Abstract
Uncertainty is a pervasive and important problem that has attracted increasing attention in health care, given the growing emphasis on evidence-based medicine, shared decision making, and patient-centered care. However, our understanding of this problem is limited, due in part to the absence of a unified, coherent concept of uncertainty. There are multiple meanings and varieties of uncertainty in health care, which are not often distinguished or acknowledged although each may have unique effects or warrant different courses of action. The literature on uncertainty in health care is thus fragmented, and existing insights have been incompletely translated to clinical practice. In this paper we attempt to address this problem by synthesizing diverse theoretical and empirical literature from the fields of communication, decision science, engineering, health services research, and psychology, and developing a new integrative conceptual taxonomy of uncertainty. We propose a three-dimensional taxonomy that characterizes uncertainty in health care according to its fundamental sources, issues, and locus. We show how this new taxonomy facilitates an organized approach to the problem of uncertainty in health care by clarifying its nature and prognosis, and suggesting appropriate strategies for its analysis and management.
Uncertainty creeps into medical practice through every pore. Whether a physician is defining a disease, making a diagnosis, selecting a procedure, observing outcomes, assessing probabilities, assigning preferences, or putting it all together, he is walking on very slippery terrain. It is difficult for nonphysicians, and for many physicians, to appreciate how complex these tasks are, how poorly we understand them, and how easy it is for honest people to come to different conclusions.
—David Eddy1
Introduction
Uncertainty pervades and motivates every activity related to health care. At the most fundamental level, it is uncertainty of one form or another that fuels medical research, prompts patients to seek care, and stimulates medical intervention.2, 3 The inability to abolish uncertainty, furthermore, promotes the perpetuation of these activities and creates difficult challenges for clinicians and patients.
The central and problematic nature of uncertainty in health care has been acknowledged by scholars since the 1950s, when the sociologist Renée Fox conducted seminal studies documenting how physicians struggle with uncertainty during their training.3, 4 More recently, uncertainty in health care has attracted growing attention due to several trends and events. The continued rise of the evidence-based medicine movement has highlighted professional awareness of the limitations of scientific knowledge. Meanwhile, public awareness and confusion has been heightened by broadening mass media coverage of medical controversies ranging from drug safety to breast cancer screening, and scientific uncertainty has come to occupy a central place in the nation’s health policy agenda. Current interest in comparative effectiveness research is ultimately driven by an explicit motivation to reduce scientific uncertainty in health care.5, 6 The informed and shared decision making movement, along with growing efforts to make health care more “patient-centered,”7 have highlighted the need to educate and help patients cope with uncertainty. A seminal publication on patient-centered communication from the National Cancer Institute identifies the management of uncertainty as a core function of the endeavor.8
Despite the growing visibility and importance of uncertainty in health care, we have a limited understanding of how to address the many problems it poses for laypersons, patients, clinicians, and health policymakers. Although groundbreaking work has been conducted by researchers from various disciplines including sociology,3, 4, 9–11 bioethics,12 health services research,13–17 communication,2 and nursing,18, 19 the body of knowledge on the uncertainties faced by clinicians and patients is fragmented and incomplete, and important insights have not been translated to clinical practice. Consequently, we know little about the optimal means and outcomes of communicating uncertainty to patients and the public,20 and even less about how to help clinicians, and patients cope with uncertainty.8
These knowledge gaps reflect limitations in empirical evidence; however, a more fundamental problem is the absence of a shared concept of uncertainty, and a lack of integration of insights from different disciplines.21 Uncertainty has many conceptual meanings that are not often distinguished or explicitly considered.2, 22, 23 Furthermore, uncertainty is not a monolithic phenomenon. There are multiple varieties of uncertainty, which may have distinct psychological effects and thus warrant different courses of action.20, 21, 24, 25 An organizing conceptual framework that categorizes these multiple varieties of uncertainty in a coherent, useful way may thus be of value to clinicians, researchers, and health policymakers. Such a framework could help researchers measure and to understand the manifestations, mechanisms, and effects of uncertainty in health care, and to develop effective, targeted interventions for managing uncertainty among clinicians and patients. A conceptual framework could also enable clinicians to establish a precise diagnosis and prognosis of the specific uncertainties in different clinical circumstances, and to implement strategies to assist patients in coping with these uncertainties.
The purpose of this paper is to summarize major theoretical insights relevant to understanding uncertainty specific to health care, and to develop an integrative conceptual taxonomy that can serve as a useful framework, based on a review of literature from the fields of decision science, psychology, communication, engineering, and health services research. To accomplish this review, we searched electronic databases (Medline, PsycINFO, Web of Science) using broad search terms (uncertainty, ambiguity) and scanning abstracts to identify the small number of papers that not only dealt with the topic of uncertainty, but attempted to develop theoretical classifications or taxonomies of this phenomenon. We also scanned reference lists of all identified papers to capture additional papers and sources (e.g., books, monographs). In this paper we synthesize the diverse theoretical perspectives found in our review, and propose a new three-dimensional taxonomy that characterizes uncertainty in health care in terms of its fundamental sources, issues, and loci. We attempt to show how the new taxonomy clarifies the nature and prognosis of uncertainty in health care, and suggests promising approaches to this important problem in research and clinical care.
The many meanings of uncertainty
The first challenge in developing an integrative conceptual framework is to settle on a working definition of the term “uncertainty.” Although much has been written about uncertainty by researchers from various disciplines, rarely has the term itself been explicitly defined. The Merriam-Webster dictionary defines uncertainty as “the state of being uncertain,” and uses a plethora of terms to define “uncertain”: indefinite, indeterminate, not certain to occur, problematical, not reliable, untrustworthy, not known beyond doubt, dubious, doubtful, not clearly identified or defined, not constant, variable, and fitful.26 These expansive descriptors clearly encompass numerous types, sources, and manifestations of uncertainty, and illustrate the challenge involved in understanding uncertainty in health care. A useful working definition of uncertainty needs to specify the concept underlying these varied meanings of the term.
Implicit in the dictionary definition of uncertainty as a “state” is a conceptualization of uncertainty as a subjective, cognitive experience of people—a state of mind rather than a feature of the objective world. The defining feature of this state, furthermore, appears to be lack of knowledge about some aspect of reality. Importantly, however, the concept of uncertainty also implies a subjective consciousness or awareness of one’s lack of knowledge, without which one could not feel uncertain; uncertainty is a form of “metacognition”—a knowing about knowing.27 Thus the decision scientist Smithson usefully distinguishes uncertainty from what he terms “meta-ignorance”—the state of “not knowing that one does not know.”21 At the most fundamental level, then, we may define uncertainty as the subjective perception of ignorance. It is this fundamental perception that makes possible the many manifestations of uncertainty catalogued in conventional definitions of the term—e.g., feelings of doubt, perceptions of indefiniteness, indeterminacy, unreliability, etc.. It is this subjective perception of ignorance that is experienced by patients and health professionals in differing ways and degrees, motivates action, and elicits a variety of psychological responses.
Taxonomies of uncertainty in health care: past approaches
Even if we accept the subjective perception of ignorance as a working definition of uncertainty, however, we are left with the challenge of classifying its many types, sources, and manifestations in a coherent and useful way. In the existing literature on uncertainty in health care there have been a few notable efforts to do so, which lay the groundwork for a taxonomy while manifesting limitations that call for new approaches.
In the nursing literature, Mishel has written extensively about patients’ experiences of “uncertainty in illness” and has developed measures of perceived uncertainty regarding acute and chronic illness.18, 19 She has defined uncertainty as “the inability to determine the meaning of illness-related events,”28 and has identified 4 distinct dimensions of patients’ experiences of uncertainty in illness: 1) ambiguity—patients’ self evaluation of the state of illness as vague or unclear; 2) complexity—the multiplicity of varied cues patients perceive about treatment and the system of care; 3) deficient information—inadequate information concerning patients’ diagnosis; and 4) unpredictability—absence of stability in the course of patients’ course of illness and outcomes.19 This taxonomy is useful in identifying factors that contribute to uncertainty in health care settings. Its weakness, however, is a lack of precision in the definitions of its factors. In the case of “ambiguity,” for example, exactly what it means for patient self-evaluations to be “vague or unclear” is itself unclear, and measures of these various factors have been found to overlap.18 Furthermore, Mishel’s taxonomy is not exhaustive; it focuses exclusively on uncertainty experienced by patients, and does not encompass other important types of uncertainty in health care, such as scientific uncertainty.
In the communication literature, Babrow has developed a more expansive conceptual taxonomy that includes 5 principal meanings or forms of uncertainty in health care: 1) complexity—arising from the multicausality, contingency, reciprocity, or unpredictability of a phenomenon; 2) qualities of information—its clarity, accuracy, completeness, volume, ambiguity, consistency, applicability, or trustworthiness; 3) probability—referring to one’s belief in a specific probability or a range of probabilities; 4) structure of information—i.e., its order or integration; and 5) lay epistemology—people’s own beliefs about a phenomenon.2 The strength of this taxonomy is its greater detail and comprehensiveness compared to Mishel’s; however, it also has limitations. First, its conceptual categories are not clearly distinct, and some may be logically combined or subsumed within others; for example, “structure of information” can be subsumed within “qualities” of information. At the same time, the taxonomy fails to identify other more fundamental conceptual distinctions that do seem important. For example, the taxonomy does not distinguish between uncertainty arising from the objective nature of “whatever is at issue” (e.g., its complexity or probabilistic nature), vs. the available information about the issue (e.g., the quality of information), vs. people’s subjective interpretation of the information (e.g., lay epistemology).
In a different vein, Kasper and colleagues developed a conceptual taxonomy including 8 categories of uncertainties experienced by cancer patients: 1) social integration; 2) diagnosis and prognosis; 3) deciphering information (regarding the behavior of medical staff or other kinds of information); 4) mastering of requirements (the ability to cope with disease-related life changes); 5) causal attribution; 6) preferred degree of involvement in the physician patient interaction; 7) physicians’ trustability; and 8) treatment (efficacy of a treatment as well as of other supporting activities).29 This taxonomy diverges from those of Babrow and Mishel in focusing on specific clinical problems and tasks that represent objects rather than sources of uncertainty. It therefore adds valuable clinical specificity and comprehensiveness, but at the expense of neglecting underlying causes of uncertainty that cross-cut multiple clinical problems. For example, uncertainties regarding both diagnosis/prognosis and deciphering information may ultimately result from “complexity” or other informational characteristics.
Taxonomies of uncertainty: insights from other fields
The utility of existing taxonomies of uncertainty in health care is limited by their focus on isolated types of uncertainty, or their failure to coherently distinguish between these types or to capture the full range of their sources and manifestations. These limitations are significant in that empirical evidence suggests that different types, sources, and manifestations of uncertainty may elicit divergent responses from people, and may thus warrant different actions on the part of health professionals.2, 21, 24 To be useful, to researchers and clinicians, a conceptual taxonomy of uncertainty needs to differentiate between the many types, sources, and manifestations of uncertainty that lead to distinct effects.
Research in fields outside of health care provides key insights that are pertinent to this task. In the decision science literature, Lipshitz and Strauss have usefully distinguished two main dimensions by which uncertainty can be conceptualized.22 The first is by source—e.g., incomplete information, inadequate understanding, or undifferentiated alternatives of equal attractiveness. The second is by issue—i.e., the particular outcomes, situation, or alternatives to which a given uncertainty applies. According to this two-dimensional organizing schema, the taxonomies of Mishel and Babrow deal mostly with source, while the taxonomy of Kasper and colleagues deals mostly with issue. Each taxonomy is thus useful in its own right; however, they fail to both distinguish between the two dimensions and to exhaust the full range of both sources and issues of uncertainty in health care.
Sources of uncertainty
For example, Smithson has identified additional important sources of uncertainty in his comprehensive “taxonomy of ignorance,” which defines “ignorance” as an erroneous cognitive state arising from either distorted or incomplete views.21, 24 In Smithson’s taxonomy, uncertainty is a specific subtype of ignorance arising from incompleteness of one’s knowledge of a phenomenon or event. This occurs when available information is limited to or characterized by probability (the likelihood of a future event), ambiguity (a multiplicity of possible states for a single concept or event), or vagueness (a multiplicity of possible values on a continuum). These sources of uncertainty themselves have underlying sources and subtypes; for example, “vagueness” can arise from either “fuzziness” (a lack of fine-graded distinctions or boundaries) or “nonspecificity” (imprecision) of information, while “ambiguity” may arise from information that is conflicting or subject to multiple interpretations. This hierarchical taxonomy has been expanded in the engineering literature by Ayyub,30 who has enumerated even more narrowly-defined subtypes or sources of uncertainty.
These taxonomies are valuable not only in their comprehensiveness, but in their coherent reduction of uncertainty to conceptually discrete elements. Smithson’s concepts of ambiguity and vagueness, for example, are more precisely defined and logically fundamental than the concept of “complexity” in the frameworks of Mishel and Babrow. These concepts also map on to sources of uncertainty that appear to have unique psychological effects, further justifying conceptual distinctions between them. For example, a large body of empirical research has shown that people respond differently to probabilities that are known—in which the uncertainty pertains to the indeterminacy of future outcomes and is expressed in terms of numeric probability estimates—as opposed to unknown, in which case discrete probability estimates are impossible or difficult to assign. The latter type of uncertainty, which decision theorists since Ellsberg (1961) have termed “ambiguity,” represents a critically important second-order, epistemic uncertainty regarding the “reliability, credibility, or adequacy” of existing risk information.31 Ambiguity has been shown to promote pessimistic appraisals of risk and avoidance of decision making—a phenomenon known as “ambiguity aversion.”31–33 The magnitude of this effect appears to depend on the source of ambiguity—i.e., conflicting vs. incomplete information33—further corroborating the influence of the source of uncertainty on people’s responses to it. A critical task for future research is to determine whether other conceptually distinct sources of uncertainty also have distinct psychological effects.
Issues of uncertainty
With respect to the second main dimension of uncertainty—its substantive issues—theoretical work outside of health care has focused largely on scientific uncertainty. This is a reflection of the disciplinary perspectives that have informed this work: engineering, risk analysis, behavioral decision theory, law. Scientific uncertainty is not the only important issue in health care; however, it is a matter of preeminent concern given the growing emphasis on evidence-based medicine and on informed and shared decision making. Because existing typologies of uncertainty in health care have not focused on the issue of scientific uncertainty, however, it is necessary to look to other disciplines for relevant insights.
In risk analysis and engineering, efforts to conceptualize scientific uncertainty have largely focused on statistical models used to assess and quantify risks. One conceptual distinction, made by risk analysis experts23 and federal regulatory organizations such as the U.S. Environmental Protection Agency (EPA),34 is between “parameter uncertainty”—lack of knowledge about the values of a model's parameters—and “model uncertainty”—lack of knowledge needed to determine the correct scientific theory on which to base a model. Another important distinction is between “stochastic” and “epistemic” uncertainty.35, 36 Stochastic uncertainty pertains to the parameters of a risk model, originates from sampling or measurement error, and can be quantified and mathematically expressed (e.g., using confidence intervals). Epistemic uncertainty, in contrast, reflects limitations in the current “state of knowledge” underlying models themselves, originates from competing theories or models, is not readily quantifiable, and is manifest by subjective confusion or indecision.35
Morgan has enumerated additional sources of scientific uncertainty pertaining to “empirical quantities” in risk analysis.37 These include: 1) statistical variation arising from random measurement error; 2) subjective judgment due to systematic measurement error; 3) linguistic imprecision in the representation of quantities; 4) variability occurring naturally in a measured quantity over time or space; 5) inherent randomness and unpredictability arising from the indeterminacy (either real or apparent) of a phenomenon; 6) disagreement in interpretations of scientific evidence; and 7) approximation due to limitations in the capacity of a model to represent real-world systems.37 The legal scholar Walker has developed a similarly expansive taxonomy of scientific uncertainty that distinguishes a broad variety of issues and causes specific to the scientific reasoning process.38, 39 He identifies 6 main types of scientific uncertainty: 1) conceptual—related to the definition and choice of descriptive concepts or variables; 2) measurement—involving the application of concepts or variables to specific, individual cases; 3) sampling—involving the generalization from specific, observed cases to unobserved cases; 4) modeling—involving the prediction of one predicate or variable as a mathematical function of other predicates or variables; 5) causal—involving the inference from certain mathematical functions between variables to conclusions about causal relationships; and 6) epistemic—involving the choice of interpretations for fundamental, logical concepts used throughout all levels.
For our purposes, the important aspect of these taxonomies is that they deal specifically with scientific uncertainty, isolating issues particular to the concerns, methods, and activities of researchers—e.g., measurement, sampling, and modeling. Yet some issues can be construed as sources rather than issues of uncertainty that apply equally outside of the domain of science. For example, causal reasoning is an important activity of everyday life, and causal uncertainty applies to and motivates judgment and decision making in many life domains.40, 41 Likewise, epistemic uncertainty pervades not only scientific but all forms of reasoning. Indeed, a broader and more basic distinction has been made between epistemic (or “epistemological”) and aleatory uncertainty—the latter pertaining to the fundamental, irreducible randomness or indeterminacy of natural events. This distinction has been the subject of longstanding debate in the philosophy of statistics and of medicine.42, 43 However, the apparent indeterminacy of any given phenomenon arguably reflects mere human ignorance of its true causes;37 thus all uncertainty, scientific or not, may ultimately be construed as epistemic—related to the incompleteness of one’s knowledge.21, 24
An integrative taxonomy of uncertainty in health care: a three-dimensional view
The foregoing analysis illustrates the diversity and richness of different understandings of uncertainty, and the challenges of developing a useful taxonomy specific to the health care domain. We lack a single overarching theoretical perspective on uncertainty in general; most existing taxonomies focus narrowly on particular sources or issues. Other taxonomies focus more broadly on multiple aspects, but fail to clearly distinguish between them. Furthermore, no taxonomy encompasses all of the salient issues in which uncertainty is manifest in health care. Conspicuously absent are issues that are more practical—i.e., related to the navigation of the health care delivery system—or existential—related to patients’ sense of meaning in life. Practical and existential uncertainties, however, may be more important to patients than uncertainties surrounding scientific information.44–46 What is needed is a coherent integrative taxonomy that is 1) sufficiently broad to capture the full range of uncertainties experienced by clinicians and patients in health care settings; and 2) sufficiently narrow to specify distinctions that are meaningful and actionable for clinicians, patients, researchers, and health policymakers. Such a taxonomy might facilitate a more rational approach to addressing the many problems that uncertainty poses in clinical care.
Building on the organizational approach of Lipshitz and Strauss, we first organize the many varieties of uncertainty in health care according to 2 discrete dimensions: source (type) and issue (domain), and begin by thinking of these dimensions separately. The initial task is to conceive the elemental sources of uncertainty; once this is done, one can then capture and logically classify the full range of salient issues in which these uncertainties are manifest in health care.
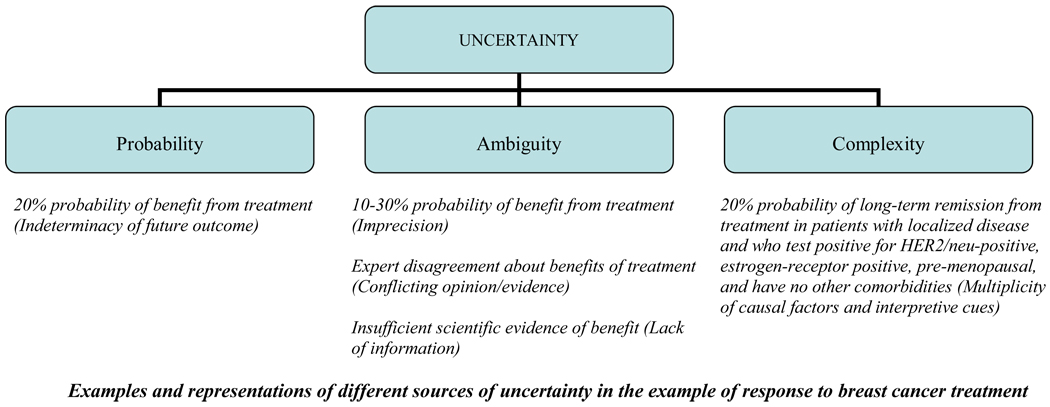
Figure 1 presents a taxonomy of the first dimension of uncertainty—its source—that is not specific to health care. This taxonomy follows Smithson’s model in postulating 3 main sources or types of uncertainty beginning with probability or risk. However, the new taxonomy differs from Smithson’s in two ways. First, it uses the term “ambiguity,” instead of Smithson’s term “vagueness,” to signify the lack of reliability, credibility, or adequacy of risk estimates. The rationale is to maintain consistency with terminology from the substantial body of behavioral decision research on ambiguity aversion.31 The term “ambiguity” provides an important theoretical link to this research, although Smithson’s terminology is linguistically accurate and favored by some decision theorists.47, 48
Figure 1.
Sources of uncertainty in health care.
The second difference is the substitution of a new category, “complexity,” in lieu of Smithson’s “ambiguity.” This more inclusive category captures a source or type of uncertainty arising not from a phenomenon’s indeterminacy (probability) or the lack of reliability, credibility, or adequacy of information about the phenomenon (ambiguity), but from aspects of the phenomenon itself that make it difficult to comprehend. Examples include multiplicity regarding possible states of an event or concept (as in Smithson’s definition of ambiguity)—such as the existence of numerous potential outcomes from a medical treatment. Multiplicity may also characterize the causes, effects, or interpretive cues related to an event (as identified in the taxonomies of both Babrow and Mishel); an example is the existence of varied risk factors, symptoms or signs of a given disease. Complexity as such is both an objective and a subjective matter; it is part of the phenomenon itself, but its extent also depends on personal judgment. Importantly, probability, ambiguity, and complexity are not always quantified or quantifiable, Figure 1 illustrates how these 3 types pertain to the exemplary issue of uncertainty about response to breast cancer treatment.
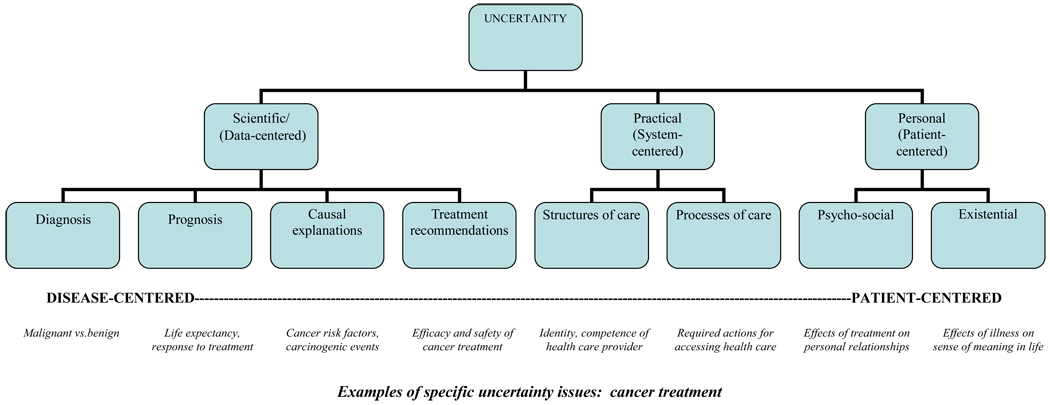
Figure 2 presents a new taxonomy of the second dimension of uncertainty in health care: its substantive issues. These can be subdivided into 3 main categories—scientific, practical, and personal—according to their substantive content and the concerns to which they pertain. Broadly speaking, scientific uncertainty is disease-centered, while practical and personal uncertainties are system- and patient-centered, respectively. These 3 main categories can be divided into more specific issues pertaining to health care; Figure 2 provides examples in the case of cancer. Scientific uncertainty encompasses uncertainties about diagnosis, prognosis, causal explanations, and treatment recommendations. Practical uncertainty applies to the structures and processes of care; examples include uncertainty about the competence of one’s physician, the quality of care one can expect to receive from a given clinician or institution, or the responsibilities and procedures one must undertake to access care. Personal uncertainty pertains to psychosocial and existential issues including the effects of one’s illness or treatment on one’s goals or outlook on life, on one’s personal relationships, the welfare of loved ones, or one’s sense of meaning in life. These non-scientific subtypes of uncertainty include issues identified in Kasper’s taxonomy—e.g., social integration, mastering of requirements, preferred role, physician trustability.
Figure 2.
Issues of uncertainty in health care
For each of these specific issues of uncertainty—scientific, practical, and personal—the underlying cause may be any of the sources comprising the 1st dimension of uncertainty: probability, ambiguity, complexity. Any or all of these sources may engender uncertainty about not only diagnosis, prognosis, causal explanations, and treatment recommendations (scientific uncertainty), but about the expected quality of care and the procedures required to access care (practical uncertainty), as well as the effects of illness or treatment on one’s personal relationships and goals in life (personal uncertainty). For example, a man contemplating radical prostatectomy for newly-diagnosed prostate cancer may experience uncertainty about numerous issues: the potential of cancer recurrence following surgery, the competence of his chosen surgeon and hospital, his ability to adapt to potential surgical side effects including erectile dysfunction and urinary incontinence, the impact of these side effects on his marital relationship, sense of well-being, and achievement of life goals. In theory, probabilities exist for all of these outcomes, although these probabilities are unknown—and thus ambiguous—in varying degrees, and further compounded by varying degrees of complexity.
The new integrative taxonomy further departs from previous efforts in specifying a third dimension of uncertainty: its locus. In any given clinical circumstance, uncertainty can exist in the minds of patients, clinicians, both, or neither, manifesting the fundamentally relational character of health care. Exactly where uncertainty resides depends on each party’s prior exposure to information about the ignorance pertaining to any given issue, and on the extent to which their mutual interactions result in a shared subjective awareness of ignorance. For example, uncertainty may be experienced by one party only, while the other remains in a state of relative metaignorance—lacking knowledge of what they do not know. This is the case when physicians are aware of scientific ignorance but fail to inform patients about it. In other cases, physicians and patients may be equally aware (uncertain) or unaware (meta-ignorant) of what they do not know. The locus of uncertainty thus constitutes a critical third dimension that manifests its subjective nature, and the extent to which uncertainty is socially constructed and addressed through the interactions of patients and health professionals.
Implications for research and clinical practice
The new integrative taxonomy synthesizes diverse theories and disciplinary perspectives on the phenomenon of uncertainty, and is intended to facilitate an organized approach to the problem of uncertainty. The taxonomy does not constitute a comprehensive theory of knowledge or ignorance, nor does it represent a causal model specifying the effects of different types of uncertainty on particular outcomes. Its categories and concepts, like those of existing taxonomies, are theoretical and have no definite grounding at an ontological level.49 Rather, the new taxonomy is a heuristic framework, the utility of which lies in its ability to map key dimensions of uncertainty—its issues (scientific, practical, personal), sources (probability, ambiguity, complexity), and locus (patient vs. clinician)—in a way that furthers its measurement and analysis by researchers and its diagnosis and management by clinicians.
The measurement and analysis of uncertainty
The principal value of the taxonomy for researchers is as a means of more precisely defining the phenomenon of uncertainty so that it can be better measured and analyzed. The new taxonomy conceptualizes uncertainty as a multi-dimensional phenomenon with theoretically distinct domains and constructs that are potentially measurable and related to different outcomes, mechanisms of action, and management strategies. This is a departure from past research which has either treated uncertainty as a monolithic phenomenon,18, 19 or has narrowly focused on uncertainties pertaining to particular sources or issues—e.g., probability, scientific uncertainty. By expanding the focus to other sources and issues as well as the locus of uncertainty, the new taxonomy provides a more comprehensive framework to guide the development of specific measures to ascertain patients’ experiences of different uncertainties, and the evaluation of how these uncertainties affect health outcomes and how well they are managed in clinical care. This is a research agenda of growing interest given broadening recognition of the management of uncertainty as a core function of patient-centered communication.8
The diagnosis, prognosis, and management of uncertainty
From a clinical standpoint, the principal value of the new taxonomy is as a means of facilitating the diagnosis and management of the uncertainties that arise in clinical practice. These include uncertainties pertaining to issues that are not only scientific but practical and personal, and that matter to patients. Differentiating these issues as well as the underlying sources of uncertainty (probability, ambiguity, complexity) enables clinicians to also establish the prognosis and thus the appropriate goals and strategies for managing uncertainty, since these characteristics dictate the extent to which uncertainty is reducible and warranted. For example, uncertainty arising primarily from complexity is theoretically reducible, as is uncertainty arising from misunderstandings of scientific evidence. In these cases, the appropriate goal is to reduce uncertainty by improving the comprehensibility and coherence of information, and correcting misconceptions. This requires specific tasks including simplifying, breaking down, and organizing information to make its gist meaning clear,50 and correcting underlying causes of misunderstanding. These causes include mixed messages and misinformation from various sources, including the deliberate “manufacturing” of scientific uncertainty in the service of other goals.51
In contrast, other types of uncertainty identified by the taxonomy are irreducible, and require different goals and management strategies. These include uncertainty arising from both probability and ambiguity—whether pertaining to the onset of disease, the benefits and harms of medical treatment, or the practical or personal consequences of illness and its treatment. In these circumstances the appropriate goal is not to reduce uncertainty but to increase it and assist coping efforts so that decisions are not impaired by anxiety but rather informed by the uncertainty, This is the instrumental goal articulated in the ideal of informed decision making, which advocates educating patients about the uncertainties regarding benefits and harms of medical interventions.52, 53
This goal of increasing uncertainty, however, poses several challenges. Prevailing wisdom and practice have supported what Babrow has termed an “ideology of uncertainty reduction” in health care.54 Furthermore, uncertainty may sometimes have undesirable psychological effects, including heightened perceptions and feelings of vulnerability and avoidance of decision making.28 Physicians are also known to be reluctant to disclose uncertainty to patients,12 and most health care interventions aim to reduce uncertainty. Furthermore, patients may also not desire or have sufficient psychological capacity to tolerate information about uncertainty.13, 55–57 There are also practical and ethical limits to increasing patient uncertainty—which takes time and risks overwhelming patients with information and diverting attention from other important clinical endeavors.58 Clinicians may not be able to fully address all of the uncertainties that present in a given situation. The challenge for future clinical practice is to develop ways of addressing these many concerns and barriers to increasing uncertainty in clinical encounters. In the meantime, the taxonomy might help clinicians to determine the scope of the uncertainties at hand, and to work with patients to prioritize which ones to address.
The new taxonomy can also facilitate the clinical diagnosis and management of uncertainty by drawing attention to the locus of uncertainty. This may clarify the respective informational needs and roles of patients and clinicians. For example, uncertainty about practical and personal issues may reside solely with the patient, while the clinician remains in a state of metaignorance. In this situation, the diagnosis of uncertainty depends on active elicitation of information by the clinician and communication by the patient. Conversely, scientific uncertainty may reside solely with the clinician, in which case its diagnosis depends on active communication by the clinician and elicitation by the patient. In either case, the new taxonomy highlights how the diagnosis of uncertainty in health care is a relational act. The relational nature of this act places differing responsibilities on clinicians and patients to exchange information and to achieve a shared consciousness of uncertainty. This is a goal articulated in the ideal of shared decision making52, 59 and in what Epstein has described as the achievement of “shared mind.”60
Yet the ultimate and most challenging task in managing uncertainty is not to establish its diagnosis or prognosis in the minds of patients and clinicians, but to help each party cope with uncertainty. We know the least about how to accomplish this task, since past work on this issue has been sparse and largely focused on the provision of information or the process of information exchange. For example, Mishel and colleagues recently developed and tested the effects of a “decision-making uncertainty management intervention” aimed at providing relevant information and teaching patient-physician communication skills to early stage prostate cancer patients.61 The intervention reportedly led to improvements in patient knowledge, information seeking and participation in decision making, and lower decisional regret, but not in mood or health-related quality of life. Yet this type of approach does not differ from previously studied informational interventions such as decision aids, all of which are built on the assumption that the successful management of uncertainty—and the most valid indicator of this outcome—consists of knowledge or care processes related to the provision or acquisition of information alone.62, 63
This cannot be the case, however, since these outcomes and indicators merely reflect the mitigation of reducible ignorance. The new taxonomy makes clear that the real problem is one of managing uncertainty arising from irreducible ignorance, and that this entails much more than filling in knowledge gaps. It requires helping patients—and health professionals—cope with the consciousness of ignorance that cannot be remediated. Such coping implies a deeper, broader acceptance of irreducible uncertainty in life, which Mishel characterizes as the adoption of a “probabilistic world view,”64 and Babrow views as a capacity to view uncertainty as a source of possibility or hope.54 This capacity is likely moderated by individual personality differences and other factors that remain to be elucidated.55, 56, 65, 66
The ultimate challenge for future clinical practice and research is to understand more precisely what coping with uncertainty entails and how it can be promoted. In the meantime, however, the new taxonomy provides a conceptual framework to help clinicians and researchers at least begin to get a handle on this problem that “creeps into every pore of medical practice.” It remains for future work to determine the utility of this taxonomy, to elucidate the mechanisms of uncertainty in health care, and to develop effective strategies for helping people cope with it in an adaptive way.
Acknowledgments
This work was supported by contract HHSN261200900524P from the National Cancer Institute, National Institutes of Health.
We thank Austin Babrow, Steve Clauser, Nananda Col, Ron Epstein, Baruch Fischhoff, Wendy Nelson, and Mary Politi for helpful discussions in the past. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Cancer Institute.
Footnotes
Portions of this work were presented at the 2009 International Conference on Communication in Healthcare, Miami, FL, October 4, 2009.
References
- 1.Eddy DM. Variations in physician practice: the role of uncertainty. Health Aff (Millwood) 1984 Summer;3(2):74–89. doi: 10.1377/hlthaff.3.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Babrow AS, Kasch CR, Ford LA. The many meaning of uncertainty in illness: toward a systematic accounting. Health Commun. 1998;10(1):1–23. doi: 10.1207/s15327027hc1001_1. [DOI] [PubMed] [Google Scholar]
- 3.Fox RC. The evolution of medical uncertainty. Milbank Mem Fund Q Health Soc. 1980 Winter;58(1):1–49. [PubMed] [Google Scholar]
- 4.Fox RC. Training for Uncertainty. In: Merton R, Reader GC, Kendall P, editors. The Student-Physician: Introductory Studies in the Sociology of Medical Education. Cambridge, MA: Harvard University Press; 1957. pp. 207–241. [Google Scholar]
- 5.Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. Washington, D.C.: The National Academies Press; 2009. Committee on Comparative Effectiveness Research Prioritization. [Google Scholar]
- 6.Congressional Budget Office. Research on the Comparative Effectiveness of Medical Treatments: Issues and Options for an Expanded Federal Role. The Congress of the United States; 2007. Dec, [Google Scholar]
- 7.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academies Press; 2001. Committee on Quality of Health Care in America. [Google Scholar]
- 8.Epstein RM, Street RLJ. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: 2007. NIH Publication No. 07-6225. [Google Scholar]
- 9.Light D., Jr Uncertainty and control in professional training. J Health Soc Behav. 1979 Dec;20(4):310–322. [PubMed] [Google Scholar]
- 10.Atkinson P. Training for certainty. Soc Sci Med. 1984;19(9):949–956. doi: 10.1016/0277-9536(84)90324-1. [DOI] [PubMed] [Google Scholar]
- 11.Gerrity MS, Earp JA, DeVellis RF, Light DW. Uncertainty and professional work: perceptions of physicians in clinical practice. American Journal of Sociology. 1992;97(4):1022–1051. [Google Scholar]
- 12.Katz J. Why doctors don't disclose uncertainty. Hastings Cent Rep. 1984 Feb;14(1):35–44. [PubMed] [Google Scholar]
- 13.Gerrity MS, DeVellis RF, Earp JA. Physicians' reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990 Aug;28(8):724–736. doi: 10.1097/00005650-199008000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Carney PA, Elmore JG, Abraham LA, et al. Radiologist uncertainty and the interpretation of screening. Med Decis Making. 2004 May-Jun;24(3):255–264. doi: 10.1177/0272989X04265480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carney PA, Yi JP, Abraham LA, et al. Reactions to uncertainty and the accuracy of diagnostic mammography. J Gen Intern Med. 2007 Feb;22(2):234–241. doi: 10.1007/s11606-006-0036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990;31(5):619–624. doi: 10.1016/0277-9536(90)90098-d. [DOI] [PubMed] [Google Scholar]
- 17.Geller G, Tambor ES, Chase GA, Holtzman NA. Measuring physicians' tolerance for ambiguity and its relationship to their reported practices regarding genetic testing. Med Care. 1993 Nov;31(11):989–1001. doi: 10.1097/00005650-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Mishel MH. The measurement of uncertainty in illness. Nurs Res. 1981 Sep-Oct;30(5):258–263. [PubMed] [Google Scholar]
- 19.Mishel MH. Adjusting the fit: development of uncertainty scales for specific clinical populations. West J Nurs Res. 1983 Fall;5(4):355–370. doi: 10.1177/019394598300500408. [DOI] [PubMed] [Google Scholar]
- 20.Politi MC, Han PK, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Med Decis Making. 2007 Sep-Oct;27(5):681–695. doi: 10.1177/0272989X07307270. [DOI] [PubMed] [Google Scholar]
- 21.Smithson M. Ignorance and Uncertainty: Emerging Paradigms. New York: Springer Verlag; 1989. [Google Scholar]
- 22.Lipshitz R, Strauss O. Coping with uncertainty: a naturalistic decision-making analysis. Organ Behav Hum Decis Process. 1997;69(2):149–163. [Google Scholar]
- 23.Thompson KM. Variability and uncertainty meet risk management and risk communication. Risk Anal. 2002 Jun;22(3):647–654. doi: 10.1111/0272-4332.00044. [DOI] [PubMed] [Google Scholar]
- 24.Smithson M. Ignorance and science: dilemmas, perspectives, and prospects. Knowledge: Creation, Diffusion, Utilization. 1993;15:133–156. [Google Scholar]
- 25.Bammer G, Smithson M, Group G. The nature of uncertainty. In: G G, Smithson M, editors. Uncertainty and Risk: Multidisciplinary Perspectives. London: Earthscan; 2008. pp. 289–304. [Google Scholar]
- 26.Merriam-Webster Online Dictionary. Merriam-Webster Online. [Accessed May 1, 2010]; Available at: http://www.merriam-webster.com/uncertainty.
- 27.Flavell JH. Metacognitive aspects of problem solving. In: Resnick LB, editor. The Nature of Intelligence. Hillsdale, N.J.: Erlbaum; 1976. pp. 231–236. [Google Scholar]
- 28.Mishel MH. Uncertainty in illness. Image J Nurs Sch. 1988 Winter;20(4):225–232. doi: 10.1111/j.1547-5069.1988.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 29.Kasper J, Geiger F, Freiberger S, Schmidt A. Decision-related uncertainties perceived by people with cancer--modelling the subject of shared decision making. Psychooncology. 2008 Jan;17(1):42–48. doi: 10.1002/pon.1190. [DOI] [PubMed] [Google Scholar]
- 30.Ayyub BM. Elicitation of Expert Opinions for Uncertainty and Risks. Boca Raton: CRC Press; 2001. [Google Scholar]
- 31.Ellsberg D. Risk, ambiguity, and the Savage axioms. Quart J Econ. 1961;75:643–669. [Google Scholar]
- 32.Camerer C, Weber M. Recent developments in modeling preferences: uncertainty and ambiguity. Journal of Risk and Uncertainty. 1992;5:325–370. [Google Scholar]
- 33.Smithson M. Conflict Aversion: Preference for Ambiguity vs Conflict in Sources and Evidence. Organ Behav Hum Decis Process. 1999 Sep;79(3):179–198. doi: 10.1006/obhd.1999.2844. [DOI] [PubMed] [Google Scholar]
- 34.U.S. Environmental Protection Agency. Guidelines for Carcinogen Risk Assessment. U.S. Environmental Protection Agency; 2005. Vol EPA/630/P-03/001F. [Google Scholar]
- 35.Marks H, Coleman M, Michael M. Further deliberations on uncertainty in risk assessment. Human and Ecological Risk Assessment. 2003;9:1399–1410. [Google Scholar]
- 36.Apostolakis G. The concept of probability in safety assessments of technological systems. Science. 1990;250:1359. doi: 10.1126/science.2255906. [DOI] [PubMed] [Google Scholar]
- 37.Morgan MG, Henrion M. Uncertainty: a Guide to Dealing with Uncertainty in Quantitative Risk and Policy Analysis. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- 38.Walker VR. The siren songs of science: toward a taxonomy of scientific uncertainty for decisionmakers. Connecticut Law Review. 1991;23:567–626. [Google Scholar]
- 39.Walker VR. Risk regulation and the "faces" of uncertainty. Risk: Health, Safety & Environment. 1998 Winter;27:27–38. [Google Scholar]
- 40.Edwards JA. Effects of causal uncertainty on the dispositional attribution process. Journal of Experimental Social Psychology. 1998;34:109–135. [Google Scholar]
- 41.Sloman SA. Causal Models: How People Think About the World and Its Alternatives. Oxford: Oxford University Press; 2005. [Google Scholar]
- 42.Spiegelhalter DJ. Understanding uncertainty. Ann Fam Med. 2008 May-Jun;6(3):196–197. doi: 10.1370/afm.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodman SN. Probability at the bedside: the knowing of chances or the chances of knowing? Ann Intern Med. 1999 Apr 6;130(7):604–606. doi: 10.7326/0003-4819-130-7-199904060-00022. [DOI] [PubMed] [Google Scholar]
- 44.Quill TE, Suchman AL. Uncertainty and control: learning to live with medicine's limitations. Humane Med. 1993 Apr;9(2):109–120. [PubMed] [Google Scholar]
- 45.Parry C. Embracing uncertainty: an exploration of the experiences of childhood cancer survivors. Qual Health Res. 2003 Feb;13(2):227–246. doi: 10.1177/1049732302239600. [DOI] [PubMed] [Google Scholar]
- 46.Kleinman A. Patients and Healers in the Context of Culture. Berkeley: University of California Press; 1980. [Google Scholar]
- 47.Budescu DV, Weinberg S, Wallsten TS. Decisions based on numerically and verbally expressed uncertainties. J of Experimental Psychology: Human Perception and Performance. 1988;14:281–294. [Google Scholar]
- 48.Wallsten TS. The costs and benefits of vague information. In: Hogarth RM, editor. Insights in Decision Making: a Tribute to Hillel J. Einhorn. Chicago: University of Chicago Press; 1990. pp. 28–43. [Google Scholar]
- 49.Winkler RL. Uncertainty in probabilistic risk assessment. Reliability Engineering and System Safety. 1996;54:127–132. [Google Scholar]
- 50.Reyna VF. A theory of medical decision making and health: fuzzy trace theory. Med Decis Making. 2008 Nov-Dec;28(6):850–865. doi: 10.1177/0272989X08327066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Michaels D, Monforton C. Manufacturing uncertainty: contested science and the protection of the public's health and environment. Am J Public Health. 2005;95(Suppl 1):S39–S48. doi: 10.2105/AJPH.2004.043059. [DOI] [PubMed] [Google Scholar]
- 52.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997 Mar;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 53.Whitney SN. A new model of medical decisions: exploring the limits of shared decision making. Med Decis Making. 2003 Jul-Aug;23(4):275–280. doi: 10.1177/0272989X03256006. [DOI] [PubMed] [Google Scholar]
- 54.Babrow AS, Kline KN. From "reducing" to "coping with" uncertainty: reconceptualizing the central challenge in breast self-exams. Soc Sci Med. 2000 Dec;51(12):1805–1816. doi: 10.1016/s0277-9536(00)00112-x. [DOI] [PubMed] [Google Scholar]
- 55.Budner S. Intolerance of ambiguity as a personality variable. Journal of Personality. 1962;30:29–59. doi: 10.1111/j.1467-6494.1962.tb02303.x. [DOI] [PubMed] [Google Scholar]
- 56.Buhr K, Dugas M. Intolerance for uncertainty scale: Psychometric properties of the English version. Behav Res Ther. 2002;40:931–946. doi: 10.1016/s0005-7967(01)00092-4. [DOI] [PubMed] [Google Scholar]
- 57.Greco V, Roger D. Coping with uncertainty: the construction and validation of a new measure. Personality and Individual Differences. 2001;31:519–534. [Google Scholar]
- 58.Epstein RM, Korones DN, Quill TE. Withholding information from patients--when less is more. N Engl J Med. Feb 4;362(5):380–381. doi: 10.1056/NEJMp0911835. [DOI] [PubMed] [Google Scholar]
- 59.Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004 Jan 6;140(1):54–59. doi: 10.7326/0003-4819-140-1-200401060-00012. [DOI] [PubMed] [Google Scholar]
- 60.Epstein RM, Peters E. Beyond information: exploring patients' preferences. Jama. 2009 Jul 8;302(2):195–197. doi: 10.1001/jama.2009.984. [DOI] [PubMed] [Google Scholar]
- 61.Mishel MH, Germino BB, Lin L, et al. Managing uncertainty about treatment decision making in early stage prostate cancer: a randomized clinical trial. Patient Educ Couns. 2009 Dec;77(3):349–359. doi: 10.1016/j.pec.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 62.Kennedy DM. On what basis should the effectiveness of decision aids be judged? Health Expect. 2003;6:255–268. doi: 10.1046/j.1369-6513.2003.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA. Rethinking the objectives of decision aids: a call for conceptual clarity. Med Decis Making. 2007 Sep-Oct;27(5):609–618. doi: 10.1177/0272989X07306780. [DOI] [PubMed] [Google Scholar]
- 64.Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch. 1990;22(4):256–262. doi: 10.1111/j.1547-5069.1990.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 65.Kruglanski AW, Webster DM. Motivated closing of the mind: "seizing" and "freezing". Psychological Review. 1996;103(2):263–283. doi: 10.1037/0033-295x.103.2.263. [DOI] [PubMed] [Google Scholar]
- 66.Sorrentino RM, Roney CJR. The Uncertain Mind: Individual Differences in Facing the Unknown. Philadelphia: Taylor & Francis; 2000. [Google Scholar]