks 24-32 (GW24-32) or GW24-40 susceptible to oxidative stress, excitotoxicity and in vitro ischemia (Figure 1) [19,20,31-35]. On the other hand, inflammatory pathway is supported by the fact that WMI is predicted by histological chorioamnionitis and vasculitis in umbilical cord and chorion plate as well as pro-inflammatory cytokines such as IL-6 and IL-8 in amniotic fluid and fetal blood [27,36,37]. In addition, microglia/macrophages in white matter lesions exhibit immunoreactivity for IL-6 and TNF-α [24]. Premyelinating oligodendrocytes (pre-OLs), which have been shown to be a key cellular target in PVL, are in a phase of active development during GW24-40 [20,33-35]. Four developmental stages of oligodendroglial maturation include (1) oligodendroglial progenitors, (2) late oligodendroglial progenitors (O4+O1- pre-oligodendrocytes), (3) immature oligodendrocytes (O4+O1+), and (4) mature myelin-producing oligodendrocytes [myelin basic protein (MBP) positive (MBP+)]. Pre-oligodendrocytes (late oligodendroglial progenitors) and immature oligodendrocytes are referred as pre-OLs. These differentiating forms, especially the O4+O1+ immature oligodendrocytes, ensheath axons for differentiation into myelin-producing oligodendrocytes. Mature, MBP-expressing and ultimately myelin-producing oligodendrocytes are not abundant in cerebral white matter until after term. During the peak period of PVL, O4+O1- late oligodendroglial progenitors predominate in cerebral white matter and at GW28 account for 90% of the total oligodendroglial population [20]. At GW28-40, O4+O1- cells begin differentiation into O4+O1+ immature oligodendrocytes, which consists of approximately 30% of total oligodendrocyte population during the later premature period and about 50% by term. These two early differentiating cells are specifically vulnerable to injurious insults, such as ischemia and inflammation, which lead to excitotoxicity and generation of free radicals. These pre-OLs show enhanced vulnerability to the following factors: (1) reactive oxygen species (ROS) and reactive nitrogen species (RNS), because of impaired antioxidant defenses; (2) excitotoxicity due to exuberant expression of calcium-permeable glutamate receptors, and enhanced expression of the main glutamate transporter, which can become a source of injurious glutamate; and (3) cytokine injury, because of both expression of the interferon-γ (IFN-ã) receptors on the pre-OLs in the context of pronounced availability of IFN-γ in the abundant astrocytes of PVL, and sensitivity to injury by tumor-necrosis factor-α (TNF-α), which is secreted by the abundant activated microglia [38-52].
Figure 1.
Developmental stage-dependent periventricular leukomalacia of rodents induced by hypoxia-ischemia. PND, post-natal day; WMI, white matter injury.
Microglia play key roles during brain development, involving apoptosis, vascularization, axonal development, and myelination [53-56]. Thus, microglia become prominent in the forebrain at GW16-22 [57-60], reaching a peak in cerebral white matter in the third trimester [60]. It is believed that microglia be key effectors of cellular injury following ischemia and/or inflammation, since they generate ROS/RNS, secrete injurious cytokines, and enhance excitotoxicity [44-48,58,61-63]. Because microglia are abundant in normal cerebral white matter during peri-natal period, their activation leads to injury to white matter constituents including pre-OLs, and also axons and subplate neurons [60]. Not surprisingly, it was found out that many activated microglia are present diffusely in cerebral white matter in association with pre-OLs injury in PVL [39].
Animal Models of PVL
According to clinical information described above, a large number of animal models of PVL have been developed. PVL can be induced either by induction of a systemic inflammatory response through administration of bacteria or its products such as LPS [64-69], or ante- or post-natal HI surgery [68,70-73]. White matter lesions can also be induced by N-methyl-D-aspartate (NMDA) [65,74] and non-NMDA receptor [68] agonists, indicating that excitotoxicity may be involved in the development of PVL. The period prior to generalized myelinogenesis represents the developmental stage with a high vulnerability of white matter [19,65,73,75-78]. The white matter vulnerability has been related to the presence of O4+O1- pre-OLs at GW24-32 in humans [19,20,73]. The pre-OLs (O4+O1-) are susceptible to HI in immature rats, whereas O4+O1+ immature oligodendrocytes are not [73]. Oligodendrocytes immunoreactive for O4 but negative for O1 predominate in the rat white matter on post-natal days 2-4 (PND2-4) [68,73], whereas O4+O1+ cells predominate on PND7. This agrees with the suggestion in mice [65] that PND5 corresponds to GW24-30 in humans with regard to white matter maturation [77]. These studies suggest that white matter vulnerability in the rat/mouse on PND4, rather than PND7, would correspond to the white matter vulnerability in pre-term infants.
Hypoperfusion models
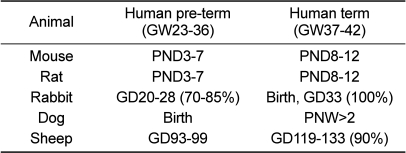
In most of the HI models of PVL, both gray and white matters are affected, except for the dog model of ischemia [79] or hemorrhagic hypotension model [71] in fetal sheep, which produced selective WMI. In general, the pattern of WMI in rabbits, cats, dogs and sheep has a distribution and morphological features closer to human pre-term brain lesions (predominantly white matter) than that in rodents (Table 1) [1]. Induction of extensive WMI is difficult in rats and mice, which may be due to the different central nervous system (CNS) anatomy of rodents that have a much lower white/gray matter ratio. However, based on the cost efficiency, availability of antibodies and transgenic animals, rodent PVL models are acceptable. Earlier, a PVL model in immature animals with unilateral carotid ligation and exposure to 8% oxygen environment for 1-3 hours was introduced [80], in which even though the vulnerability of myelinogenic zones was emphasized, most researches in this model have focused on gray matter injury. Nevertheless, it has been used successfully to study the response of immature oligodendroglial and stem/progenitor cells in white matter and periventricular zones to HI both in 9-day-old mice [81] and 7-day-old rats [73,82,83]. A corresponding model in 1-day-old rats has also been developed, which produces injury predominantly in the gray matter [84]. Recently, a modification model in rats, unilateral carotid artery ligation and 6% oxygen for 1 hour on PND7, was found to lead to selective loss of O1+ oligodendroglia and decrease of MBP in the corpus callosum and periventricular white matter 4 days later, without affecting gray matter [68]. Another study induced a loss of O4+ cells in the corpus callosum by bilateral carotid artery ligation and 10-min exposure to 8% oxygen environment [70]. In another study, permanent bilateral carotid artery ligation of PND5 or PND7 rats resulted in subcortical white and gray matter injuries [72,83]. However, because of limited survival beyond 2-3 days [83], 2-hour transient bilateral carotid ligation allowed long-term survival and still produced similar distribution of damage in subcortical regions. In comparison, permanent bilateral carotid artery ligation of 1-day-old rats allowed long-term survival longer than 2 weeks and produced WMI in corpus callosum, subcortex, internal capsule, and a significant enlargement of the ventricles [85] with limited pathology in the gray matter. Although rodent models need to be further explored, unilateral carotid artery ligation followed by exposure 8% oxygen for 2-3 hours is suitable, since various parameters to evaluate neurobehavioral deficits are obtainable, without mortality [83]. Interestingly, a model was introduced in rabbit fetuses of gestational days 21-25 (GD21-25), subjected to intrauterine hypoperfusion and WMI affecting O4+O1- pre-oligodendrocytes, were found 1-7 days after the insult [78]. Post-natal changes in magnetic resonance imaging (MRI) were found in the white matter and, moreover, severe neurological dysfunctions were demonstrated after birth approximately 10 days post-induction [86].
Table 1.
Comparative time schedule for CNS development in animals and humans [1]
PND, post-natal day; GD, gestational day; PNW, post-natal week.
Inflammation models
Extra-amniotic or intrauterine inoculation of live E. coli [67,87,88] without antibiotics induced pre-term stillbirth within 48 hours. In live pups sacrificed at 12-30 hours, brain injury was not detected [67,88]. However, antibiotic administration prevented pre-term delivery and fetal infection was delayed. Brain injury was detected in a part of pups after 2-6 days [87,88]. It is of interest to note that most fetuses with brain injury were blood culture negative, whereas there were inflammatory changes in chorioamniotic membranes. The results indicate that brain injury is related to the sustained inflammatory response rather than to passage of microbes into the brain, which is supported by the lack of massive accumulation of granulocytes in the CNS lesions [67].
Underlying mechanisms of LPS-induced PVL are not fully known. LPS is believed to activate innate immune system via interaction with toll-like receptors (TLR) on immune cells [89]. LPS binds to CD14 that facilitates activation of TLR-4, which in turn, resulting in nuclear factor-κB (NF-κB) activation and production of pro-inflammatory cytokines [89,90]. Thus, TLR-4- or CD14-deficient mice do not respond to LPS. TLR-4 receptors were found in the immature brain, and LPS administration induced an increased expression of CD14 [69]. In addition to the inflammatory response [91,92], LPS induces hypoperfusion [93], hypoglycemia [93], hyperthermia [91] and lactic acidosis, which may important factors triggering brain damage. In fact, a high dose of LPS (12 mg/kg) induced hypotension (50% decrease) as well as decrease in cerebral blood flow (CBF) in white matter, suggesting that hypoperfusion is an important contributor to injury in this region [93]. Interestingly, even a lower dose of LPS (4 mg/kg), leading to a 20-30% decrease in arterial blood pressure, was enough to induce widespread white matter lesions. Therefore, it is expected that appropriate (moderate) doses of LPS would induce hypoperfusion and injury of white matter. In young rabbits, intravenous injection of LPS (10 mg/kg) was found to decrease CBF by 25 and 43% in cerebral cortex and white matter, respectively [94]. However, brain injury was seen in the both regions, making it uncertain to what extent the decrease of CBF was the critical level for brain injury. Moreover, it was reported that WMI evolved in response to repeated doses of LPS in fetal sheep, in spite of the fact that hemodynamic effects became less pronounced, suggesting that hypoperfusion was not the critical factor [95]. Thus, it is suggested that the LPS-induced development of brain injury cannot be fully explained in terms of cerebral hypoperfusion. Especially, white or gray matter injuries in rats (PND5-7) were not successfully produced using various dose levels of LPS (0.3 mg/kg up to 100 mg/kg), in spite of a marked mRNA expression of pro-inflammatory cytokines in the white matter [66,69,96], implying that at least this form of CNS inflammation in rats was not sufficient to produce WMI. Such results indicate that LPS-induced WMI might be caused by a combination of systemic and CNS inflammatory effects.
Excitotoxic models
Intracerebral administration of excitatory amino acid (EAA) receptor agonists [NMDA and DL-α-amino-3-hydroxy-5-methyl-4-isoxalone propionic acid (AMPA)] in PND7-14 rats has been shown to induce lesions 40 times larger than in adult rats in the striatum, hippocampus and cerebral cortex [74]. Subcortical injection of ibotenate (an NMDA receptor agonist) in PND5 mice produced cortical and white matter injuries [65,97]. The topographical localization, ontogenetic window, and pharmacology of the lesions suggested that the lesions were primary, not secondary to the lesions in cerebral cortex or other gray matter areas. Indeed, microglia activation is triggered by NMDA, leading to extensive astroglial (but not oligodendroglial) death [97]. By comparison, injection of AMPA to PND7 rats caused selective WMI affecting O4+O1+ pre-oligodendroglia (expressing GluR4 receptors), which was attenuated by NBQX (an AMPA receptor antagonist), but not by dizocilpine (MK-801; an NMDA receptor antagonist) [68]. Furthermore, in pre-oligodendroglial cultures, EAA-mediated inhibition of cystine uptake led to the depletion of glutathione and susceptibility to injury evoked by oxygen free radicals [31]. In spite of partial contradiction, these studies suggest that NMDA and AMPA receptors as well as non-receptor-mediated mechanisms may be involved in WMI. Injection of high doses of excitotoxins is highly artificial and the role of excitotoxicity in WMI remains obscure, but such paradigms may be useful to explain some aspects of human disease.
Comparison of PVL models
In sheep fetuses, both LPS (100 ng) injection and asphyxia (25-min umbilical cord occlusion) caused periventricular (focal and diffuse) and subcortical (diffuse) WMI with a quite similar distribution, except for somewhat broader involvement of the gray matter (striatum and hippocampus) after umbilical cord occlusion. In both models, there were acute losses of glial fibrillary acidic protein (GFAP)-positive astroglia and cyclic nucleotide phosphohydrolase (CNPase)-positive immature oligodendroglia. In contrast, marked microglial responses were seen in both models, although microglial accumulation was more focal within the lesions induced by LPS. Furthermore, inflammatory cell infiltrations occurred much more frequently after LPS challenge, probably corresponding to macrophages/polymorphonuclear neutrophiles (PMNs) found in other models of LPS-induced WMI in cats and dogs [91,92] or after local administration of LPS into the immature brain [98]. The results suggest that PVL evoked by a systemic inflammation (inflammatory WMI) has a different morphological appearance than that produced by hypoperfusion (ischemic WMI). And comparison of the underlying mechanisms of the two lesions may be of interest as these forms of injury may have clinical relevance [26,27]. The different distribution of microglia and macrophages following the two insults may be critical, because these cells appear to have a key role in ibotenate-induced WMI [97], and because microglial toxicity depends on the density of microglia [99].
Only intraperitoneal administration of LPS to the pregnant rats or to the neonatal pups does not produce consistent brain injury [66,69]. However, LPS (0.3mg/kg), intraperitoneally given 4 hours prior to HI in 7-day-old rats (brain maturity corresponding to near term), sensitized the brain to injury; 20-min HI plus LPS injection (HIL) induced extensive lesions in all animals, whereas 20-min HI alone produced essentially minimal or no injury [69]. In contrast, administration of another endotoxin, lipoteichoic acid, 3 hours prior to HI reduced brain injury [100]. Thus, further studies are necessary to find out whether this intriguing difference can be explained by the fact that LPS and lipoteichoic acid act via different receptors [90].
The potential of infections and inflammation in brain injury is not limited to pre-term infants. The relationship between infection/inflammation and PVL including CP may be higher in term rather than in pre-term infants [101,102]. Notably, chorioamnionitis was related to serious CP with 9-fold higher risk [10], in which the levels of pro-inflammatory cytokines and chemokines were much higher [103]. Moreover, the combination of intrauterine infection and asphyxia during delivery (hard labor) appeared to confer a synergistic effect with a substantially (78-fold) higher risk of CP [104], suggesting that inflammation (or infectious products) may sensitize the fetus to additional insults.
Conclusion
Earlier, experimental researches on peri-natal brain injury have focused on hypoxic-ischemic damage to reflect the clinical problem of birth asphyxia, which has demonstrated critical clues on the pathophysiology of immature neuronal injury. However, only a small proportion of casualties suffering from PVL, especially CP, are related to asphyxia. In our recent understanding, intrauterine or peri-natal infection is emerged to be an important factor in pre-term as well as in term infants. Consequently, a number of novel animal models have been introduced in various species to demonstrate the features of WMI and explain underlying pathology in the early immature brain, either induced by hypoperfusion or infectious agents. Furthermore, recent studies have shown that bacterial endotoxin sensitize the brain to a secondary HI, supportive of the involvement of combinational factors in infantile brain injury. Conclusively, it is suggested that HIL models that consists of hypoxia-ischemia-LPS could be one of the best choices to induce extensive WMI and ensuing neurobehavioral deficits for the screening of candidate therapeutics.
Acknowledgments
This work was supported by Priority Research Centers Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009-0094035).
References
- 1.Hagberg H, Peebles D, Mallard C. Models of white matter injury: comparison of infectious, hypoxic-ischemic, and excitotoxic insults. Ment Retard Dev Disabil Res Rev. 2002;8(1):30–38. doi: 10.1002/mrdd.10007. [DOI] [PubMed] [Google Scholar]
- 2.Nelson KB, Willoughby RE. Infection, inflammation and the risk of cerebral palsy. Curr Opin Neurol. 2000;13(2):133–139. doi: 10.1097/00019052-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Deng W, Pleasure J, Pleasure D. Progress in periventricular leukomalacia. Arch Neurol. 2008;65(10):1291–1295. doi: 10.1001/archneur.65.10.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rezaie P, Dean A. Periventricular leukomalacia, inflammation and white matter lesions within the developing nervous system. Neuropathology. 2002;22(3):106–132. doi: 10.1046/j.1440-1789.2002.00438.x. [DOI] [PubMed] [Google Scholar]
- 5.Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X, Rousset CI, Hagberg H, Mallard C. Lipopolysaccharide-induced inflammation and perinatal brain injury. Semin Fetal Neonatal Med. 2006;11(5):343–353. doi: 10.1016/j.siny.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 7.de Vries LS, Eken P, Groenendaal F, van Haastert IC, Meiners LC. Correlation between the degree of periventricular leukomalacia diagnosed using cranial ultrasound and MRI later in infancy in children with cerebral palsy. Neuropediatrics. 1993;24(5):263–268. doi: 10.1055/s-2008-1071554. [DOI] [PubMed] [Google Scholar]
- 8.Krägeloh-Mann I, Petersen D, Hagberg G, Vollmer B, Hagberg B, Michaelis R. Bilateral spastic cerebral palsy-MRI pathology and origin. Analysis from a representative series of 56 cases. Dev Med Child Neurol. 1995;37(5):379–397. doi: 10.1111/j.1469-8749.1995.tb12022.x. [DOI] [PubMed] [Google Scholar]
- 9.Whitaker AH, Van Rossem R, Feldman JF, Schonfeld IS, Pinto-Martin JA, Tore C, Shaffer D, Paneth N. Psychiatric outcomes in low-birth-weight children at age 6 years: relation to neonatal cranial ultrasound abnormalities. Arch Gen Psychiatry. 1997;54(9):847–856. doi: 10.1001/archpsyc.1997.01830210091012. [DOI] [PubMed] [Google Scholar]
- 10.Grether JK, Nelson KB. Maternal infection and cerebral palsy in infants of normal birth weight. JAMA. 1997;278(3):207–211. [PubMed] [Google Scholar]
- 11.Banker BQ, Larroche JC. Periventricular leukomalacia of infancy. A form of neonatal anoxic encephalopathy. Arch Neurol. 1962;7:386–410. doi: 10.1001/archneur.1962.04210050022004. [DOI] [PubMed] [Google Scholar]
- 12.Clark DB, Anderson GW. Correlations of complications of labor with lesions in the brains of neonates. J Neuropathol Exp Neurol. 1961;20:275–278. doi: 10.1097/00005072-196104000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Leech RW, Alvord EC., Jr Morphologic variations in periventricular leukomalacia. Am J Pathol. 1974;74(3):591–602. [PMC free article] [PubMed] [Google Scholar]
- 14.Golden JA, Gilles FH, Rudelli R, Leviton A. Frequency of neuropathological abnormalities in very low birth weight infants. J Neuropathol Exp Neurol. 1997;56(5):472–478. doi: 10.1097/00005072-199705000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Gilles FH, Leviton A, Golden JA, Paneth N, Rudelli RD. Groups of histopathologic abnormalities in brains of very low birthweight infants. J Neuropathol Exp Neurol. 1998;57(11):1026–1034. doi: 10.1097/00005072-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Inder TE, Huppi PS, Warfield S, Kikinis R, Zientara GP, Barnes PD, Jolesz F, Volpe JJ. Periventricular white matter injury in the premature infant is followed by reduced cerebral cortical gray matter volume at term. Ann Neurol. 1999;46(5):755–760. doi: 10.1002/1531-8249(199911)46:5<755::aid-ana11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 17.Leviton A, Gilles F. Ventriculomegaly, delayed myelination, white matter hypoplasia, and "periventricular" leukomalacia: how are they related? Pediatr Neurol. 1996;15(2):127–136. doi: 10.1016/0887-8994(96)00157-9. [DOI] [PubMed] [Google Scholar]
- 18.Skranes JS, Nilsen G, Smevik O, Vik T, Brubakk AM. Cerebral MRI of very low birth weight children at 6 years of age compared with the findings at 1 year. Pediatr Radiol. 1998;28(6):471–475. doi: 10.1007/s002470050387. [DOI] [PubMed] [Google Scholar]
- 19.Kinney HC, Back SA. Human oligodendroglial development: relationship to periventricular leukomalacia. Semin Pediatr Neurol. 1998;5(3):180–189. doi: 10.1016/s1071-9091(98)80033-8. [DOI] [PubMed] [Google Scholar]
- 20.Back SA, Luo NL, Borenstein NS, Levine JM, Volpe JJ, Kinney HC. Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J Neurosci. 2001;21(4):1302–1312. doi: 10.1523/JNEUROSCI.21-04-01302.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marin-Padilla M. Developmental neuropathology and impact of perinatal brain damage. II: white matter lesions of the neocortex. J Neuropathol Exp Neurol. 1997;56(3):219–235. doi: 10.1097/00005072-199703000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Deguchi K, Oguchi K, Takashima S. Characteristic neuropathology of leukomalacia in extremely low birth weight infants. Pediatr Neurol. 1997;16(4):296–300. doi: 10.1016/s0887-8994(97)00041-6. [DOI] [PubMed] [Google Scholar]
- 23.Dammann O, Hagberg H, Leviton A. Is periventricular leukomalacia an axonopathy as well as an oligopathy? Pediatr Res. 2001;49(4):453–457. doi: 10.1203/00006450-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC, Chi JG. High expression of tumor necrosis factor-α and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol. 1997;177(2):406–411. doi: 10.1016/s0002-9378(97)70206-0. [DOI] [PubMed] [Google Scholar]
- 25.Dammann O, Durum S, Leviton A. Do white cells matter in white matter damage? Trends Neurosci. 2001;24(6):320–324. doi: 10.1016/s0166-2236(00)01811-7. [DOI] [PubMed] [Google Scholar]
- 26.Volpe JJ. Brain injury in the premature infant: overview of clinical aspects, neuropathology, and pathogenesis. Semin Pediatr Neurol. 1998;5(3):135–151. doi: 10.1016/s1071-9091(98)80030-2. [DOI] [PubMed] [Google Scholar]
- 27.Dammann O, Leviton A. Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res. 1997;42(1):1–8. doi: 10.1203/00006450-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Takashima S, Tanaka K. Development of cerebrovascular architecture and its relationship to periventricular leukomalacia. Arch Neurol. 1978;35(1):11–16. doi: 10.1001/archneur.1978.00500250015003. [DOI] [PubMed] [Google Scholar]
- 29.Nakamura Y, Okudera T, Hashimoto T. Vascular architecture in white matter of neonates: its relationship to periventricular leukomalacia. J Neuropathol Exp Neurol. 1994;53(6):582–589. doi: 10.1097/00005072-199411000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Pryds O. Control of cerebral circulation in the high-risk neonate. Ann Neurol. 1991;30(3):321–329. doi: 10.1002/ana.410300302. [DOI] [PubMed] [Google Scholar]
- 31.Oka A, Belliveau MJ, Rosenberg PA, Volpe JJ. Vulnerability of oligodendroglia to glutamate: pharmacology, mechanisms, and prevention. J Neurosci. 1993;13(4):1441–1453. doi: 10.1523/JNEUROSCI.13-04-01441.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fern R, Möller T. Rapid ischemic cell death in immature oligodendrocytes: a fatal glutamate release feedback loop. J Neurosci. 2000;20(1):34–42. doi: 10.1523/JNEUROSCI.20-01-00034.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rivkin MJ, Flax J, Mozell R, Osathanondh R, Volpe JJ, Villa-Komaroff L. Oligodendroglial development in human fetal cerebrum. Ann Neurol. 1995;38(1):92–101. doi: 10.1002/ana.410380116. [DOI] [PubMed] [Google Scholar]
- 34.Back SA, Volpe JJ. Cellular and molecular pathogenesis of periventricular white matter injury. Ment Retard Dev Disabil Res Rev. 1997;3(1):96–107. [Google Scholar]
- 35.Back SA, Luo NL, Borenstein NS, Volpe JJ, Kinney HC. Arrested oligodendrocyte lineage progression during human cerebral white matter development: dissociation between the timing of progenitor differentiation and myelinogenesis. J Neuropathol Exp Neurol. 2002;61(2):197–211. doi: 10.1093/jnen/61.2.197. [DOI] [PubMed] [Google Scholar]
- 36.Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC. Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol. 1996;174(5):1433–1440. doi: 10.1016/s0002-9378(96)70585-9. [DOI] [PubMed] [Google Scholar]
- 37.Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO. Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1β, and tumor necrosis factor-α), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol. 1997;177(1):19–26. doi: 10.1016/s0002-9378(97)70432-0. [DOI] [PubMed] [Google Scholar]
- 38.Khwaja O, Volpe JJ. Pathogenesis of cerebral white matter injury of prematurity. Arch Dis Child Fetal Neonatal Ed. 2008;93(2):F153–F161. doi: 10.1136/adc.2006.108837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haynes RL, Folkerth RD, Keefe RJ, Sung I, Swzeda LI, Rosenberg PA, Volpe JJ, Kinney HC. Nitrosative and oxidative injury to premyelinating oligodendrocytes in periventricular leukomalacia. J Neuropath Exp Neurol. 2003;62(5):441–450. doi: 10.1093/jnen/62.5.441. [DOI] [PubMed] [Google Scholar]
- 40.Back SA, Luo NL, Mallinson RA, O'Malley JP, Wallen LD, Frei B, Morrow JD, Petito CK, Roberts CT, Jr, Murdoch GH, Montine TJ. Selective vulnerability of preterm white matter to oxidative damage defined by F2-isoprostanes. Ann Neurol. 2005;58(1):108–120. doi: 10.1002/ana.20530. [DOI] [PubMed] [Google Scholar]
- 41.Talos DM, Follett PL, Folkerth RD, Fishman RE, Trachtenberg FL, Volpe JJ, Jensen FE. Developmental regulation of AMPA receptor subunit expression in forebrain and relationship to regional susceptibility to hypoxic/ischemic injury. II. Human cerebral white matter and cortex. J Comp Neurol. 2006;497(1):61–77. doi: 10.1002/cne.20978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Folkerth RD, Keefe RJ, Haynes RL, Trachtenberg FL, Volpe JJ, Kinney HC. Interferon-γ expression in periventricular leukomalacia in the human brain. Brain Pathol. 2004;14(3):265–274. doi: 10.1111/j.1750-3639.2004.tb00063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Folkerth RD, Haynes RL, Borenstein NS, Belliveau RA, Trachtenberg F, Rosenberg PA, Volpe JJ, Kinney HC. Developmental lag in superoxide dismutases relative to other antioxidant enzymes in premyelinated human telencephalic white matter. J Neuropathol Exp Neurol. 2004;63(9):990–999. doi: 10.1093/jnen/63.9.990. [DOI] [PubMed] [Google Scholar]
- 44.Li J, Baud O, Vartanian T, Volpe JJ, Rosenberg PA. Peroxynitrite generated by inducible nitric oxide synthase and NADPH oxidase mediates microglial toxicity to oligodendrocytes. Proc Natl Acad Sci USA. 2005;102(28):9936–9941. doi: 10.1073/pnas.0502552102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buntinx M, Moreels M, Vandenabeele F, Lambrichts I, Raus J, Seels P, Stinissen P, Ameloot M. Cytokine-induced cell death in human oligodendroglial cell lines: I. Synergistic effects of IFN-γ and TNF-α on apoptosis. J Neurosci Res. 2004;76(6):834–845. doi: 10.1002/jnr.20118. [DOI] [PubMed] [Google Scholar]
- 46.Agresti C, D'Urso D, Levi G. Reversible inhibitory effects of interferon-γ and tumour necrosis factor-α on oligodendroglial lineage cell proliferation and differentiation in vitro. Eur J Neurosci. 1996;8(6):1106–1116. doi: 10.1111/j.1460-9568.1996.tb01278.x. [DOI] [PubMed] [Google Scholar]
- 47.Andrews T, Zhang P, Bhat NR. TNFα potentiates IFNγ-induced cell death in oligodendrocyte progenitors. J Neurosci Res. 1998;54(5):574–583. doi: 10.1002/(SICI)1097-4547(19981201)54:5<574::AID-JNR2>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 48.Pang Y, Cai Z, Rhodes PG. Effect of tumor necrosis factor-á on developing optic nerve oligodendrocytes in culture. J Neurosci Res. 2005;80(2):226–234. doi: 10.1002/jnr.20450. [DOI] [PubMed] [Google Scholar]
- 49.Back SA, Gan X, Li Y, Rosenberg PA, Volpe JJ. Maturation-dependent vulnerability of oligodendrocytes to oxidative stress-induced death caused by glutathione depletion. J Neurosci. 1998;18(16):6241–6253. doi: 10.1523/JNEUROSCI.18-16-06241.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Desilva TM, Kinney HC, Borenstein NS, Trachtenberg FL, Irwin N, Volpe JJ, Rosenberg PA. The glutamate transporter EAAT2 is transiently expressed in developing human cerebral white matter. J Comp Neurol. 2007;501(6):879–890. doi: 10.1002/cne.21289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Káradóttir R, Attwell D. Neurotransmitter receptors in the life and death of oligodendrocytes. Neuroscience. 2007;145(4):1426–1438. doi: 10.1016/j.neuroscience.2006.08.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Manning SM, Talos DM, Zhou C, Selip DB, Park HK, Park CJ, Volpe JJ, Jensen FE. NMDA receptor blockade with memantine attenuates white matter injury in a rat model of periventricular leukomalacia. J Neurosci. 2008;28(26):6670–6678. doi: 10.1523/JNEUROSCI.1702-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haynes RL, Borenstein NS, Desilva TM, Folkerth RD, Liu LG, Volpe JJ, Kinney HC. Axonal development in the cerebral white matter of the human fetus and infant. J Comp Neurol. 2005;484(2):156–167. doi: 10.1002/cne.20453. [DOI] [PubMed] [Google Scholar]
- 54.Rakic S, Zecevic N. Programmed cell death in the developing human telencephalon. Eur J Neurosci. 2000;12(8):2721–2734. doi: 10.1046/j.1460-9568.2000.00153.x. [DOI] [PubMed] [Google Scholar]
- 55.Rezaie P, Male D. Differentiation, ramification and distribution of microglia within the central nervous system examined. Neuroembryology. 2002;1(1):29–43. [Google Scholar]
- 56.Hamilton SP, Rome LH. Stimulation of in vitro myelin synthesis by microglia. Glia. 1994;11(4):326–335. doi: 10.1002/glia.440110405. [DOI] [PubMed] [Google Scholar]
- 57.Rezaie P, Dean A, Male D, Ulfig N. Microglia in the cerebral wall of the human telencephalon at second trimester. Cereb Cortex. 2005;15(7):938–949. doi: 10.1093/cercor/bhh194. [DOI] [PubMed] [Google Scholar]
- 58.Rivest S. Molecular insights on the cerebral innate immune system. Brain Behav Immun. 2003;17(1):13–19. doi: 10.1016/s0889-1591(02)00055-7. [DOI] [PubMed] [Google Scholar]
- 59.Monier A, Evrard P, Gressens P, Verney C. Distribution and differentiation of microglia in the human encephalon during the first two trimesters of gestation. J Comp Neurol. 2006;499(4):565–582. doi: 10.1002/cne.21123. [DOI] [PubMed] [Google Scholar]
- 60.Billiards SS, Haynes RL, Folkerth RD, Trachtenberg FL, Liu LG, Volpe JJ, Kinney HC. Development of microglia in the cerebral white matter of the human fetus and infant. J Comp Neurol. 2006;497(2):199–208. doi: 10.1002/cne.20991. [DOI] [PubMed] [Google Scholar]
- 61.Xie Z, Wei M, Morgan TE, Fabrizio P, Han D, Finch CE, Longo VD. Peroxynitrite mediates neurotoxicity of amyloid β-peptide1-42- and lipopolysaccharide-activated microglia. J Neurosci. 2002;22(9):3484–3492. doi: 10.1523/JNEUROSCI.22-09-03484.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lehnardt S, Massillon L, Follett P, Jensen FE, Ratan R, Rosenberg PA, Volpe JJ, Vartanian T. Activation of innate immunity in the CNS triggers neurodegeneration through a Toll-like receptor 4-dependent pathway. Proc Natl Acad Sci USA. 2003;100(14):8514–8519. doi: 10.1073/pnas.1432609100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Larouche A, Roy M, Kadhim H, Tsanaclis AM, Fortin D, Sébire G. Neuronal injuries induced by perinatal hypoxic-ischemic insults are potentiated by prenatal exposure to lipopolysaccharide: animal model for perinatally acquired encephalopathy. Dev Neurosci. 2005;27(2-4):134–142. doi: 10.1159/000085985. [DOI] [PubMed] [Google Scholar]
- 64.Field NT, Newton ER, Kagan-Hallet K, Peairs WA. Perinatal effects of Gardnerella vaginalis deciduitis in the rabbit. Am J Obstet Gynecol. 1993;168(3 Pt 1):988–994. doi: 10.1016/s0002-9378(12)90858-3. [DOI] [PubMed] [Google Scholar]
- 65.Marret S, Mukendi R, Gadisseux JF, Gressens P, Evrard P. Effect of ibotenate on brain development: an excitotoxic mouse model of microgyria and posthypoxic-like lesions. J Neuropathol Exp Neurol. 1995;54(3):358–370. doi: 10.1097/00005072-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 66.Cai Z, Pan ZL, Pang Y, Evans OB, Rhodes PG. Cytokine induction in fetal rat brains and brain injury in neonatal rats after maternal lipopolysaccharide administration. Pediatr Res. 2000;47(1):64–72. doi: 10.1203/00006450-200001000-00013. [DOI] [PubMed] [Google Scholar]
- 67.Debillon T, Gras-Leguen C, Vérielle V, Winer N, Caillon J, Rozé JC, Gressens P. Intrauterine infection induces programmed cell death in rabbit periventricular white matter. Pediatr Res. 2000;47(6):736–742. doi: 10.1203/00006450-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 68.Follett PL, Rosenberg PA, Volpe JJ, Jensen FE. NBQX attenuates excitotoxic injury in developing white matter. J Neurosci. 2000;20(24):9235–9241. doi: 10.1523/JNEUROSCI.20-24-09235.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Eklind S, Mallard C, Leverin AL, Gilland E, Blomgren K, Mattsby-Baltzer I, Hagberg H. Bacterial endotoxin sensitizes the immature brain to hypoxic-ischaemic injury. Eur J Neurosci. 2001;13(6):1101–1106. doi: 10.1046/j.0953-816x.2001.01474.x. [DOI] [PubMed] [Google Scholar]
- 70.Jelinski SE, Yager JY, Juurlink BH. Preferential injury of oligodendroblasts by a short hypoxic-ischemic insult. Brain Res. 1999;815(1):150–153. doi: 10.1016/s0006-8993(98)01053-1. [DOI] [PubMed] [Google Scholar]
- 71.Matsuda T, Okuyama K, Cho K, Hoshi N, Matsumoto Y, Kobayashi Y, Fujimoto S. Induction of antenatal periventricular leukomalacia by hemorrhagic hypotension in the chronically instrumented fetal sheep. Am J Obstet Gynecol. 1999;181(3):725–730. doi: 10.1016/s0002-9378(99)70519-3. [DOI] [PubMed] [Google Scholar]
- 72.Uehara H, Yoshioka H, Kawase S, Nagai H, Ohmae T, Hasegawa K, Sawada T. A new model of white matter injury in neonatal rats with bilateral carotid artery occlusion. Brain Res. 1999;837(1-2):213–220. doi: 10.1016/s0006-8993(99)01675-3. [DOI] [PubMed] [Google Scholar]
- 73.Back SA, Han BH, Luo NL, Chricton CA, Xanthoudakis S, Tam J, Arvin KL, Holtzman DM. Selective vulnerability of late oligodendrocyte progenitors to hypoxia-ischemia. J Neurosci. 2002;22(2):455–463. doi: 10.1523/JNEUROSCI.22-02-00455.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McDonald JW, Silverstein FS, Johnston MV. Neurotoxicity of N-methyl-D-aspartate is markedly enhanced in developing rat central nervous system. Brain Res. 1988;459(1):200–203. doi: 10.1016/0006-8993(88)90306-x. [DOI] [PubMed] [Google Scholar]
- 75.Hagberg H, Bona E, Gilland E, Puka-Sundvall M. Hypoxia-ischaemia model in the 7-day-old rat: possibilities and shortcomings. Acta Paediatr Suppl. 1997;422:85–88. doi: 10.1111/j.1651-2227.1997.tb18353.x. [DOI] [PubMed] [Google Scholar]
- 76.Reddy K, Mallard C, Guan J, Marks K, Bennet L, Gunning M, Gunn A, Gluckman P, Williams C. Maturational change in the cortical response to hypoperfusion injury in the fetal sheep. Pediatr Res. 1998;43(5):674–682. doi: 10.1203/00006450-199805000-00017. [DOI] [PubMed] [Google Scholar]
- 77.Muse ED, Jurevics H, Toews AD, Matsushima GK, Morell P. Parameters related to lipid metabolism as markers of myelination in mouse brain. J Neurochem. 2001;76(1):77–86. doi: 10.1046/j.1471-4159.2001.00015.x. [DOI] [PubMed] [Google Scholar]
- 78.Tan S, Venkatasubramanian PN, Derrick M. In utero hypoxia-ischemia results in white matter injury and death of oligodendrocyte precursors in fetal rabbits. Pediatr Res. 2001;49:434A. [Google Scholar]
- 79.Yoshioka H, Goma H, Nioka S, Ochi M, Miyake H, Zaman A, Masumura M, Sawada T, Chance B. Bilateral carotid artery occlusion causes periventricular leukomalacia in neonatal dogs. Brain Res Dev Brain Res. 1994;78(2):273–278. doi: 10.1016/0165-3806(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 80.Rice JE, Vannucci RC, Brierley JB. The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol. 1981;9(2):131–141. doi: 10.1002/ana.410090206. [DOI] [PubMed] [Google Scholar]
- 81.Skoff RP, Bessert DA, Barks JD, Song D, Cerghet M, Silverstein FS. Hypoxic-ischemic injury results in acute disruption of myelin gene expression and death of oligodendroglial precursors in neonatal mice. Int J Dev Neurosci. 2001;19(2):197–208. doi: 10.1016/s0736-5748(00)00075-7. [DOI] [PubMed] [Google Scholar]
- 82.Levison SW, Rothstein RP, Romanko MJ, Snyder MJ, Meyers RL, Vannucci SJ. Hypoxia/ischemia depletes the rat perinatal subventricular zone of oligodendrocyte progenitors and neural stem cells. Dev Neurosci. 2001;23(3):234–247. doi: 10.1159/000046149. [DOI] [PubMed] [Google Scholar]
- 83.Park D, Kim TK, Choi YJ, Lee SH, Kang H, Yang YH, Bae DK, Yang G, Kim YB. Experimental models of cerebral palsy in infant rats. Lab Anim Res. 2010;26(4):345–351. [Google Scholar]
- 84.Sheldon RA, Chuai J, Ferriero DM. A rat model for hypoxic-ischemic brain damage in very premature infants. Biol Neonate. 1996;69(5):327–341. doi: 10.1159/000244327. [DOI] [PubMed] [Google Scholar]
- 85.Cai Z, Pang Y, Xiao F, Rhodes PG. Chronic ischemia preferentially causes white matter injury in the neonatal rat brain. Brain Res. 2001;898(1):126–135. doi: 10.1016/s0006-8993(01)02180-1. [DOI] [PubMed] [Google Scholar]
- 86.Derrick M, He J, Brady E. A cerebral palsy phenotype in newborn rabbits following antenatal hypoxia-ischemia to preterm fetuses. Pediatr Res. 2001;49:432A. [Google Scholar]
- 87.Yoon BH, Kim CJ, Romero R, Jun JK, Park KH, Choi ST, Chi JG. Experimentally induced intrauterine infection causes fetal brain white matter lesions in rabbits. Am J Obstet Gynecol. 1997;177(4):797–802. doi: 10.1016/s0002-9378(97)70271-0. [DOI] [PubMed] [Google Scholar]
- 88.Davies JK, Shikes RH, Sze CI, Leslie KK, McDuffie RS, Jr, Romero R, Gibbs RS. Histologic inflammation in the maternal and fetal compartments in a rabbit model of acute intra-amniotic infection. Am J Obstet Gynecol. 2000;183(5):1088–1093. doi: 10.1067/mob.2000.108888. [DOI] [PubMed] [Google Scholar]
- 89.Kopp EB, Medzhitov R. The Toll-receptor family and control of innate immunity. Curr Opin Immunol. 1999;11(1):13–18. doi: 10.1016/s0952-7915(99)80003-x. [DOI] [PubMed] [Google Scholar]
- 90.Aderem A, Ulevitch RJ. Toll-like receptors in the induction of the innate immune response. Nature. 2000;406(6797):782–787. doi: 10.1038/35021228. [DOI] [PubMed] [Google Scholar]
- 91.Gilles FH, Averill DR, Jr, Kerr CS. Neonatal endotoxin encephalopathy. Ann Neurol. 1977;2(1):49–56. doi: 10.1002/ana.410020108. [DOI] [PubMed] [Google Scholar]
- 92.Young RS, Yagel SK, Towfighi J. Systemic and neuropathologic effects of E. coli endotoxin in neonatal dogs. Pediatr Res. 1983;17(5):349–353. doi: 10.1203/00006450-198305000-00008. [DOI] [PubMed] [Google Scholar]
- 93.Young RS, Hernandez MJ, Yagel SK. Selective reduction of blood flow to white matter during hypotension in newborn dogs: a possible mechanism of periventricular leukomalacia. Ann Neurol. 1982;12(5):445–448. doi: 10.1002/ana.410120506. [DOI] [PubMed] [Google Scholar]
- 94.Ando M, Takashima S, Mito T. Endotoxin, cerebral blood flow, amino acids and brain damage in young rabbits. Brain Dev. 1988;10(6):365–370. doi: 10.1016/s0387-7604(88)80094-9. [DOI] [PubMed] [Google Scholar]
- 95.Duncan JR, Cock ML, Scheerlinck JP, Westcott KT, McLean C, Harding R, Rees SM. White matter injury after repeated endotoxin exposure in the preterm ovine fetus. Pediatr Res. 2002;52(6):941–949. doi: 10.1203/00006450-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 96.Hagberg H, Eklind S, Hallin U. Expression of cytokines and chemokines in the immature white and gray matter in response to hypoxia-ischemia or endotoxin. J Cereb Blood Flow Metab. 1999;19:S312. [Google Scholar]
- 97.Tahraoui SL, Marret S, Bodénant C, Leroux P, Dommergues MA, Evrard P, Gressens P. Central role of microglia in neonatal excitotoxic lesions of the murine periventricular white matter. Brain Pathol. 2001;11(1):56–71. doi: 10.1111/j.1750-3639.2001.tb00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lawson LJ, Perry VH. The unique characteristics of inflammatory responses in mouse brain are acquired during postnatal development. Eur J Neurosci. 1995;7(7):1584–1595. doi: 10.1111/j.1460-9568.1995.tb01154.x. [DOI] [PubMed] [Google Scholar]
- 99.Kim WG, Mohney RP, Wilson B, Jeohn GH, Liu B, Hong JS. Regional difference in susceptibility to lipopolysaccharide-induced neurotoxicity in the rat brain: role of microglia. J Neurosci. 2000;20(16):6309–6316. doi: 10.1523/JNEUROSCI.20-16-06309.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Palmer C, Roberts RL, Towfighi J. Endotoxin pretreatment protects neonatal rats from hypoxic ischemic brain injury. Pediatr Res. 2001;49:436A. [Google Scholar]
- 101.Nelson KB, Willoughby RE. Infection, inflammation and the risk of cerebral palsy. Curr Opin Neurol. 2000;13(2):133–139. doi: 10.1097/00019052-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 102.Wu YW, Colford JM., Jr Chorioamnionitis as a risk factor for cerebral palsy: A meta-analysis. JAMA. 2000;284(11):1417–1424. doi: 10.1001/jama.284.11.1417. [DOI] [PubMed] [Google Scholar]
- 103.Nelson KB, Dambrosia JM, Grether JK, Phillips TM. Neonatal cytokines and coagulation factors in children with cerebral palsy. Ann Neurol. 1998;44(4):665–675. doi: 10.1002/ana.410440413. [DOI] [PubMed] [Google Scholar]
- 104.Nelson KB, Grether JK. Potentially asphyxiating conditions and spastic cerebral palsy in infants of normal birth weight. Am J Obstet Gynecol. 1998;179(2):507–513. doi: 10.1016/s0002-9378(98)70387-4. [DOI] [PubMed] [Google Scholar]