Abstract
Background:
Laryngeal mask airway is a non invasive supraglottic device which has led to a radical change in the management of modern general anaesthesia. Propofol as a single agent is unsatisfactory and to overcome problems associated with LMA insertions. In the present study, we evaluated the haemodynamic changes and laryngeal mask airway insertion conditions comparing ketamine and opioids as adjuncts to propofol.
Patients and Methods:
90 patients were randomly divided into 3 groups of 30 each. In Group PK-ketamine 0.5mg kg-1, in Group PF-fentanyl 1ug kg-1 and in Group PB - butorphanol 20ug kg-1 was given intravenously immediately before induction with propofol 2.5 mg kg-1. Jaw relaxation was assessed according to Young's criteria and the overall conditions according to modified Scheme of Lund and Stovener.
Results:
The mean total dose of propofol required in Group PK was 160.37 ± 15.75mg, in Group PF 156.22 ± 17.18 mg and in Group PB 140.08 ± 18.97 mg. The incidence of absolute jaw relaxation was highest in Group PB (93.33%) patients, intermediate in Group PF (53.33%) patients and lowest in Group PK i.e. 36.66% patients. Excellent insertion conditions were observed in 12 (40%) patients in Group PK and 13 (43.33%) patients in Group PF and in 26 (86.67%) patients in Group PB. Group PK showed more rise in systolic and diastolic blood pressure and heart rate post LMA insertion as compared to Group PF and Group PB.
Conclusion:
It is concluded that addition of butorphanol to propofol for LMA insertion provided absolute jaw relaxation and excellent insertion conditions with stable haemodynamics Side effects like coughing, gagging, lacrimation and laryngospasm were lower as compared to the other two groups.
Keywords: LMA, Butorphanol, Fentanyl, Ketamine propofol, Insertion conditions
Airway management is one of the most important skills in the field of anaesthesiology and inability to secure the airway can lead to catastrophic results.1 Laryngeal mask airway is a non invasive supraglottic device which has the advantage of being less stimulating than the tracheal intubation as visualization of cords and entry into larynx is not required.2
Inadequate depth of anaesthesia may provoke coughing, gagging and laryngospasm which may lead to adverse haemodynamic changes and increase incidence of regurgitation and aspiration.3,4 Therefore, the optimal condition for LMA insertion mandates a generous use of an anaesthetic agent for induction. Propofol, when used alone often exceeds 2.5 mg kg-1 which causes cardiorespiratory depression. Other problems associated with it was apnoea, hypotension, excessive patient movement and laryngospasm. So, propofol as a single agent is unsatisfactory and to overcome problems associated with it, a number of other co-induction drugs have been introduced.4
Since limited literature is available on Butorphanol and propofol combination for LMA insertion, in our study we have compared ketamine - propofol, fentanyl - propofol and butorphanol - propofol for best haemodynamics and laryngeal mask airway insertion conditions.
PATIENTS AND METHODS
After obtaining institutional ethics committee approval, the present study was conducted on 90 patients in the age group of 20-50 years of either sex belonging to ASA grade I and II undergoing elective short surgical procedures. Written informed consent was taken from all patients and they were randomly divided into 3 groups of 30 each as follows: GROUP PK (Propofol - Ketamine), GROUP PF (Propofol - Fentanyl) and Group PB (Propofol - Butorphanol).
Patients at the risk of aspiration (hiatus hernia, pregnancy, full stomach, intestinal ileus) and those suffering from upper respiratory tract infection.
Patients suffering from pharyngeal pathology e.g. abscess, haematoma and tissue disruption.
Low pulmonary compliance e.g. morbid obesity, bronchospasm or pulmonary oedema.
Patients undergoing oral surgery and those allergic to propofol, ketamine, fentanyl or butarphanol.
All the patients were premedicated with glycopyrrolate 0.2 mg intramuscularly 30 minutes before the surgery. After pre-oxygenation with 100% oxygen for 3 minutes, patients were given midazolam 0.04 mg kg-1 intravenously. Then they were given their assigned drugs over 10 seconds i.e. Group PK - Inj. ketamine 0.5 mg kg-1 intravenous, Group PF - Inj. Fentanyl 1 ug kg-1intravenous and Group PB - Inj. butorphanol 20 ug kg-1 intravenous
This was followed immediately by propofol 2.5 mg kg-1 intravenously over 15 seconds. If required, further increments of propofol 0.5 mg kg-1 were given every 30 seconds until loss of consciousness and loss of eyelash reflex. Insertion of LMA was performed 60 seconds after injection of propofol by a blinded investigator.
Patients were given additional bolus dose of propofol 0.5 mg kg-1 on first unsuccessful attempt. Insertion was tried to a maximum of 3 attempts. However, the conditions during laryngeal mask airway insertion were only graded at the first attempt. Patients were kept on spontaneous respiration. Anaesthesia was maintained with 0.75 to 1% of Halothane, 60% and O2 40%. At the completion of surgery N2O and halothane was stopped and LMA was removed. Any other observations like lacrimation, vomiting or injury was noted. 100% oxygen was continued via face mask till recovery. Heart rate, NIBP and SPO2 were recorded pre-induction and immediately after induction of anaesthesia and later at one minute, three minutes, five minutes, ten minutes, every fifteen minutes intervals till the end of the surgery. ECG monitoring was done to record any arrhythmias.
Following parameters were noted during insertion of LMA
Top up dose of propofol required or not, total dose of propofol required.
No. of attempts, presence of apnoea (>30 seconds) and its duration.
Coughing and Gagging.
Laryngospasm and Movements were assessed on three point scale (nil, mild, severe).
Jaw relaxation was assessed according to Young's5 criteria.
Absolutely relaxed with no muscle tone: 1
Moderately relaxed with some muscle tone: 2
Poorly relaxed with full muscle tone : 3
The overall conditions according to modified Scheme of Lund and Stovener.6
Excellent: No gagging or coughing, no patient movement or laryngospasm
Good: Mild to moderate gagging, coughing or patient movement with no laryngospasm.
Poor: Moderate to severe gagging, coughing or patient'ss movement with no laryngospasm.
Unacceptable: Severe gagging, coughing or patient movement or laryngospasm.
The data from the present study was systematically collected, compiled and statistically analysed to draw relevant conclusions. The above mentioned parameters and patient's characteristics were compared using Chi-square test and ANOVA test for statistical analysis and p-value (p < .05 ) was taken as significant.
RESULTS
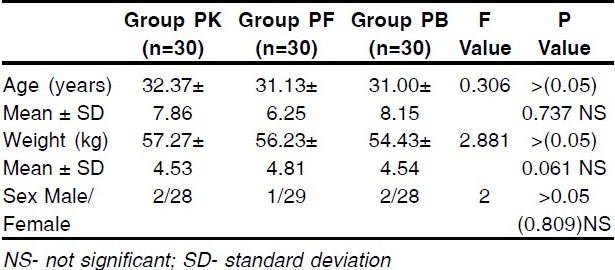
90 patients were enrolled into the study and 30 patients were randomized into each group. There was no difference in the demographic data of the groups. (Table 1)
Table 1.
Showing Demographic Data
The mean total dose of propofol required in Group PK was 160.37 ± 15.75mg, in Group PF 156.22 ± 17.18 mg and in Group PB 140.08 ± 18.97 mg. The number of patients requiring top up dose of propofol in Group PK were 18 (60%), in Group PF 17 (56.67%) and in Group PB 4 (13.33%).
Post induction, Group PK showed lesser fall in SBP and DBP as compared to Group PF and Group PB. The difference in the mean post induction SBP and DBP between Group PK and PF as well as between Group PK and PB was statistically significant but between Group PF and PB it was statistically insignificant. Post -induction, the mean heart rate (HR) increase was greatest in PK group. Group PK showed greater rise in systolic and diastolic blood pressure and heart rate after LMA insertion as compared to Group PF and Group PB. (FIG 1,2). The difference in mean SpO2 in the three groups post LMA insertion was statistically insignificant.
Figure 1.
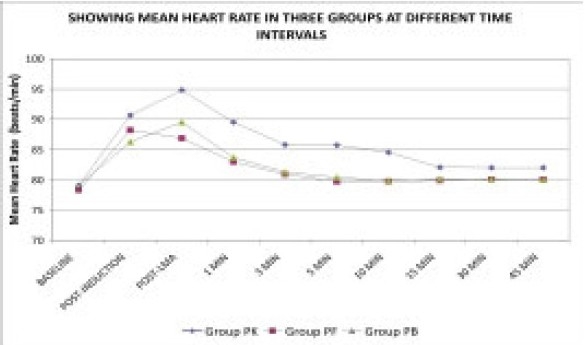
Showing Mean Heart Rate in three groups at different time intervals
Figure 2.
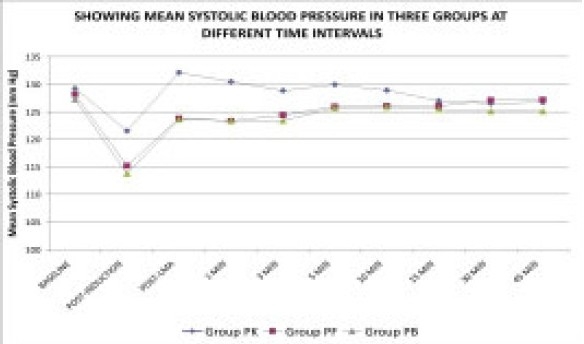
Showing Mean Systolic Blood Pressure in three groups at different time intervals
The number of patients showing apnoea was highest in Group PF 18 (60%). In Group PK 8 (26.67%) patients and in Group PB 9 (30%) patients experienced apnoea. The mean duration of apnoea was again highest in Group PF 61.67 ± 13.28 seconds, in Group PK it was 33.75 ± 1.58 seconds and in Group PB 41.22 ± 3.99 seconds. The Group PB showed significantly lower number of attempts as compared to Group PF and PB 60% patients in Group PK, 43.33% patients in Group PF and 10% patients in Group PB were inserted LMA in second attempt.
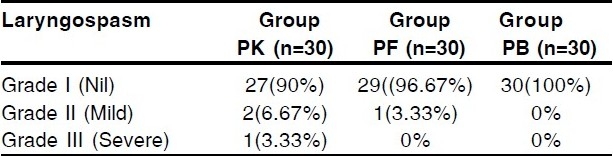
The incidence of absolute jaw relaxation was highest in Group PB 28 (93.33%) patients, intermediate in Group PF 16 (53.33%) patients and lowest in Group PK 11 (36.66%) patients, (FIG 3). It was observed that 11 (36.66%) patients in Group PK, 13 (43.33%) patients in Group PF and 4(13.33%) patients in Group PB had mild coughing and gagging. Three (10%) patients in Group PK, one (3.33%) patient in Group PF and none of the patients in Group PB had severe coughing and gagging (Table 2). Mild laryngospasm was observed in two patients (6.67%) in Group PK and one patient (3.33%) in Group PF and in no patient in Group PB. Severe laryngospasm was seen in one patient (3.33%) in Group PK (Table 3).
Figure 3.
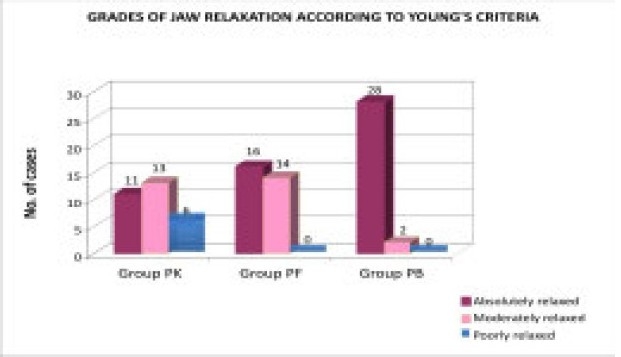
Grades of Jaw Relaxation according to younh's criteria
Table 2.
Coughing and gagging
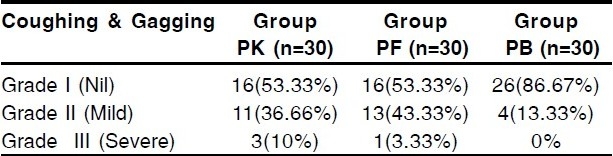
Table 3.
Showing incidence of laryngospasm
Mild movement was seen in 50% in Group PK, 40% in Group PF and 10% in Group PB (Table 4). Lacrimation was seen in four patients in Group PK and two each in Group PF and PB (Table 5). Excellent insertion conditions were observed in 12 (40%) patients in Group PK and 13 (43.33%) patients in Group PF and in 26 (86.67%) patients in Group PB. Unacceptable insertion conditions were observed in three patients (10%) in Group PK and one patient (3.33%) in Group PF (FIG 4).
Table 4.
Showing incidence of Movement
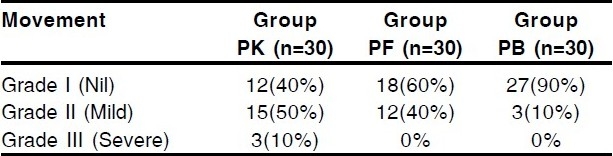
Table 5.
Showing incidence of Lacrimation
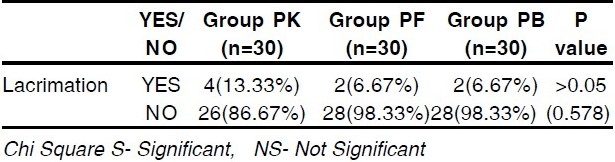
Figure 4.
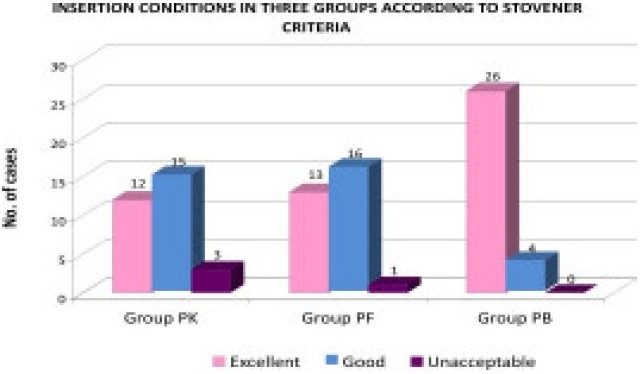
Insertion condition in three groups according to stovener criteria
DISCUSSION
LMA insertion has been revolutionized with the development of induction agents like propofol which depresses pharyngeal and laryngeal reflexes. To reduce pharyngeal and laryngeal reflexes higher doses of propofol are used which cause cardiac depression,7 so to reduce its adverse cardiorespiratory depressant effects a number of other co-induction drugs were introduced among which we compared butorphanol, fentanyl and ketamine.
In our study too, the propofol requirement was significantly less in butorphanol group (140.08 ± 18.97 mg) as compared to fentanyl group (156.22 ± 17.18 mg). Supporting our study, the mean dose of thiopentone required in study conducted by Chari P et al7 was significantly less in butorphanol group as compared to fentanyl group. They also found significantly less apnoea time in butorphanol group (33.60 seconds) as compared to fentanyl group (56.12 seconds) as shown by our results. The slightly longer duration of apnoea in our study may be due to premedication with midazolam which we used in our study whereas in the above study no premedication was given and it is a well known fact that benzodiazepines enhance the respiratory depressant effects of opioids.
Lower incidence of apnoea in butorphanol may be because of limited respiratory depression of butorphanol due to receptor specificity and mu antagonism.
Cheam EWS and Chui PT found that although fentanyl improves conditions during laryngeal mask airway insertion, it also prolongs the duration of apnea.8
In our study, the incidence of absolute jaw relaxation was highest in Group PB 28 (93.33%), intermediate in Group PF 16 (53.33%) and lowest in Group PK 11 patients (36.66%). Our results are consistent with the study conducted by Pramila Chari and Babita Ghai7 in which they compared jaw relaxation on 3 point scale for LMA insertion. Their results showed that butorphanol - thiopentone group (92.30%) had significantly higher incidence of full jaw relaxation as compared to fentanyl - thiopentone group (67.30%). (p value 0.001).
Bahk J et al had compared various doses of propofol and ketamine with lidocaine spray for LMA insertion. They had experienced lesser degree of jaw relaxation with ketamine doses lower than 3 mg kg-1.9
The Group PB showed significantly lower number of attempts as compared to Group PK and Group PF. This may be because of better jaw relaxation in the butorphanol group.
The higher incidence of coughing and gagging in the ketamine group in our study may be because of its property to increase airway reflexes and hence inappropriate for LMA insertion.
The higher incidence of coughing in the fentanyl group may be due to fact that bolus injections of intravenous fentanyl commonly induce patient coughing. In a study conducted by Wong CM et al10 higher doses of fentanyl were associated with a notable increase in the incidence of coughing. We observed lower incidence of coughing gagging in butorphanol group as compared to fentanyl group. This is probably because of the antitussive action of butorphanol.
Excellent insertion conditions were observed in butorphanol group as compared to fentanyl and ketamine group. Our results are consistent with the results of Chari P, et al7 who have found statistically significant difference in the ease of insertion of LMA in the thiopentone - butorphanol group and thiopentone - fentanyl group. Best insertion conditions were seen in 92.30% of butorphanol group and 74.15% in fentanyl group. Better insertion conditions in the butorphanol group are due to better jaw relaxation and easy insertion, lesser incidence of coughing and gagging.
Wong CM et al10 have studied 0.5, 1.0, 1.5 and 2.0 ug kg-1 fentanyl with 2.5 mg kg-1 propofol for LMA insertion. Their results showed that a standard fentanyl dose of 1 ug kg-1 co-administered with propofol 2.5 mg kg-1, provided optimal conditions in 65% of cases only.
Group PK showed more rise in systolic and diastolic blood pressure post LMA insertion as compared to Group PF and Group PB which is explained by the indirect action via the sympathomimetic effect of ketamine. Our results are consistent with the study done by Goh PK et al11 in which ketamine showed higher mean arterial pressure and heart rate throughout the study period as compared to the fentanyl group.
Mishra LD et al12 noted a significant fall in heart rate following midazolam and butorphanol. We did not observe bradycardia in our patients probably because we had used anticholinergic in premedication which was not used in their study.
To conclude, the addition of butorphanol to Propofol for LMA insertion provides absolute jaw relaxation and excellent insertion conditions with stable haemodynamics Side effects like coughing, gagging, lacrimation and laryngospasm were lower as compared to the other two groups. So, Butorphanol is a good adjuvant with propofol for LMA insertion.
Footnotes
Authors disclosure Authors have no conflict of interest and financial considerations.
REFERENCES
- 1.Brimcombe JR, Berry AM. The Laryngeal Mask Airway. In: The Difficult Airway I. Anesthesiol Clin North America. 1995;13(2):411–37. [Google Scholar]
- 2.Lamb K, James MF, Janicke PK. LMA for intra-ocular surgery.Effects on intra-ocular pressure and stress responses. Br J Anaesth. 1992;69:143–47. doi: 10.1093/bja/69.2.143. [DOI] [PubMed] [Google Scholar]
- 3.Yoshino A, Hashimoto Y, Hirashima J. Low dose Succinylcholine facilitates airway insertion during Thio-pental anaesthesia. Br J Anaesth. 1999;83:279–83. doi: 10.1093/bja/83.2.279. [DOI] [PubMed] [Google Scholar]
- 4.Salem WT. Comparison of midazolam and mini - dose Succinyl choline to aid LMA insertion during propofol anaesthesia. J Egypt Natl Canc Inst. 2000;12(1):65–69. [Google Scholar]
- 5.Young HAS, Clark RSJ, Dunder JW. Intubating condition with Ah8165 and suxamethonium. Anaesthesia. 1975;30:30–33. doi: 10.1111/j.1365-2044.1975.tb00791.x. [DOI] [PubMed] [Google Scholar]
- 6.Lund I, Stovener J. Dose responses curves for tubocurarine; alcuronium and pancuronium. Acta Anaesthesiol Scand. 1970;37:238–42. doi: 10.1111/j.1399-6576.1970.tb00916.x. [DOI] [PubMed] [Google Scholar]
- 7.Chari P, Ghai B. Comparison of butorphanol-thiopentone versus fentanyl-thiopentone for LMA insertion. J Clin Anaesth. 2006;18(1):8–11. doi: 10.1016/j.jclinane.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Cheam EWS, Chui PT. Randomised double - blind comparison of fentanyl, mivacurium or placebo to facilitate laryngeal mask airway insertion. Anaesthesia. 2000;55:323–26. doi: 10.1046/j.1365-2044.2000.01214.x. [DOI] [PubMed] [Google Scholar]
- 9.Bahk J, Sung J, Jang I. A comparison of ketamine and lidocaine spray with propofol for insertion of LMA in children. Anesth Analg. 2002;95:1586–89. doi: 10.1097/00000539-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Wong CM, Critchley LA, Lee A. Fentanyl dose response curves when inserting the LMA Classic Laryngeal mask airway. Anaesthesia. 2007;62(7):654–60. doi: 10.1111/j.1365-2044.2007.05057.x. [DOI] [PubMed] [Google Scholar]
- 11.Goh PK, Chiu CL, Wang CY, et al. Randomized double blind comparison of ketamine - propofol, fentanyl - propofol and propofol - saline on haemodynamics and laryngeal mask airway insertion conditions. Anesth Intensive Care. 2005;33(2):223–28. doi: 10.1177/0310057X0503300211. [DOI] [PubMed] [Google Scholar]
- 12.Mishra LD, Rajkumar N, Singh SN, et al. A comparative study of propofol and isoflurane using butorphanol in neurosurgery. Indian J Anaesth. 2009;53(3):324–29. [PMC free article] [PubMed] [Google Scholar]


