Abstract
A number of factors including inflammation and oxidative stress are believed to play a role in the development of chronic joint diseases. Green tea has become a popular drink and is consumed throughout the world. Extracts of green tea and polyphenols present therein have been shown to inhibit the inflammatory responses in vitro in different cell types and the development of arthritis in animal model studies. There is considerable evidence that (-)-epigallocatechin-3-gallate (EGCG), the predominant green tea polyphenol which mimic its effects, inhibits enzyme activities and signal transduction pathways that play important roles in inflammation and joint destruction in arthritis. After oral consumption EGCG become bioavailable and proteomic studies suggest that EGCG may directly interact with a large set of protein targets and alter the physiological response of the cells. Taken together these and other studies identify and support the use of EGCG as a possible chemopreventive agent with a potential to inhibit the development of arthritis. Here we review the biological effects of EGCG in an attempt to understand its pivotal molecular targets that directly affect the inflammation and joint destruction process for prevention and/or for the development of new therapeutics for arthritis in humans.
Keywords: Green Tea, EGCG, Osteoarthritis, Rheumatoid arthritis, MAPK, NF-κB
Introduction
Arthritis represents a major health problem and its global burden is rising at an alarming rate. Arthritis affects nearly 46 million people in the USA and by 2030 the number of people with arthritis is expected to rise to 67 million (Helmick et al. 2007; Lawrence et al. 2007). In the Western world and USA, arthritis and related conditions have been identified as the third largest contributor to direct health expenditure (behind cardiovascular disease and neurological disorders) (Penm et al. 2001). Osteoarthritis (OA) and rheumatoid arthritis (RA) are a group of diseases with different profiles and unknown etiology but similar outcome- joint destruction. OA involves the erosion of articular cartilage, inflammation of synovial membrane, and resorption of the underlying sub-chondral bone (vander-Kraan and vanden-Berg 2000; Arden and Nevitt 2006). On the other hand, RA is a chronic inflammatory and systemic disorder characterized by cellular infiltration and proliferation of synovium, leading to progressive destruction of the joints through the interaction between infiltrating cells and mediators they produce (Lee and Weinblatt 2001). However, pathological changes in both diseases are associated with an excessive production of pro-inflammatory molecules, which shift the balance between the synthesis and degradation of matrix components resulting in progressive destruction of the joint tissue (Kraan and Berg 2000). Pharmacologic treatment options for arthritis are diverse both in terms of mechanisms of action and delivery formulations; however, no single agent has been demonstrated to consistently offer both a high level of tolerability and a sustained degree of efficacy across a broad patient population. Current treatment options are mostly symptomatic and include Non Steroidal Anti-Inflammatory Drugs (NSAIDs) (Altman 2009) and cyclooxygenase-2 (COX-2) inhibitors (rofecoxib) (Hsiao et al. 2009) for pain relief but fail to block the progression of the disease. Unfortunately, these agents are also associated with gastrointestinal (Chan et al. 2010) and cardiovascular adverse events (Hsiao et al. 2009). Intra-articular therapies like glucocorticoids and hyaluronans injections have been used for pain relief in OA patients but recent observations suggest that intra-articular hyaluronic acid injections may accelerate cartilage breakdown in patients with symptomatic knee osteoarthritis (Gonzalez-Fuentes et al. 2010). Matrix Metalloproteases (MMPs) inhibitors have been studied as possible drugs for prevention of cartilage degradation but their clinical use has been limited by severe side-effects (Nuti et al. 2009). Recent reports showed that by blocking aggrecanase mediated cleavage in the aggrecan interglobular domain abrogates cartilage erosion and promotes cartilage repair (De Rienzo et al. 2009). However, despite ablation of a disintegrin and metalloproteinase with thrombopondin motif-5 (ADAMTS-5) activity (major factor for aggrecan loss), aggrecanolysis can still occur at two preferred sites in the chondroitin sulfate-rich region (De Rienzo et al. 2009; East et al. 2007) indicating the need for more effective inhibitors. Disease modifying anti-rheumatic drugs (DMARDs) are used to treat the clinical and radiological course of RA but have serious side effects (Feist and Burmester 2009). The use of biologics (antibodies or soluble receptors for interleukin (IL)-1, IL-6 and tumor necrosis factor (TNF)-α) has recently been introduced for treating RA, but these are also not universally effective (Feldman and Maini 2001; Choy et al. 2002; Braddock and Quinn 2004). Additionally, higher costs and increased risk of malignancies limit the use of such agents in many populations (Brown et al. 2002). Because of these limitations, there is a growing interest to use botanicals as an adjunct therapy to prevent the development of arthritis and other chronic diseases. There are many reasons why people use herbal products: conventional treatment may not be working as well as they would like; they have issues with side-effects of pharmaceutical treatment; they wish to reduce some of the stress that comes from living with a chronic illness and want to cope better; they believe that herbal products are safe, because these are ‘natural’. The objective of this review is to discuss the potential arthritis preventive and anti-inflammatory effects, as well as possible harmful effects, of green tea and its prominent polyphenol EGCG in animals and humans. This knowledge may be useful for the development of EGCG-based novel strategies for targeting pathways associated with joint destruction in arthritis.
Green tea catechins
Tea is a widely consumed beverage throughout the world and reported to possess significant health promoting effects (reviewed in Cabrera et al. 2006). Depending on the manufacturing processes, teas are classified into three major types: ‘non-fermented’ green tea (produced by drying and streaming the fresh leaves to inactivate the polyphenol oxidase); ‘semi-fermented’ oolong tea (produced when the fresh leaves are subjected to a partial fermentation stage before drying); and ‘fermented’ black and red teas which undergo a post-harvest fermentation stage before drying and streaming (Cabrera et al. 2003). Non-fermented green tea consists of more polyphenolics (30%) than black (5%) and oolong (4.5%) tea (Belitz and Grosh 1997; Zuo et al. 2002). Green tea contains proteins (15%), amino acids (4%), fiber (26%), other carbohydrates (7%), lipids (7%), pigments (2%), minerals (5%), and phenolic compounds (30%) (Cabrera et al. 2006; Belitz and Grosh 1997). The main flavonoids present in the green tea include catechins (flavan-3-ols). The principal catechins found in the green tea are epicatechin (EC; 6.4%), epicatechin-3-gallate (ECG; 13.6%), epigallocatechin (EGC; 19%), and epigallocatechin-3-gallate (EGCG; 59%), and account for 30–40% of its dry weight. The strong antioxidant potential of green tea catechins has been widely demonstrated in in vitro and in animal studies (Cabrera et al. 2003, 2006; Frei and Higdon 2003; Nakagawa and Yokozawa 2002). Green tea catechins especially EGCG has been reported to have anti-mutagenic (Cheng et al. 2009), anti-cancer (Johnson et al. 2010), anti-diabetic (Zhang et al. 2010), anti-inflammatory (Danesi et al. 2010), anti-bacterial (Osterburg et al. 2009), anti-viral (Xiao et al. 2008), anti-obesity (Moon et al. 2007) and neuro-protective effects (Smith et al. 2010). A proteomics study of human vascular senescent endothelial cells treated with EGCG, has demonstrated altered expression of various proteins associated with cytoskeleton and cell cycle (Lee et al. 2006). In addition, a combined proteomics and gene expression analysis showed that EGCG affected the expression level of diverse proteins, including proteins related to cytoskeletal components, metabolism, binding proteins and heat shock proteins associated with neuro-protective effects (Weinreb et al. 2007). The potential disease-modifying effects of green tea on arthritis came to light through our study, when in a mouse model of RA induction and severity of arthritis was ameliorated by the prophylactic administration of green tea polyphenols (GTPs) in drinking water (Haqqi et al.1999). Subsequent studies suggested that EGCG possesses remarkable potential to prevent chronic diseases like OA and RA (Ahmed et al. 2004, 2005, 2008; Singh et al. 2002; Yun et al. 2008). The anti-inflammatory and anti-arthritic effects of EGCG are supported by in vitro and in vivo data indicating that EGCG or EGCG containing green tea can regulate the expression of cytokines, chemokines, MMPs, aggrecanase, reactive oxygen species (ROS), nitric oxide (NO), COX-2, and PGE2 in cell type relevant to the pathogenesis of OA and RA (Haqqi et al. 1999; Ahmed et al. 2004, 2005, 2008; Singh et al. 2002; Yun et al. 2008). Further, EGCG is known to inhibit osteoclasts differentiation, expression of receptor activator for nuclear factor-κB (RANKL), epithelial neutrophil activating protein-78 (ENA-78), growth regulated oncogene (GRO)-α, monocyte chemotectic protein (MCP)-1 and myeloid cell leukemia sequence (Mcl)-1 in an inflamed RA joint (Morinobu et al. 2008; Ahmed et al. 2006 and 2009; Lin et al. 2008). These in vitro and in vivo observations point out the efficacy of EGCG and demonstrate that it can modulate multiple signal transduction pathways in a fashion that suppresses the expression of inflammatory mediators that play a role in the pathogenesis of arthritis.
Structure-activity relationship
Structural activity relationship with EGCG indicates that there is a linear increase of the rate constants with OH radical which correlates with the number of reactive hydroxyl group (i.e. the number of catechols or pyrogallol moieties). This suggests the importance of structure of EGCG linked to gallic acid for its antioxidant activity (Plumb et al. 1998). EGCG is reported to inhibit the IKK activity in intestinal epithelial cells and this is correlated with the presence of the gallate group because the polyphenols lacking gallate group failed to inhibit the IKK activity (Yang et al. 2001). Studies have shown that EGCG selectively inhibits the phosphorylation of c-Jun and DNA binding activity of AP-1 in human OA chondrocytes (Ahmed et al. 2002). The inhibition of AP-1 activity by EGCG and related tea catechins was also attributed to the gallate moiety (Chung et al. 1999). Structural and functional analyses have identified the galloyl and a hydroxyl group present at the 3’ position on EGCG molecule as responsible for its strong anti-inflammatory properties in articular chondrocytes (Andriamanalijaona et al. 2005). EGCG has been reported to enhance the susceptibility of TNFα-induced RA-synovial fibroblasts to apoptosis (Ahmed et al. 2009). It has been suggested that catechins without a pyrogallol-type structure showed no inhibition of apoptosis (Saeki et al. 2000). Proteasome is the major machinery in cells for protein degradation. Protein ubiquitination is a mechanism that enables proteasome to specifically degrade proteins that are destined to be destroyed (Pujol 1999). In eukaryotes, proteasome contains at least three types of catalytic activities: chymotrypsin-like, trypsin-like and caspase-like (Seemuller et al. 1995). Proteasome mediated degradation of IκB facilitate the NF-κB activation and translocation to nucleus (Saklatvala et al. 2007). Thus, proteasome mediated degradation pathway is considered an important target for the treatment inflammation and arthritis. EGCG inhibits potently and specifically the chymotrypsin-like activity of proteasome in vitro (IC5086–194 nM) and ester bond within EGCG play a critical role in this inhibitory activity (Nam et al. 2001). We have shown that EGCG-mediated inhibition of NF-κB was via inhibition of proteosome activity in human chondrocytes (Singh et al. 2002).
Anti- arthritic potential of EGCG
Recent evidences based on the molecular and cellular evaluation of green tea effects in different systems have brought to the forefront the value of green tea catechins as agents for modulating inflammation and arthritis (Haqqi et al. 1999; Ahmed et al. 2004, 2005, 2006, 2008, 2009; Singh et al. 2002; Yun et al. 2008; Morinobu et al. 2008). EGCG is a potent anti-oxidant and can alter the redox status of joint and activity of inflammatory cells involved in disease pathogenesis. EGCG has been characterized as a ligand for the 67 kDa laminin receptor (LR) as experiments performed in human lung cancer cells demonstrated that EGCG inhibit their growth via 67 kDa LR with a kd value of 39.9 nM (Tachibana et al. 2004). Beside the role of LR in cell adherence to the extracellular matrix (ECM), there is growing evidence that 67kDa LR activation induce functional changes within the cells (Nelson et al. 2008). The extracellular matrix is an "information rich" environment and interactions between the chondrocyte and ECM regulate many biological processes important in cartilage homeostasis and repair including cell attachment, growth, differentiation, and survival. Chondrocytes have been shown to express laminin β1 integrin receptor (Loeser 2000, 2002) and in synovial tissues of RA patients laminins and integrins co-localize with increased expression of inflammatory cytokines (Warstat et al. 2010; Poduval et al. 2010). These results suggest the possible interactive relationship between EGCG receptor present on chondrocytes and synovial cells for its possible anti-arthritic effect. Further in depth studies of this receptor and signaling in arthritis would help to clarify the specific effects of EGCG on chondrocytes and synoviocytes and may enable the better utilization of EGCG as a preventive or therapeutic agent.
Effect of EGCG on nuclear factor-kappa B (NF-κB) signaling pathway
NF-κB acts as a controlling switch for the regulation of genes important in cellular response, inflammation, innate immunity, and arthritis (Karin and Ben-Neriah 2000). It is well known that inflammation and cartilage degeneration is a result of increase in catabolic mediators and decrease in anabolic activity (Westacott and Sharif 1996). The anti-arthritic effects of EGCG are important not only in reducing the pro-inflammatory mediators production but also enhancing anabolic activity (Singh et al. 2002; Andriamanalijaona et al. 2005; Zheng et al. 2009; Yang et al. 2001;Wheeler et al. 2004). We have previously shown that EGCG inhibits NF-κB activity by blocking the phosphorylation of IκB-α in human OA chondrocytes (Singh et al. 2002). Recently, it has been reported that EGCG inhibits the expression of NF-κB in RAW 264.7 macrophages (Lin et al. 2009). EGCG is also reported to inhibit TNF-α and LPS mediated activation of NF-κB via inhibiting IκB-α phophorylation (Ahmad et al. 2000). Of relevance to arthritis suppressive are the studies showing effects of EGCG, that EGCG inhibits IL-1 induced protein kinase Cδ phosphorylation and NF-κB activation and nuclear translocation to suppress chemokines and collagenases production in RA synovial fibroblasts (Ahmed et al. 2006). Also EGCG not only induces apoptosis but enhances the susceptibility of RA-synovial fibroblasts to TNFα-induced apoptosis by supressing Akt and NF-κB pathways (Ahmed et al. 2009). EGCG has been shown to inhibit IκB Kinase (IKK) activity, IκB-α phophorylation and NF-κB activation in intestinal epithelial cells (Yang et al. 2001), respiratory epithelial cells (Wheeler et al. 2004), endothelial cells (Hong et al. 2007), and in mast cells (Shin et al. 2006). We have also shown that EGCG inhibits IKK-α and IKK-β activity in SAOS-2 cells with concominant down regulation of NF-κB and induction of apoptosis (Hafeez et al. 2006). This inhibition of IKK activity by EGCG related to the presence of the gallate group because the polyphenols lacking gallate group did not inhibit IKK activity (Yang et al. 2001). EGCG was also found to inhibit IKK-β kinase activity and DNA binding activity of NF-κB in human articular chondrocytes (Andriamanalijaona et al. 2005; Rasheed et al. 2009). Basically, this may occur as a direct effect on IKK protein or by interfering with the interaction of IKK with its substrate IκB. EGCG may also block NF-κB activation by inhibiting signaling events upstream of IKK or its unique structure may inhibit IKK enzyme activity directly. Both mechanisms would lead to inhibition of NF-κB activation. As EGCG becomes bioavailable after oral consumption, modulation of NF-κB pathway by EGCG in vivo could contribute to its reported anti-arthritic and anti-inflammatory activity in the joints.
Effects of EGCG on mitogen activated protein kinases (MAPKs) and activator protein-1 (AP-1) pathways
The MAPKs are an essential part of signal transduction machinery involved in the regulation of inflammation associated with gene expression, cell survival, proliferation, inducible nitric oxide synthase (iNOS) and cytokine expression, and collagenase production (Hommes et al. 2003). MAPKs have three major classes c-Jun-N terminal kinase (JNK), extracellular signal regulated kinase (ERK), and p38 MAPKs (Johnson and Lapadat 2002). Of note, all three classes of MAPKs have been shown to be expressed and activated in chondrocytes and synovial tissue of RA and OA patients (Chowdhary et al. 2008; Schett et al. 2000). Thus inhibition of MAPKs may represent legitimate therapeutic targets for the treatment of arthritis. EGCG exerted a marked inhibition of both basal and IL-1 stimulated MAPKs phosphorylation at 50µM concentration in chondrocytes (Andriamanalijaona et al. 2005). EGCG was also reported to suppress the RANKL induced activation of JNK pathway without affecting p38 and ERK (Lee et al. 2010). We have shown that EGCG selectively inhibits IL-1β-induced activation of JNK, without significantly inhibiting the phosphorylation of p38-MAPK or ERK p44/p42 in human OA chondrocytes (Singh et al. 2003). Other studies have shown that EGCG treatment inhibited TNF-α induced phosphorylation of ERK1/2, p38 MAPK, and JNK in RA synovial fibroblasts (Yun et al. 2008). Tokuda et al., have reported that EGCG enhanced prostaglandin F2alpha-induced vascular endothelial growth factor (VEGF) synthesis and reduced TGF-β-stimulated HSP27 induction through the suppression of stress activated protein kinases (SAPK)/JNK (Tokuda et al. 2007; Hayashi et al. 2008). EGCG was also reported to suppresses endothelin-1-induced IL-6 synthesis via MEK1/2 in osteoblast-like MC3T3-E1 cells (Tokuda et al. 2008). EGCG has also been reported to interfere with the activation of MAPKs to regulate various inflammatory genes in human dermal fibroblasts via inhibition of p38, JNK and ERK phosphorylation (Bae et al. 2008), in endothelial cells via p38 MAPKs (Hong et al. 2007) and in HMC cells via ERK (Shin et al. 2006). EGCG has also been shown to inhibit the oxidative stress-mediated phosphorylation of MAPKs in human epidermal keratinocytes (Katiyar et al. 2001). The down-regulation of IL-12 production by EGCG has been suggested as a mechanism for the amelioration of RA and possibly other diseases (Goodridge et al. 2003). This effect of EGCG was mediated via inhibition of phosphorylation of ERK and p38 MAPK with concomitant down-regulation of IL-12p40 production (Ichikawa et al. 2004).
AP-1 transcription factor is a heterodimer of Jun (c-Jun, Jun B, Jun D) and Fos (cFos, Fos B, Fra-1 and Fra-2) proteins and plays an important role in inflammatory response (Okamoto et al. 2008). EGCG was found to inhibit the DNA binding activity of AP-1 in human OA chondrocytes (Andriamanalijaona et al. 2005). Studies from our laboratory have also shown that EGCG selectively inhibits the IL-1β-induced phosphorylation of JNK p46 isoform resulting in the lower levels of phospho-c-Jun and DNA binding activity of AP-1 in human OA chondrocytes (Ahmed et al. 2002). EGCG mediated suppression of TNF-α-induced production of MMPs in RA synovial fibroblasts was dependent on the inhibition of AP-1 pathway (Yun et al. 2008). Overall, anti-arthritic effects of EGCG have been attributed to its ability to modulate signaling pathways controlling inflammatory gene expression and this may be of value for inhibiting bone and cartilage degeneration associated with OA and RA.
Effects of EGCG on signal transducers and activators of transcription (STAT) pathway
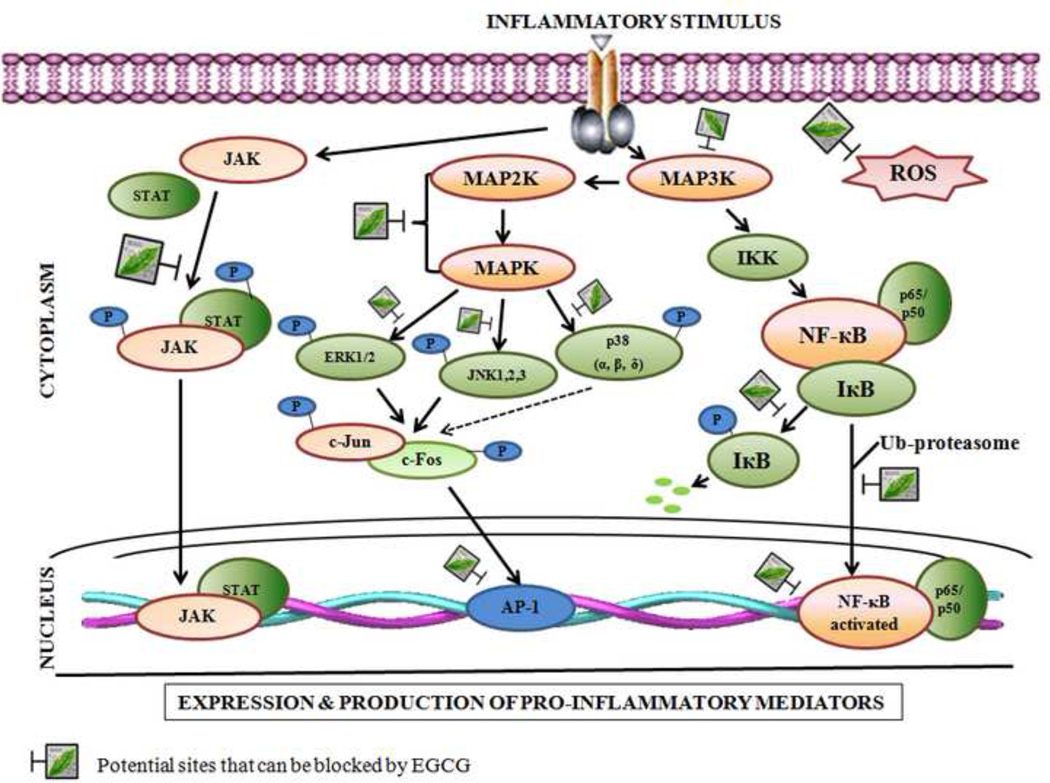
STAT proteins are involved in modulating cellular responses to pro-inflammatory cytokines, such as IL-1, TNF- α, as well as growth factors and immunomodulatory proteins, including interferon (IFN)- γ (Igaz et al. 2001). Some investigators have reported preferential activation of STAT-1, and others have reported preferential activation of STAT-3, in response to endogenous IL-6 in RA patients (de Hooge et al. 2004; Kasperkovitz et al. 2004). Inappropriate activity of STAT-3 is closely associated with experimental arthritis in vivo (Richards et al. 2006). Further, STAT-1 deficiency in mice resulted in exacerbation of the chronic inflammation and granuloma formation (de Hooge et al. 2004). However, STAT-1 has been shown to be strongly activated in synovium of RA patients (Yokota et al. 2001). Raised STAT-1 protein expression with concominant increase in its tyrosine-701 and serine-727 phosphorylation suggested that STAT-1 activation in RA synovium plays a major role in RA-associated inflammation (Kasperkovitz et al. 2004; Tedeschi et al. 2002). Therefore, STAT-1 and 3 may represent new molecular targets of anti-inflammatory drugs. Studies have shown that EGCG exert a potent and specific inhibitory effect on IFN-γ-elicited STAT1 activation in a number of human cell types with an estimated EC50 of 2–5 µM without any effect on other STATs, such as STAT3 and 6 (Tedeschi et al. 2002; Menegazzi et al. 2001). Oral administration of EGCG attenuated the magnitude of myocyte apoptosis in the rat heart exposed to I/R injury with concomitant STAT1 inhibition (Townsend et al. 2004). Recently, it was reported that EGCG can suppress oncostatin M induced activation of STAT-3 phosphorylation in human gingival (Hosokawa et al. 2009) and keloid fibroblasts (Park et al. 2008). These studies when taken together clearly identify EGCG as having distinct actions on the nuclear transcription factors activation in a cell-specific manner (Figure 1). This again demonstrates that EGCG or compounds derived from it may be of value in developing new therapeutic approaches for the treatment of OA and RA.
Fig. 1. Effect of EGCG on signal transduction pathways.
EGCG regulates inflammation and joint degeneration by modulating MAPKs, AP-1, NF-κB pathway and STAT signaling activated by TNF-α, IL-1β and IFN-γ in various cell types.
Inhibition of matrix degrading enzymes
Many inflammatory signals are orchestrated within the tissue microenvironment external to cell. A super family of proteases called metzincins (zinc dependent metallopeptidases) includes MMPs, a disintegrin and metalloproteinase (ADAM) and the secreted ADAM with thrombospondin motif (ADAMTS) (Mohammed et al. 2003). Aggrecanase-1 and -2 (ADAMTS-4 and -5) are principal proteases involved in aggrecan degradation and were found to be increased in OA and RA (Mohammed et al. 2003; Smith 2006). A major component of joint cartilage is collagen, which is susceptible to proteolytic degradation by MMPs. This suggests that MMPs and aggrecanases are promising targets for inhibiting the pathogenesis of OA and RA (Mohammed et al. 2003; Smith 2006). EGCG inhibited the degradation of human cartilage proteoglycan and type II collagen and selectively inhibited the ADAMTS-1,-4 and -5, which are known to cleave aggrecan (Vankemmelbeke et al. 2003). Previously we have shown that EGCG significantly inhibited the expression and activities of MMP-1 and MMP-13 in OA chondrocytes at physiologically achievable doses in vitro (Ahmed et al. 2004). Our recent studies showed that EGCG inhibited advance glycation end products (AGEs) induced expression of MMP-13 in human OA chondrocytes (Rasheed et al. 2009). EGCG was also found to be effective in suppressing the chemokine-induced MMP-2 activity in human colon epithelial cells (Porath et al. 2005) and TNF-α induced production of MMP-1 and MMP-3 in RA synovial fibroblasts (Yun et al. 2008). Studies have also shown that EGCG was an effective inhibitor of IL-1β-induced MMP-1, -3 and -13 expressions in human tendon fibroblasts (Corps et al. 2004). Studies have also documented that EGCG not only decreased the level of MMPs production but also increased the expression of tissue inhibitors of MMP-1 (TIMP-1) in vitro (Lee et al. 2005). Green tea polyphenols have also been reported to inhibit the gelatinolytic activity of MMP-2 and enhances its binding with TIMP-2 (Cheng et al. 2003). Overall, consumption of green tea or EGCG may inhibit the activities of MMPs involved in matrix degradation and this may have a suppressive effect on joint degradation in arthritis.
Modulation of inflammatory cytokines and chemokines expression
A prominent and characteristic feature of arthritis is the persistent production of pro-inflammatory cytokines by the inflamed synovium as well as by chondrocytes in the affected joints (Westacott and Sharif 1996; Malemud et al. 2003; Rasheed and Haqqi 2008). Therefore, the cytokine network constitutes an important target for the development of novel anti-inflammatory drugs (Alkharfy et al. 2000). Consumption of green tea polyphenols has been shown to limit inflammation and maintain joint architecture in an animal model of arthritis (Haqqi et al. 1999). In other studies, EGCG down regulated the LPS-induced inflammatory response in vivo in RAW264.7 macrophages (Yang et al. 1998) and was also shown to influence the migration of CD8+ T cells to sites of inflammation (Kawai et al. 2004). EGCG inhibited T cell proliferation at physiologically relevant concentrations of 2.5 to 10 microM without cytotoxicity or induction of apoptosis (Wu et al. 2009). EGCG supplementation resulted in lower IL-2 receptor expression and higher IL-2 accumulation, suggesting an impeded IL-2/IL-2 receptor signaling (Wu et al. 2009). These results indicate that EGCG supplementation may be beneficial to those with abnormally excessive T cell function such as in autoimmune and inflammatory disorders, but caution should be taken when it is administered at high doses to those with compromised T cell function (Wu et al. 2009). In in vivo studies EGCG was found to inhibit inflammation in mouse models by affecting the functioning of T cells and neutrophils (Aktas et al. 2004; Dona et al. 2003). EGCG (50 mg/L) inhibited the expression and level of IL-1β at wound sites (Shen et al. 2009). EGCG has also been shown to inhibit the TNF-α gene expression and its secretion in different cell types (Fujiki et al. 2003). Recently, EGCG was reported to inhibit the secretion of TNF-α and IL-6 in human mast cells (Shin et al. 2006). The pro-inflammatory cytokine IL-6 has been shown to be over-expressed in RA and is now believed to play a central role in RA joint destruction and the systemic nature of disease (Moller et al. 2006; McInnes and Liew 2005). IL-6 knockout mice were shown to be resistant to collagen induced arthritis and had reduced levels of serum TNF-α (McInnes and Liew 2005). EGCG inhibited IL-1β-induced IL-6 production and trans-signaling in RA synovial fibroblasts by inducing alternative splicing of gp130 mRNA resulting in enhanced sgp130 production (Ahmed et al. 2008). A recent report showed that EGCG significantly inhibited IL-23-induced IL-17 and TNF-α expression in T-cell lines and this proposed a new nutritional approach for the prevention and treatment of inflammatory bowel diseases (Danesi et al. 2010; Wu et al. 2009). Age related accumulation of AGEs produced by the non-enzymatic glycation of macromolecules could be an important contributing factor for the development of OA (Rasheed et al. 2009). We recently reported that EGCG inhibited AGEs-stimulated gene expression and production of TNF-α in human OA chondrocytes in vitro (Rasheed et al. 2009). Thus consumption of EGCG may prevent pathologies in which AGEs are believed to play a role.
Chemokines are a specialized family of small (8–10 kd), structurally related proteins and well-established regulators of gene transcription, cell proliferation, and leukocyte trafficking to normal and inflamed tissues (Szekanecz et al. 2004). Chemokines such as epithelial neutrophil–activating peptide 78 (ENA-78/CXCL5), RANTES (CCL5), monocyte chemo-attractant protein 1 (MCP-1/CCL2), and growth-regulated oncogene-α (GRO-α/CXCL1) are potent chemotactic agents that have been shown to be constitutively produced by RA synovial fibroblasts and are up-regulated upon stimulation with IL-1β (Szekanecz et al. 2004). Mice with CIA when given EGCG had less severe arthritis, inhibited macrophage infiltration, and the amount of CCL2 synthesizing osteoblasts in arthritic joints (Lin et al. 2008). EGCG has been shown to down-regulate IL-1β induced RANTES, MCP-1, ENA-78, and GRO-α production in human RA synovial fibroblasts (Ahmed et al. 2003, 2006). In addition, it is also reported that green tea blocks the chemokine production but up-regulates chemokine receptor expression in RA-synovial fibroblasts (Marotte et al. 2009). IL-8 is the most powerful chemo-attractant for neutrophils in the target tissue. EGCG is a very effective inhibitor of IL-1β and TNF-α induced IL-8 and macrophage inflammatory protein-3α (MIP-3α) expression in different cell types (Westacott and Sharif 1996; Porath et al. 2005; Netsch et al. 2006). Fractalkine, a chemokine involved in inflammation acts as a chemoattractant as well as an adhesion molecule in endothelial cells activated by pro-inflammatory cytokines (Lee et al. 2009). EGCG decreased TNF-α-induced fractalkine mRNA and protein expression in HUVECs (Lee et al. 2009). Overall these studies suggested that EGCG regulates various Inflammatory and anti-inflammatory cytokines and immune cells in unique ways to reduce inflammation and Table 1 summarizes the reported in vitro and in vivo modulatory effects of EGCG on various catabolic and anabolic mediators related to OA and RA.
Table 1.
In vitro and in vivo effects of EGCG on different joint anabolic and catabolic factors.
| Cytokines/ mediators |
Major activity in joint | Effect of EGCG/Mechanism | Cells /Animal model | Conc. / Dose |
Duration | Ref. |
|---|---|---|---|---|---|---|
| Anabolic activity | ||||||
| TGF-β | Stimulate production of cartilage matrix components | ↑ TGF-β1 and TGF-β2 expression in IL-1 induced chondrocytes | Bovine articular chondrocytes | 20 or 50 µM, EGC | 24 h | Andriamanalijaona et al. 2005 |
| BMP | growth and differentiation factor which induces cartilage or bone formation | ↑ cartilage formation in joints using BMP/Fibrous glass membrane implants | Wistar rats | 1 or 10µg EGCG | 1 to 2 weeks | Takita et al. 2002 |
| Catabolic activity | ||||||
| IL-1β | Potent inducer of cartilage degradation, bone resorption, MMPs, COX-2, iNOS and PGE2 | ↓ expression and level of IL-1β in cutaneous wound | Mouse | 50mg/L | 72 h | Shen et al. 2009 |
| TNF-α | Similar activity profile to IL-1β but relatively less potent, induces osteoclatic bone resorption more prominent role in RA | ↓ PMACI-induced TNF-α expression and production | HMC cells | 100 µM | - | Shin et al. 2006 |
| ↓ AGEs-induced TNF-α expression and production | Human OA chondrocytes | 25–150 µM | 24 h | Rasheed et al 2009 | ||
| ↓ TNF-α expression and production | PC-9 cells | 26 µM | - | Fujiki et al. 2003 | ||
| T lymphocytic leukemia cells | 10 µg/ml | 24 h | Danesi et al. 2010 | |||
| Modulators of anabolic and catabolic activity | ||||||
| IL-6 | A mediator of OA and RA both, IL-1 induced IL-6 activity is required to inhibit proeoglycan synthesis; involves STAT-3 signaling pathway | ↓ IL-1 induced IL-6 production by enhanced production of sgp130 | RA-synovial fibroblasts | 10–20 µM | 24 h | Ahmed et al. 2008 |
| ↓ PMACI-induced IL-6 production | HMC cells | 100 µM | - | Shin et al. 2006 | ||
| ↓ STAT-3 signaling | Keloid fibroblasts | 100 µM | 24 h | Park et al. 2008 | ||
| IL-8 | Neutrophil chemo-attractant. Stimulates neutrophils to produce superoxide ions | ↓ TNF-α-induced IL-8 expression and production | T84 and HT-29 cells | 25–50 µM | 24 h | Porath et al. 2005 |
| ↓ IL-1β induced IL-8 expression and production | Caco-2 cells | 4.02–160 µM | 24, 48, 72 h | Netsch et al. 2006 | ||
| Synovial fibroblasts | 50 µM | 12 h | Huang et al. 2009 | |||
| HMC cells | 100 µM | - | Shin et al. 2007 | |||
| Human nasal mucosal Fibroblasts and A549 cells | 2, 10, and 50 µg/ml | 24 h | Kim et al. 2006 | |||
| bFGF | Potentiate IL-1 induced protease release by chondrocytes; also secreted by tumor cells | ↓ basic fibroblast growth factors via proteosome inhibition | HCT-116 and LoVo cancer cells | 50µmol/L | 24 h | Sukhthankar et al. 2008 |
| mice | 0.01% in water | 2 month | ||||
| IFN-γ | Conflicting evidences for presence in OA but have a role in RA; involves STAT signaling induces iNOS and COX-2 expression | ↓IFN-γ induced STAT-1 via interferon regulating factor-1 (IRF-1) | MCF7, HepG2 and HeLa cells | 5–20 µM | 3 h | Tedeschi et al. 2002 |
| ↓ STAT-3 activation | MDA MB 231 cells | 50 µM | 1 h | Menegazzi et al. 2001 | ||
| Keloid fibroblasts | 100 µM | 24 h | Park et al. 2008 | |||
| Mcl-1 | Anti-apoptotic protein; increase expression is observed in RA | ↓ TNF-α induced Mcl-1 production | RA-synovial fibroblasts | 5–50 µM | 72 h | Ahmed et al. 2009 |
| MCP-1, ENA-78 GRO-α, MIP-3α | potent chemotactic agents that have been shown to be constitutively produced by RA synovial fibroblasts and up-regulated upon stimulation with IL-1β, major role in inducing MMPs activity in RA-synovial fibroblasts | ↓ IL-1β induced MCP-1, ENA-78, GRO-α and MIP-3α production via specific inhibition of protein kinase Cδ (PKCδ) phosphorylation and NF-κB activation and nuclear translocation. | RA-synovial fibroblasts | 10–50 µM | 24 h | Ahmed et al. 2006 |
| ↓ PMA-induced MCP-1 expression and production via inhibition of p38 MAPK and NF-κB activity | ECV304 cells | 5–30 µM | 4 h | Hong et al. 2007 | ||
| ↓ MCP-1 expression and production | THP-1 cells | 100 µM | 8 h | Melgarejo et al. 2009 | ||
| IL-17 | Inflammatory cytokine have a role in RA | ↓ IL-23 induced IL-17 production | Kit-225 cells | 10 µg/mL | 24 h | Danesi et al. 2010 |
| MMPs | Principal proteases involved in proteolytic degradation of collagen present in cartilage; induces anti-inflamatory cytokine expression | ↓ IL-1β induced MMP-1 and 13 expression and production via NF-κB and AP-1 | Human OA chondrocytes | 100 µM | 24 h | Ahmed et al. 2004 |
| ↓ AGEs- induced MMP-13 expression and production via suppression of p38- and JNK MAPKs and NF-κB activation | Human OA chondrocytes | 25–150 µM | 24 h | Rasheed et al. 2009 | ||
| ↓ TNF-α- induced MMP-1 and -3 mRNA and protein production via suppression of p38-, ERK and JNK MAPKs and AP-1 phosphorylation | RA-Synovial fibroblasts | 125–500 nM | 24 h | Yun et al. 2008 | ||
| ↓ IL-1β induced MMP-1 and 3 expression and production via JNK/ SAPK phosphoryllation and NF-κB activation | Human tendon-derived fibroblasts | 2.5–25 µM | 18 h | Corps et al. 2004 | ||
| ↓ MMP-1 and 3 production, MMP-2 and MMP-9 activity and ↑ TIMP-1 expression | Fibroblasts | 0.01–1 µM | 24 h | Lee et al. 2005 | ||
| ADAMTS | Principal proteases involved in aggrecan degradation in cartilage | ↓ ADAMTS 1, 4, and 5 | Cell free medium | 2 nM-2 µM | 3 h | Vankemmelbeke et al. 2003 |
| IL-13 | Th2 anti-inflammatory cytokine have important immunoregulatory role | ↑ IL-13 mRNA expression via JNK-dependent NFATc1 pathway | KU812 cells | 0.1–1 µM | 11–47 h | Wu et al. 2009 |
| COX-2, PGE-2, iNOS and NO | High levels are associated with OA and RA pathogenesis | ↓IL-1β-induced iNOS expression and NO production via suppression of NF-κB activation | Human OA chondrocytes | 1–100 µM | 12–24 h | Singh et al. 2002 |
| ↓IL-1β-induced iNOS, COX-2 expression NO and PGE2 production | Human OA chondrocytes | 20–200 µM | 24 h | Ahmed et al. 2002 | ||
| 5–10 µM | ||||||
| ↓LPS-induced iNOS expression NO production | Macrophages cells | 2.5–15 µM | 2–24 h | Lin and Lin 1997 | ||
BMP, bone morphogenic protein ; TGF-β, transforming gowth factor-β ;bFGF, basic fibroblasts growth factor; IFN-γ, interferon gamma; Mcl-1, myeloid cell leukemia sequence 1;MIP-3α, macrophage inflammatory protein 3 alpha; GRO-α, growth regulated oncogene-alpha; ENA-78, epithelial neutrophil activating protein 78; MCP-1, monocyte chemotactic protein-1 ; NF-κB, Nuclear factor-κB, MAPK, mitogen activated protein kinases;AP-1, activator protein-1; MMP, matrix metalloproteinase; ADAMTS, a disintegrin and metalloproteinase with thrombospondin motifs ;NFATc1, Nuclear factor activated T cell-1; IL, interleukin; COX-2, cyclooxygenase-2; PGE2, prosglandin E2; iNOS, inducible nitric oxide synthase; NO, Nitric oxide.
Inhibition of inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2) and prostaglandin E2 (PGE2) production
One of the hallmark of the inflammatory cytokines IL-1β and TNF-α is to up-regulate the production of nitric oxide (NO), and PGE2 by stimulating the expression or activities of iNOS, COX-2 and microsomal PGE synthase-1 (mPGES-1) in target cells. High levels of nitrates/nitrites have been found in the synovial fluid and serum of OA and RA patients (Slack et al. 1993; Farrell et al. 1992; Otero and Goldring 2007), which correlated with the increased levels of iNOS expression (McInnes and Liew 2005). Inhibition of iNOS has been shown to exert positive effects in an experimental OA model (Otero and Goldring 2007). EGCG selectively inhibited the production of iNOS in LPS stimulated macrophages (Lin and Lin 1997) and studies from our laboratory have shown that EGCG inhibits NO production in IL-1β stimulated human OA chondrocytes by suppressing iNOS mRNA and protein expression (Singh et al. 2002). Our data also showed that the inhibitory effect of EGCG on the induction and expression of iNOS was in part mediated via inhibition of NF-κ5 in human OA chondrocytes (Singh et al. 2003). Biochemical studies revealed that inhibition of iNOS activity by EGCG was via inhibition of binding of L-arginine and cofactor tetrahydrobiopterins to the active sites of the enzyme (Chan et al. 1997). COX-2 is the rate limiting enzyme in the production of PGE2 and we have reported that EGCG at 50 µM concentration inhibits the production of PGE2 via inhibition of COX-2 expression in IL-1β stimulated human OA chondrocytes (Ahmed et al. 2002). On the other hand, Koeberle et al. reported that mPGES-1 is a molecular target of EGCG, and inhibition of mPGES-1 is seemingly the predominant mechanism underlying suppression of cellular PGE-2 biosynthesis by EGCG without any affect on COX-2 up to 30 µM concentrations in vitro (Koeberle et al. 2009). Huang et al. showed down regulation of COX-2 and PGE2 in IL-1β stimulated synovial fibroblasts (Huang et al. 2009). This inhibitory effect of EGCG on COX-2 expression and activity suggests that EGCG or compound derived from it may be developed for selective and effective inhibition of COX-2 over expression without associated adverse events.
Effects of EGCG on transforming growth factor (TGF)-β expression
The anabolic activity of chondrocytes is sustained by growth factors such as bone morphogenetic proteins (BMP) and TGF-β. TGF-β down regulates the expression of IL-1 receptor (Boumediene et al. 1998) in cultured articular chondrocytes suggesting that TGF-β may be crucial for cartilage homeostasis. This is supported by studies showing that expression of TGF-β receptor II (TGF-βRII) in articular cartilage is dramatically depressed in the rabbit model of OA (Boumediene et al. 1998), and transgenic mice expressing inactive TGF-βRII develop lesions similar to human OA (Serra et al. 1997). OA cartilage break down not only involves IL-1β over-expression but also reduced responsiveness of chondrocytes to TGF-β (Serra et al. 1997). Recently, EGCG was shown to exert a stimulatory effect on TGF-β1, TGF-β2, TGF-βRI and TGF-βRII expression in the presence of IL-1 in mice (Andriamanalijaona et al. 2005). This suggests that EGCG has the potential to prevent the inhibition of TGF-β2 expression and its receptors in diseases such as OA where IL-1β-induced non-responsiveness of chondrocytes to TGF-β may be associated with the absence of cartilage repair (Andriamanalijaona et al. 2005).
Suppression of osteoclast differentiation
Local bone erosion is one of the essential pathological features of RA and osteoclasts seems to play a major role in bone erosion in joints, as evidenced by the lack of bone erosion in experimental arthritis in osteoclast deficient mice (Redlich et al. 2002). Osteoclasts are tartrateresistent acid phosphatase-positive cells in inflamed joints of RA patients (Redlich et al. 2002). Macrophage colony-stimulating factor (M-CSF) and RA synovial fibroblasts produce RANKL which is an essential cytokine for osteoclast development (Teitelbaum et al. 2003). Thus, inhibiting osteoclast development or suppressing M-CSF or RANKL expression in an inflamed joint may be an optimal approach for reducing bone erosion in RA joints (Sato and Takayanagi 2006). EGCG has been shown to be a potent inhibitor of osteoclast development in vitro and in vivo by suppressing the mRNA expression of osteoclast related molecules such as calcitonin receptor, cathepsin H,αv and β3 integrins (Lin et al. 2009; Lee et al. 2010; Morinobu et al. 2008). EGCG selectively down-regulates RANKL induced nuclear factor of activated T cell c1 (NF-ATc1), a transcription factor involved in osteoclast differentiation (Morinobu et al. 2008) suggesting that use of EGCG may be beneficial in suppressing osteoclasts development and activity in arthritic joints.
Antioxidant effects of EGCG in arthritis
Cells of the joint tissue, including chondrocytes, possesses an elaborate antioxidant defense system to cope with the physiological production of ROS and reactive nitrogen species (RNS) and the resulting oxidative stress (Baker et al. 1988). However, excessive and chronic production of ROS and RNS can overwhelm the system and result in oxidative damage to the tissue architecture. Oxygen free radicals in excessive quantities have been identified in synovial fluid of 90% of patients with RA (Kurien et al. 2006). Cytokines such as IL-1β and TNF-α known to stimulate chondrocytes and synoviocytes to produce high levels of oxygen free radicals (superoxide and hydroxyl radicals) and non-radical species (hydrogen peroxide) (Henrotin et al. 1993). ROS and oxidatively modified proteins and DNA are important mediator in the pathogenesis of arthritic diseases as they modulate intracellular signaling pathways and pro-inflammatory cytokine gene activation and expression (Lo et al. 1996). Several studies have shown that EGCG blunts ROS mediated cytotoxicity in human chondrocytes and other models of oxidative stress (Lo et al.1996; Song et al. 2002; Nie et al. 2002; Bordoni et al. 2002). Investigations from a number of laboratories have demonstrated that green tea polyphenols are efficient free radical and singlet oxygen scavengers (Kurien 1998). Therefore one possible mechanism of the observed chondro-protective effect of EGCG may be the direct ROS scavenging from both intra-cellular and extra-cellular environment. It is now known that the infiltrating leucocytes in arthritic lesions are the major source of NO and H2O2 production (Borsiczky et al. 2003) and this can create oxidative stress in the tissue microenvironment. Exposure of different cell types to H2O2 activates the MAPKs and H2O2-induced activation of MAPKs was inhibited when these cells were pretreated with EGCG indicating that EGCG has the potential to inhibit oxidative stress-mediated phosphorylation and activation of MAPKs in cell types directly relevant to inflammation (Katiyar et al. 2001; Meng et al. 2001). EGCG also considerably increased the gene expressions of catalase, superoxide dismutase, and glutathione peroxidase activities which are essential components of a robust anti-oxidant defense system (Meng et al. 2001). Oxidation of lysine, arginine and proline leads to the formation of carbonyl derivatives that affect the nature and function of the proteins. The presence of carbonylated proteins has become a widely accepted measure of oxidative damage of proteins under conditions of oxidative stress. Elevated blood carbonylated proteins and malondialdehyde with lower levels of blood concentrations of total thiols, glutathione and vitamin C is observed in RA patients and in animal models of arthritis (Kalavacherla et al. 1994; Choi 2007). Shift in the oxidant/antioxidant balance in favor of lipid peroxidation could lead to the tissue damage observed in the disease. A statistically significant increase in the concentration of antioxidants, along with a decrease in the concentration of malondialdehyde was found in RA patients after adjunct treatment with EGCG (Jaswal et al. 2000). Studies have also shown that antioxidant nutrients do protect against cartilage degradation in OA (Tiku et al. 1999; McAlindon et al. 1996). The antioxidant activity of EGCG is also due to its ability to affect the enzyme activity of the antioxidant system (McAlindon et al. 1996). Thus, consumption of a potent anti-oxidant such as EGCG may be helpful in protecting joints from oxidative damage associated with chronic inflammation in arthritis.
Metabolism and Bioavailability of Green Tea Constituents
Methylation, glucuronidation and sulfation of catechins present in the green tea have been observed. In an in vitro study when EGCG was incubated with rat, human or mouse liver microsomes and different human UGT isozymes 6 EGCG glucuronides, namely 4’-O—methyl-EGCG-glucuronide, 4’,4”-di-O-methyl-EGCG-glucuronide, EGCG-7-O-glucuronide, EGCG-3’-O-glucuronide, EGCG-3”-O-glucuronide, and EGCG-4”-O-glucuronide, with EGCG-4”-O-glucuronide being the major metabolite, were produced in all of the incubations (de Mejia and Ramirez-Mares 2009). Green tea catechins are sparsely absorbed in the small intestine and appear to pass through the biological membranes and are absorbed without deconjugation or hydrolysis. The low absorption of green tea catechins suggests that the majority of catechins, including EGCG, will reach the large intestine where the glycosides will be hydrolyzed into aglycones and various aromatic acids by the microflora (Nakagawa and Miyazawa 1997). Due to their relatively low absorption, rapid metabolism and elimination from the body, consumption of large amounts of flavonols is well tolerated by the humans. At present the safe upper limit for chronic ingestion is about 1 gram of flavonols/day (de Mejia and Ramirez-Mares 2009). The health benefits of tea consumption in preventing cancer has been intensively investigated (Khan and Mukhtar 2008; Schneider and Segre 2009). However, limited information is available about the protective effect of consumption of green tea or its bioactive components in arthritis.
The bioavailability of EGCG or other catechins is relatively low and this may be due to the short half-life which ranges from 1.87 to 4.58 hours from a 50- to 1600-mg dose (approximately 0.7–23 mg/kg body weight, based on 70 kg body weight) (Ullmann et al. 2003). This might be overcome by repeated administration of EGCG because of its reported low toxicity and high tolerance by human subjects, even when given in doses as high as 1600 mg (vanhet Hof et al. 1999). Drinking one cup of green tea could lead to a level of EGCG of 1 µmol/L in the circulation (vanhet Hof et al. 1999). EGCG at physiological concentrations of 0.1 and 1 µM increased the mRNA expression of the anti-inflammatory cytokine IL-13 by 2.25-and 2.87-fold respectively (Wu et al. 2009). In other studies relevant to arthritis EGCG showed inhibition of T cell proliferation at 2.5 to 10 µM concentration without inducing cytotoxicity or apoptosis (Wu et al. 2009) and a 1600-mg oral dose of EGCG under fasting conditions has been reported to achieve a maximum human plasma level of 7.6 µmol/L (Ullmann et al. 2003). This level is 8 times higher than the highest reported from daily intake of green tea infusion (Ullmann et al. 2003). Further, other factors may be involved in differential response of different human populations to EGCG or other catechins. These may include inter individual variation in the bioavailability of the polyphenols after oral consumption can be substantial due to genetic polymorphism in the enzymes involved in polyphenol metabolism. However, these studies do point out that pharmaceutically prepared formulation of green tea catechins could reach plasma levels equivalent to doses that have been found effective in vitro for the inhibition of inflammatory and joint degrading activities of molecules that are over expressed in arthritis.
Harmful effects of green tea consumption
Tea consumption in general has not displayed any acute or chronic toxic effects, and in fact, it is health promoting. Schwarz et al. (1994) described regular tea drinkers as individuals with a generally healthy lifestyle. However, harmful effects of green tea over consumption could be due to two main factors including (i) caffeine content and (ii) presence of aluminum. Regarding caffeine content, a daylong consumption of green tea improved the cognitive and psychomotor performance of healthy adult in a manner similar to coffee, but green tea contain less caffeine than coffee and is less likely to disrupt sleep quality at night. A cup of green tea contains 40–55 mg caffeine while a cup of coffee has 125–150 mg of caffeine (Willson 1999; McKay and Blumberg 2002). Although, green tea caffeine content is low, the negative effects produced by the overconsumption of caffeine may include nervousness, sleep disorder, vomits, headaches, tachycardia (Bruneton 2001). Studies have also shown that green tea plant has high capacity to accumulate aluminum. Minoia et al. (1994) found concentration of aluminum in green tea (as infusions) accounting for 431–2239 µg/L, which is higher than aluminum concentration of coffee (30.8 µg/L). This knowledge in cases is important of renal failure because aluminum accumulated by the body may results in neurological disorders; therefore drinking green tea of these patients may be counter indicated (Costa et al. 2002). However, black tea contain six fold more aluminum than green tea (Costa et al. 2002) and obviously its consumption too by patients with renal failure should be avoided.
Conclusions
Naturally occurring substances that are derived from diet provide new approaches to the development of therapeutics for chronic diseases like OA and RA. Green tea is regarded as one of the most promising dietary agents for the prevention and treatment of many chronic diseases. Experimental evidence documenting the health maintenance properties of green tea and its constituents is on the rise. EGCG is the predominant polyphenol in green tea and is regarded as the most active catechin of green tea. Numerous in vitro and in vivo studies have demonstrated that EGCG possesses potent antioxidant and anti-inflammatory activity as it inhibits the activation of MAPKs, AP-1, and NF-κB in different cell types. However, it is becoming clear that the anti-inflammatory effects of EGCG or green tea may be mediated via abrogation of different pathways associated with adjunct inflammatory response. Any single, several, or all the reported biological pathways may yield benefit to reduce the risk of inflammation in OA and RA. Pharmaceutical preparations of EGCG may deliver the in vivo dose equivalent to the concentration used in vitro and may be effective in suppressing inflammation and the catabolic response in arthritic joints. Based on studies reported here use of green tea polyphenols may provide an effective strategy for inhibiting disease progression in OA and RA.
Acknowledgements
This work was supported in part by National Institute of Health/National Centre for Complimentary and Alternative Medicine grant RO1-AT-003267 and R21-AT504615.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors declare that there is no conflict of interest.
References
- Ahmad N, Gupta S, Mukhtar H. Green tea polyphenol epigallocatechin-3-gallate differentially modulates nuclear factor κB in cancer cells versus normal cells. Archives of Biochemistry and Biophysics. 2000;376(2):338–346. doi: 10.1006/abbi.2000.1742. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Anuntiyo J, Malemud CJ, Haqqi TM. Biological basis for the use of botanicals in osteoarthritis and rheumatoid arthritis: a review. Evidence Based Complementary and Alternative Medicine. 2005;2(3):301–308. doi: 10.1093/ecam/neh117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S, Marotte H, Kwan K, Ruth JH, Campbell PL, Rabquer BJ, Pakozdi A, Koch AE. Epigallocatechin-3-gallate inhibits IL-6 synthesis and suppresses transsignaling by enhancing soluble gp130 production. Proceedings of National Academy of Science U S A. 2008;105(38):14692–14697. doi: 10.1073/pnas.0802675105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S, Pakozdi A, Koch AE. Regulation of interleukin-1beta-induced chemokine production and matrix metalloproteinase 2 activation by epigallocatechin-3-gallate in rheumatoid arthritis synovial fibroblasts. Arthritis & Rheumatism. 2006;54(8):2393–2401. doi: 10.1002/art.22023. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Pakozdi A, Koch AE. Regulation of interleukin-1beta-induced chemokine production and matrix metalloproteinase 2 activation by epigallocatechin-3-gallate in rheumatoid arthritis synovial fibroblasts. Arthritis & Rheumatism. 2003;54(8):2393–2401. doi: 10.1002/art.22023. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Rahman A, Hasnain A, Lalonde M, Goldberg VM, Haqqi TM. Green tea polyphenol epigallocatechin-3-gallate inhibits the IL-1 beta-induced activity and expression of cyclooxygenase-2 and nitric oxide synthase-2 in human chondrocytes. Free Radical Biology & Medicine. 2002;33(8):1097–1105. doi: 10.1016/s0891-5849(02)01004-3. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Silverman MD, Marotte H, Kwan K, Matuszczak N, Koch AE. Down-regulation of myeloid cell leukemia 1 by epigallocatechin-3-gallate sensitizes rheumatoid arthritis synovial fibroblasts to tumor necrosis factor alpha-induced apoptosis. Arthritis & Rheumatism. 2009;60(5):1282–1293. doi: 10.1002/art.24488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S, Wang N, Lalonde M, Goldberg VM, Haqqi TM. Green tea polyphenol epigallocatechin-3-gallate (EGCG) differentially inhibits interleukin-1 beta-induced expression of matrix metalloproteinase-1 and -13 in human chondrocytes. Journal of Pharmacology and Experimental Therapeutics. 2004;308(2):767–773. doi: 10.1124/jpet.103.059220. [DOI] [PubMed] [Google Scholar]
- Aktas O, Prozorovski T, Smorodchenko A, Savaskan NE, Lauster R, Kloetzel PM, Infante-Duarte C, Brocke S, Zipp F. Green tea epigallocatechin-3-gallate mediates T cellular NF-kappa B inhibition and exerts neuroprotection in autoimmune encephalomyelitis. The Journal of Immunology. 2004;173(9):5794–5800. doi: 10.4049/jimmunol.173.9.5794. [DOI] [PubMed] [Google Scholar]
- Alkharfy KM, Kellum JA, Matzke GR. Unintended immunomodulation: part II. Effects of pharmacological agents on cytokine activity. Shock. 2000;13(5):346–360. doi: 10.1097/00024382-200005000-00002. [DOI] [PubMed] [Google Scholar]
- Altman RD. Practical considerations for the pharmacologic management of osteoarthritis. American Journal of Managed Care. 2009;15(8):S236–S243. [PubMed] [Google Scholar]
- Andriamanalijaona R, Kypriotou M, Baugé C, Renard E, Legendre F, Raoudi M, Boumediene K, Gatto H, Monginoux P, Pujol JP. Comparative effects of 2 antioxidants, selenomethionine and epigallocatechin-gallate, on catabolic and anabolic gene expression of articular chondrocytes. The Journal of Rheumatology. 2005;32(10):1958–1967. [PubMed] [Google Scholar]
- Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Practice & Research: Clinical Rheumatology. 2006;20(1):3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Bae JY, Choi JS, Choi YJ, Shin SY, Kang SW, Han SJ, Kang YH. (-)Epigallocatechin gallate hampers collagen destruction and collagenase activation in ultraviolet-B-irradiated human dermal fibroblasts: involvement of mitogen-activated protein kinase. Food and Chemical Toxicology. 2008;46(4):1298–1307. doi: 10.1016/j.fct.2007.09.112. [DOI] [PubMed] [Google Scholar]
- Baker MS, Feigan J, Lowther DA. Chondrocyte antioxidant defences: the roles of catalase and glutathione peroxidase in protection against H2O2 dependent inhibition of proteoglycan biosynthesis. The Journal of Rheumatology. 1988;15(4):670–677. [PubMed] [Google Scholar]
- Belitz DH, Grosh W. Quimica de los Alientos. Zaragosa: Acribia; 1997. [Google Scholar]
- Bordoni A, Hrelia S, Angeloni C, Giordano E, Guarnieri C, Caldarera CM, Biagi PL. Green tea protection of hypoxia/reoxygenation injury in cultured cardiac cells. The Journal of Nutritional Biochemistry. 2002;13(2):103–111. doi: 10.1016/s0955-2863(01)00203-0. [DOI] [PubMed] [Google Scholar]
- Borsiczky B, Szabó Z, Jaberansari MT, Mack PP, Röth E. Activated PMNs lead to oxidative stress on chondrocytes: a study of swine knees. Acta Orthopaedica Scandinavica. 2003;74(2):190–195. doi: 10.1080/00016470310013941. [DOI] [PubMed] [Google Scholar]
- Boumediene K, Conrozier T, Mathieu P, Richard M, Marcelli C, Vignon E, Pujol JP. Decrease of cartilage transforming growth factor-beta receptor II expression in the rabbit experimental osteoarthritis--potential role in cartilage breakdown. Osteoarthritis and Cartilage. 1998;6(2):146–149. doi: 10.1053/joca.1997.0104. [DOI] [PubMed] [Google Scholar]
- Braddock M, Quinn A. Targeting IL-1 in inflammatory disease: new opportunity for therapeutic intervention. Nature Review Drug Discovery. 2004;3:330–335. doi: 10.1038/nrd1342. [DOI] [PubMed] [Google Scholar]
- Brown SL, Greene MH, Gershon SK, Edwards ET, Braun MM. Tumor necrosis factor antagonist therapy and lymphoma development: twenty-six cases reported to the Food and Drug Administration. Arthritis & Rheumatism. 2002;46(12):3151–3158. doi: 10.1002/art.10679. [DOI] [PubMed] [Google Scholar]
- Bruneton J. Pharmacognosie, Phytochimie, Plantes Medicina-les. Paris: Technique et Documentation-Lavoisier; 2001. [Google Scholar]
- Cabrera C, Giménez R, López MC. Determination of tea components with antioxidant activity. Journal of Agriculture and Food Chemistry. 2003;51(15):4427–4435. doi: 10.1021/jf0300801. [DOI] [PubMed] [Google Scholar]
- Carbera C, Artacho R, Gimenez R. Beneficial effects of green tea-A review. Journal of the American College of Nutrition. 2006;25(2):79–99. doi: 10.1080/07315724.2006.10719518. [DOI] [PubMed] [Google Scholar]
- Chan FK, Cryer B, Goldstein JL, Lanas A, Peura DA, Scheiman JM, Simon LS, Singh G, Stillman MJ, Wilcox CM, Berger MF, Breazna A, Dodge W. A novel composite endpoint to evaluate the gastrointestinal (GI) effects of nonsteroidal antiinflammatory drugs through the entire GI tract. The Journal of Rheumatology. 2010;37(1):167–174. doi: 10.3899/jrheum.090168. [DOI] [PubMed] [Google Scholar]
- Chan MM, Fong D, Ho CT, Huang HI. Inhibition of inducible nitric oxide synthase gene expression and enzyme activity by epigallocatechin gallate, a natural product from green tea. Biochemical Pharmacology. 1997;54(12):1281–1286. doi: 10.1016/s0006-2952(97)00504-2. [DOI] [PubMed] [Google Scholar]
- Cheng KW, Wong CC, Chao J, Lo C, Chen F, Chu IK, Che CM, Ho CT, Wang M. Inhibition of mutagenic PhIP formation by epigallocatechin gallate via scavenging of phenylacetaldehyde. Molecular Nutrition & Food Research. 2009;53(6):716–725. doi: 10.1002/mnfr.200800206. [DOI] [PubMed] [Google Scholar]
- Cheng XW, Kuzuya M, Kanda S, Maeda K, Sasaki T, Wang QL, Tamaya-Mori N, Shibata T, Iguchi A. Epigallocatechin-3-gallate binding to MMP-2 inhibits gelatinolytic activity without influencing the attachment to extracellular matrix proteins but enhances MMP-2 binding to TIMP-2. Archives of Biochemistry and Biophysics. 2003;415(1):126–132. doi: 10.1016/s0003-9861(03)00221-2. [DOI] [PubMed] [Google Scholar]
- Choi EM. Oxidative status of DBA/1J mice with type II collagen-induced arthritis. Journal of Applied Toxicology. 2007;27(5):472–481. doi: 10.1002/jat.1228. [DOI] [PubMed] [Google Scholar]
- Chowdhury TT, Salter DM, Bader DL, Lee DA. Signal transduction pathways involving p38 MAPK, JNK, NFkappaB and AP-1 influences the response of chondrocytes cultured in agarose constructs to IL-1beta and dynamic compression. Inflammation Research. 2008;57(7):306–313. doi: 10.1007/s00011-007-7126-y. [DOI] [PubMed] [Google Scholar]
- Choy EH, Isenberg DA, Garrood T, Farrow S, Ioannou Y, Bird H, Cheung N, Williams B, Hazleman B, Price R, Yoshizaki K, Nishimoto N, Kishimoto T, Panayi GS. Therapeutic benefit of blocking interleukin-6 activity with an anti-interleukin-6 receptor monoclonal antibody in rheumatoid arthritis: a randomized, double-blind, placebo-controlled, dose-escalation trial. Arthritis & Rheumatism. 2002;46(12):3143–3150. doi: 10.1002/art.10623. [DOI] [PubMed] [Google Scholar]
- Chung JY, Huang C, Meng X, Dong Z, Yang CS. Inhibition of activator protein 1 activity and cell growth by purified green tea and black tea polyphenols in H-ras-transformed cells: structure-activity relationship and mechanisms involved. Cancer Research. 1999;59(18):4610–4617. [PubMed] [Google Scholar]
- Corps AN, Curry VA, Buttle DJ, Hazleman BL, Riley GP. Inhibition of interleukin-1beta-stimulated collagenase and stromelysin expression in human tendon fibroblasts by epigallocatechin gallate ester. Matrix Biology. 2004;23(3):163–169. doi: 10.1016/j.matbio.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Costa LM, Gouveia ST, Nobrega JA. Comparision of heating exraction procedures for Al, Ca, Mg and Mn in tea samples. Annals of Sciences. 2002;18:313–318. doi: 10.2116/analsci.18.313. [DOI] [PubMed] [Google Scholar]
- Danesi F, Philpott M, Huebner C, Bordoni A, Ferguson LR. Food-derived bioactives as potential regulators of the IL-12/IL-23 pathway implicated in inflammatory bowel diseases. Mutation Research Epub ahead of print. 2010 doi: 10.1016/j.mrfmmm.2010.01.001. [DOI] [PubMed] [Google Scholar]
- de Hooge AS, van de Loo FA, Koenders MI, Bennink MB, Arntz OJ, Kolbe T, van den Berg WB. Local activation of STAT-1 and STAT-3 in the inflamed synovium during zymosan-induced arthritis: exacerbation of joint inflammation in STAT-1 gene-knockout mice. Arthritis & Rheumatism. 2004;50(6):2014–2023. doi: 10.1002/art.20302. [DOI] [PubMed] [Google Scholar]
- de Mejia EG, Ramirez-Mares MV, Puangpraphant S. Bioactive components of tea: cancer, inflammation and behavior. Brain Behavior & Immunology. 2009;23(6):721–731. doi: 10.1016/j.bbi.2009.02.013. [DOI] [PubMed] [Google Scholar]
- De Rienzo F, Saxena P, Filomia F, Caselli G, Colace F, Stasi L, Giordani A, Menziani MC. Progress towards the identification of new aggrecanase inhibitors. Current Medicinal Chemistry. 2009;16(19):2395–2415. doi: 10.2174/092986709788682092. [DOI] [PubMed] [Google Scholar]
- Donà M, Dell'Aica I, Calabrese F, Benelli R, Morini M, Albini A, Garbisa S. Neutrophil restraint by green tea: inhibition of inflammation, associated angiogenesis, and pulmonary fibrosis. The Journal of Immunology. 2003;170(8):4335–4341. doi: 10.4049/jimmunol.170.8.4335. [DOI] [PubMed] [Google Scholar]
- East CJ, Stanton H, Golub SB, Rogerson FM, Fosang AJ. ADAMTS-5 deficiency does not block aggrecanolysis at preferred cleavage sites in the chondroitin sulfate-rich region of aggrecan. The Journal of Biological Chemistry. 2007;282(12):8632–8640. doi: 10.1074/jbc.M605750200. [DOI] [PubMed] [Google Scholar]
- Farrell AJ, Blake DR, Palmer RM, Moncada S. Increased concentrations of nitrite in synovial fluid and serum samples suggest increased nitric oxide synthesis in rheumatic diseases. Annals of Rheumatic Diseases. 1992;51(11):1219–1222. doi: 10.1136/ard.51.11.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feist E, Burmester GR. Is tocilizumab in combination with traditional DMARDs safe and effective for patients with active RA? Nature Clinical Practice Rheumatology. 2009;5(3):128–129. doi: 10.1038/ncprheum1005. [DOI] [PubMed] [Google Scholar]
- Feldman M, Maini RN. Anti-TNF-a therapy of rheumatoid arthritis: what have we learned. Annual Review of Immunology. 2001;19:163–169. doi: 10.1146/annurev.immunol.19.1.163. [DOI] [PubMed] [Google Scholar]
- Frei B, Higdon JV. Antioxidant activity of tea polyphenols in vivo: evidence from animal studies. The Journal of Nutrition. 2003;133(10):3275S–3284S. doi: 10.1093/jn/133.10.3275S. [DOI] [PubMed] [Google Scholar]
- Fujiki H, Suganuma M, Kurusu M, Okabe S, Imayoshi Y, Taniguchi S, Yoshida T. New TNF-alpha releasing inhibitors as cancer preventive agents from traditional herbal medicine and combination cancer prevention study with EGCG and sulindac or tamoxifen. Mutation Research. 2003;523–524:119–125. doi: 10.1016/s0027-5107(02)00327-5. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Fuentes AM, Green DM, Rossen RD, Ng B. Intra-articular hyaluronic acid increases cartilage breakdown biomarker in patients with knee osteoarthritis. Clinical Rheumatology, Epub ahead of print. 2010 doi: 10.1007/s10067-010-1376-8. [DOI] [PubMed] [Google Scholar]
- Goodridge HS, Harnett W, Liew FY, Harnett MM. Differential regulation of interleukin-12 p40 and p35 induction via Erk mitogen-activated protein kinase-dependent and -independent mechanisms and the implications for bioactive IL-12 and IL-23 responses. Immunology. 2003;109(3):415–425. doi: 10.1046/j.1365-2567.2003.01689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafeez BB, Ahmed S, Wang N, Gupta S, Zhang A, Haqqi TM. Green tea polyphenols-induced apoptosis in human osteosarcoma SAOS-2 cells involves a caspase-dependent mechanism with downregulation of nuclear factor-kappaB. Toxicology and Applied Pharmacology. 2006;216(1):11–19. doi: 10.1016/j.taap.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Haqqi TM, Anthony DD, Gupta S, Ahmad N, Lee MS, Kumar GK, Mukhtar H. Prevention of collagen-induced arthritis in mice by a polyphenolic fraction from green tea. Proceedings of National Academy of Science U S A. 1999;96(8):4524–4529. doi: 10.1073/pnas.96.8.4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, Takai S, Matsushima-Nishiwaki R, Hanai Y, Kato K, Tokuda H, Kozawa O. (-)-Epigallocatechin gallate reduces transforming growth factor beta-stimulated HSP27 induction through the suppression of stress-activated protein kinase/c-Jun N-terminal kinase in osteoblasts. Life Sciences. 2008;82(19–20):1012–1017. doi: 10.1016/j.lfs.2008.02.017. [DOI] [PubMed] [Google Scholar]
- Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, Liang MH, Kremers HM, Mayes MD, Merkel PA, Pillemer SR, Reveille JD, Stone JH. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part I. Arthritis & Rheumatism. 2007;58(1):15–25. doi: 10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- Henrotin Y, Deby-Dupont G, Deby C, De Bruyn M, Lamy M, Franchimont P. Production of active oxygen species by isolated human chondrocytes. British Journal of Rheumatology. 1993;32(7):562–567. doi: 10.1093/rheumatology/32.7.562. [DOI] [PubMed] [Google Scholar]
- Hommes DW, Peppelenbosch MP, Von Deventer SJH. Mitogen activated protein (MAP) kinase signal transduction pathways and novel anti-inflammatory targets. Gut. 2003;52:144–151. doi: 10.1136/gut.52.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong MH, Kim MH, Chang HJ, Kim NH, Shin BA, Ahn BW, Jung YD. (-)-Epigallocatechin-3-gallate inhibits monocyte chemotactic protein-1 expression in endothelial cells via blocking NF-kappaB signaling. Life Sciences. 2007;80(21):1957–1965. doi: 10.1016/j.lfs.2007.02.024. [DOI] [PubMed] [Google Scholar]
- Hosokawa Y, Hosokawa I, Ozaki K, Nakanishi T, Nakae H, Matsuo T. Catechins inhibit CXCL10 production from oncostatin M-stimulated human gingival fibroblasts. The Journal of Nutritional Biochemistry Epub ahead of print. 2009 doi: 10.1016/j.jnutbio.2009.04.005. [DOI] [PubMed] [Google Scholar]
- Hsiao FY, Tsai YW, Huang WF. Changes in physicians' practice of prescribing cyclooxygenase-2 inhibitor after market withdrawal of rofecoxib: A retrospective study of physician-patient pairs in Taiwan. Clinical Therapy. 2009;31(11):2618–2627. doi: 10.1016/j.clinthera.2009.11.022. [DOI] [PubMed] [Google Scholar]
- Huang GS, Tseng CY, Lee CH, Su SL, Lee HS. Effects of (-)-epigallocatechin-3-gallate on cyclooxygenase 2, PGE(2), and IL-8 expression induced by IL-1beta in human synovial fibroblasts. Rheumatology International, Epub ahead of print. 2009 doi: 10.1007/s00296-009-1128-8. [DOI] [PubMed] [Google Scholar]
- Ichikawa D, Matsui A, Imai M, Sonoda Y, Kasahara T. Effect of various catechins on the IL-12p40 production by murine peritoneal macrophages and a macrophage cell line, J774.1. Biological & Pharmaceutical Bulletin. 2004;27(9):1353–1358. doi: 10.1248/bpb.27.1353. [DOI] [PubMed] [Google Scholar]
- Igaz P, Toth S, Falus A. Biological and clinical signifi cance of the JAK-STAT pathway: lessons from knockout mice. Inflammation Research. 2001;50:435–441. doi: 10.1007/PL00000267. [DOI] [PubMed] [Google Scholar]
- Jaswal S, Mehta HC, Sood AK, Kaur J. Antioxidant status in rheumatoid arthritis and role of antioxidant therapy. Clinical Chemica Acta. 2000;338:123–129. doi: 10.1016/j.cccn.2003.08.011. [DOI] [PubMed] [Google Scholar]
- Johnson GL, Lapadat R. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science. 2002;298:1911–1916. doi: 10.1126/science.1072682. [DOI] [PubMed] [Google Scholar]
- Johnson JJ, Bailey HH, Mukhtar H. Green tea polyphenols for prostate cancer chemoprevention: a translational perspective. Phytomedicine. 2010;17(1):3–13. doi: 10.1016/j.phymed.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalavacherla US, Ishaq M, Rao UR, Sachindranath A, Hepsiba T. Malondialdehyde as a sensitive marker of inflammation in patients with rheumatoid arthritis. Journal of Association of Physicians India. 1994;42(10):775–776. [PubMed] [Google Scholar]
- Karin M, Ben-Neriah Y. Phosphorylation meets ubiqutination:the control of NFκB activity. Annual Reviews of Immunology. 2000;18:621–626. doi: 10.1146/annurev.immunol.18.1.621. [DOI] [PubMed] [Google Scholar]
- Kasperkovitz PV, Verbeet NL, Smeets TJ, van Rietschoten JG, Kraan MC, van der Pouw Kraan TC, Tak PP, Verweij CL. Activation of the STAT1 pathway in rheumatoid arthritis. Annals of Rheumatic Diseases. 2004;63(3):233–239. doi: 10.1136/ard.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katiyar SK, Afaq F, Azizuddin K, Mukhtar H. Inhibition of UVB-induced oxidative stress-mediated phosphorylation of mitogen-activated protein kinase signaling pathways in cultured human epidermal keratinocytes by green tea polyphenol (-)-epigallocatechin-3-gallate. Toxicology and Applied Pharmacology. 2001;176(2):110–117. doi: 10.1006/taap.2001.9276. [DOI] [PubMed] [Google Scholar]
- Kawai K, Tsuno NH, Kitayama J, Okaji Y, Yazawa K, Asakage M, Hori N, Watanabe T, Takahashi K, Nagawa H. Epigallocatechin gallate attenuates adhesion and migration of CD8+ T cells by binding to CD11b. Journal of Allergy and Clinical Immunology. 2004;113(6):1211–1217. doi: 10.1016/j.jaci.2004.02.044. [DOI] [PubMed] [Google Scholar]
- Kawase M, Wang R, Shiomi T, Saijo R, Yagi K. Antioxidative activity of (-)-epigallocatechin-3-(3"-O-methyl)gallate isolated from fresh tea leaf and preliminary results on its biological activity. Biosci Biotechnol Biochem. 2000 Oct;64(10):2218–2220. doi: 10.1271/bbb.64.2218. [DOI] [PubMed] [Google Scholar]
- Khan N, Mukhtar H. Multitargeted therapy of cancer by green tea polyphenols. Cancer Letters. 2008;269(2):269–280. doi: 10.1016/j.canlet.2008.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim IB, Kim DY, Lee SJ, Sun MJ, Lee MS, Li H, Cho JJ, Park CS. Inhibition of IL-8 production by green tea polyphenols in human nasal fibroblasts and A549 epithelial cells. Biological & Pharmaceutical Bulletin. 2006;29(6):1120–1125. doi: 10.1248/bpb.29.1120. [DOI] [PubMed] [Google Scholar]
- Koeberle A, Bauer J, Verhoff M, Hoffmann M, Northoff H, Werz O. Green tea epigallocatechin-3-gallate inhibits microsomal prostaglandin E(2) synthase-1. Biochemical and Biophysics Research Communication. 2009;388(2):350–354. doi: 10.1016/j.bbrc.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Kraan PM, Berg WB. Anabolic and destructive mediators in osteoarthritis. Current Opinion in Clinical Nutrition & Metabolic Care. 2000;3:205–209. doi: 10.1097/00075197-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Kurien BT, Hensley K, Bachmann M, Scofield RH. Oxidatively modified autoantigens in autoimmune diseases. Free Radical Biology & Medicine. 2006;41(4):549–556. doi: 10.1016/j.freeradbiomed.2006.05.020. [DOI] [PubMed] [Google Scholar]
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis & Rheumatism. 2007;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AS, Jung YJ, Kim DH, Lee TH, Kang KP, Lee S, Lee NH, Sung MJ, Kwon DY, Park SK, Kim W. Epigallocatechin-3-O-gallate decreases tumor necrosis factor-alpha-induced fractalkine expression in endothelial cells by suppressing NF-kappaB. Cell Physiology & Biochemistry. 2009;24(5–6):503–510. doi: 10.1159/000257494. [DOI] [PubMed] [Google Scholar]
- Lee DM, Weinblatt ME. Rheumatoid arthritis. Lancet. 2001;358:903–911. doi: 10.1016/S0140-6736(01)06075-5. [DOI] [PubMed] [Google Scholar]
- Lee JH, Chung JH, Cho KH. The effects of epigallocatechin-3-gallate on extracellular matrix metabolism. Journal of Dermatology Science. 2005;40(3):195–204. doi: 10.1016/j.jdermsci.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Lee JH, Jin H, Shim HE, Kim HN, Ha H, Lee ZH. Epigallocatechin-3-gallate inhibits osteoclastogenesis by down-regulating c-Fos expression and suppressing the nuclear factor-kappaB signal. Molecular Pharmacology. 2010;77(1):17–25. doi: 10.1124/mol.109.057877. [DOI] [PubMed] [Google Scholar]
- Lee JH, Chung KY, Bang D, Lee KH. Searching for aging-related proteins in human dermal microvascular endothelial cells treated with anti-aging agents. Proteomics. 2006;6(4):1351–1361. doi: 10.1002/pmic.200500287. [DOI] [PubMed] [Google Scholar]
- Lin RW, Chen CH, Wang YH, Ho ML, Hung SH, Chen IS, Wang GJ. (-)-Epigallocatechin gallate inhibition of osteoclastic differentiation via NF-kappaB. Biochemical and Biophysics Research Communication. 2009;379(4):1033–1037. doi: 10.1016/j.bbrc.2009.01.007. [DOI] [PubMed] [Google Scholar]
- Lin SK, Chang HH, Chen YJ, Wang CC, Galson DL, Hong CY, Kok SH. Epigallocatechin-3-gallate diminishes CCL2 expression in human osteoblastic cells via up-regulation of phosphatidylinositol 3-Kinase/Akt/Raf-1 interaction: a potential therapeutic benefit for arthritis. Arthritis & Rheumatism. 2008;58(10):3145–3156. doi: 10.1002/art.23937. [DOI] [PubMed] [Google Scholar]
- Lin YL, Lin JK. (-)-Epigallocatechin-3-gallate blocks the induction of nitric oxide synthase by down-regulating lipopolysaccharide-induced activity of transcription factor nuclear factor-kappaB. Molecular Pharmacology. 1997;52(3):465–472. [PubMed] [Google Scholar]
- Lo YY, Wong JM, Cruz TF. Reactive oxygen species mediate cytokine activation of c-Jun NH2-terminal kinases. The Journal of Biological Chemistry. 1996;271(26):15703–15707. doi: 10.1074/jbc.271.26.15703. [DOI] [PubMed] [Google Scholar]
- Loeser RF. Chondrocyte integrin expression and function. Biorheology. 2000;37(1–2):109–116. [PubMed] [Google Scholar]
- Loeser RF. Integrins and cell signaling in chondrocytes. Biorheology. 2002;39(1–2):119–124. [PubMed] [Google Scholar]
- Malemud CJ, Islam N, Haqqi TM. Pathophysiological mechanisms in osteoarthritis lead to novel therapeutic strategies. Cells Tissues Organs. 2003;174(1–2):34–48. doi: 10.1159/000070573. [DOI] [PubMed] [Google Scholar]
- Marotte H, Ruth JH, Campbell PL, Koch AE, Ahmed S. Green tea extract inhibits chemokine production, but up-regulates chemokine receptor expression, in rheumatoid arthritis synovial fibroblasts and rat adjuvant-induced arthritis. Rheumatology (Oxford) 2009;49(3):467–479. doi: 10.1093/rheumatology/kep397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlindon TE, Jacques P, Zhang Y, Hannan MT, Aliabadi P, Weissman B, Rush D, Levy D, Felson DT. Do antioxidant micronutrients protect against the development and progression of knee osteoarthritis? Arthritis & Rheumatism. 1996;39(4):648–656. doi: 10.1002/art.1780390417. [DOI] [PubMed] [Google Scholar]
- McInnes IB, Liew FY. Cytokine networks--towards new therapies for rheumatoid arthritis. Nature Clinical Practice & Rheumatology. 2005;1(1):31–39. doi: 10.1038/ncprheum0020. [DOI] [PubMed] [Google Scholar]
- McKay DL, Blumberg JB. The role of tea in human health: An update. Journal of American College of Nutrition. 2002;21:1–13. doi: 10.1080/07315724.2002.10719187. [DOI] [PubMed] [Google Scholar]
- Melgarejo E, Medina MA, Sánchez-Jiménez F, Urdiales JL. Epigallocatechin gallate reduces human monocyte mobility and adhesion in vitro. British Journal of Pharmacology. 2009;58(7):1705–1712. doi: 10.1111/j.1476-5381.2009.00452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menegazzi M, Tedeschi E, Dussin D, De Prati AC, Cavalieri E, Mariotto S, Suzuki H. Anti-interferon gamma action of epigallocatechin-3-gallate mediated by specific inhibition of STAT1 activation. FASEB Journal. 2001;15(7):1309–1311. doi: 10.1096/fj.00-0519fje. [DOI] [PubMed] [Google Scholar]
- Meng Q, Velalar CN, Ruan R. Effects of epigallocatechin-3-gallate on mitochondrial integrity and antioxidative enzyme activity in the aging process of human fibroblast. Free Radical Biology & Medicine. 2001;44(6):1032–1041. doi: 10.1016/j.freeradbiomed.2007.11.023. [DOI] [PubMed] [Google Scholar]
- Mohammed FF, Smookler DS, Khokha R. Metalloproteinases, inflammation, and rheumatoid arthritis. Annals of Rheumatic Diseases. 2003;62(2):ii43–ii47. doi: 10.1136/ard.62.suppl_2.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möller B, Villiger PM. Inhibition of IL-1, IL-6, and TNF-alpha in immune-mediated inflammatory diseases. Springer Seminar in Immunopathology. 2006;27(4):391–408. doi: 10.1007/s00281-006-0012-9. [DOI] [PubMed] [Google Scholar]
- Moon HS, Lee HG, Choi YJ, Kim TG, Cho CS. Proposed mechanisms of (-)-epigallocatechin-3-gallate for anti-obesity. Chemo Biological Interaction. 2007;167(2):85–98. doi: 10.1016/j.cbi.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Morinobu A, Biao W, Tanaka S, Horiuchi M, Jun L, Tsuji G, Sakai Y, Kurosaka M, Kumagai S. (-)-Epigallocatechin-3-gallate suppresses osteoclast differentiation and ameliorates experimental arthritis in mice. Arthritis & Rheumatism. 2008;58(7):2012–2018. doi: 10.1002/art.23594. [DOI] [PubMed] [Google Scholar]
- Nakagawa K, Miyazawa T. Absorption and distribution of tea catechin, (-)-epigallocatechin-3-gallate, in the rat. Journal of Nutrition Science and Vitaminology (Tokyo) 1997;43(6):679–684. doi: 10.3177/jnsv.43.679. [DOI] [PubMed] [Google Scholar]
- Nakagawa T, Yokozawa T. Direct scavenging of nitric oxide and superoxide by green tea. Food and Chemical Toxicology. 2002;40(12):1745–1750. doi: 10.1016/s0278-6915(02)00169-2. [DOI] [PubMed] [Google Scholar]
- Nam S, Smith DM, Dou QP. Ester bond-containing tea polyphenols potently inhibit proteasome activity in vitro and in vivo. The Journal of Biological Chemistry. 2001;276(16):13322–13330. doi: 10.1074/jbc.M004209200. [DOI] [PubMed] [Google Scholar]
- Nanjo F, Goto K, Seto R, Suzuki M, Sakai M, Hara Y. Scavenging effects of tea catechins and their derivatives on 1,1-diphenyl-2-picrylhydrazyl radical. Free Radical Biology & Medicine. 1996;21(6):895–902. doi: 10.1016/0891-5849(96)00237-7. [DOI] [PubMed] [Google Scholar]
- Nelson J, McFerran NV, Pivato G, Chambers E, Doherty C, Steele D, Timson DJ. The 67 kDa laminin receptor: structure, function and role in disease. Bioscience Reproducion. 2008;28(1):33–48. doi: 10.1042/BSR20070004. [DOI] [PubMed] [Google Scholar]
- Netsch MI, Gutmann H, Aydogan C, Drewe J. Green tea extract induces interleukin-8 (IL-8) mRNA and protein expression but specifically inhibits IL-8 secretion in caco-2 cells. Planta Medicine. 2006;72(8):697–702. doi: 10.1055/s-2006-931597. [DOI] [PubMed] [Google Scholar]
- Nie G, Jin C, Cao Y, Shen S, Zhao B. Distinct effects of tea catechins on 6-hydroxydopamine-induced apoptosis in PC12 cells. Archives of Biochemistry and Biophysics. 2002;397(1):84–90. doi: 10.1006/abbi.2001.2636. [DOI] [PubMed] [Google Scholar]
- Nuti E, Casalini F, Avramova SI, Santamaria S, Cercignani G, Marinelli L, La Pietra V, Novellino E, Orlandini E, Nencetti S, Tuccinardi T, Martinelli A, Lim NH, Visse R, Nagase H, Rossello A. N-O-isopropyl sulfonamido-based hydroxamates: design, synthesis and biological evaluation of selective matrix metalloproteinase-13 inhibitors as potential therapeutic agents for osteoarthritis. Journal of Medicinal Chemistry. 2009;52(15):4757–4773. doi: 10.1021/jm900261f. [DOI] [PubMed] [Google Scholar]
- Okamoto H, Cujec TP, Yamanaka H, Kamatani N. Molecular aspects of rheumatoid arthritis: role of transcription factors. FEBS Journal. 2008;275(18):4463–4470. doi: 10.1111/j.1742-4658.2008.06582.x. [DOI] [PubMed] [Google Scholar]
- Osterburg A, Gardner J, Hyon SH, Neely A, Babcock G. Highly antibiotic-resistant Acinetobacter baumannii clinical isolates are killed by the green tea polyphenol (-)-epigallocatechin-3-gallate (EGCG) Clinical Microbiology and Infection. 2009;15(4):341–346. doi: 10.1111/j.1469-0691.2009.02710.x. [DOI] [PubMed] [Google Scholar]
- Otero M, Goldring MB. Cells of the synovium in rheumatoid arthritis. Chondrocytes. Arthritis Research & Therapy. 2007;9(5):220–226. doi: 10.1186/ar2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park G, Yoon BS, Moon JH, Kim B, Jun EK, Oh S. Green tea polyphenol epigallocatechin-3-gallate suppresses collagen production and proliferation in keloid fibroblasts via inhibition of the STAT3-signaling pathway. Journal of Investigative Dermatology. 2008;128:2429–2441. doi: 10.1038/jid.2008.103. [DOI] [PubMed] [Google Scholar]
- Penm E, Dixon T, Bhatia K. Health expenditure for arthritis and musculoskeletal conditions in Australia, 2000-01. Australian Institute of Health and Welfare. 2006 Bulletin no. 46 (catalogue no. AUS 83) [Google Scholar]
- Plumb GW, De Pascual-Teresa S, Santos-Buelga C, Cheynier V, Williamson G. Antioxidant properties of catechins and proanthocyanidins: effect of polymerisation, galloylation and glycosylation. Free Radical Research. 1998;29(4):351–358. doi: 10.1080/10715769800300391. [DOI] [PubMed] [Google Scholar]
- Poduval P, Sillat T, Virtanen I, Dabagh M, Konttinen Y. Immigration check for neutrophils in RA lining: laminin alpha5 low expression regions act as exit points. Scandinavian Journal of Rheumatology. 2010 doi: 10.3109/03009740903198980. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Porath D, Riegger C, Drewe J, Schwager J. Epigallocatechin-3-gallate impairs chemokine production in human colon epithelial cell lines. Journal of Pharmacology and Experimental Therapeutics. 2005;315(3):1172–1180. doi: 10.1124/jpet.105.090167. [DOI] [PubMed] [Google Scholar]
- Pujol JP. TGF-beta and osteoarthritis: in vivo veritas? Osteoarthritis and Cartilage. 1999;7(5):439–440. doi: 10.1053/joca.1999.0248. [DOI] [PubMed] [Google Scholar]
- Rasheed Z, Anbazhagan AN, Akhtar N, Ramamurthy S, Voss FR, Haqqi TM. Green tea polyphenol epigallocatechin-3-gallate inhibits advanced glycation end product-induced expression of tumor necrosis factor-alpha and matrix metalloproteinase-13 in human chondrocytes. Arthritis Research & Therapy. 2009;11(3):R71. doi: 10.1186/ar2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed Z, Haqqi TM. Updates on targets of biologic therapies for rheumatoid arthritis. Current Rheumatology Review. 2008;4:246–253. doi: 10.2174/157339708786263915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redlich K, Hayer S, Ricci R, David JP, Tohidast-Akrad M, Kollias G, Steiner G, Smolen JS, Wagner EF, Schett G. Osteoclasts are essential for TNF-alpha-mediated joint destruction. The Journal of Clinical Investigation. 2002;110(10):1419–1427. doi: 10.1172/JCI15582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards PJ, Nowell MA, Horiuchi S, McLoughlin RM, Fielding CA, Grau S. Functional characterization of a recombinant human soluble gp130 isoform and its therapeutic capacity in an experimental model of inflammatory arthritis. Arthritis & Rheumatism. 2006;54:1662–1672. doi: 10.1002/art.21818. [DOI] [PubMed] [Google Scholar]
- Saklatvala J. Inflammatory signaling in cartilage: MAPK and NF-kappaB pathways in chondrocytes and the use of inhibitors for research into pathogenesis and therapy of osteoarthritis. Current Drug Targets. 2007;8(2):305–313. doi: 10.2174/138945007779940115. [DOI] [PubMed] [Google Scholar]
- Sato K, Takayanagi H. Osteoclasts, rheumatoid arthritis, and osteoimmunology. Current Opinion in Rheumatology. 2006;18(4):419–426. doi: 10.1097/01.bor.0000231912.24740.a5. [DOI] [PubMed] [Google Scholar]
- Schett G, Tohidast-Akrad M, Smolen JS. Activation, differential localization, and regulation of the stress-activated protein kinases, extracellular signal-regulated kinase, c-JUN N terminal kinase, and p38 mitogen-activated protein kinase, in synovial tissue and cells in rheumatoid arthritis. Arthritis & Rheumatism. 2000;43:2501–2506. doi: 10.1002/1529-0131(200011)43:11<2501::AID-ANR18>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Schneider C, Segre T. Green tea: potential health benefits. American Family Physician. 2009;79(7):591–594. [PubMed] [Google Scholar]
- Schwarz B, Bischof HP, Kunze M. Coffee, tea and lifestyle. Preventive Medicine. 1994;23:377–384. doi: 10.1006/pmed.1994.1052. [DOI] [PubMed] [Google Scholar]
- Seemüller E, Lupas A, Stock D, Löwe J, Huber R, Baumeister W. Proteasome from Thermoplasma acidophilum: a threonine protease. Science. 1995;268(5210):579–582. doi: 10.1126/science.7725107. [DOI] [PubMed] [Google Scholar]
- Serra R, Johnson M, Filvaroff EH, LaBorde J, Sheehan DM, Derynck R, Moses HL. Expression of a truncated, kinase defective TGF-β type II receptor in mouse skeletal tissue promotes terminal chondrocyte differentiation and osteoarthritis. The Journal of Cell Biology. 1997;139:541–552. doi: 10.1083/jcb.139.2.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafini M, Ghiselli A, Ferro-Luzzi A. In vivo antioxidant effect of green and black tea in man. European Journal of Clinical Nutrition. 1996;50:28–32. [PubMed] [Google Scholar]
- Shen YJ, Li WG, Zhang H, Li B, Yuan HX, Zhang JJ. Effects of (-)-epigallocatechin-3-gallate on interleukin-1beta expression in mouse wound healing. Fen Zi Xi Bao Sheng Wu Xue Bao. 2009;42(3–4):179–185. [PubMed] [Google Scholar]
- Shin HY, Kim SH, Jeong HJ, Kim SY, Shin TY, Um JY, Hong SH, Kim HM. Epigallocatechin-3-gallate inhibits secretion of TNF-alpha, IL-6 and IL-8 through the attenuation of ERK and NF-kappaB in HMC-1 cells. International Archives of Allergy and Immunology. 2006;142(4):335–344. doi: 10.1159/000097503. [DOI] [PubMed] [Google Scholar]
- Singh R, Ahmed S, Islam N, Goldberg VM, Haqqi TM. Epigallocatechin-3-gallate inhibits interleukin-1beta-induced expression of nitric oxide synthase and production of nitric oxide in human chondrocytes: suppression of nuclear factor kappaB activation by degradation of the inhibitor of nuclear factor kappaB. Arthritis & Rheumatism. 2002;46(8):2079–2086. doi: 10.1002/art.10443. [DOI] [PubMed] [Google Scholar]
- Singh R, Ahmed S, Malemud CJ, Goldberg VM, Haqqi TM. Epigallocatechin-3-gallate selectively inhibits interleukin-1beta-induced activation of mitogen activated protein kinase subgroup c-Jun N-terminal kinase in human osteoarthritis chondrocytes. Journal of Orthopedic Research. 2003;21(1):102–109. doi: 10.1016/S0736-0266(02)00089-X. [DOI] [PubMed] [Google Scholar]
- Saeki K, Hayakawa S, Isemura M, Miyase T. Importance of a pyrogallol-type structure in catechin compounds for apoptosis-inducing activity. Phytochemistry. 2000;53(3):391–394. doi: 10.1016/s0031-9422(99)00513-0. [DOI] [PubMed] [Google Scholar]
- Slack J, McMahan CJ, Waugh S, Schooley K, Spriggs MK, Sims JE, Dower SK. Independent binding of interleukin-1 alpha and interleukin-1 beta to type I and type II interleukin-1 receptors. The Journal of Biological Chemistry. 1993;268(4):2513–2524. [PubMed] [Google Scholar]
- Smith A, Giunta B, Bickford PC, Fountain M, Tan J, Shytle RD. Nanolipidic particles improve the bioavailability and alpha-secretase inducing ability of epigallocatechin-3-gallate (EGCG) for the treatment of Alzheimer's disease. International Journal of Pharmacology. 2010 doi: 10.1016/j.ijpharm.2010.01.012. Epub ahead of publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GN., Jr The role of collagenolytic matrix metalloproteinases in the loss of articular cartilage in osteoarthritis. Frontiers in Biosciences. 2006;11:3081–3095. doi: 10.2741/2034. [DOI] [PubMed] [Google Scholar]
- Song DU, Jung YD, Chay KO, Chung MA, Lee KH, Yang SY, Shin BA, Ahn BW. Effect of drinking green tea on age-associated accumulation of Maillard-type fluorescence and carbonyl groups in rat aortic and skin collagen. Archives of Biochemistry and Biophysics. 2002;397(2):424–429. doi: 10.1006/abbi.2001.2695. [DOI] [PubMed] [Google Scholar]
- Sukhthankar M, Yamaguchi K, Lee SH, McEntee MF, Eling TE, Hara Y, Baek SJ. A green tea component suppresses posttranslational expression of basic fibroblast growth factor in colorectal cancer. Gastroenterology. 2008;134(7):1972–1980. doi: 10.1053/j.gastro.2008.02.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szekanecz Z, Koch AE. Therapeutic inhibition of leukocyte recruitment in inflammatory diseases. Current Opinion in Pharmacology. 2004;4(4):423–428. doi: 10.1016/j.coph.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tachibana H, Koga K, Fujimura Y, Yamada K. A receptor for green tea polyphenol EGCG. Nature Structural & Molecular Biology. 2004;11(4):380–381. doi: 10.1038/nsmb743. [DOI] [PubMed] [Google Scholar]
- Takita H, Kikuchi M, Sato Y, Kuboki Y. Inhibition of BMP-induced ectopic bone formation by an antiangiogenic agent (epigallocatechin 3-gallate) Connective Tissue Research. 2002;43(2–3):520–523. doi: 10.1080/03008200290000772. [DOI] [PubMed] [Google Scholar]
- Tedeschi E, Suzuki H, Menegazzi M. Antiinflammatory action of EGCG, the main component of green tea, through STAT-1 inhibition. Annals of New York Academy of Science. 2002;973:435–437. doi: 10.1111/j.1749-6632.2002.tb04678.x. [DOI] [PubMed] [Google Scholar]
- Teitelbaum SL, Ross FP. Genetic regulation of osteoclast development and function. Nature Review Genetics. 2003;4(8):638–649. doi: 10.1038/nrg1122. [DOI] [PubMed] [Google Scholar]
- Tiku ML, Gupta S, Deshmukh DR. Aggrecan degradation in chondrocytes is mediated by reactive oxygen species and protected by antioxidants. Free Radical Research. 1999;30(5):395–405. doi: 10.1080/10715769900300431. [DOI] [PubMed] [Google Scholar]
- Tokuda H, Takai S, Hanai Y, Matsushima-Nishiwaki R, Yamauchi J, Harada A, Hosoi T, Ohta T, Kozawa O. (-)-Epigallocatechin gallate inhibits basic fibroblast growth factor-stimulated interleukin-6 synthesis in osteoblasts. Hormone and Metabolic Research. 2008;40(10):674–678. doi: 10.1055/s-2008-1073164. [DOI] [PubMed] [Google Scholar]
- Tokuda H, Takai S, Matsushima-Nishiwaki R, Akamatsu S, Hanai Y, Hosoi T, Harada A, Ohta T, Kozawa O. (--)-epigallocatechin gallate enhances prostaglandin F2alpha-induced VEGF synthesis via upregulating SAPK/JNK activation in osteoblasts. Journal of Cellular Biochemistry. 2007;100(5):1146–1153. doi: 10.1002/jcb.21104. [DOI] [PubMed] [Google Scholar]
- Townsend PA, Scarabelli TM, Pasini E, Gitti G, Menegazzi M, Suzuki H, Knight RA, Latchman DS, Stephanou A. Epigallocatechin-3-gallate inhibits STAT-1 activation and protects cardiac myocytes from ischemia/reperfusion-induced apoptosis. FASEB Journal. 2004;18(13):1621–1623. doi: 10.1096/fj.04-1716fje. [DOI] [PubMed] [Google Scholar]
- Ullmann U, Haller J, Decourt JP, Girault N, Girault J, Richard-Caudron AS. A single ascending dose study of epigallocatechin gallate in healthy volunteers. Journal of International Medical Research. 2003;31:88–101. doi: 10.1177/147323000303100205. [DOI] [PubMed] [Google Scholar]
- vander-Kraan PM, vanden-Berg WB. Anabolic and destructive mediators in osteoarthritis. Current Opinion in Clinical Nutrition & Metabolic Care. 2000;3(3):205–211. doi: 10.1097/00075197-200005000-00007. [DOI] [PubMed] [Google Scholar]
- vanhet Hof KH, Wiseman SA, Yang CS, Tijburg LB. Plasma and lipoprotein levels of tea catechins following repeated tea consumption. Proceedings of the Society of Experimental Biology and Medicine. 1999;220(4):203–209. doi: 10.1046/j.1525-1373.1999.d01-34.x. [DOI] [PubMed] [Google Scholar]
- Vankemmelbeke MN, Jones GC, Fowles C, Ilic MZ, Handley CJ, Day AJ, Knight CG, Mort JS, Buttle DJ. Selective inhibition of ADAMTS-1, -4 and -5 by catechin gallate esters. European Journal of Biochemistry. 2003;270(11):2394–2403. doi: 10.1046/j.1432-1033.2003.03607.x. [DOI] [PubMed] [Google Scholar]
- Warstat K, Hoberg M, Rudert M, Tsui S, Pap T, Angres B, Essl M, Smith TJ, Cruikshank WW, Klein G, Gay S, Aicher WK. Transforming growth factor beta1 and laminin-111 cooperate in the induction of interleukin-16 expression in synovial fibroblasts from patients with rheumatoid arthritis. Annals of Rheumatic Diseases. 2010;69(1):270–275. doi: 10.1136/ard.2008.091116. [DOI] [PubMed] [Google Scholar]
- Westacott CI, Sharif M. Cytokines in osteoarthritis: mediators or markers of joint destruction? Seminars in Arthritis and Rheumatism. 1996;25(4):254–272. doi: 10.1016/s0049-0172(96)80036-9. [DOI] [PubMed] [Google Scholar]
- Weinreb O, Amit T, Youdim MB. A novel approach of proteomics and transcriptomics to study the mechanism of action of the antioxidant-iron chelator green tea polyphenol (-)-epigallocatechin-3-gallate. Free Radical Biology & Medicine. 2007;43(4):546–556. doi: 10.1016/j.freeradbiomed.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Wheeler DS, Catravas JD, Odoms K, Denenberg A, Malhotra V, Wong HR. Epigallocatechin-3-gallate, a green tea-derived polyphenol, inhibits IL-1 beta-dependent proinflammatory signal transduction in cultured respiratory epithelial cells. The Journal of Nutrition. 2004;134(5):1039–1044. doi: 10.1093/jn/134.5.1039. [DOI] [PubMed] [Google Scholar]
- Willson KC. Coffee, Cocoa and tea. New York: CABI Publishing; 1999. [Google Scholar]
- Wu D, Guo Z, Ren Z, Guo W, Meydani SN. Green tea EGCG suppresses T cell proliferation through impairment of IL-2/IL-2 receptor signaling. Free Radical Biology & Medicine. 2009;47(5):636–643. doi: 10.1016/j.freeradbiomed.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Wu H, Qi H, Iwasaki D, Zhu B, Shimoishi Y, Murata Y, Nakamura Y. JNK-dependent NFATc1 pathway positively regulates IL-13 gene expression induced by (-)-epigallocatechin-3-gallate in human basophilic KU812 cells. Free Radical Biology & Medicine. 2009;47(7):1028–1038. doi: 10.1016/j.freeradbiomed.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Xiao X, Yang ZQ, Shi LQ, Liu J, Chen W. Antiviral effect of epigallocatechin gallate (EGCG) on influenza A virus. Zhongguo Zhong Yao Za Zhi. 2008;3(22):2678–2682. [PubMed] [Google Scholar]
- Yang F, de Villiers WJ, McClain CJ, Varilek GW. Green tea polyphenols block endotoxin-induced tumor necrosis factor-production and lethality in a murine model. The Journal of Nutrition. 1998;128(12):2334–2340. doi: 10.1093/jn/128.12.2334. [DOI] [PubMed] [Google Scholar]
- Yang F, Oz HS, Barve S, de Villiers WJ, McClain CJ, Varilek GW. The green tea polyphenol (-)-epigallocatechin-3-gallate blocks nuclear factor-kappa B activation by inhibiting I kappa B kinase activity in the intestinal epithelial cell line IEC-6. Molecular Pharmacology. 2001;60(3):528–533. [PubMed] [Google Scholar]
- Yokota A, Narazaki M, Shima Y, Murata N, Tanaka T, Suemura M, Yoshizaki K, Fujiwara H, Tsuyuguchi I, Kishimoto T. Preferential and persistent activation of the STAT1 pathway in rheumatoid synovial fluid cells. The Journal of Rheumatology. 2001;28(9):1952–1959. [PubMed] [Google Scholar]
- Yun HJ, Yoo WH, Han MK, Lee YR, Kim JS, Lee SI. Epigallocatechin-3-gallate suppresses TNF-alpha -induced production of MMP-1 and -3 in rheumatoid arthritis synovial fibroblasts. Rheumatology International. 2008;29(1):23–29. doi: 10.1007/s00296-008-0597-5. [DOI] [PubMed] [Google Scholar]
- Zhang ZF, Li Q, Liang J, Dai XQ, Ding Y, Wang JB, Li Y. Epigallocatechin-3-O-gallate (EGCG) protects the insulin sensitivity in rat L6 muscle cells exposed to dexamethasone condition. Phytomedicine. 2010;17(1):14–18. doi: 10.1016/j.phymed.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Zheng W, Li R, Pan H, He D, Xu R, Guo TB, Guo Y, Zhang JZ. Role of osteopontin in induction of monocyte chemoattractant protein 1 and macrophage inflammatory protein 1beta through the NF-kappaB and MAPK pathways in rheumatoid arthritis. Arthritis & Rheumatism. 2009;60(7):1957–1965. doi: 10.1002/art.24625. [DOI] [PubMed] [Google Scholar]
- Zuo Y, Chen H, Deng Y. Simultaneous detection of the catechin, caffeine and gallic acid in green tea, oolong, black and pu-erh teas using HPLC with a photodiode array detector. Talanta. 2002;57:307–315. doi: 10.1016/s0039-9140(02)00030-9. [DOI] [PubMed] [Google Scholar]