Abstract
Cerebrospinal fluid (CSF) otorrhoea is an uncommon condition arising from defects in the tegmen and middle cranial fossa. 33 year gentleman presented with post-mastoidectomy CSF otorrhoea of 5 year duration. Imaging finding were suggestive of fracture in the tegmen region. A combined middle cranial fossa/transmastoid was used to repair the defect. Defect was identified in the tegmen plate and it was closed with pedicled pericranial graft, laterally based pedicled temporalis muscle graft reinforced by bone dust and supported with intact mucosal flap. The leak stopped completely following surgery. The patient is doing well at follow up. Repair of these defects need careful analysis of imaging findings to understand pathological anatomy, and a well planned surgical approach to achieve meticulous repair.
Keywords: Temporal bone, Fracture, Otorrhoea, Cerebrospinal fluid, Mastoidectomy
Introduction
Cerebrospinal fluid (CSF) otorrhoea is an uncommon condition arising from defects in the tegmen and middle cranial fossa and may be spontaneous or secondary to trauma, chronic ear disease, tumour or surgical procedures those extends through or into the temporal bone [1–3]. We discuss imaging and operative findings in a case of post- mastoidectomy CSF otorrhoea and describe our combined middle cranial fossa and transmastoid approach.
Case Reports
33 year gentleman presented with watery discharge from left ear for last 5 years. He underwent left sided mastoid exploration 5 year back for chronic suppurative otitis media with choleastetoma. He developed this watery discharge immediately following mastoidectomy that was persisting off and on. There was no history of fever or altered sensorium in the past. On ear examination, the patient had an open well healed mastoid cavity with healthy granulations tissue. There were no focal deficits except conductive hearing loss in left ear. Otoendoscopy showed collection of clear fluid collection in the area of Troutman’s triangle without any obvious site of leak. Watery discharge from the ear was positive for glucose suggestive of CSF and fluid culture was sterile. Thin sliced CT scan showed evidence of mastoidectomy and a break in continuity of the tegmen (Figs. 1, 2). Magnetic resonance imaging (MRI) showed the thickening of mastoid mucosa and upward extension of mucosal pocket (Figs. 3, 4). Based on imaging findings fracture involving the tegmen region with CSF fistula was suspected. The patient was planned for combined intracranial and trans-mastoid approach for the repair of the defect. Previous incision was extended in question marked manner to facilitate combined approach and wider exposure (Fig. 5). Scalp flap was raised and at the same time pedicled pericranial graft was harvested (Fig. 6) for middle cranial fossa repair and also muscle graft was prepared for closure of defect through mastoid cavity (Fig. 7). Temporal craniotomy was performed and bone dust was collected. Anterior and superior surface of petrous temporal bone were exposed from lateral to medial aspect. Initially there were vascular markings confined to the inner table without any breach in the bone (Fig. 8). Further exploration revealed a large defect over the anterior surface of the 4 petrous bone (Fig. 9). Margins of the defect were irregular and mastoid mucosa could be seen through the defect. Bony defect was defined all around and the dura was elevated around the defect. There was leakage of CSF through the defect in the dura (Fig. 9a). It was difficult to repair the deep seated dural defect. Bone dust collected during craniotomy was placed in the defect to facilitate osteogenesis. Pedicled pericranial graft harvested in the beginning lay down outside the dura while covering the defect completely. Gel foam was placed over the graft and outside the dura to keep it in place and at the same time a hitch stitch was taken to hold the graft in place. Following intracranial repair mastoid cavity was explored and mucosal flap was raised. Defect was identified in the tegmen plate and the defect was closed by bone dust and reinforced with laterally based pedicled temporalis muscle graft supported with intact mucosal flap. The leak stopped completely following surgery. The patient is doing well at 18 months follow up.
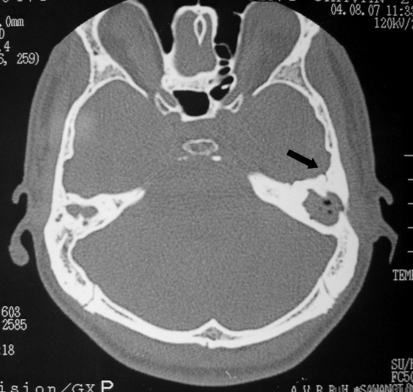
Fig. 1.
CT scan axial image bone window showing linear fracture running through the anterior surface of petrous temporal bone (arrow)
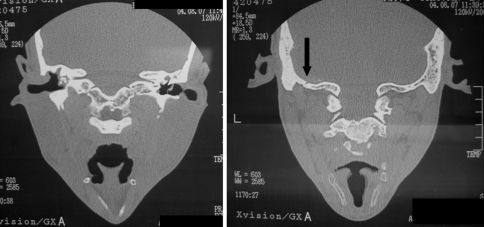
Fig. 2.
CT scan direct coronal cuts bone window showing thinned out petrous temporal bone (left) and linear fracture (right image arrow)
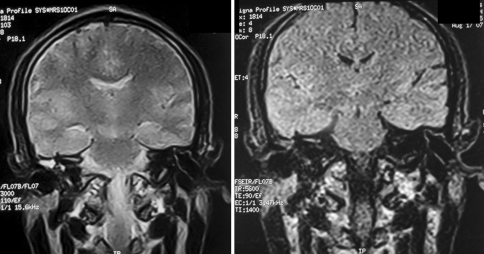
Fig. 3.
MRI coronal sections T2W (left) and FLAIR (right) images showing thickened mucosa in left mastoid with protrusion of a pocket towards dura
Fig. 4.
MRI FLAIR image magnified view showing thickening and upward protrusion of mucosa
Fig. 5.
Clinical photograph showing previous scar (left) and planned incision (right)
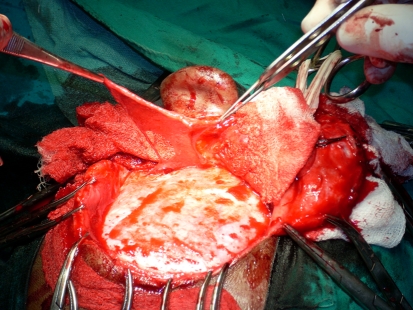
Fig. 6.
Clinical photograph showing wide exposure of mastoid and petrous temporal area and pedicled long pericranial graft
Fig. 7.
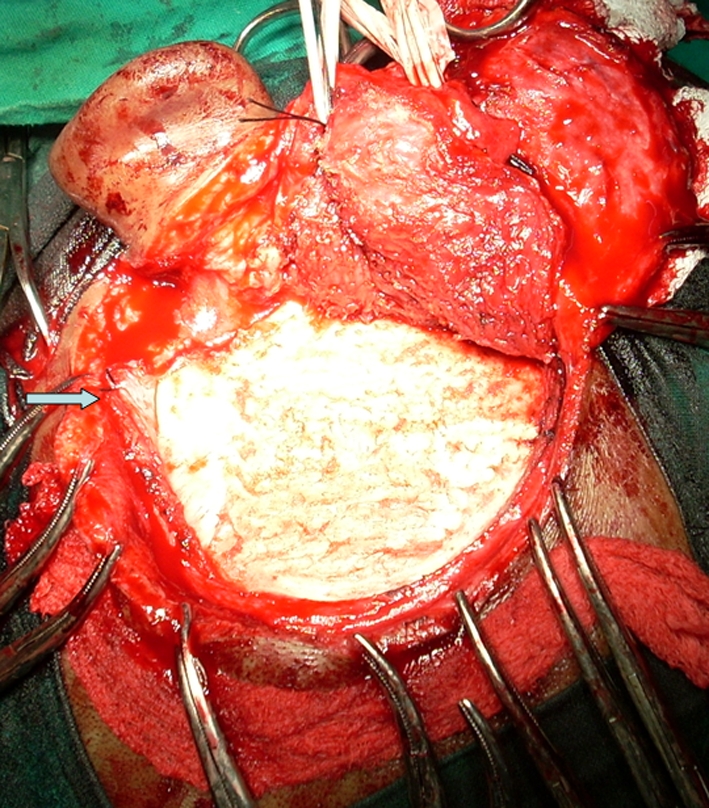
Clinical photograph showing pedicled temporalis muscle graft (white arrow) used to reinforce the closure of mastoid process from lateral side
Fig. 8.
Intra-operative photograph showing vascular marking mimicking linear fracture
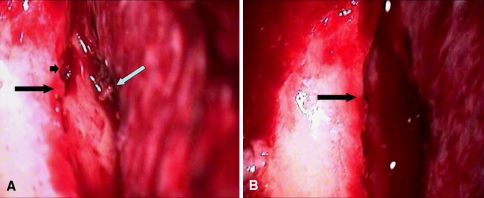
Fig. 9.
a Intra-operative photograph showing linear fracture with irregular margins (long black arrow) and dural tear (white arrow), mastoid mucosa can be seen through the fracture (long black arrow). b Close view of the fracture line
Discussion
The temporal lobe of the brain is separated from the middle ear and the mastoid process by a thin plate of bone known as tegmen [3]. CSF egress from the subarachnoid space into the pneumatised spaces of the temporal bone and most commonly results from fracture of the temporal bone particularly associated with laceration of dura and arachnoid. The pulsatile CSF pressure progressively drives the dura through the bone defect and one way valve system and blocking action of brain tissue keeps the defect patent [4]. In present case patient underwent mastoidectomy 5 year back, probably the use of chisel and hammer to perform the surgery would had been resulted in the fracture of thin tegemen plate and laceration of dura with consequent CSF leak. Because of pulsatile nature of brain the defect continued to be patent and the CSF leak was persisting. High resolution CT scan with and without using contrast may locate defects of the legmen plate which may be associated with soft tissue density in the mastoid. On CT scan pre-operatively we could suspect defect in the tegmen, however exact extent could not be determined. Role of MRI has been questioned as it does not have any added advantage over CT scan, since herniating brain tissue is non-functioning [5]. The soft tissue density may indicate either granulation tissue or herniating brain tissue [5]. However in present case upward extension of mastoid mucosa on MRI supported our suspicion of fracture and this mucosal extension could be visualized intra-operatively (Fig. 2a, small black arrow). CSF otorrhoea arising from defects in the tegmen and middle fossa dura can be managed by an intra-cranial repair, extracranial transmastoid or a combined approach with their advantages and disadvantages (Table 1). Because we were not sure about the extent of the defect and patient had problem for a quite long time we opted for the combined middle cranial fossa/transmastoid approach successfully. Materials used to repair and reinforce the defect include temporalis fascia, free muscle graft, Oxycel cotton, calvarial bone, pericranium, bone wax, and fibrin glue [1, 6]. Acellular dermal allograft is used successfully for skull base defects as these are easy to manipulate endoscopically, provides an effective seal and barrier in skull base reconstruction and avoids the need for a donor site [7]. Bone plate can effectively seal multiple defects in the tegmen plate without any risk of migration [6]. In our case use of pedicled pericranial graft, pedicled temporalis muscle graft and judicious use of bone dust avoided the need of any other material either from donor site or commercial. Post operative CSF drainage by lumbar puncture or drain can act as a safety measure and depends upon size and site of defect. Yet the very need for post operative lumbar drainage may be questioned [8]. Multiple layers of support in our case prevented us to use post-operative lumbar drain. As per recommendation we used intravenous antibiotic for couple of days followed by oral antibiotic for one week. Though, the use of antibiotic prophylaxis is controversial and not routinely indicated [5, 8]. To prevent CSF otorrhoea during mastoidectomy, a thorough knowledge of the surgical anatomy of the temporal bone is very essential. The surgeon must be careful while drilling near the tegmen and posterior fossa dura. Now a day’s use of drills has prevented such type of trauma. Still in developing and underdeveloped where the facilities are meager these complications do occur. Repair of these defects need careful analysis of imaging findings to understand pathological anatomy, and a well planned surgical approach to achieve meticulous repair.
Table 1.
Summary of approaches their indication, advantages and disadvantages for the management of CSF otorrhoea
| Approach | Indications and advantages | Disadvantages |
|---|---|---|
| Transmastoid approach [9] | Reduces patient morbidity by obviating the need for middle cranial fossa approach | Less than satisfactory [6] |
| Use of hydroxyappetite cement avoid donor soft tissue sites | Inadequate if there are multiple tegmen defects [1] | |
| No spinal drainage | ||
| The intra-cranial and combined approach [1] | Direct visualization and precise intra- and/or extra-dural intracranial placement of a graft can be secured by sutures [10] | The morbidity associated with a temporal craniotomy [10] |
| Useful in multiple tegmen defects [1] | ||
| Middle cranial fossa approach [6] | Provides extended exposure | |
| More effective than the transmastoid approach for the repair of CSF leaks and brain hernias through tegmen plate defects | ||
| Can be used in cases with recurrence after attempted closure from the mastoid | ||
| Useful in very large tegmen tympani defect, multiple defects | ||
| Hearing preservation | ||
| Transmastoid repair with mini craniotomy [2, 10] | When the defect is either questionable on CT scan or localized in the posterior part of the tegmen tympani | Only for small and accessible defects |
| Avoid the morbidity of middle fossa craniotomy |
References
- 1.Brown NE, Grundfast KM, Jabre A, Megerian CA, O’Malley BW, Jr, Rosenberg SI. Diagnosis and management of spontaneous cerebrospinal fluid-middle ear effusion and otorrhea. Laryngoscope. 2004;114(5):800–805. doi: 10.1097/00005537-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gacek RR, Gacek MR, Tart R. Adult spontaneous cerebrospinal fluid otorrhea: diagnosis and management. Am J Otol. 1999;20(6):770–776. [PubMed] [Google Scholar]
- 3.Glasscock ME, Dickins JRE, Jackson CG, Wiet RJ, Feenstra L. Surgical management of brain tissue herniation into the middle car and mastoid. Laryngoscope. 1979;89:1743–1754. doi: 10.1288/00005537-197911000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Neely JG, Neblett CR, Rose JE. Diagnosis and treatment of spontaneous cerebrospinal fluid otorrhea. Laryngoscope. 1982;92:609–612. doi: 10.1288/00005537-198206000-00001. [DOI] [PubMed] [Google Scholar]
- 5.McGuirt WF, Stool SE. Cerebrospinal fluid fistuala: the identification and management in pediatric temporal bone features. Laryngoscope. 1995;105(4):359–364. doi: 10.1288/00005537-199504000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Dutt SN, Mirza S, Irving RM. Middle cranial fossa approach for the repair of spontaneous cerebrospinal fluid otorrhoea using autologous bone pate. Clin Otolaryngol Allied Sci. 2001;26(2):117–123. doi: 10.1046/j.1365-2273.2001.00438.x. [DOI] [PubMed] [Google Scholar]
- 7.Lorenz RR, Dean RL, Hurley DB, Chuang J, Citardi MJ. Endoscopic reconstruction of anterior and middle cranial fossa defects using acellular dermal allograft. Laryngoscope. 2003;113(3):496–501. doi: 10.1097/00005537-200303000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Pachauri R, Nagaonkar S, Kirtane MV. Spontaneous CSF otorrhoea—presenting as conductive deafness. Indian J Otolaryngol Head Neck Surg. 2002;54(1):51–54. doi: 10.1007/BF02911008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kveton JF, Goravalingappa R. Elimination of temporal bone cerebrospinal fluid otorrhea using hydroxyapatite cement. Laryngoscope. 2000;110(10 Pt 1):1655–1659. doi: 10.1097/00005537-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Adkins WY, Osguthorpe JD. Minicraniotomy for management of CSF otorrhoea from tegmen defects. Laryngoscope. 1983;93:1038–1040. doi: 10.1288/00005537-198308000-00012. [DOI] [PubMed] [Google Scholar]