Abstract
Background:
Till date, different combinations of adjuncts with induction agents have been tried for Laryngeal Mask Airway (LMA) insertion; yet, the ideal combination that provides the best insertion conditions with minimal side effects has not been identified, particularly in children.
Patients & Methods:
Hundred paediatric ASA grade I and II patients, aged 3-12 years, were randomly allocated to receive intravenously either fentanyl 2μg kg-1 (Group F, n=50) or ketamine 0.5 mg kg-1 (Group K, n=50), before induction of anaesthesia with propofol 3.5 mg kg-1. Arterial blood pressure and heart rate were measured before induction (baseline), immediately before induction, immediately before LMA insertion, and at 1, 3 and 5 minutes after LMA insertion. Following LMA insertion, the following six subjective endpoints were graded by a blinded anaesthetist using ordinal scales graded 1 to 3: mouth opening, gagging, swallowing, head and limb movements, laryngospasm and resistance to insertion. Duration and incidence of apnoea was also recorded.
Results:
The incidence of resistance to mouth opening, resistance to LMA insertion and incidence of swallowing was not statistically significant between the two groups. Coughing/ gagging was seen in 8% patients in group K as compared to 28% patients in group K. Limb/ head movements were observed in 64% patients in the fentanyl group and in 76% patients in the ketamine group. Laryngospasm was not seen in any patient in either group. Incidence of apnoea was 80% in the fentanyl group and 50% in the ketamine group. The heart rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure were consistently higher in the ketamine group as compared to the fentanyl group.
Conclusion:
The combination of fentanyl (2μg kg-1) and propofol (3.5mg kg-1) provides better conditions for LMA insertion in children than a combination of ketamine (0.5 mg kg-1) and propofol (3.5mg kg-1).
Keywords: Ketamine: Propofol, Fentanyl: blood pressure, heart rate, laryngeal mask airway insertion
Since the introduction of Laryngeal Mask Airway (LMA) by Brain,it hasbecomean importantaddition to the anaesthetist's armamentarium for airway management.1 The insertion of LMA requires sufficient depth of anaesthesia for the jaw muscles to relax and the inserted LMA to be tolerated without undue coughing, gagging, breath holding and patient movement.1,2 A number of induction agents and adjuncts have been triedto facilitatesmooth insertion of LMA.3,4 Many studies have shown propofol to be superior to thiopentone in this respect.3,4 Although, propofol appears to provide the best conditions for LMA insertion,3,5it frequently causes apnoea and hypotension.5,6 The addition of adjuvants, such as midazolam, ketamine, low dose muscle relaxants, opioids and sevoflurane have been advocated to further improve the LMA insertion conditions.7,8 The addition of opioids have been shown to improve the insertion conditions with an overall success rate of up to85-95%.9 Unfortunatelythese medications also increase the incidence and duration of apnoea. Ketamine is well known for its airway-maintaining activity as well as for its increases in heart rate and cardiac output, which are favourable characteristics in paediatric anaesthesia.10 The addition of ketamine to propofol has been reported to produce similar conditions of LMA insertion but less prolonged apnoea than a combination of fentanyl-propofol or placebo.11 Sevoflurane added to propofol also improves the insertion but its availability is limited in our setup. Till date, different combinations of adjuncts with induction agents have been tried for LMA insertion;7,8,9 yet, the ideal combination that provides the best insertion conditions with minimal side effects has not been identified, particularly in children. The present study had been planned to comparatively evaluate the conditions for laryngeal mask airway insertion using ketamine VS fentanyl with propofol in children and to study the haemodynamic response with both the drugs.
PATIENTS & METHODS
After approval from the institution review board, 100 consecutive patients of ASA grade I and II, aged 3-12 years, scheduled to undergo elective surgery in which general anaesthesia with spontaneous breathing using an LMA was deemed most appropriate were recruited for the study. Patients at risk of aspiration, anatomical abnormalities of the airway, anticipated difficult airway, upper respiratory tract infection, history of asthma, allergy to propofol, fentanyl or ketamine, seizure disorder and neuromuscular diseases were excluded from the study.
After a thorough systemic examination, an informed consent was taken from the parents or guardians of the patients. After fasting as per the American Association of Anaesthesiologists pre-procedure fasting guidelines,12 patients were premedicated with oral midazolam (0.5mg kg-1) 30 minutes prior to injecting the test drug. Midazolam (5mg per ml) was mixed with a teaspoon of honey and administered to the patients. On arrival in the operation theatre, standard anaesthesia monitors were attached, which included non-invasive blood pressure, electrocardiogram and pulse oximetry and an intravenous access was secured. Baseline heart rate (HR), blood pressure (BP) and oxygen saturation (SpO2) were monitored and recorded. Inj. glycopyrrolate (0.005mgkg-1) was administered intravenously 5 minutes prior to injecting the test drug. Patients were randomly allocated by a computer generated random table into 2 groups, i.e., Group F- Fentanyl group (n=50) and Group K-Ketamine group (n=50)
Propofol was prepared in a 10ml syringe with 1ml of 1% preservative free lidocaine. Both fentanyl and ketamine were taken as per the calculated doses based on body weight and that volume was subsequently diluted in normal saline to make a volume of 10ml by an anaesthesiology resident not involved in the study. Inj. fentanyl in a dose of 2μg kg-1 was then given intravenously over 10 seconds to group F13 and inj. ketamine in a dose of 0.5mg kg-1 was given intravenously over 10 seconds to group K.11 Each patient was preoxygenated with 100% oxygen for 3 minutes. General anaesthesia was induced with inj. propofol (premixed with preservative free lidocaine) in the dose of 3.5mg kg-1 given over 15 seconds,14 3 minutes after the test drug, and the i.v line was flushed with 3ml normal saline.
Insertion of LMA (whose size was selected on basis of body weight) was performed 90 seconds15 after the start of propofol injection by a blinded investigator. All LMA insertions were performed by the same blinded investigator who also assessed the LMA insertion conditions using a six-variable, three point score which included resistance to mouth opening, ease of LMA insertion and patient response, i.e., swallowing, coughing/gagging, limb & head movements & laryngospasm.
Following insertion, the positioning of LMA and airway patency was checked by observing the patient's respiratory movement and the capnography or in apneic patients, by observing chest expansion and capnograph. Any malpositioned or non-functioning LMA was removed, the patient was given a further dose of propofol (1mg kg-1) and 60 seconds later a reinsertion was attempted. After 3 failed attempts at LMA insertion and lung ventilation, patient's trachea was intubated. The total number of attempts at LMA insertion were recorded.
Once the LMA was successfully inserted, patients were allowed to breathe spontaneously, if spontaneous respiration was present and adequate. Whenever apnea occurred (defined as absence of respiration for more than 30 seconds), ventilation was manually assisted via the LMA to maintain the arterial oxygen saturation above 95% until regular spontaneous respiration resumed. The presence of apnoea (absence of spontaneous respiration for more than 30 seconds) and its duration was noted. Prolonged apnoea was defined as the absence of spontaneous respiration for more than 5 minutes. Anaesthesia was maintained with 66% nitrous oxide in oxygen and 1% sevoflurane and no further data was collected.
The parameters observed were: heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), respiratory rate (RR) and oxygen saturation (SpO2). ECG and SpO2 were monitored continuously. These parameters were recorded at the following time intervals: baseline value, immediately before induction, immediately before LMA insertion, 1 minute after LMA insertion and thereafter at 3 minutes and 5 minutes. LMA insertion conditions were assessed using six variables on a 3 point scale as follows9,16:
Resistance to mouth opening - no/significant/undue force required
Resistance to insertion - easy/difficult/impossible
Swallowing - nil/slight/gross
Coughing/gagging - nil/slight/gross
Limb/head movements - nil/slight/gross
Laryngospasm- nil/partial/total
The number of attempts at LMA insertion were also noted. The summed score for LMA insertion was calculated by summing the insertion score for each patient and then totalling the score for all the patients in the group.
Statistical analysis
A pilot study done had revealed that limb and head movements were the most commonly observed patient response to LMA insertion. A power analysis indicated that with limb and head movements as the outcome variable 45 patients in each group would be required to detect a 25% difference between the two groups with an a error of 0.05 and a power of 0.8 with an effect size of 0.533. Analyses were performed using SPSS Version 10.0 (SPSS Ltd, Chicago, IL, U.S.A). Values are presented as mean (SD or range) or number (%). Hemodynamic data were analysed using 2-tailed student's t-test for intergroup comparison and paired t-test for intragroup comparison. Ordinal categorical data such as LMA insertion conditions and number of attempts were analysed with the Chi Square Test. Nominal categorical data such as gender was also analysed with the Chi Square test. A p value < 0.05 was accepted as statistically significant.
RESULTS
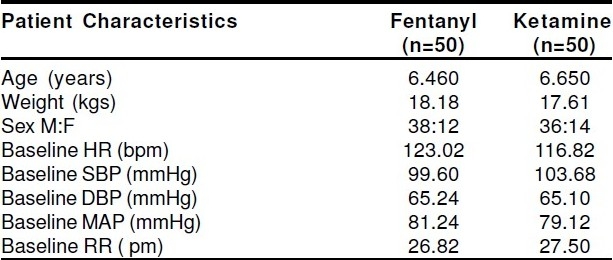
Anaesthesia and surgery were uncomplicated in all 100 patients studied. The two study groups were well matched for age, weight, gender, baseline HR, SBP, DBP MBP and RR (Table 1). The LMA was inserted in first attempt in 49/ 50 (98%) patients in the fentanyl group and in 48/50 (96%) patients in the ketamine group. This was not statistically significant (p=0.558). One patient in group F and two in group K required additional propofol for successful insertion of LMA. The SpO2 in all patients of both the groups was above 95% at all times.
Table 1.
Patient Demographics
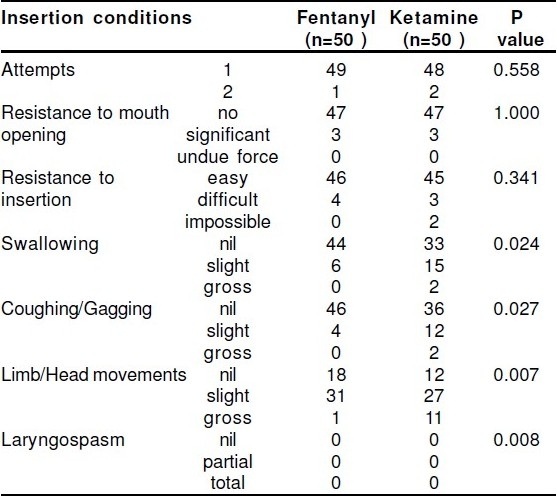
There was no difference in the incidence of resistance to mouth opening in both the groups (p=1.0). Mouth opening was not ideal in three patients in each group. Resistance to LMA insertion was seen in 4/50 (8%) patients in group F as compared to 5/50 (10%) patients in group K. The difference was not statistically significant (p=0.341). Six/fifty (12%) patients in group F had swallowing as compared to 17/50 (34%) patients in group K, which was statistically significant (p=0.024). Coughing/ gagging was seen in 4/50 (8%) patients in group F as compared to 14/50 (28%) patients in group K, the difference being significant statistically (p=0.027). Limb and head movements were observed in 32/50 (64%) patients in group F and 38/50(76%) patients in group K. This difference was highly significant (p=0.007). Laryngospasm was not seen in any patient in either group. The summed score for LMA insertion was better (50) in the fentanyl group as compared to the ketamine group (94). The difference was statistically highly significant (p=0.008). [Table 2].
Table 2.
Insertion Conditions of LMA
Statistically, a highly significant difference (p=0.002) was seen in the incidence of apnea between the two groups. Apnoea was seen in 40/50 (80%) patients in the fentanyl group and in 25/50 (50%) patients in the ketamine group. However, a slightly higher incidence of prolonged apnoea (>5 minutes) was seen in the ketamine group (14% patients) as compared to the fentanyl group (12% patients), which was statistically insignificant (p=0.255) [Table 3]. Heart rate (Fig 1), systolic blood pressure, diastolic blood pressure and mean blood pressure (Fig 2) were significantly higher in the ketamine group as compared to the fentanyl group. The difference in HR was statistically significant at 1, 3 and 5 minutes (p<0.05). The difference was statistically significant in systolic blood pressure after giving the test drug till 5 minutes after the LMA insertion between both groups. The diastolic blood pressure difference was significant between the fentanyl and ketamine group after giving the test drug, 90 seconds after propofol injection and 1 minute after the LMA insertion. The difference in mean blood pressure was statistically significant between the fentanyl and ketamine group only 90 seconds after the propofol injection. After injection of ketamine the RR was higher in group K as compared to group F, the change was statistically highly significant (p=0.000). At 1, 3 and 5 minutes the RR was higher in group K as compared to group F, the difference being statistically significant at all points (p=0.013, p=0.017 and p=0.002 respectively. (Fig 3)
Table 3.
Incidence of Apnoea
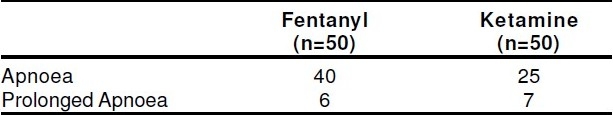
Figure 1.
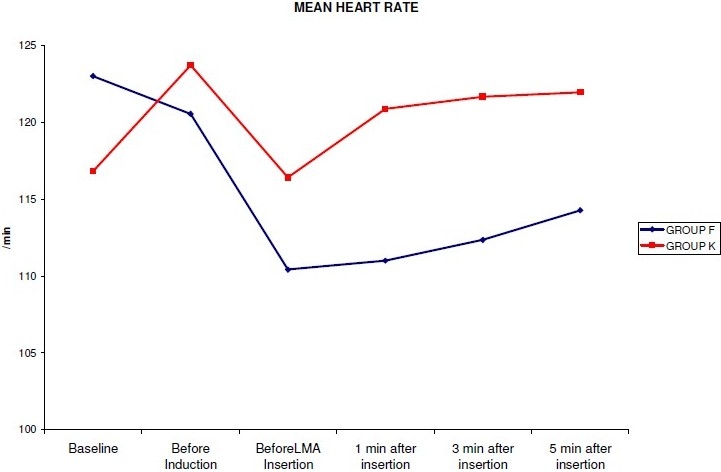
Changes in Mean Heart Rate following Induction and LMA Insertion
Figure 2.
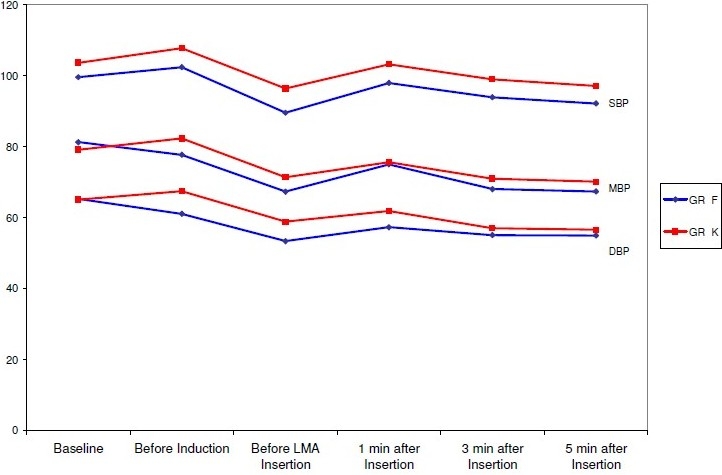
Changes in Mean SBP, Mean DBP and Mean MAP Following Induction and LMA Insertion
DISCUSSION
Smooth insertion and correct positioning of an LMA requires adequate mouth opening and sufficient depth of anaesthesia to prevent complications such as gagging, coughing, swallowing, head and limb movements and laryngospasm.1,2 Traumatic LMA insertion also increases post operative sore throat.8 Propofol is currently the induction agent of choice for LMA insertion. However when propofol is used alone it provides less than satisfactory LMA insertion conditions.4 We have shown that with a combination of fentanyl 2μg kg-1 with propofol 3.5mg kg-1 we were able to achieve satisfactory conditions for LMA insertion, significantly better than with a combination of ketamine of 0.5mg kg-1 with propofol 3.5mg kg-1.
In our study, the LMA insertion conditions were recorded using an unvalidated methodology based on a 6 variable, 3 grade score proposed by Sivalingham et al16 and Cheam EWS et al.9 We were able to use this score to assess both the ease of placement and the patient's response. We graded 4 fundamental patient responses to LMA insertion, swallowing, coughing/gagging, head and limb movements and laryngospasm. Along with this, resistance to mouth opening and LMA insertion was also graded.
Limb and head movements were the most frequent of the patient's response that we encountered in our study. Although a large number of patients in both groups showed limb and head movements, the difference in incidence between the two groups was statistically highly significant (p=0.007). The higher incidence of limb movements is probably related to the use of propofol and ketamine as both the drugs are known to cause involuntary movements.17 Previous studies have shown that for the smooth insertion and tolerance of LMA in the hypopharynx the swallowing reflex along with coughing and gagging must be suppressed.9,18,19 The difference in the incidence of swallowing (p=0.024) and coughing / gagging (p=0.027) between the two groups in our study was statistically significant. This high incidence of swallowing, coughing and gagging seen in the ketamine group is probably due to the fact that pharyngeal and laryngeal reflexes are usually preserved with ketamine.17 We observed no difference in the incidence of resistance to LMA insertion (p=0.0341) and resistance to mouth opening (p=1.0) in both the groups. In our study, the least frequent patient response observed was laryngospasm (none of the patients had any laryngospasm), though it is not uncommon for LMA insertion to cause some transient cord closure. This may be due to high initial boluses of propofol (3.5mg kg-1) given in our patients. We found that since the incidence of limb and head movements, swallowing and coughing/gagging was significantly higher in the ketamine group as compared to the fentanyl group the summed score which describes the overall LMA insertion conditions was significantly better in the fentanyl group (50) as compared to the ketamine group (94).
Although LMA insertion conditions in children have been studied previously by a few authors, we found no study comparing intravenous ketamine with fentanyl. Many different agents have been used to improve insertion conditions but with differing results. In a study20 comparing ketamine and lidocaine spray with propofol for the insertion of LMA in children, the authors observed that overall satisfactory and acceptable results in every patient were achieved only in ketamine 3.0 or 3.5 mgkg-1 subgroups and that no propofol dose was completely satisfactory; involving either apnoea or airway obstruction. The authors did not use any opioid at the time of induction. Opioids do improve the insertion conditions but have been associated with a prolonged duration of apnoea.9,21 Recently, the effects of ketamine or alfentanil administration prior to propofol anaesthesia on the ProSeal laryngeal mask airway (PLMA) insertion conditions and haemodynamic changes in children were studied.21 It was found that, compared with alfentanil 20 μg kg-1, the administration of ketamine 0.5 mgkg-1 with propofol 4 mgkg-1 preserved haemodynamic stability and reduced the time to the return of spontaneous ventilation; the conditions for insertion of the PLMA with ketamine were however similar to those found with alfentanil. Another recent study on the efficacy of ketamine and midazolam as co-induction agents with propofol for laryngeal mask insertion in children showed that, the combination of propofol with ketamine or midazolam produced stable hemodynamics and improved LMA insertion conditions but was associated with delayed recovery.22 Propofol and sevoflurane were compared for laryngeal mask anaesthesia for magnetic resonance imaging (MRI) in paediatric patients and it was found that sevoflurane, provided shorter induction and faster recovery times than IV propofol for LMA anaesthesia in children undergoing MRI.23
As in our study Goh PK et al11 also compared LMA insertion conditions using fentanyl and ketamine with propofol but in adults and reported a much higher incidence of cases requiring additional propofol for successful insertion. Twenty three percent of patients in the fentanyl group and 10% patients in the ketamine group required an additional bolus of propofol. This may have been due to a lower dose of fentanyl (1μg kg-1) used in their study. They also reported a higher incidence of head and limb movements with the use of ketamine (40%) as compared to fentanyl (16%) although the incidence was less than what we observed. In contrast to our study the authors have reported an incidence of 10% of coughing/gagging in both fentanyl and ketamine group. Similar to our results, other authors9,19 have also reported lower incidence of coughing/ gagging with the use of fentanyl. Goh PK et al11 have reported a higher resistance than ours to LMA insertion and mouth opening in the fentanyl group and a lower incidence in ketamine group (16.7% vs 3.3% and 50% vs 36.6%, respectively). This difference probably has resulted because we used a higher dose of both propofol and fentanyl as compared to them. Various other authors have also similarly reported a much higher incidence of resistance to mouth opening with the use of fentanyl.9,19 Further more Goh PK et al11 reported a 6.6% incidence of laryngospasm in the fentanyl group, but none in the ketamine group and their summed insertion score was similar in both the fentanyl and ketamine groups.
In a study by Sayyid SMS et al24 a combination of sevoflurane-propofol for induction was associated with a higher incidence of successful LMA insertion at the first attempt (93.5%) than with either sevoflurane (46%) or propofol alone (61.5%) (p < 0.001). Cheam EWS et al9 have reported a lower incidence of limb and head movements with the use of fentanyl (42%) as compared to mivacurium (56%) and demonstrated that the summed score was only slightly better in the mivacurium group, as compared to fentanyl group.
Statistically, a highly significant difference was seen in the incidence of apnoea (lasting >30 seconds) between the 2 groups (p=0.002) in our study. This is to be expected because fentanyl given as an intravenous bolus is known to cause apnoea.25 However, in our study the incidence of prolonged apnoea (>5 minutes) was slightly higher in the ketamine group as compared to the fentanyl group (14% vs 12% patients). The incidence of apnoea in our study is comparable to that reported by Goh PK et al11, although the dose of fentanyl used in our study was 2μg kg-1 as compared to 1μg kg-1used by them. They have reported a higher incidence of prolonged apnoea in the fentanyl group (23.3%) as compared to the ketamine group (6.3%).
In the present study the baseline measurements of heart rate (p=0.264), systolic blood pressure (p=0.219), diastolic blood pressure (p=0.95) and mean arterial pressure (p=0.394) were similar in both the groups. The patients in the ketamine group showed an elevation of heart rate from the baseline value, whereas decreased heart rate was a feature of the fentanyl group. The indirect sympathomimetic effect of ketamine on the sinus node may be the possible mechanism for an increase in heart rate. We also observed consistently higher systolic blood pressure, diastolic blood pressure and mean blood pressure in the ketamine group as compared to the fentanyl group. Our results are similar to those of Goh PK et al11 who found higher HR and higher systolic and mean blood pressures in the ketamine group-propofol group than the fentanyl-propofol or propofol alone group. In a recent study,22 the authors showed a significantly greater decrease in SBP when propofol was used alone for induction than when a combination of propofol and ketamine was used for LMA insertion in children.
To conclude our study has shown that the summed score describing the overall LMA insertion conditions was better in the fentanyl group as compared to the ketamine group. Although resistance to mouth opening and resistance to LMA insertion was comparable in both the groups, swallowing, coughing/gagging and limb/head movements were significantly more in the ketamine group as compared to fentanyl group. Incidence of apnoea was higher in the fentanyl group; however the duration of apnoea was slightly prolonged in the ketamine group. The HR, SBP, DBP, and MAP were consistently higher in the ketamine group as compared to the fentanyl group. Therefore the combination of fentanyl (2μg kg-1) and propofol (3.5mg kg-1) provides better conditions for LMA insertion in children than a combination of ketamine (0.5 mg kg-1) and propofol (3.5mg kg-1).
REFERENCES
- 1.Brain AIJ, Mc Ghee TD, Mc Ateer EJ, Thomas A, Abu-Saad MAW, Bushman JA. The laryngeal mask airway. Development and preliminary trials of a new type of airway. Anaesthesiay. 1985;40:356–361. [PubMed] [Google Scholar]
- 2.Brimacombe J, Berry AM. The laryngeal mask airway-anatomical and physiological implications. Acta Anaesthesiol Scand. 1996;40:201–209. doi: 10.1111/j.1399-6576.1996.tb04420.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown GW, Patel N, Ellis FR. Comparison of propofol and thiopentone for laryngeal mask insertion. Anaesthesia. 1991;46:771–772. doi: 10.1111/j.1365-2044.1991.tb09776.x. [DOI] [PubMed] [Google Scholar]
- 4.Scanlon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of anaesthesia with propofol or thiopentone. Can J Anaesth. 1993;40:816–818. doi: 10.1007/BF03009250. [DOI] [PubMed] [Google Scholar]
- 5.Bahk JH, Han SM, Kim SD. Management of paediatric difficult airway with a laryngeal mask airway under propofol anaesthesia. Paed Anaesth. 1999;9:163–166. doi: 10.1046/j.1460-9592.1999.9220305.x. [DOI] [PubMed] [Google Scholar]
- 6.Seavell CR, Cook TM, Cox CM. Topical lignocaine and thiopentone for insertion of a laryngeal mask airway: a comparison with propofol. Anaesthesia. 1996;51:699–701. doi: 10.1111/j.1365-2044.1996.tb07860.x. [DOI] [PubMed] [Google Scholar]
- 7.Driver IK, Wiltshire S, Mills P, Lillywhite N, Howard-Griffin R. Midazolam co-induction and laryngeal mask insertion. Anaesthesia. 1996;51:782–784. doi: 10.1111/j.1365-2044.1996.tb07897.x. [DOI] [PubMed] [Google Scholar]
- 8.Chui PT, Cheam EWS. The use of low dose mivacurium to facilitate insertion of laryngeal mask airway. Anaesthesia. 1998;53:486–510. doi: 10.1046/j.1365-2044.1998.00321.x. [DOI] [PubMed] [Google Scholar]
- 9.Cheam EWS, Chui PT. Randomised double-blind comparison of fentanyl, mivacurium or placebo to facilitate laryngeal mask airway insertion. Anaesthesia. 2000;55:323–326. doi: 10.1046/j.1365-2044.2000.01214.x. [DOI] [PubMed] [Google Scholar]
- 10.Dollery C. Edinburgh: Churchill Livingstone; 1991. Therapeutic drugs; pp. K7–13. [Google Scholar]
- 11.Goh PK, Chiu CL, Wang CY, Chan YK, Loo PL. Randomised double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol-saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intens Care. 2005;33:223–228. doi: 10.1177/0310057X0503300211. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non anesthesiologists. Anesthesiology. 2002;96:1004–1017. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 13.Goyagi T, Tanaka M, Nishikawa T. Fentanyl decreases propofol requirement for laryngeal mask airway insertion. Acta Anaesthesiol Scand. 2003;47:771–774. doi: 10.1034/j.1399-6576.2003.00123.x. [DOI] [PubMed] [Google Scholar]
- 14.Martlew RA, Meakin G, Wadsworth R, Sharples A, Baker RD. Dose of propofol for laryngeal mask airway insertion in children: effect of premedication with modazolam. Br J Anaesth. 1996;76:308–309. doi: 10.1093/bja/76.2.308. [DOI] [PubMed] [Google Scholar]
- 15.Ko SH, Kim DC, Han YJ, Song HS. Small-dose Fentanyl: Optimal Time of Injection for Blunting the Circulatory Responses to Tracheal Intubation. Anesth Analg. 1998;86:658–661. doi: 10.1097/00000539-199803000-00041. [DOI] [PubMed] [Google Scholar]
- 16.Sivalingham P, Kandasamy R, Madhaven G, Dhakshi-namoorthi P. Conditions for laryngeal mask insertion. A comparison of propofol versus sevoflurane with or without alfentanil. Anaesthesia. 1999;54:271–276. doi: 10.1046/j.1365-2044.1999.00663.x. [DOI] [PubMed] [Google Scholar]
- 17.Ng K C, Ang S Y. Sedation with Ketamine for Paediatric Procedures in the Emergency Department - A Review of 500 cases. Singapore Med J. 2002;43(6):300–304. [PubMed] [Google Scholar]
- 18.Hui JK, Critchley LA, Karmakar MK, Lam PK. Co-administration of alfentanil-propofol improves laryngeal mask airway insertion compared to fentanyl-propofol. Can J Anaesth. 2002;49:508–512. doi: 10.1007/BF03017932. [DOI] [PubMed] [Google Scholar]
- 19.Wong CM, Cirtchley LA, Lee A, Shaw KS, Kee WDN. Fentanyl dose-response curves when inserting the LMA ClassicTM laryngeal mask airway. Anaesthesia. 2007;62:654–660. doi: 10.1111/j.1365-2044.2007.05057.x. [DOI] [PubMed] [Google Scholar]
- 20.JH Bahk, J Sung, IJ Jang. Comparison of ketamine and lidocaine spray with propofol for the insertion of LMA in children- a double blind randomized trial. Anesth Analg. 2002;95:1586–1589. doi: 10.1097/00000539-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Begec Z, Demirbilek S, Onal D, et al. Ketamine or alfentanil administration prior to propofol anaesthesia: the effects on ProSeal laryngeal mask airway insertion conditions and haemodynamic changes in children. Anaesthesia. 2009;64(3):282–286. doi: 10.1111/j.1365-2044.2008.05782.x. [DOI] [PubMed] [Google Scholar]
- 22.Goel S, Bhardwaj N, Jain K. Efficacy of ketamine and midazolam as co-induction agents with propofol for laryngeal mask insertion in children. Paediatric Anaesthesia. 2008;18:628–634. doi: 10.1111/j.1460-9592.2008.02563.x. [DOI] [PubMed] [Google Scholar]
- 23.Kol I O, Egilmez H, Kaygusuz K, et al. Open-label, prospective, randomized comparison of propofol and sevoflurane for laryngeal mask anesthesia for magnetic resonance imaging in pediatric patients. Clinical Therapeutics. 2008;30(2):175–181. doi: 10.1016/j.clinthera.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 24.Sayyid SMS, Aouad MT, Taha SK, Daaboul DG, Deeb PG, Massouh FM, Muallem MRA, et al. A comparison of sevoflurane-propofol versus sevoflurane or propofol for laryngeal mask airway insertion in adults. Anesth Analg. 2005;100(4):1204–1209. doi: 10.1213/01.ANE.0000148166.29749.3B. [DOI] [PubMed] [Google Scholar]
- 25. http://www.baxter.com/products/anesthesia/anesthetic_pharmaceuticals/ downloads/fentanyl.pdf .


