Abstract
A young man presenting with complaints of progressive deafness in both ears with recent onset of facial paralysis was found to have necrotic debris in the nasal cavity. He was diagnosed to have limited form of Wegener’s granulomatosis on the basis of nasal biopsy. There was delay in diagnosis as the patient was having atypical and predominantly otological presentation of a potentially serious systemic disorder, Wegener’s granulomatosis. In this case report, emphasis was given on the necessity of comprehensive evaluation of the patients to avoid pitfalls in diagnosis.
Keywords: Wegener Granulomatosis, Facial paralysis, Otitis media, Deafness
Introduction
Wegener’s Granulomatosis is an idiopathic necrotizing systemic vasculitis involving both upper and lower respiratory tracts with cutaneous lesions and renal involvement. It is called limited Wegener’s Granulomatosis when kidneys are not involved. The main otolaryngological manifestation is rhinosinusitis. We are reporting a case of Wegener’s Granulomatosis presenting with otological symptoms which is a rare occurrence.
Case Report
A 25 year male patient presented with complaints of hardness of hearing in both ears since 6 months, facial asymmetry since 4 months, cutaneous ulceration over both distal legs since 1 month and cough since 2 weeks. Patient was treated in vain, for his progressive bilateral hearing loss by tympanostomy tube placement at a different centre 4 months back. Cutaneous ulceration over both legs was preceded by vesiculo-bullous lesions followed by sloughening. Detailed history revealed significant weight loss and general debility over the past 6 months. Progressive weight loss and cutaneous ulceration led us to suspect presence of a systemic pathology rather than a localized ENT disorder.
On examination patient has bilateral tympanic membrane perforation with granulations in middle ear, moderately severe mixed hearing loss, right facial nerve lower motor neuron paralysis (Fig. 1), and bilateral crepitations in all lung fields. Extensive cutaneous ulceration with sloughening over both lower legs was suggestive of cutaneous vasculitis. Diagnostic nasal endoscopy revealed minimal blackish crusting with granulation tissue at posterior end of nasal septum and bilateral peritubal area. Nasal biopsy was obtained from multiple sites including granulations.
Fig. 1.

Clinical photograph of the patient showing right lower motor neuron paralysis
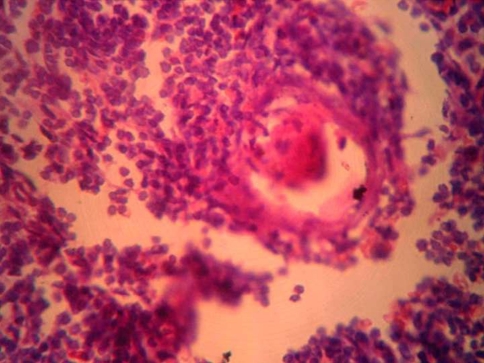
Serology was positive for granular cytoplasmic staining pattern antineutrophil cytoplasmic antibodies (c-ANCA), C Reactive Protein and Rheumatoid factor. Erythrocyte sedimentation rate was highly raised. Computerized tomography (CT) scan of chest revealed a soft tissue density lesion in left upper lobe. CT scan of temporal bones revealed soft tissue density in bilateral middle ear cavity and mastoid with erosion of bone overlying horizontal portion of right facial nerve. Renal function tests were normal. Nasal biopsy revealed (Fig. 2) granulomatous inflammation of the vascular vessel wall which confirmed the diagnosis of limited form of Wegener’s Granulomatosis without renal involvement.
Fig. 2.
Histopathological examination revealing granulomatous inflammation surrounding vascular vessel walls
Patient was initiated on medical treatment with Azathioprime 150 mg/day and oral prednisalone 20 mg t.i.d with a plan to gradually taper. Regression of granulations in nose and ear along with improvement of general condition was noted over the following weeks with the medical treatment. Cough subsided, cutaneous ulcers started to heal. Patient did not give consent for right mastoid exploration and facial nerve decompression as he was experiencing generalized physical weakness. In view of the rarity of occurrence of the disease and the rapidity of progression in our patient, our institutional review board has accepted our proposal to send the patient’s information for consideration towards scientific publication.
Discussion
Wegener’s Granulomatosis (WG) was first described by Heinz Klinger (1931) but later named after Frederich Wegener (1938), which is characterized histologically by appearance of necrotizing granulomas in upper and lower respiratory tracts, cutaneous involvement and focal glomerulonephritis. The main otolaryngological manifestations are blood stained nasal discharge, oral ulceration, sinusitis, secretory otitis media, conductive or sensorineural hearing loss and facial palsy [1]. Predominant otological presentation is rare [2].
Nasal biopsy is useful for confirming the diagnosis with a reported sensitivity of 53% [3]. C-ANCA is useful as a diagnostic and prognostic indicator [4].
Medical treatment is induction with cyclophosphamide and steroids [5]. Remission management is with Azathioprine.
Conclusion
The main purpose of reporting this case is to highlight the varied and uncommon and limited presentation of WG with initial otological complaints. More importantly lack of comprehensive evaluation of the patient as a whole, like not obtaining history of progressive weight loss and general debility, with emphasis only on otolaryngological aspect leads to undue delay in diagnosis and treatment of such potentially serious systemic disorders.
References
- 1.Llompart X, Aumaître O, Kémény JL, et al. Early otorhinolaryngological manifestations of Wegener’s granulomatosis. Analysis of 21 patients (in French) Ann Otolaryngol Chir Cervicofac. 2002;119(6):330–336. [PubMed] [Google Scholar]
- 2.Jordanl J, Siemińska A, Kuczkowski J, et al. Otologic signs and symptoms as first manifestations of Wegener’s granulomatosis with very severe clinical course–review of the literature and case report (in Polish) Otolaryngol Pol. 2004;58(3):521–527. [PubMed] [Google Scholar]
- 3.Del Buer EA, Flint A. Diagnostic usefulness of nasal biopsy in Wegener’s granulomatosis. Hum Pathol. 1991;22(2):107–110. doi: 10.1016/0046-8177(91)90030-S. [DOI] [PubMed] [Google Scholar]
- 4.Koldingsnes W, Nossent JC. Baseline features and initial treatment as predictors of remission and relapse in Wegener’s granulomatosis. J Rheumatol. 2003;30(1):80–88. [PubMed] [Google Scholar]
- 5.Erickson VR, Hwang PH. Wegener’s granulomatosis: current trends in diagnosis and management. Curr Opin Otolaryngol Head Neck Surg. 2007;15(3):170–176. doi: 10.1097/MOO.0b013e3281568b96. [DOI] [PubMed] [Google Scholar]