Abstract
OBJECTIVE:
To examine the relationship between BMI status (normal, overweight, and obese) and preventive screening among adolescents at their last checkup.
METHODS:
We used population-based data from the 2003–2007 California Health Interview Surveys, telephone interviews of adolescents aged 12 to 17 years with a checkup in the past 12 months (n = 9220). Respondents were asked whether they received screening for nutrition, physical activity, and emotional distress. BMI was calculated from self-reported height and weight: (1) normal weight or underweight (<85th percentile); (2) overweight (85th–94th percentile); and (3) obese (>95th percentile). Multivariate logistic regression models tested how screening by topic differed according to BMI status, adjusting for age, gender, income, race/ethnicity, and survey year.
RESULTS:
Screening percentages in the pooled sample (all 3 years) were higher for obese, but not overweight, adolescents for physical activity (odds ratio: 1.4; P < .01) and nutrition (odds ratio: 1.6; screening did not differ P < .01). Stratified analysis by year revealed higher screening for obese (versus normal-weight) adolescents for nutrition and physical activity in 2003 and for all 3 topics in 2005. However, by 2007, screening did not differ according to BMI status. Overall screening between 2003 and 2007 declined for nutrition (75%–59%; P < .01), physical activity (74%–60%; P < .01), and emotional distress (31%–24%; P < .01).
CONCLUSIONS:
Obese adolescents receive more preventive screening versus their normal-weight peers. Overweight adolescents do not report more screening, but standards of care dictate increased attention for this group. These results are discouraging amid a rise in pediatric obesity and new guidelines that recommend screening by BMI status.
Keywords: preventive services, adolescent, obesity, screening, mental health
WHAT'S KNOWN ON THIS SUBJECT:
Guidelines ask providers to target adolescent diet and physical activity counseling by BMI status, but providers do not consistently provide this service and often rely on inspection alone versus calculating BMI percentile.
WHAT THIS STUDY ADDS:
This study investigated whether providers target adolescent preventive screening on the basis of BMI status, with a focus on overweight adolescents, given recent guidelines. The study is strengthened by the use of adolescent self-report versus relying on provider or parent report.
Recently released guidelines set the new standard of care for pediatric obesity screening and treatment. The 2008 Expert Committee recommendations and the 2010 US Preventive Services Task Force guidelines ask providers to target efforts differently for 3 BMI percentile groups: normal weight (0–84th percentile); overweight (85th–94th percentile); and obese (>95th percentile).1,2 The increased attention on the overweight group highlighted the new commitment to early intervention. They also recommend incorporating mental health and psychosocial assessment with obesity screening given the high rate of depression and anxiety among overweight youth.2 These recommendations were drawn from growing evidence for the importance of primary care screening and treatment of pediatric obesity. Patients who are identified as obese are more likely to receive physical activity and nutrition screening and proper laboratory testing and referrals.3–6 In addition, adolescents who are told that they are obese by their providers are more likely to report attempting weight loss in the past year and report better nutrition.7
Previous studies on primary care screening for pediatric obesity focus on whether providers measure BMI and provide recommended counseling.8–12 However, because the new standard of care is not just to calculate the BMI but to also calculate the percentile, data are needed regarding how ready providers are to meet this expectation. The most recent data from Klein et al6 reveal that although 99% of patients have height and weight measured at their visit, only 52% of providers calculate the BMI percentile. Few studies investigate whether providers target screening differently on the basis of BMI status or incorporate mental health screening as advised in recent guidelines.
Data are lacking on differences by year in primary care screening for nutrition and physical activity in the context of increased public awareness and the release of new guidelines. Ma et al13,14 used the National Ambulatory Medical Care Survey to investigate trends in diet and physical activity in adults and adolescents from 1992 to 2000. They found that there was a modest increasing trend in counseling for both adults and adolescents, but overall it was quite low. This study is limited by the use of National Ambulatory Medical Care Survey data set, which relies on provider coding of obesity diagnosis and provider report of counseling services and now is outdated.15
Our study investigates screening for nutrition, physical activity, and emotional distress from the adolescent perspective using data from the 2003–2007 biennial California Health Interview Survey (CHIS). We extend previous knowledge by investigating screening separately by all 3 categories of BMI status and also including mental health as a screening topic. Our primary aim was to investigate if overweight adolescents (85th–94th BMI percentile) in addition to obese adolescents (>95th percentile) have a higher proportion screened for nutrition, physical activity, and emotional distress. Our secondary aim was to describe screening percentages by year during a time of increased public awareness of pediatric obesity.
METHODS
Procedures
We used adolescent data from the 2003, 2005, and 2007 CHISs, a population-based household telephone survey of 3 cohorts of California residents. The CHIS is the largest representative state health survey in the United States and includes adult (aged ≥18 years), adolescent (aged 12–17 years), and child surveys (aged ≤12 years). Data were collected by Westat and housed at the University of California, Los Angeles, Center for Health Policy Research. Procedures were approved by the internal review boards at the University of California, Los Angeles, the state of California, Westat, and the federal Office of Management of the Budget. Random sampling of households was conducted by Westat from all California counties, and adolescent interviews were conducted with 1 randomly selected adolescent from households that had residents aged 12 to 17 years. Data are weighted using a household and population weight. Missing values were replaced using relational imputation by the CHIS staff for the public-use data file. Detailed descriptions of the CHIS procedures can be found in the CHIS 2005 Methodology Series (www.chis.ucla.edu).16
Participants
All CHIS adolescent respondents who reported a checkup within the past 2 years completed a series of questions asking whether they had talked to their provider about specific health-related topics at their most recent physical examination. To reduce recall bias and to be consistent with American Academy of Pediatrics guidelines for yearly health maintenance examination, we limited our analysis to adolescents who reported an examination in the last 12 months (n = 9220), which is 79% of the total CHIS adolescent sample (n = 11 677) for the 3 survey years.1* The rate of having a checkup in the past 12 months was higher in 2007 (81.3%) than in 2003 (75.6%) (P = .0002). This could be explained by the increasing enrollment in state health insurance. In fact, 93% of the sample in 2007 reported being currently insured versus 90% in 2003 (P = .01).
Measures
Age, race/ethnicity, and gender were self-reported by the adolescent. Race and ethnicity were coded into 5 categories: white, black, Hispanic/Latino, Asian, and other (includes mixed race/ethnicity and American Indian/Alaskan Natives). Income status was taken from parent-report and categorized as less than 300% or 300% or greater of the federal poverty level. Preventive health screening was measured by 3 items that asked adolescents if they talked to their physician at last checkup about physical activity, nutrition, and emotions or moods. Age-adjusted BMI was calculated using self-reported height and weight and categorized into 3 levels according to Centers for Disease Control and Prevention percentile: (1) normal-weight/underweight (<85th percentile); (2) overweight (85th–94th percentile); and (3) obese (>95th percentile).
Analysis
We first analyzed the pooled sample across years (n = 9220), using multivariate logistic regression analyses, to test how BMI status (predictor) impacts screening for nutrition, physical activity, and emotional distress (outcome). On the basis of our previous work on demographic factors that are associated with screening, we adjusted for age, race/ethnicity, income status, and gender in our models.17–19 We repeated this analysis stratified by year to investigate whether the relationship between BMI status and screening by topic differed within each year. We then used χ2 testing to determine whether differences in screening by year were statistically significant in an exploratory bivariate analysis. Estimates were weighted to represent California population totals in Stata (StataCorp, College Station, TX) using the SVY procedure to accommodate replicate weights and the complex sample design.20 For our pooled sample, we assume similar sampling and weighting procedures.
RESULTS
Sample Characteristics
Table 1 presents the sample characteristics for each year of the survey. There were no statistically significant differences across years for gender, age, or BMI status. However, there was a statistically significant increase in adolescents in the “other” race/ethnicity category from 4.9% to 17.2% and income level higher than 300% poverty status from 43.8% to 49%.
TABLE 1.
Sample Characteristics Among Adolescents Aged 12 to 17 Years Who Had a Checkup in the Past 12 Months, 2003–2007
| 2003 (N = 3041), % | 2005 (N = 3235), % | 2007 (N = 2944), % | |
|---|---|---|---|
| Characteristics | |||
| Gender | |||
| Male | 50.8 | 51.8 | 50.8 |
| Female | 49.2 | 48.2 | 49.2 |
| Age | |||
| 12–14 y | 54.2 | 52.3 | 49.1 |
| 15–17 y | 45.8 | 47.6 | 50.9 |
| Race/ethnicity | |||
| White | 42.2 | 41.9 | 36.7 |
| Latino | 33.4 | 27.3 | 29.1 |
| Asian | 9.9 | 10.3 | 9.7 |
| Black | 9.5 | 8.6 | 7.4 |
| Other | 4.9 | 11.8 | 17.2 |
| Income level | |||
| <300% of poverty level | 56.2 | 52.6 | 51.0 |
| ≥300% of poverty level | 43.8 | 47.3 | 49.0 |
| BMI status | |||
| Normal weight/underweight (0–84th percentile) | 70.9 | 69.9 | 72.4 |
| Overweight (85th–94th percentile) | 16.9 | 15.8 | 14.8 |
| Obese (>95th percentile) | 12.2 | 14.3 | 12.8 |
Screening by BMI Status (Pooled Sample)
Table 2 presents multivariate logistic regression models that predict the odds of screening for each topic in a pooled sample with data from all 3 years. In these models, our main predictor is BMI status, controlling for year and known demographic factors. Obese (compared with normal-weight) adolescents were more likely to report screening for physical activity (odds ratio [OR]: 1.4; P < .01) and nutrition (OR: 1.6; P < .01) but not emotional distress. Overweight adolescents were not more likely to receive screening in any area. Certain demographic groups, such as girls, younger adolescents, blacks, and Latinos, were more likely to be screened, although this was not consistent across screening topic.
TABLE 2.
Multivariate Logistic Regression Analysis Predicting Preventive Visit Screening Among Adolescents With a Checkup in the Last 12 Months, 2003–2007 Pooled Sample (N = 9220)
| Physical Activity |
Nutrition |
Emotional Distress |
||||
|---|---|---|---|---|---|---|
| % | Adjusted OR (95% Confidence Interval) | % | Adjusted OR (95% Confidence Interval) | % | Adjusted OR (95% Confidence Interval) | |
| Year | ||||||
| 2003 | 74.1 | — | 75.1 | — | 30.7 | — |
| 2005 | 75.8 | 1.1 (0.9–1.3) | 72.0 | 0.9 (0.7–1.0) | 21.9 | 0.6 (0.5–0.7)a |
| 2007 | 59.8 | 0.5 (0.4–0.6)a | 58.9 | 0.5 (0.4–0.6)a | 23.7 | 0.7 (0.6–0.8)a |
| Gender | ||||||
| Male | 68.7 | — | 66.3 | — | 20.7 | — |
| Female | 70.4 | 1.1 (1.0–1.3) | 70.3 | 1.2 (1.1–1.4)a | 30.0 | 1.7 (1.5–1.9)a |
| Age | ||||||
| 12–14 y | 70.1 | — | 72.8 | — | 25.7 | — |
| 15–17 y | 68.9 | 1.0 (0.8–1.1) | 63.3 | 0.7 (0.6–0.8)a | 24.8 | 1.0 (0.8–1.1) |
| Race/ethnicity | ||||||
| White | 69.0 | — | 64.0 | — | 24.4 | — |
| Latino | 73.4 | 1.3 (1.1–1.6)a | 74.4 | 1.5 (1.3–1.8)a | 28.1 | 1.1 (0.9–1.3) |
| Asian | 64.9 | 0.9 (0.7–1.0) | 62.9 | 1.0 (0.8–1.2) | 20.8 | 0.8 (0.6–1.1) |
| Black | 70.2 | 1.1 (0.8–1.3) | 76.2 | 1.7 (1.4–2.2)a | 25.9 | 1.0 (0.8–1.3) |
| Other | 64.7 | 1.0 (0.7–1.1) | 66.2 | 1.2 (1.0–1.5) | 24.2 | 1.1 (0.8–1.4) |
| Income level | ||||||
| <300% of poverty level | 70.0 | — | 65.0 | — | 23.3 | — |
| ≥300% of poverty level | 69.1 | 0.8 (0.7–0.9)a | 71.1 | 1.0 (0.9–1.2) | 27.0 | 1.1 (1.0–1.3) |
| BMI status | ||||||
| Normal weight/underweight (0–84th percentile) | 68.6 | — | 66.2 | — | 24.8 | — |
| Overweight (85th–94th percentile) | 68.8 | 1.0 (0.8–1.2) | 69.7 | 1.1 (0.9–1.3) | 25.6 | 1.1 (0.9–1.3) |
| Obese (>95th percentile) | 75.5 | 1.4 (1.1–1.7)a | 77.6 | 1.6 (1.3–2.0)a | 27.3 | 1.2 (1.0–1.5) |
Reference groups for statistically significant change are year 2003, male gender, age 12 to 14 years, white race, and normal weight/underweight.
P < .01.
Screening by BMI Status (Stratified According to Year)
Table 3 presents the results of screening by BMI status stratified by year. Obese versus normal-weight adolescents were more likely to be screened for nutrition and physical activity in 2003 and 2005 but not 2007. Obese versus normal-weight adolescents were more likely to be screened for emotional distress in 2005 only. Overweight adolescents were not more likely than normal-weight adolescents to be screened for any topic in any year.
TABLE 3.
Multivariate Logistic Regression Analysis Predicting Preventive Visit Screening Among Adolescents With a Checkup in the Last 12 Months by BMI Status (Normal, Overweight, and Obese) Stratified According to Year, 2003–2007 (N = 9220)
| BMI Status | Physical Activity |
Nutrition |
Emotional Distress |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 2003 (N = 3041) | 2005 (N = 3235) | 2007 (N = 2944) | 2003 (N = 3041) | 2005 (N = 3235) | 2007 (N = 2944) | 2003 (N = 3041) | 2005 (N = 3235) | 2007 (N = 2944) | |
| Normal weight/underweight (<85th percentile), % | 72.8 | 75.5 | 58.7 | 73.2 | 68.7 | 58.1 | 31.1 | 20.7 | 23.1 |
| Adjusted OR (95% confidence interval) | — | — | — | — | — | — | — | — | — |
| Overweight (85th–94th percentile), % | 74.4 | 70.7 | 61.3 | 75.9 | 73.8 | 59.5 | 30.0 | 20.4 | 26.5 |
| Adjusted OR (95% confidence interval) | 1.1(0.8–1.5) | 0.8 (0.6–1.1) | 1.1 (0.8–1.4) | 1 (0.8–1.4) | 1.3 (0.9–1.8) | 1 (0.8–1.4) | 1.0 (0.7–1.2) | 1 (0.7–1.4) | 1.2 (0.9–1.7) |
| Obese (>95th percentile), % | 80.6 | 82.2 | 64.0 | 84.5 | 86.2 | 62.9 | 29.1 | 29.4 | 23.6 |
| Adjusted OR (95% confidence interval) | 1.7 (1.1–2.5)a | 1.5 (1.1–2.1)a | 1.1 (0.8–1.5) | 1.8 (1.2–2.6)b | 2.7 (1.8–4.1)b | 1.1 (0.8–1.5) | 1.0 (0.7–1.4) | 1.7 (1.1–2.4)b | 1 (0.7–1.5) |
Multivariate logistic regression adjusting for age, gender, income status, and race/ethnicity. The reference group is normal weight/underweight.
P < .05.
P < .01.
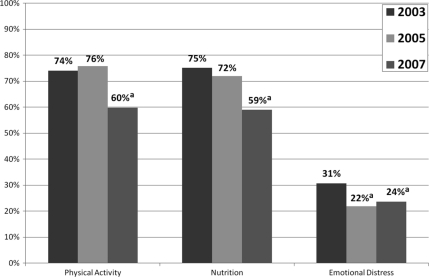
Preventive Screening by Year
Fig 1 shows a bivariate comparison of screening by topic and year. Provider screening was higher in 2003 than 2007 for physical activity (74% vs 60%; P < .01), nutrition (75% vs 59%; P < .01), and emotional distress (31% vs 24%; P < .01). However, overall screening for emotional distress was quite low, at less than one-half the rate of the other 2 topics. Differences in screening between 2003 and 2005 were only seen for emotional distress (31% vs 22%; P < .01) and were not significant for nutrition and physical activity. Paired t tests of nutrition and physical activity with emotional distress indicate that the proportion screened for nutrition and physical activity versus emotional distress was significantly different (P < .001).
FIGURE 1.
Preventive screening from 2003 to 2007 for physical activity, nutrition, and emotional distress among adolescents aged 12 to 17 years. Shown are differences in screening prevalence for 2005 and 2007 compared with 2003 using χ2 testing. a P < .01.
Table 2 shows that in a multivariate model controlling for known factors that contribute to screening, the OR for screening in 2007 for physical activity (OR: 0.5; P < .01), nutrition (OR: 0.5; P < .01), and emotional distress (OR: 0.7; P < .01) are significantly different from that in 2003. For emotional distress, there is the same result in the multivariate (versus bivariate) comparisons, that the odds of screening also is lower in 2005 than in 2003 (OR: 0.6; P < .01). This is not seen for physical activity and nutrition.
DISCUSSION
Increased Screening for Obese, but Not Overweight, Adolescents
Our results show that obese adolescents report higher screening than normal-weight respondents (2003–2005). This supports previous work that shows that obese adolescents are more likely to be screened.3–6 By 2007, the increased odds of nutrition and physical activity screening for obese adolescents was still present but less dramatic and no longer significantly different. These results are strengthened by the fact that we controlled for demographic factors known from previous work to be associated with higher screening rates, such as younger age, female gender, Latino ethnicity, and black race. The higher odds of screening seen in female subjects for emotional distress and Latinos/black subjects for nutrition and physical activity also is consistent with previous findings.17,18
The change by 2007 is important given that this was the year that the new recommendations were released.2 Furthermore, overweight adolescents do not experience significantly higher screening during any survey year despite the evidence that they are the group most amenable to early and brief interventions. In 2007, the BMI category name was changed from “at risk for overweight” to “overweight.” It will be useful to see how screening for this group compares in future years and if there is any impact of this change in terminology on provider screening.
There are several possible explanations for why overweight adolescents in particular do not experience higher screening levels. First, providers face barriers to screening, such as doubt that screening is effective, shorter visit times, and low reimbursement.3,4,6,21 Many pediatricians also lack local resources in pediatric weight management to which they can refer patients, further reducing their inclination to address this issue in their practice. Studies also show that providers may rely on visual inspection for identifying obese patients versus measuring the BMI directly. Subjective identification ranges from 20% to 50%, whereas rates of calculating BMI are much lower, ranging from 0.5% to 19%.8–12 Overweight patients would be less likely to be identified by inspection alone. And finally, pediatricians should be screening all adolescents regardless of BMI, so inspection should not be initiating screening.
Missed Opportunity for Screening for Emotional Distress
In our study, overall screening for emotional distress is low and not consistently linked with BMI status. It is well known that obese adolescents have a higher prevalence of depression and stigma.22 Previous studies report that adolescents entering treatment for obesity have significant depressive symptoms.23 Children with significant depression also are more likely to engage in unhealthy dieting practices and less likely to be able to adopt improved diet and exercise.24 Although the low overall rate of screening among all adolescents has been found in previous research,17 this study provides the first look into the lack of attention paid by pediatricians to this issue in overweight or obese teens. Previous studies have concluded that the lower rate of screening among teenagers likely relates to the lack of available referral resources and provider confidence and training in this area.
A Decline in Preventive Screening Overall
Our preliminary analysis of values over the 3 years reveals a decline in screening from 2003 to 2007 for physical activity, nutrition, and emotional distress. Although there are no comparable data on screening over time in adolescents, these results are consistent with the findings of McAlpine et al,21 using the National Ambulatory Medical Care Survey data in adults. Their data show that screening for diet and physical activity declined between 1995–1996 and 2003–2004 but that screening was higher in patients who had an obesity diagnosis.
There are several possible explanations for why provider screening declined between 2003 and 2007. One possibility is that the overall insurance status, payer mix, or the frequency with which adolescents received preventive health care visits changed over time. The addition of more immunization requirements between 2003 and 2007, with the introduction of the human papillomavirus vaccine, may have contributed to providers feeling overburdened and short on time. Also, during this time California was rapidly increasing its enrollment in Medicaid through the Children's Health Insurance Program, increasing the number of adolescents with insurance and access to primary care visits, thereby increasing patient load. All these factors may contribute to lower provider screening.
Limitations
Our study is limited by our reliance on self-reported weight and height. Several studies25–27 have shown that self-reported weight may be underestimated in girls and height overestimated in boys, but these differences are modest. We cannot comment on the specific content of the nutrition and physical activity screening because this was beyond the scope of the survey. Also, given that these are cross-sectional data, we only are able to look at overall screening prevalence. We cannot comment on the impact of this screening on individual adolescent behavior because this would require longitudinal data. Our data also come from a state-specific sample and may not be generalizable to the entire United States. However, the CHIS is the largest state population-based survey in the United States and includes a broad range of ethnic and racial diversity. We also are limited by being able to take into account only factors that have been measured in the CHIS; other factors that might influence screening, such as provider discipline, could not be considered. Although there were no known changes in CHIS methodology or measures to explain the changes in screening by year, these analyses will be strengthened by the availability of future years of data.
Finally, our study relies on self-report of screening at the last visit. Although this report could be influenced by respondent recall, adolescent self-report measures are considered a valid source of data about the prevision of preventive screening and have been incorporated into the development of quality measures.28 Our overall screening level is actually higher than those reported using physician- and parent-report data and is consistent with other studies using adolescent self-report.12,29
CONCLUSIONS
Given the recent release of the Expert Committee recommendations and the US Preventives Services Task Force report, these data have several important clinical and policy implications. Provider education on the importance of focusing attention on the overweight group is needed, as well as research around understanding the barriers for counseling this group. Strategies also are needed to train providers in mental health screening and referrals and to provide a link to these services and weight management. Finally, even with universal understanding of the recommendations by providers, adherence will remain hindered by reimbursement. Until we can provide pediatricians with the tools, reimbursement, and time to intervene in pediatric obesity, primary care remains a missed opportunity in the prevention of obesity.
ACKNOWLEDGMENTS
This work was supported by the Maternal and Child Health Bureau (grants T71MC00003, U45MC00023, and U45MC0002); the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (grant T32 HD04433106); Staglin Family Fund; the Young Adult and Family Center, University of California San Francisco Department of Psychiatry; the National Institute of Nursing Research (grant NR009397); the National Center for Research Resources, National Institutes of Health; and the University of California San Francisco Clinical and Technical Science Institute (grant UL1 RR024131).
We thank E. Richard Brown, CHIS Principal Investigator, and David Grant, CHIS Director, for ensuring that the CHIS public-use data files are available to all researchers.
FINANCIAL DISCLOSURE: The authors have indicated they have no personal financial relationships relevant to this article to disclose.
Funded by the National Institutes of Helth (NIH).
Of 11 677 subjects who responded to the survey, 9220 (79%) had a checkup in the past 12 months. The samples only differed according to age (younger respondents were more likely to have had a checkup; P = .01) and income (those with higher income were more likely to have a checkup; P =.004). We controlled for both these factors in our analyses.
Abbreviations:
- CHIS
- California Health Interview Survey
- OR
- odds ratio
REFERENCES
- 1. Barton M; US Preventive Services Task Force Screening for obesity in children and adolescents: US preventive services task force recommendation statement. Pediatrics. 2010;125(2):361–367 [DOI] [PubMed] [Google Scholar]
- 2. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192 [DOI] [PubMed] [Google Scholar]
- 3. Ma J, Xiao L. Assessment of body mass index and association with adolescent preventive care in U.S. outpatient settings. J Adolesc Health. 2009;44(5):502–504 [DOI] [PubMed] [Google Scholar]
- 4. Voelker R. Improved use of BMI needed to screen children for overweight. JAMA. 2007;297(24):2684–2685 [DOI] [PubMed] [Google Scholar]
- 5. Sesselberg TS, Klein JD, O'Connor KG, Johnson MS. Screening and counseling for childhood obesity: results from a national survey. J Am Board Fam Med. 2010;23(3):334–342 [DOI] [PubMed] [Google Scholar]
- 6. Klein JD, Sesselberg TS, Johnson MS, et al. Adoption of body mass index guidelines for screening and counseling in pediatric practice. Pediatrics. 2010;125(2):265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kant AK, Miner P. Physician advice about being overweight: association with self-reported weight loss, dietary, and physical activity behaviors of US adolescents in the National Health and Nutrition Examination Survey, 1999–2002. Pediatrics. 2007;119(1). Available at: www.pediatrics.org/cgi/content/full/119/1/e142 [DOI] [PubMed] [Google Scholar]
- 8. Halpern-Felsher BL, Ozer EM, Millstein SG, et al. Preventive services in a health maintenance organization: how well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000;154(2):173–179 [DOI] [PubMed] [Google Scholar]
- 9. O'Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114(2). Available at: www.pediatrics.org/cgi/content/full/114/2/e154 [DOI] [PubMed] [Google Scholar]
- 10. Dorsey KB, Wells C, Krumholz HM, Concato JC. Diagnosis, evaluation, and treatment of childhood obesity in pediatric practice. Arch Pediatr Adolesc Med. 2005;159(7):632–638 [DOI] [PubMed] [Google Scholar]
- 11. Dilley KJ, Martin LA, Sullivan C, Seshadri R, Binns HJ. Identification of overweight status is associated with higher rates of screening for comorbidities of overweight in pediatric primary care practice. Pediatrics. 2007;119(1). Available at: www.pediatrics.org/cgi/content/full/119/1/e148 [DOI] [PubMed] [Google Scholar]
- 12. Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110(1 pt 2):222–228 [PubMed] [Google Scholar]
- 13. Ma J, Urizar GG, Jr, Alehegn T, Stafford RS. Diet and physical activity counseling during ambulatory care visits in the United States. Prev Med. 2004;39(4):815–822 [DOI] [PubMed] [Google Scholar]
- 14. Ma J, Wang Y, Stafford RS. U. S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36(5):441. [DOI] [PubMed] [Google Scholar]
- 15. Eneli IU, Keast DR, Rappley MD, Camargo CA., Jr Adequacy of two ambulatory care surveillance systems for tracking childhood obesity practice patterns. Public Health. 2008;122(7):700–707 [DOI] [PubMed] [Google Scholar]
- 16. Cervantes IF, Brick JM. CHIS 2005 Methodology Series: Report 1: Sample Design. Los Angeles, CA: University of California Los Angeles Center for Health Policy Research; 2007 [Google Scholar]
- 17. Ozer EM, Zahnd EG, Adams SH, et al. Are adolescents being screened for emotional distress in primary care? J Adolesc Health. 2009;44(6):520–527 [DOI] [PubMed] [Google Scholar]
- 18. Adams SH, Husting S, Zahnd E, Ozer EM. Adolescent preventive services: rates and disparities in preventive health topics covered during routine medical care in a California sample. J Adolesc Health. 2009;44(6):536–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ozer E. Are adolescents being screened for depression in primary care? Society for Adolescent Medicine Annual Meeting Denver, CO, March 28–31, 2007 [Google Scholar]
- 20. Stata Base Reference Manual. College Station, TX: Stata Press; 2005 [Google Scholar]
- 21. McAlpine DD, Wilson AR. Trends in obesity-related counseling in primary care: 1995–2004. Med Care. 2007;45(4):322–329 [DOI] [PubMed] [Google Scholar]
- 22. Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord. 2002;26(1):123–131 [DOI] [PubMed] [Google Scholar]
- 23. Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity. 2006;14(1):122–130 [DOI] [PubMed] [Google Scholar]
- 24. Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med. 2004;38(6):865–875 [DOI] [PubMed] [Google Scholar]
- 25. Klein JD, Postle CK, Kreipe RE, et al. Do physicians discuss needed diet and nutrition health topics with adolescents? J Adolesc Health. 2006;38(5):608e601–606e601 [DOI] [PubMed] [Google Scholar]
- 26. Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health. 2003;32(4):281–287 [DOI] [PubMed] [Google Scholar]
- 27. Lee K, Valeria B, Kochman C, Lenders CM. Self-assessment of height, weight, and sexual maturation: validity in overweight children and adolescents. J Adolesc Health. 2006;39(3):346–352 [DOI] [PubMed] [Google Scholar]
- 28. Bethell C, Klein J, Peck C. Assessing health system provision of adolescent preventive services: the Young Adult Health Care Survey. Med Care. 2001;39(5):478–490 [DOI] [PubMed] [Google Scholar]
- 29. Irwin CE, Jr, Adams SH, Park MJ, Newacheck PW. Preventive care for adolescents: few get visits and fewer get services. Pediatrics. 2009;123(4). Available at: www.pediatrics.org/cgi/content/full/123/4/e565 [DOI] [PubMed] [Google Scholar]