Abstract
Aim:
This study compares the compressive strength and microleakage of three nanofilled composites using radioactive isotope Ca45.
Materials and Methods:
Thirty-six freshly extracted human premolars were used in this study. Standardized Class I preparation was carried out and then randomly divided into three different groups: A, B, and C with 12 teeth in each group which were restored with nanofilled composite restoration and then subjected to thermocycling. Microleakage was tested using radioactive isotope Ca45. Kruskal–Wallis and Mann–Whitney tests were used to compare the microleakage scores of the three groups. For measuring the compressive strength of three nanofilled composite resin restorations, 12 specimens of each material were prepared in customized stainless steel cylindrical moulds of 6 mm ×4 mm. The compressive test was performed using the Universal Testing Machine. The values were analyzed with ANOVA and Bonferroni's test.
Results:
The findings of this study indicate that the synergy has the least microleakage and highest compressive strength followed by the Grandio and Filtek Z-350.
Conclusions:
Introduction of nanocomposites (packable) appears to have improved the performance of both anterior and posterior restorations with regard to mechanical properties, marginal integrity, and esthetics.
Keywords: Compressive strength, microleakage, nanocomposites
INTRODUCTION
In the past few years, nanomaterials have attracted tremendous international interest in various fields.[1] In dentistry several new materials containing nanoparticles have been developed with improved properties.
Adhesively bonded composites have the advantage of conserving the sound tooth structure while at the same time providing a cosmetically acceptable restoration.[2] Since the very first dental composites were developed, many efforts to improve their clinical performance have been undertaken.[3]
Nanotechnology is the production of functional structures in the range of 0.1–100 nm by various physical or chemical methods. Nano is derived from the Greek word meaning “dwarf”. A nanometer is 10–9 m, or one-billionth of a meter.[4]
Nanocomposites are the premises of new materials that can be applied in many fields due to their improved mechanical properties, lightweight, and light-conducting properties.[5]
Clinical application of composite resins for restoration of posterior teeth requires some mechanical properties to avoid marginal degradation and fracture of restorations. Composite resin posterior restorations are influenced by mechanical properties, such as fracture toughness, compressive strength, flexural strength, wear resistance, and diametral tensile strength. Composite resins have better mechanical properties, such as compressive strength, than other restorations such as conventional or resin-modified glass ionomers, suggesting a longer clinical life in regions submitted to occlusal loads.[6]
Marginal integrity is another important property of the restoration-tooth interface. Marginal leakage is clinically undetectable passage of bacteria, fluids, chemical substances between the tooth and its restoration. Marginal leakage is used as a measure by which clinicians and researchers can predict the performance of a restorative material.[7]
There are several methods by which microleakage can be studied such as the use of dyes, chemical tracers, radioactive isotopes, artificial caries, scanning electron microscopy, neutron activation analysis, and electrical conductivity. Autoradiography is a sensitive technique for determining microleakage. Ca45 has been the most popular isotope to be used, because it is a low-energy β emitter.[8]
The purpose of this study was to compare the microleakage using radioisotope Ca45 and compressive strength of three nanofilled composites currently used in clinical practice. The nanofilled composites compared were Grandio (Voco), Synergy (Coltene Whaldent), and Filtek Z-350 (3M ESPE).
MATERIALS AND METHODS
Thirty-six freshly extracted noncarious human premolars were collected. The extracted teeth were scaled to remove debris, calculus, and rinsed with sodium hypochlorite to remove organic tissue and then stored in distilled water.
The collected teeth were used to check the microleakage at the tooth-restoration interface. Standardized Class I preparation was carried out on all 36 teeth with an airotor handpiece under air/water spray. The size of the preparations was made proportional to the dimensions of the tooth to minimize variations resulting from the tooth size. Standard preparations were to the following specifications: the occlusal isthmus width of 1/3 of distance between cusp tips, the depth of the cavity was 2–2.5 mm and all internal line angles were rounded. After preparation, the toilet of the cavity was performed and the cavity was dried.
The teeth were then etched for 20 s using 37% phosphoric acid and then rinsed with water for 20 s. Prime and Bond NT, a bonding agent, was applied and cured for 15 s. The teeth were then randomly divided into three different groups: A, B, and C with 12 teeth in each group. In Group A, the teeth were restored with Filtek Z-350 as per the manufacturer instructions. The horizontal layering technique for composites was followed, with the incremental curing of each layer using the conventional curing light (Translux CL®, Kulzer) for 40 s. The final layer was contoured and polished using the composite polishing kit (Shofu). In Group B, the teeth were restored with Synergy and in Group C with Grandio as per the manufacturer instructions. The same procedure was followed to restore the cavity as discussed under group A. All specimens were stored at room temperature in distilled water for 24 h. The teeth were then subjected to thermocycling between 5° C and 55° C for 500 cycles. The dwell time in each bath and the time intervals at room temperature between baths were 20 s.
For the autoradiographic examination, the entire external surface of the teeth apart from the restoration and approximately 1 mm beyond the margins were coated with a layer of nail polish to prevent leakage through the root canal, cracks in the enamel, or exposed dentin which can obliterate the true picture of adaptation of the restorative material.
The coated teeth were immersed for 24 h in Ca45 solution, which was diluted with water to give a solution of 0.1 mCi/mL. After removal from the isotope solution, the teeth were rinsed for 1 h in running water and then sectioned mesiodistally using a diamond disc. Two sections were obtained per tooth, and each section was placed on the Kodak film and left for 28 h exposure in the dark. The overall microleakage pattern of each tooth was then examined, and a microleakage score was given as follows:
Score 0: No evidence of isotope at the interface of the tooth and the restorative material.
Score 1: Slight evidence of isotope penetrating through the occlusal margin in the dentin.
Score 2: Moderate evidence of isotope penetrating along the cavity wall but not including the floor of the cavity.
Score 3: Gross evidence of isotope penetrating all around the cavity wall and the floor of cavity.
Kruskal–Wallis and Mann–Whitney tests were used to compare the microleakage scores of the three groups.
For measuring the compressive strength, 12 specimens of each material were prepared in customized stainless steel cylindrical moulds (6 mm × 4 mm). The samples were light cured using the conventional curing unit (Translux CL®, Kulzer) for 60 s. The specimens were stored in distilled water for 24 h and then were subjected to compressive test using the Universal Testing Machine with a load cell of 20 kN. Load was applied at a crosshead speed of 0.1 mm/s at an angle of 90° to the restoration. The load was applied until visible or audible evidence of failure was observed.
The data obtained were subjected to analysis of variance (ANOVA) and Bonferroni's test to compare the compressive strength of three groups.
RESULTS
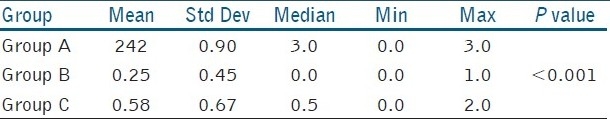
The Kruskal–Wallis test [Table 1] showed a significant difference between the three groups with respect to the microleakage scores (P < 0.001). The Mann–Whitney test concluded that group A has the highest microleakage followed by groups C and B. The mean (and median) difference between groups A and B and groups A and C is statistically significant (P < 0.001). However, the mean (and median) difference between groups B and C is not statistically significant (P > 0.05).
Table 1.
Mean scores for microleakage for various groups
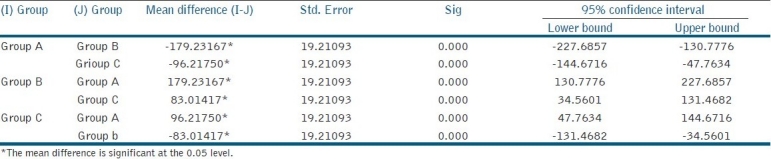
From the above ANOVA results, we conclude that there is a significant difference between all the three groups (P < 0.001). The mean compressive strength is found to be more in group B followed by group C and group A, and this difference is found to be statistically significant. The mean compressive strength in group B is higher than group C, and this difference is also statistically significant [Table 2].
Table 2.
Mean scores of compressive strength of various groups
DISCUSSION
The development of polymeric dental composites has revolutionized the field of dentistry over the past 30 years. Despite these developmental advances, dental composites are still affected by problems such as polymerization shrinkage and wear resistance. With the recent advances in nanotechnology, it is postulated that mechanical properties and polymerization shrinkage of dental composites can be significantly improved.
Filtek Supreme was the first composite resin to show these characteristics and was introduced in the dental market in 2002. This new type of composite was developed because of the increasing demand for a universal restorative material indicated for all types of direct restorations including posterior teeth.[9]
Sol-gel technology has been used extensively in the synthesis of nanoporous materials.[10] There are two types of nanofiller particles used to make nanocomposites. The nanomeric (NM) particles are monodisperse nonaggregated silica nanoparticles which are made from the aqueous colloidal silica sols to synthesize dry powders of nanosized silica particles 20 and 75 nm in diameter. These silica particles are treated with 3-methacryloxypropyltrimethoxysilane (MPTS), a coupling agent. MPTS also allows chemical bonding of the NM filler to the resin matrix during curing.[2]
There are two types of nanoclusters (NC) fillers used. The first type consists of zirconia/silica particles synthesized from a colloidal solution of silica and a zirconyl salt. The primary particle size of this NC filler ranges from 2 to 20 nm, while the spheroidal agglomerated particles have an average particle size of 0.6 μm. The second type of NC fillers, which are synthesized from 75-nm primary particles of silica, has a broad secondary particle size distribution with a 0.6-μm average. Both types of nanocluster filler particles are treated with an MPTS coupling agent.[2] This manufacturing process lowers the possibility of air voids.
Nanotechnology may provide composite resins with filler particles that are smaller, that can be dispersed in higher concentrations, and are polymerized into the resin system with molecules designed to be compatible when coupled with a polymer, and provide unique characteristics (physical, mechanical, and optical).[11]
Tooth and restorations are always subjected to both flexural and compressive forces during the chewing procedure. In this study, the compressive strength of Filtek Z-350 ranged from 316.08–460.35 MPa while for synergy it ranged from 460.19–597.92 MPa and for Grandio it ranged from 397.37–556.52 MPa.
The results of this study are in agreement with prior work done[12–14] where the mechanical properties of nanocomposites are better than the hybrid, microhybrid, and microfilled composites.[15] In addition, it is reasonable to assume that the nanocomposite with a higher compressive strength also has higher fatigue limits as shown in earlier studies.[16]
Microleakage at the tooth–restoration interface is considered to be a major factor influencing the longevity of dental restorations. It may lead to staining at the margins of restorations, recurrent caries, and hypersensitivity of restored teeth and the development of pulpal pathology.[8]
Thermocycling is an in vitro process of subjecting a restoration and a tooth to temperature extremes that confirm to those found in the oral cavity. Evaluation of microleakage must include thermocycling in order to simulate intraoral conditions.
In this study for detecting the microleakage pattern, radioactive isotopes (Ca45) have been used. In general, Ca45 has been the most popular isotope to be used because it is low energy beta emitter[8] and permits detection of minute amount of leakage, as the smaller isotope molecule measures only 40 nm and can penetrate up to 1–2 μm. It has shown that radioisotopes have advantage over dyes as tracers, for their presence can be readily detected even in very small concentrations.[17] Hence radioisotope tracer (Ca45) was employed in this study.
There is great diversity in the brands of nanocomposites. The results of this study may be explained by the volumetric content of the inorganic particles, as the filler content and size directly determine the physical and mechanical properties of composite resin materials. Grandio has 85% w/w or 67.4% vol of the filler content, Filtek Z-350 has 78.5% w/w or 59.5% vol of the filler content, and synergy has 83% w/w or 65% vol of the filler content according to the manufacturer.
Today in market there are various nanocomposites available. The clinician is often baffled to choose the correct material to achieve the optimal strength along with the low post-operative sensitivity. The purpose of this study was to compare the microleakage and compressive strength of three different nanocomposites available in the market. Within the limits of this study, synergy gave the highest compressive strength and the lowest microleakage scores. Thus, it can be assumed that synergy will be more suited in the clinical practice to restore the tooth to its strength with low post-operative sensitivity. Further clinical trials are required to support the results of this study.
CONCLUSIONS
Within the limitations of this study, it can be concluded that:
Synergy has the highest compressive strength followed by Grandio and 3M Filtek Z-350.
Synergy has resulted in the least microleakage, followed by Grandio and 3M Filtek Z-350.
Long-term clinical studies need to be carried out to substantiate the results of this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Saravana Kumar, Vijayalakshmi R. R. Nanotechnology in dentistry. Ind J Dent Res. 2006;17:62–5. doi: 10.4103/0970-9290.29890. [DOI] [PubMed] [Google Scholar]
- 2.Mitra S, Dong W, Brian N. Holmes. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003;134:1382–90. doi: 10.14219/jada.archive.2003.0054. [DOI] [PubMed] [Google Scholar]
- 3.Xu HH, Sun L, Weir MD, Antonucci JM, Takagi S, Chow LC. Nano DCPA whisker composites with high strength and Ca and PO4 release. J Dent Res. 2006;85:722–7. doi: 10.1177/154405910608500807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schleyer TL. Nanodentistry Fact of Fiction. J Am Dent Assoc. 2000;131:1567–8. doi: 10.14219/jada.archive.2000.0085. [DOI] [PubMed] [Google Scholar]
- 5.Colceriu A, Moldovan M, Prejmerean C, Buruiana T, Buruiana EC, Furtos G, et al. Prodan and C.Tamas. Nanocomposite used in dentistry. Eur Cells Mater. 2005;10:19. [Google Scholar]
- 6.Della Bona A, Benetti P, Borba M, Cecchetti D. Flexural and diametral strength of composite resins. Braz Oral Res. 2008;22:84–9. doi: 10.1590/s1806-83242008000100015. [DOI] [PubMed] [Google Scholar]
- 7.Alani AH, Toh CG. Detection of microleakage around dental restorations: A review. Oper Dent. 1997;22:173–85. [PubMed] [Google Scholar]
- 8.Hersek N, Canay S, Akca K, Ciftci Y. Comparison of microleakage properties of three different filling materials. An autoradiographic study. J Oral Rehabil. 2002;29:1212. doi: 10.1046/j.1365-2842.2002.00972.x. [DOI] [PubMed] [Google Scholar]
- 9.Lopes GC. Gustavo Mussi Stefan Oliveria Direct composite resin restorations in posterior teeth. Compendium of continuing education in dentistry. [Last accessed on 2010 Sep 15]. Available from: Available from: http://ce.compendiumlive.com . [PubMed]
- 10.Sun Z. Novel sol-gel nanoporous materials, nanocomposites and their applications in bioscience. Philadelphia: Drexel University Thesis; 2005. [Google Scholar]
- 11.Soh S, Sellinger M, Alan UJ, Yap A. Dental Nanocomposites. Curr Nanoscinone. 2006;2:373–81. [Google Scholar]
- 12.Mota EG, Oshima HM, Burnett LH, Jr, Pires LA, Rosa RS. Evaluation of diametral tensile strength and knoop microhardness of five nanofilled composites in dentin and enamel shades. Stomatologija. 2006;8:67–9. [PubMed] [Google Scholar]
- 13.Chen MH, Chen CR, Hsu SH, Sun SP, Su WF. Low shrinkage light curable nanocomposite for dental restorative material. Dent Mater. 2006;22:138–45. doi: 10.1016/j.dental.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Yamazaki PC, Bedran-Russo AK, Pereira PN, Wsift EJ., Jr Microleakage evaluation of a new low-shrinkage composite restorative material. Oper Dent. 2006;31:670–6. doi: 10.2341/05-129. [DOI] [PubMed] [Google Scholar]
- 15.Yap AU, Teoh SH. Comparison of flexural properties of composite restoratives using the ISO and mini flexural tests. J Oral Rehabil. 2003;30:171–7. doi: 10.1046/j.1365-2842.2003.01004.x. [DOI] [PubMed] [Google Scholar]
- 16.Robert A. Draughn. Compressive fatigue limits of composite restorative materials. J Dent Res. 1979;58:1091–6. doi: 10.1177/00220345790580031101. [DOI] [PubMed] [Google Scholar]
- 17.Fortin D, Vargas MA. The spectrum of composites: New techniques and materials. J Am Dent Assoc. 2000;131:26–30. doi: 10.14219/jada.archive.2000.0399. [DOI] [PubMed] [Google Scholar]


