Abstract
Aims and Objectives:
To compare the microleakage in class II nanocomposite restorations without liner, with resin-modified glass ionomer liner and flowable composite liner.
Materials and Methods:
Thirty-six sound premolars extracted for orthodontic reasons were selected and randomly assigned into three groups of 12 teeth each (Group I, II and III). Class II cavities of specified dimensions were prepared with margins located in the enamel. Cavities in group I were lined with resin modified glass ionomer (GC Fuji II LC-Improved), group II were lined with flowable composite (Filtex Z350 Flowable Restorative) and no liner was placed for cavities in group III. All the teeth were restored with nanocomposite (Z 350 Universal Restorative). The teeth were immersed in 0.5% methylene blue dye, sectioned mesiodistally and observed under stereomicroscope.
Results:
Group III showed maximum leakage compared to group I and II which was statistically significant. Microleakage was lesser in group lined with resin-modified glass ionomer as compared to flowable composite group but not statistically significant.
Conclusions:
Placement of liner beneath nanocomposite restoration results in significant reduction in microleakage. Both resin-modified and flowable composite liners under nanocomposite restorations result in comparable reduction of microleakage.
Keywords: Liner, microleakage, nanocomposite
INTRODUCTION
In the past 10 years a dramatic improvement in adhesive technology and resin composite formulations has occurred. The recently developed nanocomposites show esthetic properties similar to those of microfills while maintaining physical properties equivalent to those of hybrid composites. This allows the clinician to use them for both anterior and posterior restorations.[1,2]
Microleakage of posterior composite restorations is a matter of concern to the clinician as it leads to staining at the margins of restorations, recurrent caries, hypersensitivity and pulp pathology.[3] Polymerization shrinkage is one of the important factors leading to microleakage. The use of liners has been considered as it may act as a flexible intermediate layer, relieving the stresses of polymerization shrinkage.[4,5] Resin-modified glass ionomers and flowable composites, resinous liners have been used as lining materials.[6] The use of resin-modified glass ionomer has various advantages such as bonding chemically to tooth structure and micromechanically to composites, improved biocompatibility, fluoride release and marginal integrity.[7] Flowable composites have been recommended as liners beneath composites due to their low viscosity, increased elasticity and wettability. This results in an intimate union with the floors and walls of the cavity preparations.[8,9] However, whether the elastic layer concept can actually decrease microleakage is not yet conclusive as previous in vitro studies have yielded conflicting results.[10] Also, there is no clear agreement over what type of liner material would provide the best performance.[4]
Although in vitro and in vivo studies have been carried out with glass ionomers and flowable composites as liners, the efficacy of one over the other is yet to be proven. Moreover, recently developed nanocomposite restorative material has not been studied with these liners. Hence this study was done with an objective to compare the microleakage in Class II nanocomposite restorations without liner, with resin-modified glass ionomer liner and nanofilled flowable composite liner.
MATERIALS AND METHODS
Tooth selection and cavity preparation
Thirty six non carious upper premolar teeth extracted for orthodontic purposes were selected. The teeth were stored in normal saline soon after extraction and cleaned with slurry of pumice and water prior to preparation. Standard class II cavities were prepared using a high-speed hand piece under air-water spray and diamond burs (Shofu#440M and #411, Shofu Inc, Japan) as shown in Figure 1. Measurement of the cavity preparations were standardized using metallic scale and calibrated periodontal probe. All teeth were stored in distilled water to prevent desiccation. The teeth were randomly divided into three groups with 12 teeth in each group.
Figure 1.
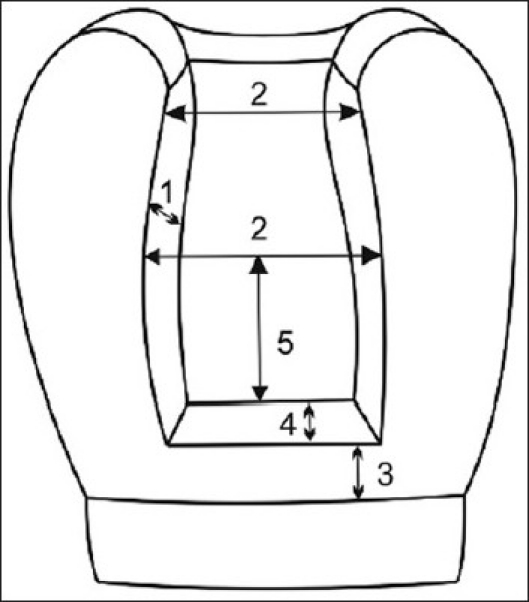
Schematic representation of the cavity preparation dimension: proximal view, Depth of occlusal preparation = 1.5 mm, Width of occlusal and proximal preparation = 3 mm, Location of gingival cavosurface = 1.5 mm occlusal to cemento enamel junction, Width of gingival floor from enamel = 1.5 mm, Depth of the axial wall = 3 mm
Restoration
Group I: Dentin conditioner (GC Dentin Conditioner, GC Dental Corp, Japan) was applied using a cotton pellet for as per manufacturer's instructions. Universal Tofflemire matrix band with retainer were adapted to the teeth. Resin-modified glass ionomer liner (Fuji II LC Improved, GC Dental Corp, Japan) of 1-mm thickness was placed with a cement carrier extending to the full width of pulpal floor, gingival seat, axial wall and light cured for 20 seconds. The remaining walls were etched for 20 seconds with 37% phosphoric acid (Scotch Bond, 3M ESPE, USA) and rinsed with water for 10 seconds and air dried. Two coats of a single component total etch adhesive (Adper™ Single Bond 2, 3M ESPE, USA) was applied with the nylon-bristled brush, as per manufacturer's instructions. Nano composite (Filtek Z350 Universal Restorative, 3M ESPE) was built up in a diagonal increment technique of 2-mm thickness with a plastic filling instrument with each increment cured for 40 seconds.
Group II: Etching enamel and dentin, application of matrix band and single component total etch adhesive application to the etched surface was done as described in group I. One-millimeter thick flowable composite material (Filtex™ Z 350 Flowable Restorative, 3M ESPE, USA) was placed on pulpal, axial walls and the gingival seat as cavity liner the thickness of which was maintained by a groove on the delivery needle. This was light cured for 40 seconds. Then the composite material was placed over the flowable restorative and restored in the same manner as described in Group I.
Group III: The cavities were restored with nanocomposite material without any liner. The same technique was followed as in group I for etching of enamel and dentin, application of matrix band, dental adhesive and placement of composite material.
Light curing was done using Cool Blue™ LED (Milestone Scientific, Livingston, NJ, USA) with a light intensity of 400 mW/cm2. Following completion of restoration, excess cement was removed using a super fine diamond burs and finishing was done with a series of Sof-Lex disks (3M ESPE, USA). The restored teeth of all the three groups were stored in a container of distilled water at room temperature for 1 week.
Thermocycling procedure and dye immersion
The teeth were subjected to thermocycling which consisted of 250 times in water baths maintained at 5°C, 37°C and 55°C with a dwell time of 30 seconds. Then the apex of each tooth was sealed with acrylic resin and the teeth were painted with two coats of nail varnish, except for the area of 2 mm from the periphery of the restorations. The coated teeth were immersed in 0.5% methylene blue dye for 48 hours. The teeth were then rinsed with tap water, dried and sectioned mesiodistally through the centre of the restorations using a carborandum disc.
Dye penetration evaluation
Each specimen was examined with a stereomicroscope (Sterostar zoom stereomicroscope, Reichert Jung Co., Germany) and graded according to dye penetration. Dye penetration was measured from both occlusal and gingival margins. Scoring was done by an independent examiner first; observations were confirmed by another trained examiner.
The scoring criteria were[11]
Occlusal margin
0 = No evidence of dye penetration
1 = Superficial penetration of dye at the margin but less than one-third of the width of mesial/distal wall
2 = Penetration along the margin beyond one-third of the width of mesial /distal wall, up to the pulpal floor
3 = Penetration along the pulpal floor
Gingival margin
0 = No evidence of dye penetration
1 = Superficial penetration of dye at the margin but less than one-third of the gingival width
2 = Penetration along the margin beyond one-third of the gingival width up to the axial wall
3 = Penetration along the axial wall
Statistical analysis
Data was analyzed using SPSS for Windows release 11.5 (SPSS, Chicago, IL, USA). Pearson's χ2 test was used to assess differences between the groups and Mann-Whitney U test was used to investigate the pair wise differences between different groups.
RESULTS
Table 1 shows the distribution of scores based on dye penetration into cavity preparation at the occlusal level and gingival level, respectively. At the occlusal level 36.1% restorations were totally free of microleakage. Only one specimen from control group showed no dye penetration and in group I and group II 50% of specimens had dye penetration score corresponding to 0.
Table 1.
Distribution of dye penetration scores at the occlusal and gingival level
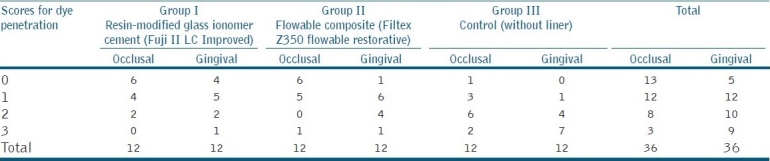
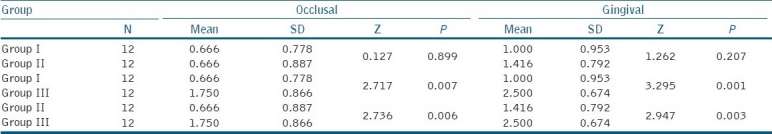
Pearson's χ2 test revealed that there was statistically significant difference in microleakage between the groups at both occlusal (χ2 = 13.34; P= 0.038) and gingival levels (χ2 = 17.50; P=0.008). Pair wise comparison using Mann-Whitney U test revealed that Group III had significantly higher microleakage at both occlusal and gingival levels as compared to Group I and Group II. At gingival level, Group I exhibited slightly lesser microleakage than group II but was not statistically significant [Table 2]. Group I showed no significant difference between microleakage at occlusal and gingival level (Z=0.866; P=0.387). However, in Group II and Group III, there was significantly greater microleakage at the gingival level (Z= 2.31 and 2.19; P= 0.021 and 0.027, respectively).
Table 2.
Pairwise comparison of occlusal and gingival microleakage using Mann-Whitney U test
DISCUSSION
In this study, the resin modified glass ionomer liners in Group I were not acid etched as it causes weakening of the cement matrix.[12] Also, resin-modified glass ionomers chemically bond with resin composites which is enhanced by placement of adhesives.[13] The diagonal increment technique used in this study minimizes the stress at resin-tooth interface. By placing successive layers of apicoocclusal wedges of composite, the C-factor for each layer is decreased, thus decreasing the overall polymerization shrinkage.[14]
The results of this study potentiate the importance of using liners under nanocomposite restorations, as the group without liner showed significantly higher microleakage. Polymerization shrinkage of nanocomposites can produce cracks at the resin-tooth interface, which contribute to microleakage. Both resin-modified glass ionomer liners and flowable composite liners have lower modulus of elasticity and hence deform and/or flex to a degree when subjected to an external force.[15] This characteristic is thought to attenuate shrinkage stress from the subsequently placed higher modulus composite restoratives. Also, application of liners reduces the volume of composite and configuration factor (C-factor) of the cavity.[13] Although resin-modified glass ionomer has low tensile strength compared to composite leading to cohesive failure, the effect of low tensile strength was reduced by using resin-modified glass ionomer as a thin liner.[7] Some of the previously published studies[16,17] have reported that flowable composites as liners under posterior composites do not significantly reduce microleakage. Despite their low elastic modulus, the contraction stress generated during curing process pulls the flowable composite away from the tooth wall leading to gap formation and microleakage.[17] But findings from this study revealed that flowable composite lining improved marginal adaptation of composite compared to group without liner. Perhaps the relatively thin layer of liner used in this study would have minimized the effect of polymerization shrinkage. Chuang et al,[18] concluded in their study that use of 0.5-1.0 mm thick layer of flowable composites liner under packable composite restorations results in significant reduction in microleakage.
However, use of liners did not totally prevent microleakage. Among the group with liners, 33.33% specimens showed dye penetration at the occlusal level, and 52.8% at gingival level. Thus optimal dentin bonding is quite important to compensate for shrinkage stress.[9] Findings from this study support the findings of earlier studies,[19–21] which demonstrate that gingival margins are potentially a greater source of microleakage in class II composite restorations compared to occlusal margin. This is due to lesser thickness of enamel at the cavosurface margin of the proximal aspect which requires adhesion of the restorative materials to greater proportion of dentin; a less reliable, more complex substrate than enamel.[22] Another reason for increased gingival microleakage relates to the distance of light source from the material at the proximal box base as compared to occlusal surfaces.[21] Resin-modified glass ionomer group was better than others in this respect as there was no statistically significant difference in microleakage between occlusal and gingival margins.
Microleakage at gingival level was more in flowable liner group when compared to resin-modified glass ionomer group, but not statistically significant in this study. The marginally better performance of resin-modified glass ionomer may be due to its ability to both micromechanically and chemically interact with dentin and form strong bonds.[23] The intrinsic porosity and water sorption of the resin-modified glass ionomer can compensate for polymerization shrinkage.[5] Also, the coefficient of thermal expansion and elastic modulus similar to dentin.[24] On the other hand, flowable composites shrink more than nanocomposite as they have lesser filler loading and a greater proportion of resin matrix.[16] The difference in coefficient of thermal expansion and elastic modulus between the composite and dentin causes stress in the interfacial gaps contributing to microleakage.[25] Use of syringe delivery system for flowable composites as compared to hand instrument for resin modified glass ionomer may have contributed to better adaptation of flowable composite to cavity walls resulting in comparable levels of microleakage in this study.
CONCLUSIONS
Under the conditions of this in vitro study
Gingival margins are more susceptible to microleakage than occlusal margins in class II cavities.
Placement of 1-mm thickness liner beneath nanocomposite restorations results in significant reduction in microleakage but does not totally prevent it.
Both resin-modified glass ionomer and flowable composite can be used as liners under nano composite restorations as reduction in microleakage was comparable.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mitra SB, Wu D, Holmes BN. An application of nanotechnology on advanced dental materials. J Am Dent Assoc. 2003;134:1382–90. doi: 10.14219/jada.archive.2003.0054. [DOI] [PubMed] [Google Scholar]
- 2.Chen MH. Update on dental nanocomposites. J Dent Res. 2010;89:19–28. doi: 10.1177/0022034510363765. [DOI] [PubMed] [Google Scholar]
- 3.Dresch W, Volpato S, Gomes JC, Ribeiro NR, Reis A, Loguercio AD. Clinical evaluation of a nanofilled composite in posterior teeth: 12 month results. Oper Dent. 2006;31:409–17. doi: 10.2341/05-103. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz J JL, Mitra S. Using cavity liners with direct posterior composite restorations. Compend Contin Educ Dent. 2006;27:347–51. [PubMed] [Google Scholar]
- 5.Davidson CL. Glass-ionomer bases under posterior composites. J Esthet Dent. 1994;6:223–4. doi: 10.1111/j.1708-8240.1994.tb00863.x. [DOI] [PubMed] [Google Scholar]
- 6.Dewaele M, Asmussen E, Devaux J, Leloup G. Class II restorations: Influence of a liner with rubbery qualities on the occurrence and size of cervical gaps. Eur J Oral Sci. 2006;114:535–41. doi: 10.1111/j.1600-0722.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 7.Aboushala A, Kugel G, Hurley E. Class II composite resin restorations using glass-ionomer liners: Microleakage studies. J Clin Pediatr Dent. 1996;21:67–70. [PubMed] [Google Scholar]
- 8.Bayne SC, Thompson JY, Swift EJ, Jr, Stamatiades P, Wilkerson P. A characterization of first generation flowable composites. J Am Dent Assoc. 1998;129:567–77. doi: 10.14219/jada.archive.1998.0274. [DOI] [PubMed] [Google Scholar]
- 9.Attar N, Tam LE, McComb D. Flow, strength, stiffness and radioopacity of flowable resin composites. J Can Dent Assoc. 2003;61:516–21. [PubMed] [Google Scholar]
- 10.Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent. 2007;9:469–75. [PubMed] [Google Scholar]
- 11.Leevailoj C, Cochran MA, Matis BA, Moore BK, Platt JA. Microleakage of posterior packable resin composites with and without flowable liners. Oper Dent. 2001;26:302–7. [PubMed] [Google Scholar]
- 12.Sheth JJ, Jensen ME, Sheth PJ, Versteeg J. Effect of etching glass-ionomer cements on bond strength to composite resin. J Dent Res. 1989;68:1082–7. doi: 10.1177/00220345890680060501. [DOI] [PubMed] [Google Scholar]
- 13.Arora V, Kundabala M, Parolia A, Thomas MS, Pai V. Comparison of the shear bond strength of RMGIC to a resin composite using different adhesive systems: An invitro study. J Conserv Dent. 2010;13:80–3. doi: 10.4103/0972-0707.66716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liebenberg WH. Successive cusp build-up: an improved placement technique for posterior direct resin restorations. J Can Dent Assoc. 1996;62:501–7. [PubMed] [Google Scholar]
- 15.Sidhu SK, Henderson LJ. In vitro marginal leakage of cervical composite resins restorations lined with a light-cured glass ionomer. Oper Dent. 1992;17:7–12. [PubMed] [Google Scholar]
- 16.Tollidos K, Setcos JC. Initial degree of polymerization shrinkage exhibited by flowable composite resins. J Dent Res. 1999;78:483–5. [Google Scholar]
- 17.Tredwin CJ, Stokes A, Moles DR. Influence of flowable liners and margin location on microleakage of conventional and packable class II resin composites. Oper Dent. 2005;30:32–8. [PubMed] [Google Scholar]
- 18.Chuang SF, Jin YT, Liu JK, Chang CH, Shieh DB. Influence of flowable lining thickness on class II composite restorations. Oper Dent. 2004;29:301–8. [PubMed] [Google Scholar]
- 19.Derhami K, Colli P, Brannstrom M. Microleakage in Class 2 composite restorations. Oper Dent. 1995;20:100–5. [PubMed] [Google Scholar]
- 20.Hilton TJ, Schwartz RS, Ferracane JL. Microleakage of four class II resin composite insertion techniques at intra oral temperature. Quintessence Int. 1997;28:135–44. [PubMed] [Google Scholar]
- 21.Demarco FF, Ramos OL, Mota CS, Formolo E, Justino ML. Influence of different restorative techniques on microleakage in class II cavities with gingival wall in cementum. Oper Dent. 2001;26:253–9. [PubMed] [Google Scholar]
- 22.Coli P, Brannstrom M. The marginal adaptation of different bonding agent of four different bonding agents in class II composite restorations applied in bulk or in two increments. Quintessence Int. 1993;24:583–91. [PubMed] [Google Scholar]
- 23.Bona AD, Pinzetta C, Rosa V. Effect of acid etching of glass ionomer cement surface on the microleakage of sandwich restorations. J Appl Oral Sci. 2007;15:230–4. doi: 10.1590/S1678-77572007000300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitra SB, Conway WT. Coefficient of thermal expansion of some methacrylate modified glass ionomers. J Dent Res. 1994;73:21. 9 Abstract ≠ 944. [Google Scholar]
- 25.Carvalho RM, Pereira JC, Yoshiama M, Pashley DH. A review of polymerization contraction: The influence of stress development versus stress relief. Oper Dent. 1996;21:17–24. [PubMed] [Google Scholar]


