Abstract
Aim:
The study aims to evaluate and compare total gap surface area formed after restoration of class II cavities with Filtek Z350 and P60 at room temperature, 37°C and 54°C.
Materials and Methods:
Thirty extracted maxillary and mandibular molars were taken and divided into six groups of five teeth each. Standardized class II cavities were made and were restored with Filtek Z350 and P60, both at room temperature, 37°C and 54°C. Group 1(a) was restored with Filtek Z350 at room temperature, Group 1(b) with Filtek Z350 at 37°C and Group 1(c) with Filtek Z350 at 54°C. Group 2(a) was restored with P60 at room temperature, Group 2(b) with P60 at 37°C and Group 2(c) with P60 at 54°C. After storing the samples in distilled water at room temperature for 48 hours, longitudinal sectioning was done to obtain tooth restoration interface. The interfaces were then examined under compound light microscope with digital output and analyzed using Image J analysis software.
Results:
The results demonstrated better adaptation and less total gap area formation at 54°C as compared to room temperature and 37°C.
Conclusions:
Based on the results of this study, it is suggested that use of P60 is better suited for posterior restorations at 54°C as compared to Filtek Z350 universal nanohybrid at room temperature.
Keywords: Class II restorations, gap formation, Image analysis software, preheating composite resin
INTRODUCTION
For more than a century, amalgam has enjoyed the preference for class I and II restorations. The rising demand for use of esthetic materials in posterior teeth has increased dramatically over the past two decades, surpassing amalgam. Excellent esthetics, thermal non-conductivity, absence of mercury and bonding to tooth structure led to promising role of composite resin as a substitute for amalgam. However, composite exhibits shortcomings like polymerization shrinkage, postoperative sensitivity, inadequate proximal contact,[1] poor wear resistance and lack of proper adaptation in some clinical situations.[2] Furthermore, many contemporary composite resins are sticky and difficult to manipulate, resulting in problems during placement.[3]
Some potential ways to overcome these issues of adaptability and polymerization shrinkage are:
Use of lower viscosity flowable composites in non-stress bearing areas;
Use of flowable liner in conjunction with regular composites; and
Preheating the composites to lower their viscosity.[4]
The effect of lower viscosity in improvement of adaptation has been proven important. This is the primary basis for development for flowable resin composites. Lower viscosity can be achieved in these flowable composites by decreasing their filler content and by making changes in matrix chemistry, which severely reduces their physical properties enabling them to be used in posterior restorations.[4] An inverse relationship has been shown to exist between inorganic filler loading and monomer conversion (Miyazaki et al, 1991; Razak and Harrison, 1997; Labella et al, 1999; Barron, Rueggebergand Schuster, 1992). Plastic flow allows part of the shrinkage to take place without stress build-up at the interface and will determine the proportion of remaining shrinkage that manifests itself as detrimental rigid contraction.[5]
Many polymers exhibit lower viscosity when they are heated. The theory behind this is that thermal vibrations force the composite monomer/oligomers further apart, allowing them to slide by each other more readily.[4]
We evaluated the effect on nanofilled universal hybrid (Filtek Z350, 3M ESPE, St. Paul, Minn, USA) and packable composite (P60, 3M ESPE, USA) at room temperature, 37°C and 54°C.
MATERIALS AND METHODS
Selection of specimens
Thirty extracted caries-free human molars (both maxillary and mandibular) were selected. The teeth were examined visually for any hypoplastic defects or fracture/craze lines. The surface deposits and stains were carefully removed with ultrasonic scaling. The specimens were stored in water at room temperature until use.
Tooth preparation
Two class II preparations were made on each tooth (mesial and distal) with high-speed handpiece (NSK, Tokyo, Japan) using water spray and diamond fissure (SF-4, Dia burs, MANI, Tochigi, Japan) and inverted cone burs (SI 46, Dia burs, MANI, Tochigi, Japan).
The dimensions of all the cavities prepared were kept constant: buccolingual width of proximal box was 2 mm, depth of pulpal floor (from central fissure) was 2 mm, depth of gingival seat (from central fissure) was 3 mm. All dimensions were measured using a William's periodontal probe and a steel scale.
Grouping of teeth
All the prepared teeth were randomly divided into six groups (five teeth/group). The groupings are as follows.
In Group 1, teeth were restored with Filtek Z350 at room temperature [Group 1(a) as control], at 37°C [Group 1(b)], and at 54°C [Group 1(c)].
In Group 2, teeth were restored with posterior composite P60 at room temperature [Group 2(a) as control], at 37°C [Group 2(b)], and at 54°C [Group 2(c)].
Teeth restorations
All the restorations were performed by a single operator.
All cavities were acid etched (Scotchbond Multipurpose, 3M ESPE) for 20 seconds, followed by rinsing with water for 10 seconds. The specimens were allowed to dry. Following this, single layer application of adhesive (Adper Single Bond 2, 3M ESPE) was done and cured for 20 seconds.
Restoration of teeth that were to be restored at room temperature was done first. Multiple increments were compacted in the cavities for both groups 1(a) and 2(a) with Filtek Z350 and P60, respectively. Light curing was done using LED curing lamp (Woodpecker) for 20 seconds for each increment.
Materials from compules of Filtek Z350 and P60 were taken in Petri dishes, (in order to avoid any temperature difference between the surface and core of the composite tube) and heated to temperatures of 37°C and 54°C. The materials in the respective incubators were allowed to be heated for 10 minutes.
Each increment was taken from the respective Petri dishes and was compacted in the respective sample cavities and cured for 20 seconds, until build-up was complete.
Final finishing and polishing of the restorations were done using Enhance Finishing and Polishing kit (Dentsply, Melford, DE, USA).
All the specimens were stored in water at room temperature for 48 hours, until performing the sectioning procedure.
Sectioning methodology and gap total surface area measurement
For each tooth, the radicular portion was separated from the crown. The crown thus obtained (with two proximal restorations) was sectioned off at the midline longitudinally in buccopalatal direction, thus splitting the tooth into mesial and distal halves. Again, each proximal half thus obtained was reduced in buccopalatal direction, from either buccal/lingual aspect, to obtain tooth restoration interface.
Post sectioning, each sample was smoothened with fine grit sandpaper. The samples were thus made ready for observation under light microscope. Before observation of the samples, standardization for measurement was done using a stage micrometer observed under compound light microscope (Olympus, Tokyo, Japan) at 4× magnification. A specific distance between 0.0 and 0.1 mm was measured in pixels (in this case, 572.31) using Image J analysis software 1.42q (NIH, USA). The reading was kept constant throughout the observations.
Each section was observed under a compound light microscope at 4× magnification, and a photomicrograph was taken for every sample with a camera (Olympus, Japan) mounted over the microscope with separate attachment apparatus. Each photomicrograph was subjected to color enhancement, contrast and brightness adjustments, and converted into 8-bit grayscale image.
Appropriate threshold was adjusted to ensure selection of gaps at tooth restoration interface, and total surface area of the gaps for each sample was recorded.
Statistical analysis
The void areas obtained between the samples manipulated at room temperature, 37°C and 54°C were compared using analysis of variance (ANOVA) test. Further assessment of comparison between the subgroups was done using post hoc Tukey test. Overall comparison between Filtek Z350 and P60 was done using Mann–Whitney U test.
RESULTS
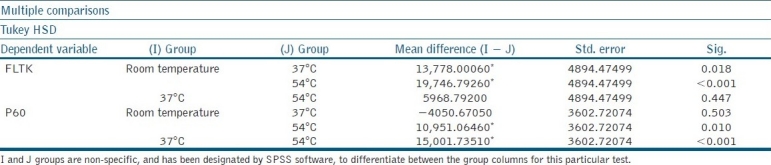
The results given in Table 1 denote that in case of Filtek Z350, the material showed significant differences between Group 1(a) and Group 1(b) (significance 0.018) and also between Group 1(a) and Group 1(c) (<0.001). The table also shows that in case of P60, there was a significant difference between Group 2(a) and Group 2(c) (0.010) and also between Group 2(b) and Group 2(c) (<0.010).
Table 1.
Post hoc Tukey test
DISCUSSION
In recent years, resin composites have become more useful as posterior restorative materials. Polymerization shrinkage is one of the primary deficiencies which complicate the use of composites to its full potential.[6] Current methods for placing composite into cavity preparations have many problems. High viscosity and stickiness of highly filled composite makes the insertion, as well as adaptation, of the material to preparation walls difficult and unpredictable. Also, the extent of resin polymerization under room temperature conditions yields polymers of relatively low monomer conversion.[7]
The packable composites are designed to be inherently more viscous to afford “feel” upon insertion similar to amalgam.[6] But compared to amalgam, the technique for composite placement is far more time consuming and demanding because of its high plastic and paste like consistency in precured state.[8] These packable composites cannot be compacted vertically into a cavity in such a way that material flows laterally as well as vertically to ensure intimate contact; hence, void remains. The packable composites were developed for situations in which improved condensability is needed, e.g. class I and class II restorations.
The nanofilled hybrids combine the properties of high mechanical strength for posterior restorations and can also be used for anterior restorations because of their superior esthetics. These properties are achieved by reduced dimension of particles and wide distribution range. As a consequence, filler load increases and polymerization shrinkage decreases. The small size of filler particles also improves their optical properties, as their (particles’) diameters are a fraction of wavelength of visible light (0.4–0.8 μm), resulting in inability of the human eye to detect the particles. Also, a small particle has a large surface area to volume ratio compared to a large particle, which has a small surface area to volume ratio. Therefore, for a given volume of filler, larger the size of filler, lesser is the resin required to envelop the filler particles and greater is the mass of resin matrix in between, hence resulting in greater shrinkage.[1]
Advantages of preheating the resin are to make more durable, highly filled, highly viscous conventional composite resin, to reduce the viscosity, to provide flow values that are similar to those of less filled, flowable composite resins, without undermining the mechanical properties. An additional advantage of heating the resin prior to placement is an accompanying increase in monomer conversion and polymerization rate.[3] With increased paste temperature, free radicals and propagating polymer chains become more mobile as a result of decreased paste viscosity and react to a greater extent, resulting in a more complete polymerization reaction and greater cross-linking.[9] In their study, Daronch et al. observed that increase in polymerization temperature increases the conversion of dimethacrylate monomers, but only up to a certain temperature limit. After the limit, monomer conversion decreases with subsequent temperature increase. The phenomenon resulted due to reactant evaporation and photoinitiator degradation.[7]
The viscosity of resins decreases and flow increases by heating them prior to placement and curing procedure. The flow characteristics of resin composites affect their ability to adapt to cavity preparation. A resin composite with higher flow adapts more easily to the intricacies of a cavity preparation than the one with lower flow values.[10]
The purpose of this study was to evaluate the effect of polymerization shrinkage on gap formation at tooth–restoration interface, at three different temperatures, i.e. room temperature, 37°C, 54°C. As a secondary analysis it was also evaluated which of the two materials performed better at elevated temperatures, showing less gap formation at the interface.
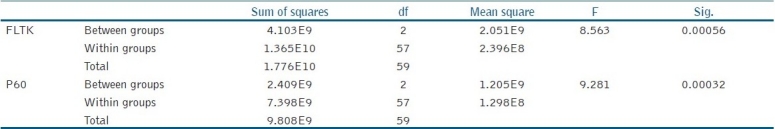
In Table 2, it can be seen that there was an average reduction in total gap surface area, from room temperature to 54°C, in both Filtek Z350 and P60 groups. This can be explained by decrease in system viscosity and enhanced radical mobility at increased temperatures, resulting in additional polymerization and higher conversion.[11] The collision frequency of unreacted active groups and radicals increases with elevated curing temperature when below glass transition temperature.[10] Also, at elevated temperatures, there is free volume increase, giving the trapped radicals increased mobility, resulting in further conversion.[11]
Table 2.
ANOVA test
In Table 1, it can be seen that there was a significant difference between Group 1(a) and Group 1(b) (0.018) and also between Group 1(a) and Group 1(c) (<0.001), indicating that total area of voids reduced as the temperature was raised to 37°C and to a greater extent at 54°C.
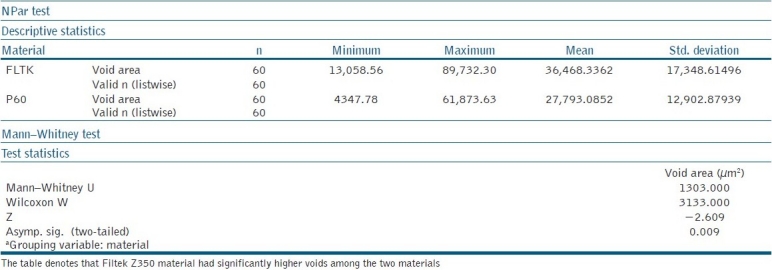
In Table 3, an overall comparison has been made between Filtek Z350 and P60. It can be seen that the Filtek Z350 material showed significantly greater area of voids.
Table 3.
Total void area assessment between the two materials
Another concern is regarding delivery of the preheated composite resin. In a study by Walter, it was reported that the warmed resin loses approximately 50% of the increased temperature within 2 minutes after removal from the device and the loss is about 90% within 5 minutes. The rate of heat loss could be affected by placement into a cavity preparation, which could act as a heat sink.[12] Also, in a study by Daronch, it was argued that the resin be additionally heat soaked for a longer period to counter the cooling effect when the composite compule is removed from the heating unit. Given the fact that composite cools at a very rapid rate after removal from the heating unit, any time saving is essential in enhancing the performance of pre-warmed composite. A time of 4.5 seconds was responsible for a 3° difference between the two methods. Therefore, placement of the compule directly into the delivery syringe during compule preheating seems advantageous over preheating only the individual compule itself.[7]
A concern regarding preheating is the impact of this elevated temperature on the pulp tissue. According to Maeda et al., the intraoral physiologic temperature range in humans is from 34.2°C to 36.6°C. Other studies reported critical temperature limit for pulpal fibroblast to be 41.5°C.[9] According to Trujillo et al., the pulp vitality may potentially be compromised by temperature rises of greater than about 5°C from the baseline level of approximately 32–34°C.[13]
Contrary to the concern, it has been reported that in clinical situations when the resin composite is preheated, the temperature of the resin composite could affect the pulp tissue when it is placed in the cavity, but in the time delay between dispensing it from the syringe and placing it into the preparation, a significant decrease occurs.[9] Daronch et al. found no significant differences in the intrapulpal temperature between room temperature and preheated resin composite at similar restorative stages.[14] In another study, Daronch et al. concluded that the resin composite temperature decreased rapidly upon removal of compule from the heating device.[15] It was observed that upon placement of composite preheated to 54.5°C, the temperature rise recorded by a thermocouple situated in the pulp chamber was only 2.4 ± 0.3°C. Such a temperature rise would suggest that the composite could be placed with relative safety.[13]
CONCLUSIONS
Under the conditions of present study, the following conclusions can be made.
Preheating the resin composite to elevated temperature, i.e. 54°C, increases the adaptation and lowers the total gap surface area. This in vitro study has shown that posterior composite (P60) proved better for class II restorations, at higher temperatures of 54°C, than universal nanohybrid Filtek Z350.
However, further studies with a larger sample size, involving various restorative materials, need to be undertaken in order to assess the result of preheating for optimum clinical advantage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Aw TC, Nicholls JI. Polymerization Shrinkage of Densely-Filled resin Composites. Oper Dent. 2001;26:498–504. [PubMed] [Google Scholar]
- 2.Deliperi S, Bardwell DN. An alternative to reduce polymerization shrinkage in direct posterior composite restorations. J Am Dent Assoc. 2002;133:1387–98. doi: 10.14219/jada.archive.2002.0055. [DOI] [PubMed] [Google Scholar]
- 3.Blalock JS, Holmes R, Rueggeberg FA. Effect of temperature on unpolymerized composite resin film thickness. J Prosthet Dent. 2006;96:424–32. doi: 10.1016/j.prosdent.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 4.Wagner WC, Asku MN, Neme AL, Linger JB, Pink FE, Walker S. Effect of Pre-heating Resin Composite on RestotationMicroleakage. Oper Dent. 2008;33:72–8. doi: 10.2341/07-41. [DOI] [PubMed] [Google Scholar]
- 5.Labella R, Lambrechts P, Meerbeek BV, Vanherle G. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent Mat. 1999;15:128–37. doi: 10.1016/s0109-5641(99)00022-6. [DOI] [PubMed] [Google Scholar]
- 6.Roberson TM, Heymann HO, Ritter AV. Introduction to Composite restorations. In: Roberson TM, editor. Art and Science of Operative Dentistry. 4th ed. New Delhi: Elsevier; 2004. p. 478. [Google Scholar]
- 7.Daronch M, Rueggeberg FA, Moss L, De Goes MF. Clinically Relevant Issues Related to Preheating Composites. J Esthet Restor Dent. 2006;18:340–51. doi: 10.1111/j.1708-8240.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 8.Rawls HR, Upshaw JE. Restorative Resins. In: Anusavice, editor. Science of Dental Materials. 11th ed. New Delhi: Elsevier; 2005. p. 429. [Google Scholar]
- 9.Uctasli MB, Arisu HD, Lasilla LV, Valittu PK. Effect of Preheating on the Mechanical Properties of Resin Composites. Eur J Dent. 2008;2:263–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Knight JS, Fraughn R, Norrington D. Effect of temperature on the flow properties of resin composite. General Dentistry. 2006;54:14–6. [PubMed] [Google Scholar]
- 11.Daronch M, Rueggeberg FA, De Goes MF, Guidici R. Monomer Conversion of Pre-heated Composite. J Dent Res. 2005;84:663–7. doi: 10.1177/154405910508400716. [DOI] [PubMed] [Google Scholar]
- 12.Walter R, Swift E, Jr, Sheikh H, Ferracane JL. Effects of temperature on composite resin shrinkage. Quintessence Int. 2009;40:843–7. [PubMed] [Google Scholar]
- 13.Trujillo M, Newman SM, Stansbury JW. Use of near-IR to monitor the influence of external heating on dental composite photopolymerization. Dent Mat. 2004;20:766–77. doi: 10.1016/j.dental.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Daronch M, Rueggeberg FA, Hall G, De Goes MF. Effect of composite temperature on in vitro intrapulpal temperaturerise. Dent Mater. 2007;23:1283–8. doi: 10.1016/j.dental.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 15.Daronch M, Rueggeberg FA, De Goes MF, Guidici R. Polymerization kinetics of Pre-heated composite. J Dent Res. 2006;85:38–43. doi: 10.1177/154405910608500106. [DOI] [PubMed] [Google Scholar]


