Abstract
Life-saving medical implants like pacemakers and defibrillators face a big drawback that their batteries eventually run out and patients require frequent surgery to have these batteries replaced. With the advent of technology, alternatives can be provided for such surgeries. To power these devices, body energy harvesting techniques may be employed. Some of the power sources are patient's heartbeat, blood flow inside the vessels, movement of the body parts, and the body temperature (heat). Different types of sensors are employed, such as for sensing the energy from the heartbeat the piezoelectric and semiconducting coupled nanowires are used that convert the mechanical energy into electricity. Similarly, for sensing the blood flow energy, nanogenerators driven by ultrasonic waves are used that have the ability to directly convert the hydraulic energy in human body to electrical energy. Another consideration is to use body heat employing biothermal battery to generate electricity using multiple arrays of thermoelectric generators built into an implantable chip. These generators exploit the well-known thermocouple effect. For the biothermal device to work, it needs a 2°C temperature difference across it. But there are many parts of the body where a temperature difference of 5°C exists – typically in the few millimeters just below the skin, where it is planned to place this device. This study focuses on using body heat as an alternative energy source to recharge pacemaker batteries and other medical devices and prevent the possibility of life-risk during repeated surgery.
Keywords: Biothermal battery, pacemakers, thermoelectric generators
The two concepts of life risk and money should always remain under consideration while dealing with surgical medical appliances. Thus, for helping the people concerning such devices a new idea can be thought upon. This includes the concept of energy harvesting. Energy harvesting can be defined as the extraction of energy from one form to another useful form and these devices convert ambient energy into electrical energy. Using the concept of energy harvesting, we can run electric motor from windmill energy; hydraulic energy, etc. It is also possible to utilize the same concept in case of human body itself. There are various means to apply the above mentioned concept for helping the people with pacemakers.[1] It includes the energy harvested from the body itself. As body constitutes various kinds of energies, it may be employed as a source of energy for operating such devices. Body is having basic energies like heart beat, blood flow inside arteries and veins, body motion, and the body heat that can be harvested to have electrical energy for operating a pacemaker having requirement of voltage 6 V, in the case of a heart failure.[1,2]
In humans, it happens many times that the body parts fail to work due to some internal failures, such as in the case of heart, the natural pacemaker, sino-atrial node (SA node), can malfunction, leading to abnormal heartbeats. These arrhythmias can be very serious, causing heart attacks, and even death. To grease the wheels of patient's life, pacemaker maintains an adequate heart rate, either because the heart's native pacemaker is not fast enough, or there is a block in the heart's electrical conduction system. The heart of pacemaker circuitry is the battery. It provides the energy or power to the whole circuit of the pacemaker to operate. There are many types of batteries that can be employed to operate the system. Some examples of these are lead batteries; the estimated life of these batteries is assumed to be 8–10 years. After this time period, these batteries get ruined due to various reasons like aging, mechanical weaknesses, quality systems and quality management, change in physical characteristics (morphology) of the working chemicals, chemical loss through evaporation, etc.
So after an interval of this time period these need to be replaced. This repetitive surgery causes the discomfort and life risk too to the patient. As these artificial pacemakers are implanted in the body by employing surgical procedure and require replacement thence, we can think of some alternatives that can avoid such incidents. The body may itself be used as the source of power.[2,3] In this article, we discuss about the body as an energy source.
Body as a Source of Energy
As discussed earlier, to have an alternative source for the charging of devices like pacemaker or defibrillator with low power requirements, it may be considered to employ different body activities as the source of energy. We can carve up the power generation methods based on these above mentioned activities into two basic categories[4,5] : (i) power generation using piezoelectric element and (ii) power generation using thermocouple.
Power generation using piezoelectric element
This category employs the use of piezoelectric crystal for sensing the body energy from the sources such as the heart beat, blood flow, and the body motion. It converts these different forms of energies into electrical energy.
Principle
The basic principle is to employ piezoelectric and semiconducting coupled nanowires, such as zinc oxide, to convert mechanical energy into electricity. The piezoelectric crystals works on the principle of deformation in the crystal due to changes in the condition of the body parameters and it converts the pressure energy into electrical one. Similarly; a semiconductor nanogenerator has the potential to directly convert pressure energy in the human body, produced due to blood flow, heart beat, and contraction of blood vessels, into electric energy. At the present time, these nanogenerators are able to generate electricity in biocompatible fluid as driven by ultrasonic waves. It consists of zinc oxide (ZnO) nanowires.[4] When the system is subjected to vibrations, it converts these mechanical vibrations into the electrical signals.
The nanogenerator with nanowires embedded in the generator with size of the order of about 2 mm2. There are more than 1 million nanowires in each of these generators. An array of aligned ZnO nanowires was covered by a zigzag silicon electrode coated with platinum. The platinum is used to enhance the conductivity of the electrode. When the chemically grown wires placed on end of electrode bend in response to vibration, the ions are displaced. This unbalances the charges and creates an electric field that produces a current when the nanowire is connected to a circuit and can be used as potential source of energy.[5] These results confirm a theory that zinc oxide nanowires show a powerful piezoelectric effect, which is the production of electricity in response to mechanical pressure. If we can convert a fraction of this, we can power an electronic device. It has been calculated that we can convert 17–30% of this energy to useful energy. With the help of different studies it has been found that when one walks, 67 W of power is generated. A finger movement generates 0.1 W power and ones breathing can generate 1 W of power.[4,5] All these potential sources of power may be employed for energy generation.
Power generation using thermocouple
This category employs the use of thermocouples to sense the body heat. Thermocouple converts the heat into the potential difference that can be used to charge the battery. It is thought to develop a thermoelectric power system based on temperature differentials in the human body.[6] An innovation in thermoelectric materials (TMs) using nanoscale-based thin-film materials to convert body heat into electrical energy has been developed. The resulting power can be used to ‘trickle charge’ batteries for medium-power devices such as defibrillators, or to directly power low energy devices, such as pacemakers. These power systems have the potential to run for as long as 30 years – a fivefold increase in service life over existing technology – and thus may reduce the number of medical procedures needed for implant replacement throughout a patient's life, reducing costs and potential complications. Semiconductor materials that produce electrical energy as a result of differential temperatures between hot and cold surfaces of the material are used.[7]
Principle
A battery is supposed to turn the body's own heat into electricity. It will generate electricity using arrays of thousands of thermoelectric generators built into an implantable chip. These generators exploit the well-known thermoelectric effect in which a small voltage is generated when the junctions between two dissimilar materials are kept at different temperatures.[7]
Basic concept
The biothermal battery uses TMs made up of the semiconductor bismuth telluride. The material is doped with impurities that give one side of the thermocouple an abundance of electrons (negative or n-type), whereas the other side contains impurities lacking electrons (positive or p-type). The transfer of heat is normally from a high temperature object to a lower temperature object. Heat transfer changes the internal energy of both systems (objects). In a TM, there are free carriers which carry both electrical charge and thermal energy. If two objects maintained at different temperatures are connected by means of a TM, the molecules (free carriers) at the high temperature end will diffuse farther than the molecules at the colder end causing a net buildup of molecules (higher density) at the cold end. This density gradient causes the molecules to diffuse back to the hot end. At steady state, the density gradient counteracts the effect of the temperature gradient to minimize the net flow of molecules.[8] On the other hand, when the molecules are charged, the buildup of charge at the cold end produces a repulsive electrostatic force (and therefore an electric potential) to push the charges back to the hot end. For positive free charges, the material is called p-type and builds up positive charge on the cold end resulting in a positive potential. Similarly, for negative free charges, the material is called n-type and builds up negative charge on the cold end resulting in a negative potential [Figure 1a]. If the hot ends of the n-type and p-type material are electrically connected, and a load connected across the cold ends, the voltage produced causes the current to flow through the load, generating thermoelectrical power [Figure 1b]. Good TMs are typically heavily doped semiconductors. Also, a single type of carrier ensures optimization of thermoelectric power generation. Mixed n-type and p-type conduction also leads to an adverse effect and low thermopower.[9]
Figure 1.
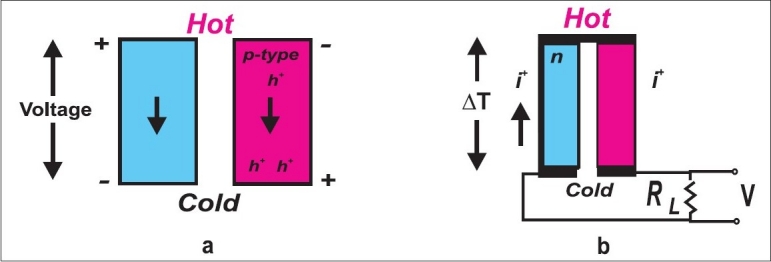
Schematic representation of generation of (a) positive/negative charges due to difference in temperature and (b) positive/negative potentials generated due to difference in temperature[6]
Observations
To obtain a useful voltage it is necessary to arrange thousands of semiconductor units in series. The device has about 4000 thermocouples in series, each generating a few microvolts for each 1°C of temperature difference. A typical battery has an array of 2.5 cm2, a total of about 6.0 cm2surface areas from all sides, which generates 4 V and delivers a power of 100 μW. The device aims to extend implantable cardioverter-defibrillator (ICD) and pacemaker battery life expectancy to more than three decades by continuously trickle charging them.[10] It might even be able to power some low power pacemakers directly. For the biothermal device [Figure 2] to work, it needs a 2°C temperature difference across it. This temperature difference can be easily obtained by placing the device a few millimeters below the surface of skin; as there are many parts of the body where a temperature difference of as much as 5°C exists.[10,11]
Figure 2.
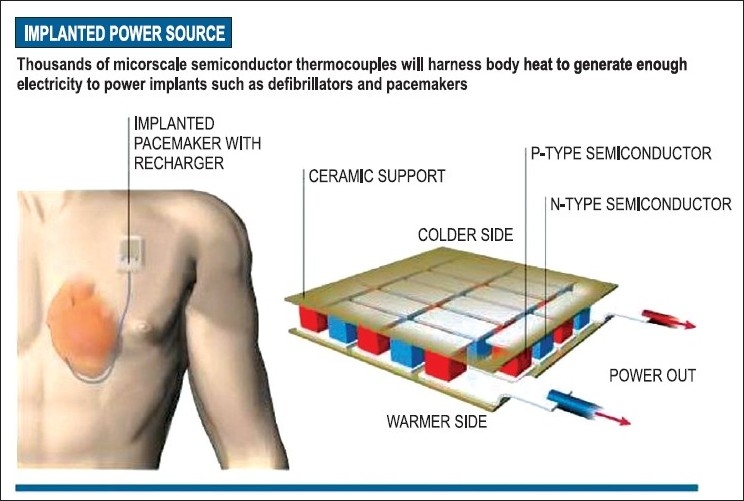
Biothermal battery: P-N junction array[2]
Technical challenge and technology competitors
The challenge is to create a thermoelectric module for 100 μW power at 3 V with 1°C temperature difference. The thermoelectric module requires approximately 4000 elements on a 6-cm2 surface.
There are different technological competitors which are available in the market. The lithium ion battery technology provides rechargability and extended battery life. Also, lithium/carbon monofluoride battery technology has been developed in mid-90s, though has not been widely used. Nanocrystalline cathode components have been developed that extend the battery life of lithium. None of these competitors currently offer the potential to provide service life of around 30 years.[12]
Basic charging circuit
Figure 3 shows the circuit which uses the principle of biothermal battery charging the pacemaker device. In this circuit, the voltage level of the battery is monitored. It automatically cuts off the charging process when its output terminal voltage increases above the predetermined voltage level. Timer IC NE555 is used to charge and monitor the voltage level in the battery. Control voltage pin 5 of IC1 is provided with a reference voltage of 5.6 V by zener diode ZD1. Threshold pin 6 is supplied with a voltage set by VR1 and trigger pin 2 is supplied with a voltage set by VR2. When the discharged battery is connected to the circuit, the voltage given to trigger pin 2 of IC1 is below 1/3 Vcc and hence the flip-flop in the IC is switched on to take output pin 3 high. When the battery is fully charged, the output terminal voltage increases the voltage at pin 2 of IC1 above the trigger point threshold. This switches off the flip-flop and the output goes low to terminate the charging process. Threshold pin 6 of IC1 is referenced at 2/3 Vcc set by VR1. T1 transistor is employed for enhancing charging current in the circuit. Resistor R3 is critical for providing the required charging current. For a 39-Ω resistor, the charging current is approximately 180 mA.[11,12] This circuit receives the power from the array of semiconductor thermocouple mounted on a chip. These thermocouples (based on chip) are attached with the body at two points considering one as cold and other one as hot. These points can be found by taking one at the surface of body and other at approximately 3 in. below the skin so that appropriate temperature difference can be achieved to generate the required potential difference to charge the battery of the pacemaker.
Figure 3.
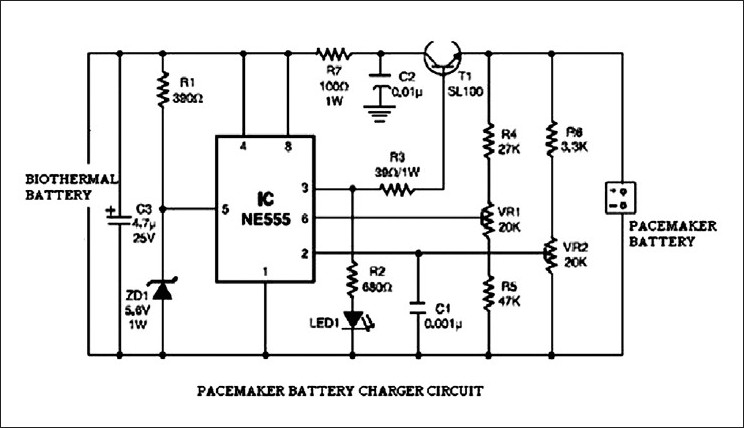
Charger circuit[9]
Battery charger algorithm
The Battery Charger implements a three-stage charging algorithm. [Figure 4] The charging process starts from Precharge Stage; then, when the battery voltage reaches a certain point, it switches to the Bulk Charge Stage. Next, the charging process is finalized in the Absorption (Constant Voltage) Stage. The charger can then maintain the battery charge in Float Stage. When the charger is disconnected from the power line, it automatically switches off within 1 min by default. This protects the battery from being discharged by the charger electronics.[11,12]
Figure 4.
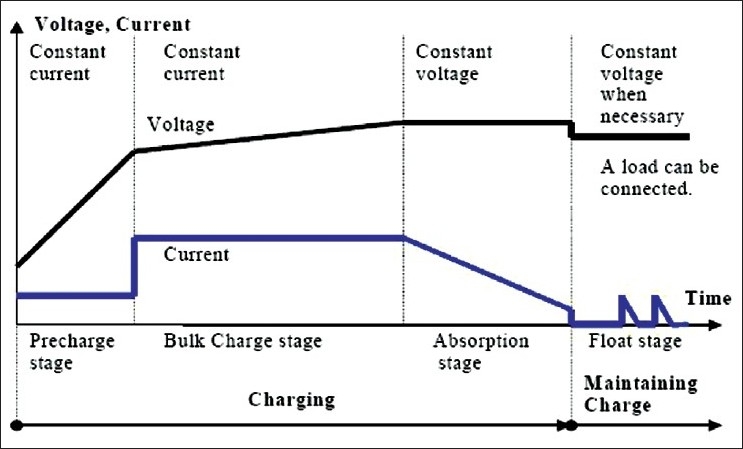
Three-stage charging algorithm[11]
Conclusion
Human power is a low-density form of renewable energy that has large-scale generation potential due to its abundant availability. Due to high costs associated with purchasing the technology required to recover small amounts of recreationally spent human energy, applications are limited by economic feasibility. Refinement and development of recovery technology could result in improved effectiveness and reduced capital costs, thereby decreasing limitations caused by economic feasibility. Rising electricity costs could also make recovery more feasible by decreasing the capital cost payback periods of recovery technology.[13]
With the advent of nanotechnology revolution, the ability to put thousands of these small semiconductor nodes that convert heat to electricity in the small space, similar to the size of one or two postage stamps, has become feasible. Scientists believe that battery can be implanted in the skin, where temperature differences of up to 5°C exist. This device may then be employed to power pacemakers as well as other devices, such as the tiny neurotransmitters that are implanted in the brain for treatment of Parkinson's disease.[13,14] Hence, it would be possible to replace the existing toxic batteries with natural and safe charging devices which may not require replacement at all, and hence surgical procedures, thereby enhancing patient safety by minimizing the risk involved.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Crespi AM, Somdahl SK, Schmidt CL, Skarstad PM. Evolution of power sources for implantable cardioverter defibrillators. J Power Sources. 2001;96:33–8. [Google Scholar]
- 2.Graham-Rowe D. Can implants run on body heat? New Scientist. [last cited in 2004 June]. Available from: http://www.newscientist.com/
- 3.Bullis K. Free Electricity from Nano Generators throw away your batteries. [last cited in 2010 Jan 5]. Available from: http://www.technologyreview.com .
- 4.Wong, George SK. (Gloucester, CA,US),Body heat power generator. [last cited in 2010 Jan 5]. Available from: http://www.freepatentsonline.com/6075199.html .
- 5.Ashok Kumar Biosensors Based on Piezoelectric Crystal Detectors: Theory and Application. [last cited in 2010 Jan 5]. Available from: http://www.tms.org/pubs/journals/JOM/0010/Kumar/Kumar-0010.html .
- 6.Snyder GJ, Ursell TS. Thermoelectric efficiency and compatibility. Phys Rev Lett. 2003;91:148301. doi: 10.1103/PhysRevLett.91.148301. [DOI] [PubMed] [Google Scholar]
- 7.Holmes CF, Brown WR. NY: The Electrochemical Society; 1980. Power sources for biomedical implantable applications and ambient temperature lithium batteries, “Effects of anode precoating on the characteristics of the lithium/Iodine pacemaker battery” Pennington; pp. 187–84. [Google Scholar]
- 8.Researchers at the Fraunhofer Institute for Integrated Circuits in Erlangen. [last cited in 2004 Aug 19]. Available from: http://www.iis.fraunhofer.de/fhg/
- 9.Wang ZL. Working on thermocouple. [last cited in 2002]. Available from: http://www.en.wikipedia.org/wiki/Energy_harvesting .
- 10.Kumar MD. Electronics for you (EFY), Circuit Ideas. [last cited in 2004 Mar]. Available from: http://www.electronicsforu.com .
- 11.Hanief, Moontasir, Ravigururajan TS. Bio-Thermal Battery for ICDs, Shocker Open Access Repository. [last cited in 2010 Jan 5]. Available from: http://hdl.handle.net/10057/634 .
- 12.Kistler Instrument Corporation GlobalSpec.com Technical library. [ast cited in 2010 Jan 5]. Available from: http://www.globalspec.com .
- 13. [last cited in 2010 Jan 5]. Available from: http://www.ieib.com .
- 14. [last cited in 2010 Jan 5]. Available from: http://news.bbc.co.uk/2/hi/science/nature/


