Abstract
Skull base metastases though a rare entity, is a known end stage presentation of Bronchogenic carcinoma. Skull base metastases can present as various cranial dysfunction syndromes, namely: Collet-Siccard syndrome, Villaret syndrome, Occipital condyle syndrome, Jugular foramen syndrome, and Parasellar syndrome. Skull base metastases need to be differentiated from Primary Temporal Bone malignancy. We in this article present a case report of Skull base metastases from Bronchogenic carcinoma with associated metastases to external auditory canal and upper cervical lymph nodes; hitherto unreported association.
Keywords: Skull base metastases, Bronchogenic carcinoma, Collet-siccard syndrome
Introduction
The true incidence of skull base metastases is unknown. The estimated incidence of brain metastases is in the range of 12–35% of all cancer patients [1–3]. The largest series dealing with skull base metastasis demonstrated breast, lung, prostate, and head and neck carcinomas as the most common malignancies [4]. Skull base metastases tend to localize to certain areas. The middle fossa, jugular foramen, and parasellar sites are most frequently involved.
We report the first case in English literature of Collet-Siccard syndrome with associated metastasis to external auditory canal and upper cervical lymph nodes from Small cell Bronchogenic carcinoma.
Case Report
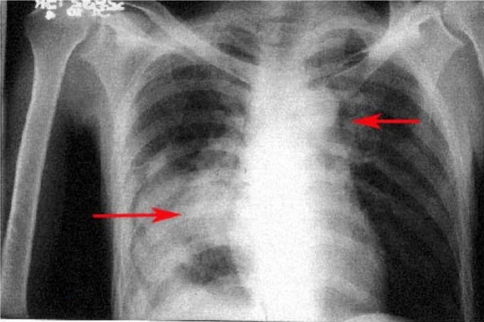
A 40 year male patient presented to the Out Patient Department of ENT and Head and Neck Surgery of Adesh Institute of Medical Sciences and Research with the complaints of fever, productive cough, hemoptysis and weight loss for 3 months duration. He was diagnosed outside as case of pulmonary tuberculosis and was on antitubercular therapy. For 1 month he had developed dysphagia, hoarseness of voice, nasal regurgitation and deviation of face to the left side; along with one episode of general tonic clonic seizures during this period. He also complained of severe right sided frontotemporal headache, nausea and vomiting. He denied any history of diplopia, decreased hearing, weakness of limbs, ataxia, and any other neurological problem. Otological examination revealed bleeding lesion in the postero-superior and postero-inferior quadrants of the right external auditory canal. There was 2 × 2 cm level II hard, mobile lymph node on the right side with associated 7th, 9→12th cranial nerve palsies on the right side. On auscultation of chest, there were bilateral coarse crepts. Abdominal examination was normal. Keeping primary temporal bone malignancy with cervical lymph node metastases as the initial diagnosis, biopsy from external auditory canal and fine needle aspiration cytology (FNAC) from cervical lymph node metastases was done. Biopsy and FNAC both revealed the lesion to be Small cell carcinoma, probably metastatic. Patient was further investigated. X-ray chest revealed bilateral lung infiltrates (Fig. 1). CECT Chest revealed 5 × 6 × 9 cm size well defined heterogeneous mass lesion encasing bronchus intermedius and right lower lobe bronchus and its segmental divisions with subcarinal adenopathy and multiple well defined size nodules in both lung fields suggestive of metastases. CT guided FNAC of lung lesion revealed it to be Small cell carcinoma. MR imaging of Brain with contrast revealed a large soft tissue lesion in the region of base of skull on right side around the clivus involving the ipsilateral occipital condyle with extension into the mastoid air cells and right half of the anterior arch of the atlas and right cervicomedullary cistern with extradural extension across right cerebellar hemisphere (Figs. 2, 3, 4). This workup placed patient in Extended Stage category. Palliative radiotherapy was started but the patient succumbed to the disease within 15 days.
Fig. 1.
X-ray chest antero-posterior view showing B/L lung infiltrates (marked as arrows)
Fig. 2.

Gadolinium enhanced MR scan axial view showing non-contrast enhancing large soft tissue lesion in the region of base of skull on right side around the clivus with extension into the mastoid air cells (marked as arrow)
Fig. 3.
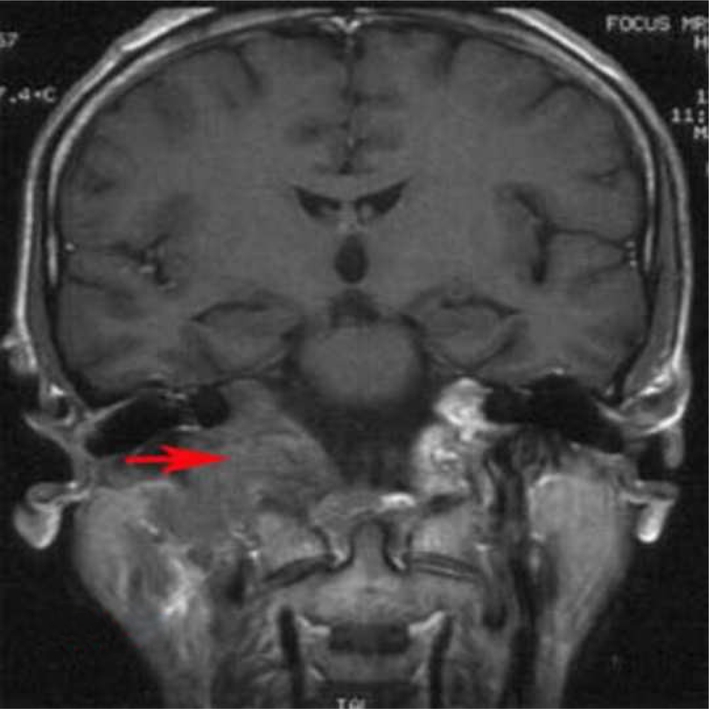
Gadolinium enhanced MR scan coronal view showing soft tissue lesion in base of skull on right side with extension into the ipsilateral occipital condyle and right half of the atlas (marked as arrow)
Fig. 4.

T2 MR scan sagittal view showing soft tissue lesion in the skull base with extradural extension across right cerebellar hemisphere (marked as arrow)
Discussion
A surprisingly wide variety of primary tumors can metastasize to the skull base. Often these patients present with cranial nerve deficits or other focal symptoms from the metastatic tumor and are without symptoms referable to the primary site. Not infrequently, the primary tumor is not identified until biopsy tissue is obtained. Prostate and lung have been reported as the most common primary sites [5]. Other tumors include carcinomas of pancreas, kidney, thyroid, breast and colon.
The most detailed studies on skull metastases are on those located in the orbit and temporal bone. Metastatic tumors to the temporal bone are uncommon and usually are seeded by the hematogenous route [6, 7]. The most common metastatic lesion in the temporal bone is breast carcinoma [8]. Lung, prostate, and renal carcinomas are all well documented for their metastatic potential to the temporal bone.
Metastases to the skull base affect the neurovascular structures entering the foramina of the basicranium. Greenberg et al. [4] described cranial dysfunction syndromes caused by skull base metastases. These include Collet-Siccard syndrome [9], which is a palsy of the lower four cranial nerves; Villaret syndrome [10], which is a palsy of the lower four cranial nerves with ipsilateral Horner syndrome; Occipital condyle syndrome [11], which consists of unilateral occipital pain with ipsilateral 12th nerve paresis; Jugular foramen syndrome [12] with dysphagia and neck pain; Parasellar syndrome [13] with extra ocular palsy and isolated 3rd, 6th or 7th cranial nerve palsies. Cranial nerve palsies secondary to skull base metastases represent an uncommon presentation of advanced bronchogenic carcinoma. Nonetheless, these palsies usually have a significant impact on a patient’s quality of life. Our patient had presented with lower cranial nerve palsies i.e. Collet-Siccard syndrome along with 7th cranial nerve palsy.
Small cell carcinoma is an aggressive pulmonary neoplasm that comprises about 15–20% of all pulmonary carcinomas [14]. Invasion of small blood vessels and lymphatics is evident in most tumors at an early stage, and local lymphangitic spread is not uncommon in the adjacent lung. Extra thoracic metastases develop from spread via the lymphatics and blood vessels [15]. Metastasis occurs frequently to the scalene group of lymph nodes [16]. However, metastasis to upper cervical lymph nodes is a rare presentation. The patient described above had presented with Level II cervical lymph node metastases; this presentation along with Collet-Siccard syndrome has not been described before. Cerebral metastases are common in patients who have small cell carcinoma, being discovered at autopsy in 40% of patients in one series [17]. Parenchymal and leptomeningeal metastases are the more common among these [18]. Skull base metastases with associated lower cranial nerve palsies are a rare presentation.
Due to its high-resolution bone algorithms, it is believed that CT scanning is superior to MRI studies for determining bone involvement and destruction at the skull base, whereas MRI studies are more sensitive in detecting leptomeningeal, dural, or cranial nerve involvement [19–21]. Therefore, both CT and MRI appear to have role in patients who present with cranial nerve deficits, because they may be used in a complimentary fashion to demonstrate the full extent of the disease.
With regard to treatment, a brief course of external beam radiation therapy in association with corticosteroid administration is extremely effective in achieving palliative benefits. The dose schedules of 3000 cGy in 10 fractions or 2000 cGy in 5 fractions both are considered standard palliative treatment regimens that offer similar biologic equivalent doses.
The patient died before any potential treatment benefit could be assessed. Typically, the significance of such wide ranging metastasis in a patient with disseminated bronchogenic carcinoma is the poor prognosis it imparts.
Conclusion
The diagnosis of metastases to the skull base should be considered strongly in patients who have cranial nerve palsies and bronchogenic carcinoma. Although the presentation is heterogeneous, it can be diagnosed readily with the use of modern imaging techniques. Although the development of cranial nerve deficits is often a poor prognostic sign, a cohort of patients who live for a significant time can benefit from palliative radiation therapy.
References
- 1.Martinez AJ. Classification and pathology of skull base tumors. In: Tindall GT, Cooper PR, Barrow DL, editors. The practice of neurosurgery, vol I. Baltimore: Williams and Wilkins; 1996. pp. 889–900. [Google Scholar]
- 2.Galicich JH, Arbit E, Wronski M. Metastatic brain tumors. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. 2. New York: Macgraw Hill; 1996. pp. 807–821. [Google Scholar]
- 3.Possner JB, Chunik NL. Intracranial metastases from systemic cancer. Adv Neurol. 1978;19:119–120. [PubMed] [Google Scholar]
- 4.Greenberg HS, Deck MDF, Vikram B. Metastasis to the base of the skull: clinical findings in 43 patients. Neurology. 1981;31:530–537. doi: 10.1212/wnl.31.5.530. [DOI] [PubMed] [Google Scholar]
- 5.Hirai O, Kikuchi H, Hashimoto N. Skull base metastasis. Head Neck. 1991;13:89. doi: 10.1002/hed.2880130202. [DOI] [PubMed] [Google Scholar]
- 6.Feinmesser R, Libson Y, Uzicly B, et al. Metastatic carcinoma to the temporal bone. Am J Otol. 1986;7:119–120. [PubMed] [Google Scholar]
- 7.Hill BA, Kohut RI. Metastatic adenocarcinoma of the temporal bone. Arch Otolaryngol. 1976;102:568–571. doi: 10.1001/archotol.1976.00780140100015. [DOI] [PubMed] [Google Scholar]
- 8.Imamura S, Mukakanki Y. Secondary malignant tumors of the temporal bone. A histopathologic study and review of the world literature. J Oto-Rhino-Laryngol Soc Japan (Nippon Jibinkoka Gakkai Kacho) 1991;94:924–937. doi: 10.3950/jibiinkoka.94.924. [DOI] [PubMed] [Google Scholar]
- 9.Prashant R, Franks A. Collet-Siccard syndrome-a report and review. Lancet Oncology. 2003;4:376–377. doi: 10.1016/S1470-2045(03)01097-0. [DOI] [PubMed] [Google Scholar]
- 10.Sicenica T, Venkata Balaji G, Klein A, et al. Villaret’s syndrome in a man with prostate carcinoma. Am J Med. 2000;108:516–517. doi: 10.1016/S0002-9343(99)00319-8. [DOI] [PubMed] [Google Scholar]
- 11.Capobianco DJ, Brazis PW, Rubino FA, et al. Occipital condyle syndrome. Headache. 2002;42:142–146. doi: 10.1046/j.1526-4610.2002.02032.x. [DOI] [PubMed] [Google Scholar]
- 12.Wilson H, Johnson DH. Jugular foramen syndrome as a complication of metastatic cancer of the prostate. South Med J. 1984;77:92–93. doi: 10.1097/00007611-198401000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Ransom DT, Dinapoli RP, Richardson RL. Cranial nerve lesions due to base of the skull metastases in prostate carcinoma. Cancer. 1990;65:586–589. doi: 10.1002/1097-0142(19900201)65:3<586::AID-CNCR2820650333>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 14.Carter D. Small cell carcinoma of the lung. Am J Surg Pathol. 1983;7:787. doi: 10.1097/00000478-198312000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Hirsch FR. Histopathologic classification and metastatic pattern of small cell carcinoma of the lung. Copenhagen: Munksgaard; 1983. [Google Scholar]
- 16.Shields TW. An evaluation of bronchogenic carcinoma in scalene lymph nodes. Union Internationalis Contra Cancrum Acta. 1959;15:508. [PubMed] [Google Scholar]
- 17.O’Neill BP, Buckner JC, Coffrey RJ. Brain metastatic lesions. Mayo Clinics Proc. 1994;69:1062. doi: 10.1016/s0025-6196(12)61374-3. [DOI] [PubMed] [Google Scholar]
- 18.Burgess RE, Burgess VF, Dibella NJ. Brain metastases in small cell carcinoma of the lung. JAMA. 1979;242:2084. doi: 10.1001/jama.242.19.2084. [DOI] [PubMed] [Google Scholar]
- 19.Weber AL. Radiologic evaluation of the jugular foramen. Anatomy, vascular variants, anomalies, and tumors. Neuroimaging Clin N Am. 1994;4(3):579–598. [PubMed] [Google Scholar]
- 20.Durden DD, Williams DW., III Radiology of skull base neoplasms. Otolaryngol Clin North Am. 2001;34:1043–1064. doi: 10.1016/S0030-6665(05)70364-9. [DOI] [PubMed] [Google Scholar]
- 21.Chong VF, Khoo JB, Fan YF. Imaging of the nasopharynx and skull base. Magn Reson Imaging Clin N Am. 2002;10:547–571. doi: 10.1016/S1064-9689(02)00010-7. [DOI] [PubMed] [Google Scholar]