Abstract
Background:
80% of patients undergoing surgical procedures experience postoperative pain1 and requires adequate pain relief. Nowadays drugs like COX2 inhibitors and calcium channel modulators (Pregabalin and Gabapentin) are been increasingly used for postoperative pain management effectively. We conducted this study to find whether preoperative pregabalin has any effect in postoperative analgesic requirement in patients undergoing hysterectomy under spinal anaesthesia.
Patients & Methods:
This randomized, double-blind, placebo-controlled trial was conducted in 150 patients undergoing hysterectomy under spinal anaesthesia, divided in three groups - Group I (PO) - Control group, Group II (P150) received 150 mg pregabalin and Group III (P300) received 300 mg pregabalin. We used VAS for anxiety, Ramsay sedation scale and VAS for patient satisfaction regarding pain relief.
Results:
There was significant reduction in anxiety in groups P (150) and P (300) than placebo group P (0) during intraoperative and postoperative period than preoperative period. There was significant sedation seen in groups P (150) and P (300) than placebo group P (0). First rescue analgesia in group P (300) was202.42±6.77 and in group P (150) was176.38±4.80on average, group P (0) was131.38±5.15. Dizziness was 44.44% in group P (300), 36.11% in group P (150), and 19.44% in group P (0). Patient satisfaction was better in P (300) group than other two groups.
Conclusions:
Pregabalin being an oral drug which would be easy for the patients to take and also its prolongation of the neuraxial block helps in immediate postoperative analgesia and further reduction of other parentral analgesics. Pregabalin 150mg would be the optimal preemptive dose for hysterectomy under spinal anaesthesia.
Keywords: Subarachanoid Block, Pregabalin, Hysterectomy
Every patient who undergoes surgery is in need of postoperative pain relief. 80% of patients undergoing surgical procedures experience postoperative pain1 and requires adequate pain relief. Opioids are the important analgesic used for intraoperative and postoperative pain relief. But opioids itself has its own side effects2. Nowadays drugs like COX2 inhibitors and calcium channel modulators (Pregabalin and Gabapentin) are been increasingly used for postoperative pain management effectively. This has the advantage of avoiding the side effects of oipiods. Pregabalin and Gabapentin are structural analog of GABA. Pregabalin selectively binds to á2ä subunit of voltage-dependent Ca2+ channels which results in reduction of neurotransmitter release and hence a decrease in neuronal hyperexcitability3,4. Pregabalin is several times more potent than the gabapentin. It is rapidly absorbed orally, achieves peak plasma levels within 30 min to 2 h5. Pregabalin has fewer side effects, with the most common adverse events being dizziness and somnolence. Any visceral irritation causes release of excitatory neurotransmitters which causes pain6. Spinal anaesthesia is the common anaesthesia in which the gynecological procedures are performed.
The main objective of our study is to find whether preoperative pregabalin has any effect in postoperative analgesic requirement in patients undergoing hysterectomy under spinal anaesthesia.
PATIENTS AND METHODS
After getting clearance from ethical committee from our institution this randomized, double-blind, placebo-controlled trial was conducted in 150 patients undergoing hysterectomy under spinal anaesthesia between janauary 2009 and october 2009 with ASA Grade 1 and 2. The exclusion criteria were Patient refusal for consent, Coagulapathy and bleeding diasthesis, Anticoagulant therapy, Spinal deformity, raised intracranial pressure, Local sepsis.
Using a computer-derived random number sequence, 150 women's were allocated by means of sealed opaque envelopes into three groups,
Group I (P0) control group
Patient receiving 0.5% hyperbaric bupivacaine 0.3mgkg-1intrathecally.
Group II (P150)
Patient receiving 0.5% hyperbaric bupivacaine 0.3 mg kg-1 intrathecally + oral pregabalin 150mg one hour before surgery.
Group III (P300)
Patient receiving 0.5% hyperbaric bupivacaine 0.3mg kg-1 intrathecally + oral pregabalin 300mg one hour before surgery.
VAS (Visual analogue scale) for anxiety was explained to the patient at the pre-operative visit itself.
This is a 100 mm long scale on which the patients are asked to make a mark across the scale to indicate how she is feeling about undergoing surgery and anaesthesia. A baseline score was recorded at the preoperative visit. 60 minutes after premedication.
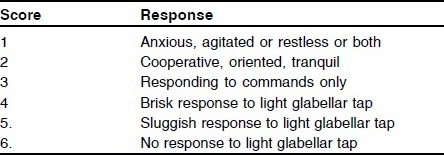
Scoring of sedation was done using Ramsay sedation scale:
All patients were taken inside the operation theatre after thorough preoperative assesment and intravenous cannula was applied and preloaded with 15 ml kg-1 of ringer's solution. All standard monitors were applied. before anaesthesia, scoring on the visual analogue scale (VAS) for anxiety was done by the patient for the second time All patients received spinal anaesthesia with 0.5% hyperbaric bupivacaine 0.3mg kg-1 through L1-L2 interspace after aseptic precautions in lateral position.
The following parameters were measured: -
Demographic details such as age, weight, height.
Mean Arterial blood pressure every two minutes for first 10 minutes and every 10 minutes for upto one hour and the lowest reading was noted.
Heart rate to find out the lowest reading, recorded in similar manner as blood pressure
Time for requirement for first rescue analgesia
Any adverse events.
Patient satisfaction regarding pain relief was noted as,
In the event of any complication standard protocols was followed. The patients were followed for first 24 hours.
RESULTS
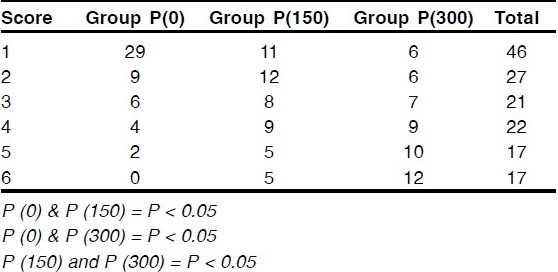
A total of 174 patients were assessed for eligibility from January 2009 to October 2009, out of which 150 subjects received study medication after randomization. There was no substantial difference among the groups with regard to age, weight, and height (Table 1). VAS score for anxiety showed that there was significant reduction in anxiety in groups P (150) and P (300) than placebo group P (0) during intraoperative and postoperative period than preoperative period. There was no significant difference between groups P (150) and P (300) (Table 2). On comparing sedation score there was significant sedation seen in groups P (150) and P (300) than placebo group P (0). Group P (300) showed more sedation score than P (150) (Table 3).
Table 1.
Demographic detail
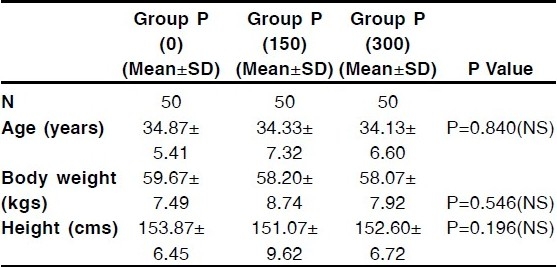
Table 2.
Comparison of vas score for anxiety
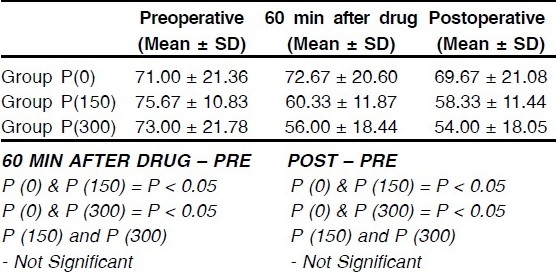
Table 3.
Comparison of sedation score
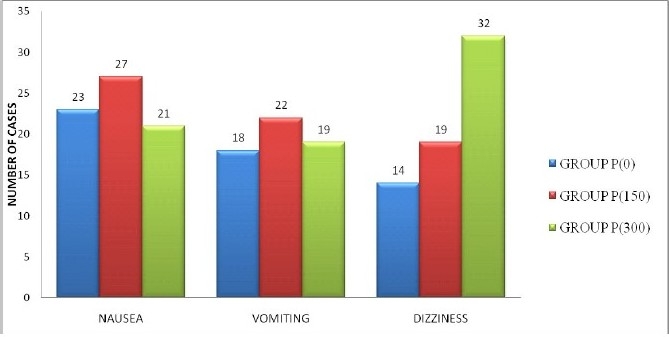
Comparison of time required for first rescue analgesia in group P (300) was202.42±6.77 and in group P (150) was176.38±4.80on average, group P (0) was131.38±5.15 on an average, these showed significant difference between the groups (Table 4). Lowest mean blood pressure (MBP) showed that there was significant reduction in MBP in groups P (150) and P (300) than placebo group P (0) during intraoperative and postoperative period than preoperative period. There was no significant difference between groups P (150) and P (300) (Table 5). Lowest pulse rate showed that there was significant reduction in groups P (150) and P (300) than placebo group P (0) during intraoperative and postoperative period than preoperative period. There was no significant difference between groups P (150) and P (300) (Table 6). There was no significant difference in nausea and vomiting between all three groups. Dizziness was 44.44% in group P (300), 36.11% in group P (150), and 19.44% in group P (0) which showed significant increase in dizziness in pregabalin group (Table 7). Patient satisfaction was better in P (300) group than other two groups (Table 8).
Table 4.
Time required for first rescue analgesia
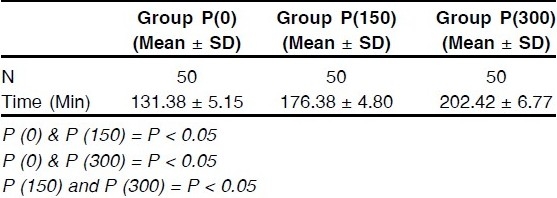
Table 5.
Comparison of mean blood pressure
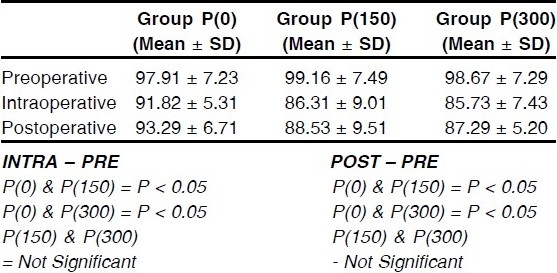
Table 6.
Comparison of lowest pulse rate
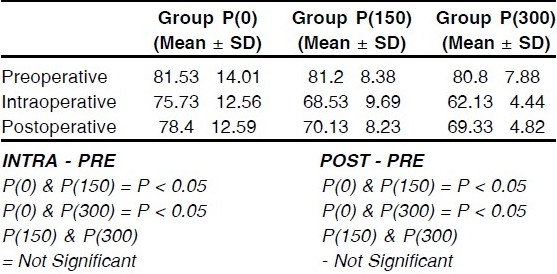
Table 7.
Complications
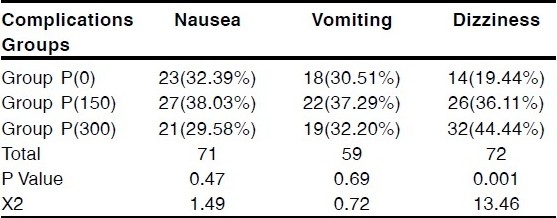
Table 8.
Patient satisfaction
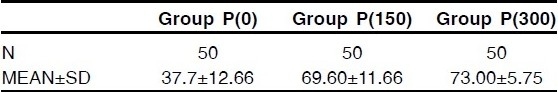
Figure 1.
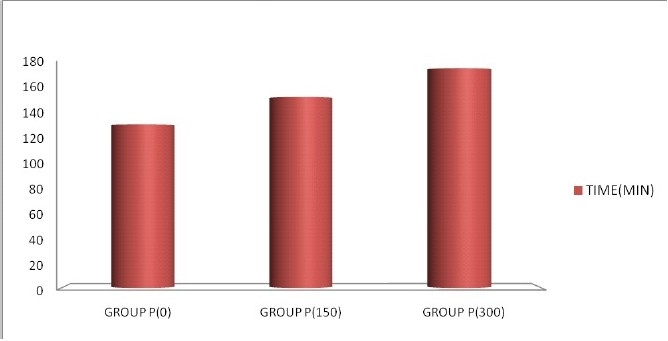
Time required for first rescue analgesia
Figure 2.
Complications
Figure 3.
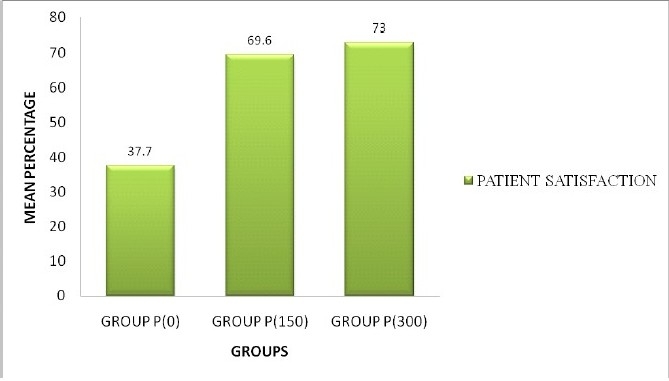
Patient satisfaction
DISCUSSION
In our study we saw that the pregabalin group showed reduced anxiety scores. In a study conducted by R. Jokela et al, showed no reduction in anxiety scores seen with 75mg and 150mg, which was conducted in laparoscopic surgery under general anesthesia7. The reduction in anxiety score showed no difference between pregabalin 150mg and pregabalin 300mg groups, but was appreciably better than the placebo group. As our study was conducted in patients with spinal anaesthesia who were conscious we were able to assess the anxiety level more appropriately. The time of rescue analgesia required by the patients was increased in pregabalin group. Pregabalin 300mg showed more effective prolongation of analgesia than pregabalin group 150mg and group P (0). Pregabalin 300mg showed prolonged analgesia after spinal anaesthesia. This prolongation in the analgesia was correlating well with the half life of pregabalin which is 4.6 hrs to 6.8 hrs8. The advantage was that along with prolongation of analgesia there was no hemodynamic instability.
Experimental models of neuropathic pain and inflammatory hyperalgesia have shown that g-aminobutyric acid analogues such as gabapentin and pregabalin have antinociceptive and antihyperalgesic properties9. Central neuronal sensitization may result in an amplification of postoperative pain10, and that preoperative administration of gabapentin, may reduce the degree of central sensitization11. Because of its absence of hepatic metabolism, it has good pharmacokinetic properties and fewer drug interactions which make it a better drug than Gabapentin12.
On comparing the complications like sedation, dizziness, nausea and vomiting, the incidences of dizziness in patients receiving pregabalin 300mg was more than those who receiving 150mg and placebo group. Incidence of the nausea and vomiting (P=0.47, and P=0.69) showed no significant difference between the groups.
A. Agarwal et al13 showed that a single dose of pregabalin 150mg was effective in reducing postoperative pain after laproscopic cholecystectomy. He also showed that 150mg has no significant complication than placebo group.
In a study conducted by Hill et al14 compared pregabalin (50 and 300 mg) to placebo and 400 mg of ibuprofen in 198 patients who had undergone elective surgery to remove one or two third molars in terms of pain relief and pain intensity. Pain relief and pain intensity were significantly better in the 300 mg pregabalin group.
In a study conducted by Wichai Ittichaikulthol MD et al15 300 mg pregabalin administered 1 hr pre-operatively before abdominal hysterectomy with/without salphingo-oophorectomy significantly reduced, VNRS pain score and improved satisfaction score at 24 hr post operatively.
In a study conducted by R. Jokela et al16 they found that 300 mg of pregabalin was more effective than pregabalin 150 mg. The incidence of dizziness, headache and blurred vision were higher in the 300 mg pregabalin group. Garaj17 reviewed the pharmacology of pregabalin and found that somnolence (29.2%) and dizziness (22.2%) were the most common side effects which were similar to the present study (dizziness/ somnolence 34.21%) which was well seen in our study.
Patient satisfaction in our study also showed good with pregabalin 300mg group (73.00±5.75) than 150mg group (69.60±11.66) and group P(0) (37.7±12.66).
The reduction in mean blood pressure and heart rate was seen in all groups, which was significant between pregabalin group and placebo group. But there was no significant difference seen between 300mg and 150mg groups. This may be due to the effect of spinal anaesthesia which was given, but further studies have to be done to evaluate this finding.
With this study, we came to know that pregabalin significantly reduced anxiety level, requirement of supplementary analgesic, than placebo group. Complications like sedation, dizziness was more with 300mg than 150mg, and patient satisfaction showed almost equal between 150 and 300mg group.
We conclude that Pregabalin 150mg would be the optimal preemptive dose for hysterectomy under spinal anaesthesia. Pregabalin being an oral drug which would be easy for the patients to take and also its prolongation of the neuraxial block helps in immediate postoperative analgesia and further reduction of other parentral analgesics. Further studies should be done to find optimal dose of pregabalin for other various surgery done under neuraxial block.
REFERENCES
- 1.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postop-erative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–40. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 2.Kehlet H, Wilmore DW. Multimodal strategies to im-prove surgical outcome. Am J Surg. 2002;183:630–41. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 3.Kavoussi R. Pregabalin: from molecule to medicine. Euro Neuropsychopharmacol. 2006;16(suppl 2):S128–33. doi: 10.1016/j.euroneuro.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Shneker BF, McAuley JW. Pregabalin: a new neuromodulator with broad therapeutic indications. Ann Pharmacother. 2005;39:2029–37. doi: 10.1345/aph.1G078. [DOI] [PubMed] [Google Scholar]
- 5.Frampton JE, Scott LJ. Pregabalin in the treatment of painful diabetic peripheral neuropathy. Drugs. 2004;64:2813–20. doi: 10.2165/00003495-200464240-00006. [DOI] [PubMed] [Google Scholar]
- 6.Feng Y, Cui M, Willis W. Gabapentin markedly reduces acetic acid-induced visceral nociception. Anesthesiology. 2003;98:729–33. doi: 10.1097/00000542-200303000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. Premedication with pregabalin 75 or 150 mg with ibuprofen to control pain after day-case gynaecological laparoscopic surgery. British Journal of Anaesthesia. 2008;100(6):834–40. doi: 10.1093/bja/aen098. [DOI] [PubMed] [Google Scholar]
- 8.Frampton JE, Foster RH. Pregabalin in the treatment of postherpetic neuralgia. Drugs. 2005;65:111–8. doi: 10.2165/00003495-200565010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Kong VK, Irwin MG. Gabapentin: a multimodal perioperative drug? Br J Anaesth. 2007;99:775–86. doi: 10.1093/bja/aem316. [DOI] [PubMed] [Google Scholar]
- 10.Wolf CJ, Chong MS. Pre-emptive analgesia treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362–79. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 11.Werner FM, Frederick M, Perkins K, Holte K, Pedersen JL, Kehlet H. Effects of gabapentin in acute inflamma-tory pain in humans. Reg Anesth Pain Med . 2001;26:322–8. doi: 10.1053/rapm.2001.25070. [DOI] [PubMed] [Google Scholar]
- 12.Shneker BF, McAuley JW. Pregabalin: a new neuromodulator with broad therapeutic indications. Ann Pharmacother. 2005;39:2029–37. doi: 10.1345/aph.1G078. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal A, Gautam S, Gupta D, Agarwal S, Singh P K, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. British Journal of Anaesthesia. 2008;101(5):700–4. doi: 10.1093/bja/aen244. [DOI] [PubMed] [Google Scholar]
- 14.Hill CM, Balkenohl M, Thomas DW, Walker R, Mathe H, Murray G. Pregabalin in patients with postoperative dental pain. Eur J Pain. 2001;5:119–24. doi: 10.1053/eujp.2001.0235. [DOI] [PubMed] [Google Scholar]
- 15.Ittichaikulthol Wichai, MD, Virankabutra Tanit, MD, Kunopart Mutita, MD, Khamhom Wachirapol, MD, Putarawuthichai Pipat, MD, Rungphet Suyawej, BN, Ittichaikulthol Wichai, MD, Virankabutra Tanit, MD, Kunopart Mutita, MD, Khamhom Wachirapol, MD, Putarawuthichai Pipat, MD, Rungphet Suyawej., BN J Med Assoc Thai. 2009;92(10):1318–23. [PubMed] [Google Scholar]
- 16.Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. A randomized controlled trial of perioperative ad-ministration of pregabalin for pain after laparoscopic hysterectomy. Pain. 2008;134:106–12. doi: 10.1016/j.pain.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Gajraj NM. Pregabalin: its pharmacology and use in pain management. Anesth Analg. 2007;105:1805–15. doi: 10.1213/01.ane.0000287643.13410.5e. [DOI] [PubMed] [Google Scholar]


