SUMMARY
A one-step surgical procedure is presented, including maxillary sinus floor elevation in association with functional endoscopic sinus surgery to remove rhino-sinusal malformations or pathoses that might contraindicate sinus floor elevation. Over a 2-year period, 10 patients requiring a sinus floor augmentation procedure to restore the missing dentition with endosseous implants, but presenting with local and reversible rhinologic contraindications to the augmentation procedure were consecutively treated with a surgical approach that included simultaneously functional endoscopic sinus surgery and a sinus floor elevation procedure through an intra-oral approach. Then 4-6 months after this procedure, oral implants were inserted and after a further waiting period, ranging from 3 to 6 months, patients were restored with prostheses and followed for 1 to 3 years after the completion of prosthetic restoration. In all 10 patients, complete recovery of para-nasal sinuses function was demonstrated and occurred in all cases within one month. All cases showed good integration and consolidation of the graft material used for maxillary sinus floor augmentation. None of the implants placed were lost during the follow-up period after completion of prosthetic loading. In conclusion, despite the limits of this study (which included only 10 patients), the combination of maxillary sinus augmentation procedures and functional endoscopic sinus surgery, to treat local contraindications to sinus augmentation has proven to be both effective and safe and has allowed the patient to avoid a second surgical procedure and a longer waiting period before final prosthetic rehabilitation. No sinusal complications related to sinus floor augmentation were encountered and the survival rate of implants placed in the augmented areas was consistent with those reported in cases of sinus floor augmentation performed in patients presenting with a healthy rhino-sinusal system.
KEY WORDS: Maxillary sinus, Transnasal endoscopy, Sinus lift complication, One-step procedure
RIASSUNTO
Lo studio propone un nuovo approccio chirurgico, che riassume in un unico tempo associato due interventi abitualmente eseguiti in tempi successivi: il grande rialzo del seno mascellare (procedura odontoiatrica di tipo pre-impiantologico) e la chirurgia endoscopica rinosinusale volta a correggere malformazioni o patologie rinosinusali che controindicherebbero l'esecuzione isolata del rialzo stesso. In due anni sono stati arruolati 10 pazienti consecutivi con una indicazione odontoiatrica all'esecuzione di rialzo del seno, ma non candidabili all'intervento per presenza di controindicazioni rinosinusali locali e reversibili. In tutti i casi è stata eseguita una procedura combinata per via endoscopica nasosinusale ed endorale odontoiatrica. Dopo 4-6 mesi è stata eseguita in tutti i casi la procedura implantologica e dopo ulteriori 3-6 mesi è stata completata la riabilitazione protesica. Il follow-up successivo è stato di 1-3 anni. In tutti i casi entro un mese dall'intervento è stata recuperata una corretta funzione naso-sinusale. Allo stesso modo la procedura pre-implantologica ed implantologica è stata coronata da successo, con integrazione e consolidamento del materiale di rialzo. Nel periodo di follow-up nessun impianto ha subito una mobilizzazione. In conclusione, pur considerando i limiti quantitativi dell'esperienza e le sue caratteristiche di studio preliminare, è possibile affermare che la combinazione del rialzo del seno e di chirurgia endoscopica rinosinusale si è dimostrata efficace, sicura e ha consentito ai pazienti di evitare un secondo intervento chirurgico e un ulteriore tempo di attesa di 3-4 mesi prima della riabilitazione implantologica. In particolare non si è osservata alcuna complicanza naso-sinusale secondaria al rialzo del seno, in contrasto con quanto prevedibile per l'esecuzione di rialzo come unica procedura in presenza di controindicazioni rino-sinusali.
Introduction
Maxillary sinus floor elevation via a lateral approach (sinus lift) is a well documented method to increase bone volume of the edentulous posterior maxilla to allow implant placement in cases of bone deficiency due to atrophy or sinus expansion 1-3. The procedure was conceived and introduced by Tatum in 1976, was first published by Boyne and James in 1980 4 and consists of creating a mucoperiosteal pocket between Schneider's membrane and the maxillary floor and filling it with graft materials, which can be autografts, allografts, xenografts, or alloplastic materials. The main aim is to increase bone volume by promoting osteoconduction and/or osteoinduction in order to place, at the same time, or in a second stage, osteointegrated implants of adequate dimensions. As stated in the Babson College Consensus Conference, in 1996, this procedure is considered a safe and predictable method, provided that the maxillary sinus is healthy. In particular, it is considered mandatory to respect the natural homeostasis of the maxillary sinus and to perform surgery in the presence of an efficient ciliary movement, a normal sinusal mucosa and a pervious sinus ostium 5. In the absence of one or more of these natural defense mechanisms, the risk for developing complications after a sinus lift procedure becomes much more consistent 5 6. As a consequence, we must accept that contraindications to the Sinus Lift exist and that these are due to their potential of compromising the sinus homeostasis before, during or after the procedure.
These rhino-sinusal contraindications have already been well described in the literature and can be classified as reversible and irreversible 5. Potentially reversible contraindications can be represented by several clinical conditions such as anatomic-structural impairments of the maxillary sinus drainage pathways (such as a concha bullosa, relevant septal deviations), inflammatory infectious processes, large mucous cysts of the maxillary sinus, and benign naso-sinusal neoplasms of limited extension 7.
Irreversible contraindications are generally found in more uncommon situations, such as: a) relevant post-traumatic or post-surgical scars or sequelae of radiotherapy, that may severely interfere with the normal naso-sinusal homeostasis; b) granulomatous processes such as the Wegener Syndrome; c) benign naso-sinusal neoplasms and malignant naso-sinusal neoplasms that probably could severely affect naso-sinusal homeostasis even after treatment.
The reversible (chronic) rhino-sinusal contraindications are generally treated surgically and functional endoscopic sinus surgery (FESS) is currently considered the gold standard. In order to perform a sinus lift in patients with reversible contraindications, a two-step surgery (FESS followed by the sinus lift after a healing period of 4-6 months) has already been proposed and reported with encouraging results 5.
Aim of this study was to verify whether in selected clinical conditions it is possible to avoid two separate surgical procedures, converting them into a one step procedure, which comprises FESS as well as the sinus lift. For safety reasons, in this first experimental phase, the Authors decided to exclude all those cases presenting infection of the sinuses at the time of surgery.
Material and methods
Over a 2-year period, 10 consecutive healthy patients (6 male, 4 female), mean age 51.6 ± 4.95 years, presenting with edentulism of the posterior maxilla associated with insufficient bone volume to receive oral implants to allow implant-supported prosthetic restorations were referred to one of the participating centres: the Ear, Nose & Throat Department at the San Paolo Hospital, University of Milan, the Oral Surgery Unit of the San Paolo Hospital, University of Milan, or the Maxillo-Facial Department of the Istituto Stomatologico Italiano, Milan, Italy.
All 10 patients, presenting with reversible contraindications to the procedure, were investigated with nasal endoscopy and with maxillo-facial computed tomography (CT) scan. Four patients presented with large maxillary sinus cysts (one of these with a paradoxical bending of the middle turbinate and one with an associated concha bullosa), 3 with a mono-lateral concha bullosa (two of these also showed a significant septal deviation), 2 with bilateral concha bullosa and 1 septal deviation with small polyps in the middle meatus (but no signs of sinusitis). Clinically, most patients were symptom-free (4 patients), reported recurrent minor rhino-sinusitis (3 patients) or minor nasal obstruction (3 patients). In these patients, the reduction of the maxillary sinus dimensions and the potential inflammatory reaction, following the sinus floor elevation procedure, could expose the patient to a high risk of obstruction of the sinus and osteo-meatal complex (OMC) with reduction of sinus ventilation, stasis of sinusal secretions, and consequent development of maxillary sinusitis and/or infection of the graft material used for sinus elevation. The patients were treated under general anaesthesia in a single surgical session involving an ENT surgeon (who performed the FESS) and a maxillo-facial surgeon (who performed the sinus floor elevation procedure through an intra-oral approach). The first procedure was always the FESS. Depending upon the extension and type of anatomic-structural impairment of the maxillary sinus drainage pathways, the endoscopic transnasal approach may include partial middle turbinectomy, septoplasty, inferior uncinectomy, middle antrostomy, and removal of maxillary cysts.
Once the FESS procedure was concluded and no chronic or active infection were detected (as in all the patients included in this study), the oro-tracheal intubation was converted into a naso-tracheal type and the maxillo-facial surgeon proceeded with the sinus floor elevation procedure. In all patients, the elevation and the integrity of the Schneiderian's membrane was verified endoscopically from inside the sinus with a 4 mm, 45-degree rigid endoscope. In 6 out of 10 cases, the sinus floor elevation was programmed and performed bilaterally. In the 6 cases of bilateral sinus lift, the graft was harvested from the anterior iliac crest, while in the remaining 4 cases of mono-lateral sinus lift the graft was harvested from the mandibular ramus.
Antibiotic treatment with 1 g of Ceftriaxone was administered intra-operatively and followed by Cefuroxime 500 mg twice daily for the following 6 days.
Nasal packing with Merocel® (Medtronic, Mystic Connecticut, USA) was performed mono- or bilaterally in 5 patients and was removed 24 hours after the surgery. The patients were instructed to use saline solution for nasal rinse (twice daily for the following 10 days) and an antibiotic nasal cream (Bactroban®, Glaxo Smith Kline, Middlesex, UK) twice daily for 5 days.
Results
Hospitalization, after surgery, varied from 1 to 3 days (mean: 1.5 days). Post-operative recovery of the treated patients was uneventful in all cases. Follow-up ranged from 12 to 36 months. Complete recovery of paranasal sinus function, demonstrated clinically and endoscopically, was achieved in all the cases, within one month. All cases showed good integration and consolidation of the graft. After 4-6 months, end osseous implants were inserted in the areas of the grafted sinuses and after a further healing period needed for osteo integration, implants were prosthetically loaded. None of the implants placed were lost during the follow-up period (1 to 3 years after the start of prosthetic loading). A clinical case treated with this approach is presented in Figure 1-6.
Fig. 1.
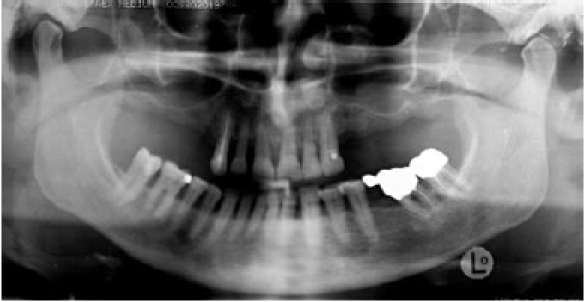
Initial clinical situation showing loss of teeth in right and left posterior maxilla with expansion of maxillary sinuses and atrophy of alveolar ridges not permitting placement of dental implants due to insufficient bone volume.
Fig. 6.
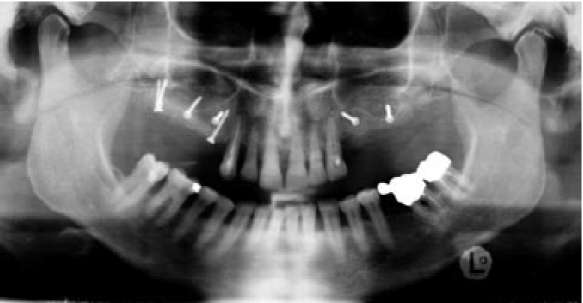
X-ray control after surgery showing bone volume increase.
Fig. 2.

CT scan shows bilateral mucous cysts in maxillary sinuses (in particular on right side) and a concha bullosa of the right middle turbinate, which represent contraindications to the sinus grafting procedure needed for implant placement, due to risk of ostium obstruction and secondary sinusitis.
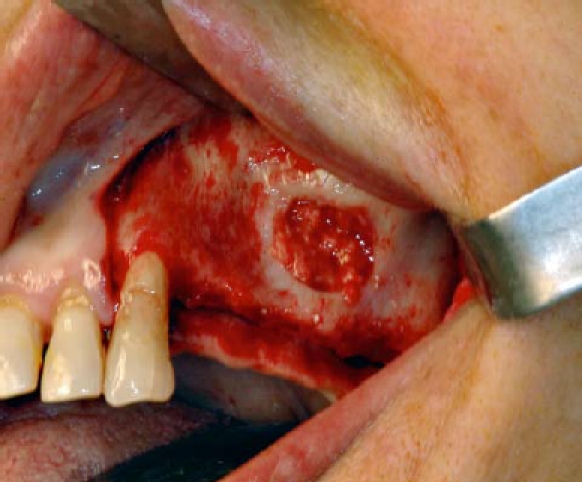
Fig. 3.

FESS allows enlargement of ostium and removal of cyst (left side).
Fig. 4.
In the same surgical session, it is now possible to proceed with a sinus grafting procedure with autogenous bone taken from the anterior ilium.
Fig. 5.

Sinus graft is associated with an onlay graft to increase also the width of the atrophic ridge.
Discussion
It is well known that the presence of pre-operative rhinosinusal disease is highly correlated with the development of acute sinusitis after sinus floor augmentation procedures 8. It is also well recognized that alterations in rhinosinusal ciliary function and/or the absence of patency of the maxillary sinus ostium increases the risk of complications following sinus elevation procedures 6 9.
Therefore, careful pre-operative planning, including not only evaluation of the volume of residual bone, in the posterior maxilla, in order to insert oral implants of adequate dimensions, but also a thorough analysis of the rhino-sinusal condition is fundamental in order to avoid potential complications following this type of surgery. It is, therefore, mandatory that the sinus lift candidate presenting with a bacterial or a mycotic form of sinusitis or with an impaired maxillary sinus ostium patency be treated by an ENT surgeon. The standard approach is two-step surgery in which the first procedure is represented by treatment of the nasal-sinusal impairment performed with FESS. Secondly, after a healing period of 4-6 months, the candidates to sinus grafting procedures will be re-evaluated either by endoscopy and/or computed tomography and if the rhinosinusal complex appears in healthy conditions, augmentation of the maxillary sinus floor can be performed. The main drawback of this approach is represented primarily by a lower acceptance on the part of the patients, due to the larger number of surgical procedures required.
The one-step procedure proposed in this study (for noninfectious sinus pathoses) not only avoids the patient having to undergo a second surgical procedure and is more cost-effective, but also enhances the patient's compliance in completing the prosthetic rehabilitation. In our hands the combination of FESS, to treat specific contraindications to sinus augmentation, and of the sinus lift in a onestep surgical preocedure, has proven effective and safe as all 10 cases presented normal recovery of the operated sinuses, adequate integration and consolidation of the graft material and no loss of implants during the followup period, after completion of prosthetic rehabilitation. Moreover, the FESS procedure itself is to be considered a minimally invasive surgical technique with little or no post-surgical oedema, discomfort or pain and is, therefore, well accepted by the patients.
Conclusion
The one-step approach is still not an alternative in the event of major local contraindications to sinus grafting procedures, but could be considered a safe and cost-effective option for treating minor reversible contraindications. Furthermore, this approach shows excellent patient satisfaction, as they can avoid a second operation and a longer time frame before concluding prosthetic rehabilitation.
Despite the limited number of patients, these results appear encouraging, however a larger number of patients need to be submitted to this surgical approach before proposing this procedure as routine.
References
- 1.Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants. 2009;24(Suppl):237–259. [PubMed] [Google Scholar]
- 2.Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006;17(Suppl 2):136–159. doi: 10.1111/j.1600-0501.2006.01357.x. [DOI] [PubMed] [Google Scholar]
- 3.Pjetursson BE, Tan WC, Zwahlen M, et al. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35(8 Suppl):216–240. doi: 10.1111/j.1600-051X.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 4.Boyne PJ, James RA. Surgical Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 5.Pignataro L, Mantovani M, Torretta S, et al. ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Acta Otorhinolaryngol Ital. 2008;28:110–119. [PMC free article] [PubMed] [Google Scholar]
- 6.Timmenga NM, Raghoebar GM, Boering G, et al. Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg. 1997;55:936–939. doi: 10.1016/s0278-2391(97)90063-x. discussion 940. [DOI] [PubMed] [Google Scholar]
- 7.Beaumont C, Zafiropoulos GG, Rohmann K, et al. Prevalence of maxillary sinus disease and abnormalities in patients scheduled for sinus lift procedures. J Periodontol. 2005;76:461–467. doi: 10.1902/jop.2005.76.3.461. [DOI] [PubMed] [Google Scholar]
- 8.Tidwell JK, Blijdorp PA, Stoelinga PJ, et al. Composite grafting of the maxillary sinus for placement of endosteal implants. A preliminary report of 48 patients. Int J Oral Maxillofac Surg. 1992;21:204–209. doi: 10.1016/s0901-5027(05)80219-x. [DOI] [PubMed] [Google Scholar]
- 9.Timmenga NM, Raghoebar GM, Liem RS, et al. Effects of maxillary sinus floor elevation surgery on maxillary sinus physiology. Eur J Oral Sci. 2003;111:189–197. doi: 10.1034/j.1600-0722.2003.00012.x. [DOI] [PubMed] [Google Scholar]


