Abstract
Background:
To compare the effects of addition of Clonidine (60 μg) to Epidural Bupivacaine (0.125%) for labour analgesia, with regard to duration of analgesia, duration of labour, ambulation, incidence of instrumentation and caesarean section, foetal outcome, patient satisfaction and side effects.
Patients & Methods:
On demand, epidural labour analgesia was given to 50 nulliparous healthy term parturients (cephalic presentation), divided in two groups randomly. Group I received bupivacaine (0.125%) alone, whereas Group II received bupivacaine (0.125%) along with Clonidine (60 μg). 10 ml of 0.125% bupivacaine was injected as first dose and further doses titrated with patient relief (Numerical Rating Scale <3). Top ups were given whenever Numerical Rating Scale went above 5.
Results:
There was statistically significant prolongation of duration of analgesia in Group II, with no difference in duration of labour, ambulation, incidence of instrumentation and caesarean section or foetal outcome. Also clonidine gave dose sparing effect to bupivacaine and there was better patient satisfaction without any significant side effects in Group II.
Conclusion:
Clonidine is a useful adjunct to bupivacaine for epidural labour analgesia and can be considered as alternative to opioids.
Keywords: Epidural, Labour analgesia, Bupivacaine, Clonidine
Labour pains are one of the most distressing pain a human being may have to bear; there is no other circumstance where it is considered acceptable for a person to experience such severe pain, amenable to safe intervention, while under a physician's care. Hence option of labour analgesia should be given to all pregnant females”.1
Regional Epidural block is the most commonly used method of analgesia during child birth in western countries, and the trend for same is rising in India too. The mainstay of block lies in providing maximum analgesia with minimum motor block as ambulation of parturient is associated with better establishment and progression of active labour.2,3
For the development of ambulatory labour analgesia, studies are being continuously undertaken using less concentrated local anaesthetic agents with or without adjuncts. Lipophilic opioids like fentanyl and sufentanil are being used in majority of the institutions with good results. But some side effects can occur with the use of opioids like sedation, pruritis, lower apgar scores and shivering, etc.4,5
Clonidine is a α2-adrenergic agonist that produces analgesia via a non-opioid mechanism, and the combination of epidural clonidine with bupivacaine for labor analgesia has been previously studied.6–11 However, there is concern about its hemodynamic effects (maternal hypotension and bradycardia) and its potential consequences on uteroplacental flow, in addition to maternal sedative effects.
We undertook this study to compare the effects of addition of Clonidine (60 μg) to Epidural Bupivacaine (0.125%) for labour analgesia, with regard to duration of analgesia, duration of labour, ambulation, incidence of instrumentation and caesarean section, foetal outcome, patient satisfaction and side effects.
PATIENTS AND METHODS
Approval from the ethical committee and well informed consent from all the patients were taken to carry out the study. On demand, epidural labour analgesia was given to 50 nulliparous, healthy (ASA I), term parturients (cephalic presentation) presenting with labour pains at 3 cm cervical dilatation. The patients were excluded on criteria of general epidural block contraindications and obstetric causes like cephalo-pelvic disproportion, preeclampsia, diabetes and multiple pregnancy.
The patients were preloaded with 0.5 L of Ringer lactate and monitoring with NIBP, ECG and Pulse oximetery was done. Baseline pain score was taken using Numerical Rating Scale (NRS) with 0 being no pain and 10 being worst pain imaginable. Epidural catheter was inserted in L3-L4 interspace, with patient in left lateral position using 18 G Tuohy's needle. The catheter was inserted cephalad to keep 4 cm in epidural space. Position of the catheter was confirmed by negative aspiration and by injecting 15μg adrenaline through the catheter. Lignocaine was not used as it can give false results due to its own action on motor blockade in test dose 12.
The patients were divided randomly by computer generated randomization into two groups:
Group I received 10 ml of bupivacaine (0.125%) alone, whereas Group II received 10 ml bupivacaine (0.125%) along with Clonidine 60 μg through the catheter using all aseptic precautions. The doses were given in graded fashion, while checking for intrathecal response. Patients were monitored for blood pressure (every 5 minutes for 30 minutes from drug administration and then every 15 minutes) and heart rate continuously and foetal wellbeing was assured by cardiotocogram.
Onset of analgesia was defined as the time taken to decrease NRS by two levels. If the patient did not reach NRS = 3 by first dose, they were administered repeat dose consisting of 3-5 ml of 0.125% bupivacaine in both the groups after waiting for 15 minutes.
Duration of analgesia was defined as time taken when top up was needed, that is when NRS went above 5. Top up consisted of 5-7 ml 0.125% bupivacaine, then 3-5 ml after 15 minutes titrated to patient satisfaction (NRS = 3). Total volume of drug needed to each patient was noted.
Ambulation was checked while taking all precautions. It was graded into three: I-could walk herself, but with attendant holding arm, II-could walk with difficulty, leaning on the attendant, III- could not walk at all.
Duration of labour was checked: (I) from 3 cm (insertion of catheter) to full dilatation, (II) -second stage.
Need for instrumentation (forceps delivery or ventouse) as well as incidence of caesarean section was noted. Expulsive force was assessed by obstetrician as: I – Good, II – fair, III – poor. Foetal outcome was assessed by Apgar at 1 and 5 minutes.
Patient satisfaction was graded on a scale of 0 to 10 after delivery. Side effects, if any were noted with respect to hypotension (more than 20 % decrease in systolic blood pressure), bradycardia (heart rate < 50 bpm), need for urinary catheterization, sedation (said to be present if no response on normal verbal commands), respiratory depression and nausea and vomiting.
RESULTS
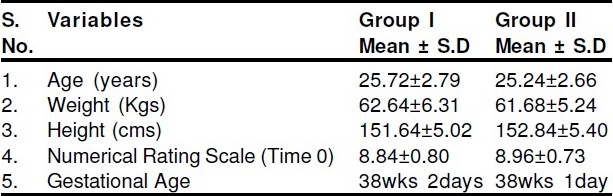
The Demographic data was statistically similar in both the groups (Table 1).
Table 1.
Demographic Data
There was statistically significant difference in: dose required to bring NRS = 3 (lower in Group II), NRS at 30 minutes (lower in Group II), duration of analgesia (higher in Group II), total dose required (lower in group II) and there was significantly better patient satisfaction in group II. Rest all the variables were similar statistically (Table 2). Also there was no statistically significant difference in ability to ambulate, expulsive force (as assessed by obstetrician) and mode of delivery (Table 3 & 4). The results were compared using SPSS professional software.
Table 2.
Results
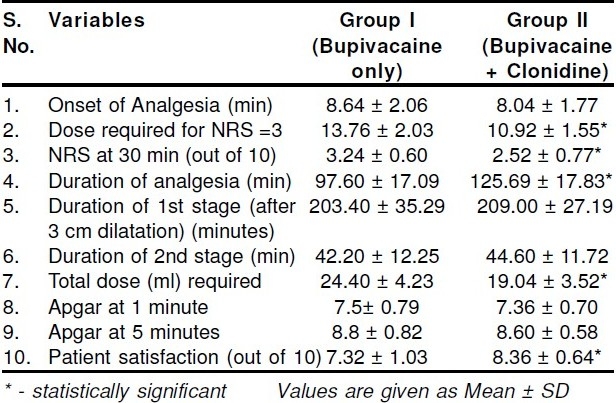
Table 3.
Ambulation*
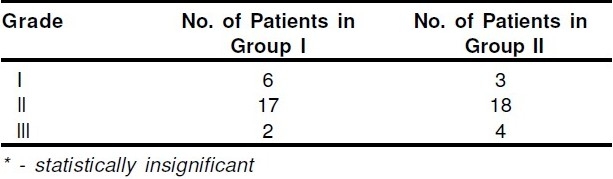
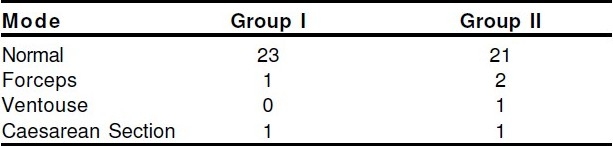
Table 4.
Mode of delivery
DISCUSSION
Epidural analgesia is the most efficient and most used method of providing pain relief during child birth. It is important that least amount of local anaesthetic agents with minimum concentrations are used, so that there is minimal motor blockade. Ambulation during labour as well as good expulsive force during second stage is important for good foetal outcomes.2,3 To provide this either low concentration of local anaesthetic agents are used or other agents (usually lipophilic opioids) are added.
We have used 0.125% bupivacaine, as 0.0625% concentration used alone produces inadequate analgesia & requires large volume & 0.25% concent-ration is associated with significant motor blockade.13,14
Clonidine is a α2 receptor agonist, which has been shown to have local sparing and analgesic effects, thus prolonging duration of analgesia by local anaesthetic agents.6–11 We used clonidine as a bolus of 60 μg because smaller doses (30 μg) have been shown not to improve analgesia significantly11, whereas larger doses (150 μg as bolus or in repeated doses) have resulted in maternal bradycardia7,8, decreased fetal heart rate variability, increased late decelerations7, and maternal sedation (120 μg).16
Onset of analgesia in both the groups was similar, which contradicts study by Landau R and coworkers17 where addition of clonidine lead to earlier onset of analgesia with ropivacaine, but their definition of ′onset′ was till maximum targeted pain relief. Onset in our study (NRS levels decreasing by two levels) is determined probably by bupivacaine volume and concentration. No change in onset times were also noted in other studies.7,9,16
Clonidine decreases the dose requirement to provide NRS = 3 scores and also gives better NRS scores at 30 minutes from the time of injection This result goes with the analgesic and local anaesthetic sparing properties of clonidine.6–11 Similar results were also found in other studies using clonidine with local anaesthetics for labour analgesia.8,9,17,18 Kizilarsalaran S and coworkers even found clonidine to increase the duration of analgesia more than fentanyl, when both were combined with bupivacaine.19
Duration of analgesia was significantly prolonged in group II (126 vs 97 minutes), due to same properties. Also total amount of bupivacaine required is significantly reduced due to addition of clonidine. These are similar to other studies in different blocks20–23 as well as in epidural labour analgesia.8,9 Clonidine 120 μg, in fact has been found to give similar pain relief scores as with 50 μg fentanyl, combined with bupivacaine.6
Addition of clonidine to bupivacaine did not affect the duration of labour, i.e. it remains similar to labour analgesia with bupivacaine alone, in consistence with other studies.24,25 This result is against the study conducted by Cigarini I and others, who found that addition of clonidine to bupivacaine increases the duration of labour. This may be due to higher dose of clonidine used in their study (75 μg).8
Ambulation has been found to be associated with good establishment and progression of labour.2,3 The ability to ambulate was statistically similar in both the groups. However, number of patients with inability to walk at all (grade III) was more in clonidine group, whereas number of patients walking without leaning (grade I) was more in group I (Table 3). We also found that there was no difference in expulsive force in either group, with the result that duration of 2nd stage and mode of delivery remained statistically similar, thus indirectly negating major motor effects of clonidine. Other studies using clonidine with local anaesthetic agents have given varied results with respect to motor block, from increasing it significantly25 to decreasing it due to local anaesthetic sparing effect.17 Further studies should be undertaken to check its motor effects.
Neonatal outcome was similar with regards to Apgar at 1 and 5 minutes in both the groups. It is consistent to findings in other studies.17,19 There was no statistically significant side effects in the clonidine group, though there was one incidence of hypotension and one of sedation in clonidine group, while none in group I. Haemodynamic effects like hypotension and bradycardia as well as sedation has been shown to be associated with higher doses of clonidine.7,8,16,17 Difficulty in voiding was not increased by clonidine.
There was higher patient satisfaction scores in group II (8.36 vs 7.32 out of 10), which is expected as there was lower NRS scores and longer duration of analgesia due to clonidine. This was also found in other studies.8,9,17
Hence, clonidine (60 μg) can be considered a useful adjunct in labour analgesia with bupivacaine as it provides longer and better analgesia with local anaesthetic sparing effect without any significant side effects, but large scale studies are indicated before strong recommendation for its routine use in epidural labour analgesia.
REFERENCES
- 1.Vincent RD, Chestnut DH. Epidural Analgesia during labour. American family Physician. 1998;58:8–12. [PubMed] [Google Scholar]
- 2.Nageotte MP, Larson D, Rumney PJ, et al. Epidural analgesia compared with combined spinal-epidu-ral analgesia during labour in nulliparous women. N Eng J Med. 1997;337:1715–9. doi: 10.1056/NEJM199712113372402. [DOI] [PubMed] [Google Scholar]
- 3.Albers LL, Anderson D, Cragin L, et al. The relation-ship of ambulation in labour to operative delivery. J Nurse Midwifery. 1997;42:4–8. doi: 10.1016/s0091-2182(96)00100-0. [DOI] [PubMed] [Google Scholar]
- 4.Olofsson C, Ekblom A, Ekman-Ordeberg G, Irestedt L. Obstetric outcome following epidural analgesia with bupivacaine-adrenaline 0.25% or bupivacaine 0.125% with sufentanil: a prospective randomized controlled study in 1000 parturients. Acta Anaesthesiol Scand. 1998;42:284–92. doi: 10.1111/j.1399-6576.1998.tb04918.x. [DOI] [PubMed] [Google Scholar]
- 5.Murphy JD, Henderson K, Bowden MI, Lewis M, Cooper G M. Bupivacaine versus bupivacaine plus fentanyl for epidural analgesia: effect on maternal satisfaction. BMJ. 1991;302:564–7. doi: 10.1136/bmj.302.6776.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buggy DJ, MacDowell C. Extradural analgesia with clonidine and fentanyl compared with 0.25% bupivacaine in the first stage of labour. Br J Anaesth. 1996;76:319–21. doi: 10.1093/bja/76.2.319. [DOI] [PubMed] [Google Scholar]
- 7.Chassard D, Mathon L, Dailler F, et al. Extradural clonidine combined with sufentanil and 0.0625% bupivacaine for analgesia in labour. Br J Anaesth. 1996;77:458–62. doi: 10.1093/bja/77.4.458. [DOI] [PubMed] [Google Scholar]
- 8.Cigarini I, Kaba A, Bonnet F, et al. Epidural clonidine combined with bupivacaine for analgesia in labor: effects on mother and neonate. Reg Anesth. 1995;20:113–20. [PubMed] [Google Scholar]
- 9.Claes B, Soetens M, Van Zundert A, Datta S. Clonidine added to bupivacaine-epinephrine-sufentanil improves epidural analgesia during child-birth. Reg Anesth Pain Med. 1998;23:540–7. doi: 10.1016/s1098-7339(98)90078-5. [DOI] [PubMed] [Google Scholar]
- 10.Eisenach JC, Castro MI, Dewan DM, Rose JC. Epi-dural clonidine analgesia in obstetrics: sheep stud-ies. Anesthesiology. 1989;70:51–6. doi: 10.1097/00000542-198901000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Le Polain B, De Kock M, Scholtes JL, Van Lierde M. Clonidine combined with sufentanil and bupivacaine with adrenaline for obstetric analgesia. Br J Anaesth. 1993;71:657–60. doi: 10.1093/bja/71.5.657. [DOI] [PubMed] [Google Scholar]
- 12.Cohen ES, Yeh JY, Edward T, Riley T, Vogel TM. Walking with Labor Epidural Analgesia.Impact of Bupivacaine Concentration & a Lidocaine - Epineph- rine Test Dose. Anesthesiology. 2000;92:387–92. doi: 10.1097/00000542-200002000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Mantha S, Arora MK, Gode GR, Kaul HL. Low concentration bupivacaine for extradural analgesia for labour: comparison of 0.125 percent and 0.25 percent bupivacaine. J Anaesth Clin Pharmacol. 1991;7:177–83. [Google Scholar]
- 14.Capogna G, et al. Minimum analgesic concentration of bupivacaine increases with progression of labour. Br J Anaesth. 80(1):11–3. doi: 10.1093/bja/80.1.11. [DOI] [PubMed] [Google Scholar]
- 15.Chiari A, et al. Analgesia and haemodynamic effects of intrathecal clonidine as the sole analgesic agent during first stage labour - a dose response study. Anesthesiology. 1999;91:388–96. doi: 10.1097/00000542-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 16.O′Meara ME, Gin T. Comparison of 0.125% bupivacaine with 0.125% bupivacaine and clonidine as extradural analgesia in the first stage of labour. Br J Anaesth. 1993;71:651–6. doi: 10.1093/bja/71.5.651. [DOI] [PubMed] [Google Scholar]
- 17.Landau R. The dose sparing effect of clonidine added to ropivacaine for labour epidural analgesia. Anaesth Analg. 2002;95:728–34. doi: 10.1097/00000539-200209000-00036. [DOI] [PubMed] [Google Scholar]
- 18.Dewandre RY, et al. Impact of the addition of sufentanyl 5 ig or clonidine 75 ig on the minimum local anaesthetic concentration of ropivacaine for epidural analgesia in labour: A randomized com-parison. IJOA. 2008;17:315–21. doi: 10.1016/j.ijoa.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Kizilarsalaran S, Kivaki B, Onul U, Sagiroglu E. Epidural fentanyl – bupivacaine compared with clonidine – bupivacaine for analgesia in labour. Eur J Anaesth. 2001;17(11):692–7. doi: 10.1046/j.1365-2346.2000.00740.x. [DOI] [PubMed] [Google Scholar]
- 20.Casati A, Magistris L, Fanelli G, et al. Small-dose clonidine prolongs postoperative analgesia after sci-atic- femoral nerve block with 0.75% ropivacaine for foot surgery. Anesth Analg. 2000;91:388–92. doi: 10.1097/00000539-200008000-00029. [DOI] [PubMed] [Google Scholar]
- 21.El Saied AH, Steyn MP, Ansermino JM. Clonidine pro-longs the effect of ropivacaine for axillary brachial plexus blockade. Can J Anaesth. 2000;47:962–7. doi: 10.1007/BF03024866. [DOI] [PubMed] [Google Scholar]
- 22.De Kock M, Gautier P, Fanard L, et al. Intrathecal ropivacaine and clonidine for ambulatory knee arthroscopy: a dose-response study. Anesthesiol-ogy. 2001;94:574–8. doi: 10.1097/00000542-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 23.De Negri P, Ivani G, Visconti C, De Vivo P. How to prolong postoperative analgesia after caudal ana-esthesia with ropivacaine in children: S-ketamine versus clonidine. Paed Anaesth. 2001;11:679–83. doi: 10.1046/j.1460-9592.2001.00742.x. [DOI] [PubMed] [Google Scholar]
- 24.Parker RK, et al. Epidural clonidine added to a bupivacaine infusion increases analgesic duration in labor without adverse maternal or fetal effects. J Anesth. 2007;21(2):142–7. doi: 10.1007/s00540-006-0476-8. [DOI] [PubMed] [Google Scholar]
- 25.Giane N, et al. Labor analgesia with ropivacaine added to clonidine: a randomized clinical trial. São Paulo medical journal. 2008;126(2):102–6. doi: 10.1590/S1516-31802008000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]


