Abstract
At present, the only approved inhaled antipseudomonal antibiotics for chronic pulmonary infections in patients with cystic fibrosis (CF) are nebulized solutions. However, prolonged administration and cleaning times, high administration frequency, and cumbersome delivery technologies with nebulizers add to the high treatment burden in this patient population. PulmoSphere™ technology is an emulsion-based spray-drying process that enables the production of light porous particle, dry-powder formulations, which exhibit improved flow and dispersion from passive dry powder inhalers. This review explores the fundamental characteristics of PulmoSphere technology, focusing on the development of a dry powder formulation of tobramycin for the treatment of chronic pulmonary Pseudomonas aeruginosa (Pa) infection in CF patients. This dry powder formulation provides substantially improved intrapulmonary deposition efficiency, faster delivery, and more convenient administration over nebulized formulations. The availability of more efficient and convenient treatment options may improve treatment compliance, and thereby therapeutic outcomes in CF.
Key words: PulmoSphere™, dry powder inhaler, nebulization, cystic fibrosis, tobramycin, tobramycin inhalation powder (TIP™)
Introduction
Chronic pulmonary infection with Pseudomonas aeruginosa (Pa) is a significant cause of morbidity and mortality in patients with cystic fibrosis (CF).(1) Effective antibiotic therapy directed against this pathogen is an integral part of the daily treatment regimen for CF patients chronically infected with Pa.(2) Pa infection is primarily localized to the endobronchial space in CF. Therefore, aerosol delivery of antibiotics is an attractive option for treating these infections. Inhaled antibiotics deliver high doses directly to the site of infection, while minimizing systemic exposure and risk of toxicity.(2)
At present, the only approved inhaled antibiotic treatments are nebulizer solutions, specifically, tobramycin inhalation solution [TIS (TOBI®; Novartis AG, Switzerland; Bramitob®; Chiesi Farmaceutici S.p.A., Italy)], colistimethate sodium (Colomycin®; Forest Laboratories, Inc, UK; and Promixin® ; Profile Pharma, Ltd, UK; in a few European Countries only), and more recently, aztreonam inhalation solution [AZLI (Cayston®; Gilead Sciences, Inc., Forest City, CA, USA)]. Tobramycin and aztreonam inhalation solutions have demonstrated efficacy and safety in CF patients with chronic Pa infection.(3,4) TIS is recommended by the Cystic Fibrosis Foundation guidelines for treatment of chronic Pa infection in CF patients ≥6 years.(5) Despite that, less than 70% of qualified patients in the US CF Patient Registry were prescribed TIS in 2008.(6) Also, most patients who are prescribed TIS have far fewer prescription refills than necessary to maintain alternate month cycles.(7) A variety of reasons may exist for the disconnect between real-world usage of inhaled antibiotics and recommendations in the treatment guidelines.
Time burden is an important factor in chronic diseases like CF. These patients may be required to administer many daily chronic inhaled therapies, including bronchodilators, mucolytics, hypertonic saline, and inhaled antibiotics. These aerosol treatments, added to airway clearance maneuvers, take patients an average of almost 2 h to complete.(8) TIS is administered twice daily with the PARI-LC® PLUS or comparable jet nebulizer (with a suitable compressor) over a period of 15–20 min.(9) Aztreonam for inhalation solution is administered with an electronic vibrating mesh nebulizer (Altera®; Pari Innovative Manufacturers, Inc., Midlothian, VA, USA). The solution only takes 2–3 min to inhale, and is administered three times a day versus twice a day for TIS. Furthermore, both aztreonam inhalation solution and colistimethate must be reconstituted immediately before nebulization, increasing the handling time and delivery complexity for these antibiotics. All nebulizers require regular cleaning after each use to prevent bacterial contamination and to ensure that the performance of the device is not compromised. This is a time-consuming process, and many patients do not clean their nebulizer as directed.(10) In addition to the time burden, nebulizer/compressor combinations are noisy, bulky, and require a power source. Furthermore, tobramycin and aztreonam inhalation solutions must be stored in a refrigerator, decreasing convenience.
The ability to deliver therapeutic doses of antibiotics with a portable inhaler in a fraction of the time required for the entire process of nebulization would be a significant advance that may improve patient compliance and clinical outcomes.(9) The principal reason that nebulizers have been utilized for aerosol delivery of anti-infectives lies in the high lung doses required for effective treatment. For example, the lung dose for TIS is approximately 35 mg.(11) Recent developments in particle engineering, in particular the development of PulmoSphere™ technology, has enabled the delivery of a large amount of dry powder (up to 25 mg) to the lungs in a single actuation.(12)
Early development of dry powder antipseudomonal antibiotic formulations
Traditional formulation approaches for producing dry powders for inhalation have relied on “top-down” manufacturing methods, where large crystalline drug particles are milled (micronized) to produce fine crystals with a median diameter suitable for inhalation (i.e., 1–5 μm). The micronization process is analogous to throwing a crystal ball against a steel wall. The crystal shatters into millions of pieces, with a broad particle size distribution and limited control of particle morphology. Milling generally produces particles with flat interfaces with the potential for large areas of contact and strong interparticle cohesive forces. Moreover, milling processes often produce charged surfaces with amorphous character, leading to an increased tendency for particles to agglomerate. Owing to the strong interparticle cohesive forces, fine micronized drug particles are often blended with coarse lactose carrier particles to improve powder flow and fluidization.(13,14) Nonetheless, cohesive forces between the micronized drug and carrier particles remain strong, and lung delivery efficiencies of 10–30% of the nominal dose are typically observed.(12,15) The high percentage of carrier particles [typically about 65:1 weight for weight (w/w)],(13,14) and the moderate lung delivery efficiencies limit the maximum lung dose that can be delivered with standard micronized blends to just a few milligrams per inhalation.(12)
The limitations of micronized drug blends to deliver large doses of drug to the lungs was illustrated for aminoglycosides.(16,17) In these studies, 15–32 inhalations of micronized gentamicin were needed to deliver a therapeutic dose. Completing such a large number of inhalations is time consuming and not feasible in clinical practice. Despite this, patients preferred the dry powder inhaler (DPI) delivery system to either the nebulizer or intravenous administration in this single-dose study, providing evidence for the potential of dry powders to improve adherence.(16)
PulmoSphere technology
The evolution of ‘bottom-up’ processing methods (e.g., spray drying) where the drug substance is dissolved in a solvent and then precipitated to produce fine particles, affords greater control of particle properties, including particle size and distribution, morphology, porosity, density, and surface energy.(12) These factors are critical in controlling bulk powder properties such as powder flow and dispersibility.(12,14,18,19) The improved powder properties are achieved without the addition of carrier particles. Consequently, drug loadings as high as 90–95% w/w are possible.(12,20)
The decreased interparticle cohesive forces achieved with spray-dried powders, particularly those with highly porous surfaces, leads to improvements in lung delivery efficiencies, with up to 60% of the nominal dose delivered to the lungs.(18,19) The increases in drug loading and lung delivery enable more effective delivery of high doses of anti-infectives in fewer inhalations. The spray-dried powders discussed herein typically have interpatient variabilities in total lung deposition of 10–20%, versus 30–50% for micronized drug blends.(20,21) Delivery of porous particles is also largely independent of the patient's peak inspiratory flow rate, further reducing dosing variability.(18,19)
Formulation development
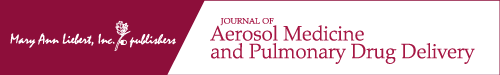
PulmoSphere particles are manufactured by an emulsion-based spray-drying process, designed to create porous particles with a sponge-like morphology.(15,22,23) The spray-drying process can be divided into four subprocesses: (1) feedstock preparation, (2) atomization, (3) drying, and (4) collection (Fig. 1). Submicron oil-in-water emulsion droplets are created by high-pressure homogenization of perfluorooctyl bromide (Perflubron) in water.(24) The dispersed oil droplets are stabilized against coarsening by a monolayer of a long-chain phospholipid [i.e., distearoylphosphatidylcholine (DSPC)]. Long-chain phosphatidylcholines, such as DSPC, are the principal components of endogenous pulmonary surfactant.(25) The active pharmaceutical ingredient (i.e., tobramycin) is incorporated in the emulsion by dissolving it in the continuous water phase. The resulting feedstock is then atomized with a twin fluid nozzle into a hot air stream. Each droplet contains a large number of dispersed emulsion droplets. During the initial stages of the drying process, the continuous water phase begins to evaporate leading to decreases in the diameter of the atomized droplet. Emulsion droplets are concentrated at the interface of the receding droplet, whereas the tobramycin readily diffuses to the center of the evaporating droplet. As the drying continues, a shell is formed at the surface of the atomized droplet; the shell is made up primarily of the excipients present in the emulsion droplets. After further drying, the perflubron evaporates, leaving behind pores in the particle. The volatile perflubron is collected in the spray-drying process. The particles are separated from the airstream with cyclone separators. Owing to the short drying time (in the order of milliseconds), tobramycin is present as an amorphous solid in the spray-dried particles. The role of the components used in the manufacturing process and in the final spray-dried particles is delineated in Table 1.
FIG. 1.
Schematic of the PulmoSphere™ manufacturing process. An emulsion-based feedstock is prepared by high-pressure homogenization. The emulsion consists of oil droplets (Perflubron) dispersed in a continuous water phase. The oil droplets are stabilized by a monolayer of a phospholipid (distearoylphosphatidylcholine). The tobramycin drug substance and calcium chloride excipient are dissolved in the continuous phase of the emulsion. The feedstock is atomized with a twin fluid nozzle into a spray dryer. As the atomized droplets containing dispersed emulsion droplets are dried, the slow diffusing emulsion droplets are concentrated at the droplet interface. As the drying continues, a shell is formed at the surface of the atomized droplet. Eventually, the Perflubron evaporates leaving behind pores in the particle shell. The resulting dry powder comprising porous particles is collected from the airstream with a cyclone separator.
Table 1.
Role of materials used in the manufacture of porous particles via the Pulmosphere™ process
| Component | Role in process | Role in drug product |
|---|---|---|
| Tobramycin | Drug substance | Drug substance |
| Distearoylphosphatidylcholine (DSPC) | Emulsifier (surfactant) | Principal excipient Hydrophobic shell-former |
| Calcium chloride (CaCl2) | Stabilize emulsion against flocculation and sedimentation | Secondary excipient Shell-former |
| Perflubron | Process aid (pore-forming agent) None: removed to residual levels |
|
| Water for irrigation | Process aid (solvent for water-soluble excipients and drug substance) None: removed to residual levels |
|
| Sulphuric acid | pH adjustment and salt formation | Counterion in salt form of drug substance |
PulmoSphere particles: physical characteristics
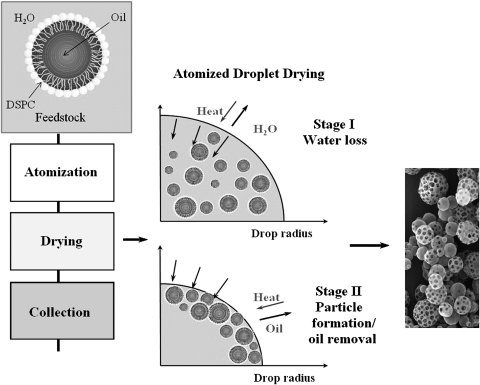
Scanning electron microscopic images of micronized drugs and spray-dried tobramycin inhalation powder (TIP™) particles are shown in Figure 2. Micronized drug substances (Fig. 2a) are typically characterized by smooth plate-like crystals, with a broad particle size distribution ranging from tens of nanometers to a few microns. The micronized drug is highly agglomerated with smaller crystals (less than 1 μm) adhering to larger crystals. The agglomerates are often tens of microns in size. Owing to their rectangular shape, the area of contact between the small crystals and the larger sized crystals is high. In contrast, spray-dried PulmoSphere particles (Fig. 2b and c) are spheroidal, with geometric sizes between 1 and 5 μm, and a more uniform distribution of sizes. The particles are also highly porous with a sponge-like morphology. The spheroidal shape and porous surface decrease the area of contact between particles, leading to less particle agglomeration. Moreover, despite the fact that phospholipid makes up just 14% of the bulk composition of the particles, approximately 90% of the surface is made up of DSPC. The enrichment of the DSPC at the surface is critical in lowering the surface energy of the spray-dried particles, further aiding in decreasing interparticle cohesive forces. Consequently, PulmoSphere particles readily flow and disperse from portable DPIs with little applied energy. In this regard, low inspiratory effort is needed to generate an aerosol of the PulmoSphere particles. Thus, younger patients (≥6 years old), and those with reduced pulmonary function can consistently create the inspiratory flow rate necessary to deliver a full dose via the T-326 Inhaler (see below for further information on this device).(9,26,27)
FIG. 2.
Scanning electron microscope images of: (a) typical micronized drug particles, (b) TIP particles, and (c) TIP particle (closeup).
The oropharynx is an effective filter; therefore, particle size is an extremely important consideration when creating novel inhaled therapies. Models of aerosol deposition show that particles with a diameter greater than 5 μm deposit in the oropharynx, whereas particles ranging from 1 to 5 μm deposit in the airways and alveoli.(28) PulmoSphere particles have median geometric diameters (as determined by laser diffraction) of 1.7–2.7 μm, and mass median aerodynamic diameter <4 μm.(29) This size range is ideal for targeting the powder aerosol to the site of the Pa infection in the airways.
Dry powder inhaler development
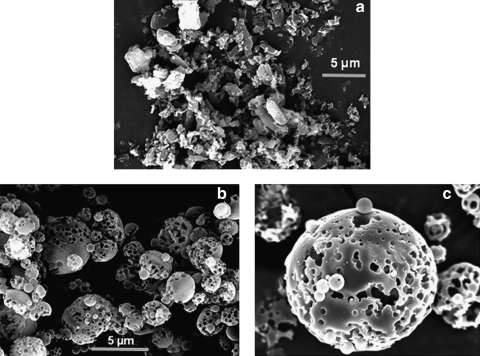
TIP is delivered via the breath-actuated T-326 Inhaler (Novartis Pharmaceuticals, San Carlos, CA, USA). The T-326 Inhaler is a portable, capsule-based DPI, which is mechanical and does not require an external power source or electronics (Fig. 3).
FIG. 3.
The portable breath-actuated T-326 Inhaler. A hypromellose capsule is loaded into the device by first removing the mouthpiece and inserting the capsule into the chamber. The mouthpiece is screwed back onto the body. The button is depressed to pierce the capsule, and the patient then inhales through the mouthpiece. The capsule rotates rapidly in the chamber causing powder to be emptied from the capsule.
The ability to achieve adequate inspiratory flow rates and inhaled volumes is paramount for effective and reproducible dose delivery.(26) As described earlier, PulmoSphere particles have favorable characteristics to be effectively dispersed by the inspiratory effort of CF patients. The T-326 Inhaler was designed to have a low airflow resistance [approximately 0.08 (cm H2O)½/LPM], to allow patients to generate high airflow rates, and in turn, attain reliable dose delivery.(29) The T-326 Inhaler resistance is intermediate between the Diskus® [R = 0.07 (cm H2O)½/LPM] and Turbohaler® [R = 0.11 (cm H2O)½/LPM] devices, and significantly less than the Handihaler® [R = 0.18 (cm H2O)½/LPM].(30,31) A study was conducted to assess the breathing profiles of 96 CF patients of varying age and disease severity when asked to breathe forcefully through resistances that span that of the T-326 Inhaler.(26,27) The results are presented in Table 2. The young adults (n = 24) and adults (n = 39) had mean peak flows of 79.3 L/min (SD 15.0) and 81.1 L/min (SD 14.4), respectively, and inhaled volumes of 1.63 L (SD 0.60) and 2.06 L (SD 0.68), whereas the 6–10-year-olds (n = 33) reached 68.7 L/min (SD 13.1) and 1.2 L (SD 0.39). In turn, the breathing profiles for various patient subgroups (pediatric, young adult, and adult) were simulated in in vitro studies to assess powder emptying from the capsule. The fill mass in the capsule was selected to ensure that most patients (including pediatric patients as young as 6 years old) can effectively empty the contents of the capsule in a single actuation.(27) Indeed, provided the patient has an inhaled volume >1.0 L, they will be able to empty more than 90% of the capsule contents, although the instructions for use call for a second inhalation to ensure that all patients are able to empty the capsule. Confirmation of dose delivery is easily accomplished by inspecting the capsule postinhalation. If significant powder remains, the capsule may be reinserted and an additional inhalation maneuver performed.(29)
Table 2.
| Age group | n | Age (year) | FEV1 (% of predicted) | Inhaled volume (L) | PIF (LPM) | Inspiratory time (sec) | |
|---|---|---|---|---|---|---|---|
| 6–10 | 33 | Mean | 8.4 | 92.0 | 1.20 | 68.7 | 1.65 |
| (pediatric) | SD | 1.3 | 15.5 | 0.39 | 13.1 | 0.43 | |
| 11–18 | 24 | Mean | 15.0 | 68.6 | 1.63 | 79.3 | 1.82 |
| (young adult) | SD | 2.4 | 29.6 | 0.60 | 15.0 | 0.49 | |
| >18 | 39 | Mean | 32.9 | 54.1 | 2.06 | 81.1 | 2.39 |
| (adult) | SD | 9.3 | 27.1 | 0.68 | 14.4 | 0.72 |
The deposition fraction of TIP via the T-326 Inhaler is approximately three times higher than that of TIS via the PARI-LC® Plus, as determined by gamma scintigraphic images in healthy volunteers.(20,32) Interpatient variability for TIP was lower than TIS (17 vs. 24–40%) (Table 3). Reduced interpatient variability is also observed for tobramycin concentrations in serum and sputum in CF patients.(9) Despite the fact that the breathing pattern for liquid delivery (tidal breathing), and dry powder delivery (forceful inhalation) differ significantly, the relative distribution of tobramycin within the central, intermediate, and peripheral airways is similar for both formulations, with a trend for greater deposition in the peripheral versus central airways.(20) The ratio of peripheral to central deposition (P/C), for TIP was 1.6 ± 0.4 versus 1.5 ± 0.4 for TIS.(20) Based on 24-h clearance studies, these P/C ratios correspond to deposition in nonconducting peripheral airways of 66 and 63%, respectively.(33) Serum pharmacokinetic profiles for TIS and TIP were also comparable, indicating rapid dissolution of the amorphous dry powder into epithelial lining fluid, and comparable lung clearance for the two formulations.(20) In CF patients, the distribution of tobramycin in the lungs will be more affected by airway geometry and disease than by aerosol characteristics.(34) It is expected that increases in airway disease will result in comparable total lung deposition, with increased central deposition relative to the results presented above for healthy volunteers. The deposition pattern will also be dependent on the anatomy of the oropharynx and the breathing pattern of the patient.(28) With that said, PulmoSphere powders fluidize and disperse effectively even at the extremes of the breathing patterns observed in patient breathing studies (Table 2). For example, a study examining aerosol performance showed that the delivered dose and aerodynamic particle size distribution did not differ significantly with variations in temperature (ranging from 10 to 40°C), relative humidity (ranging from 10 to 65%), and flow rate (ranging from 40 to 85 L/min).(29) A flow rate of 40 L/min represents a flow rate more than 2 standard deviations below the mean peak inspiratory flow rates measured for pediatric patients in the breathing study (Table 2). Indeed, similar lung exposures were observed for pediatric and adult CF patients based on pharmacokinetic modeling of data from TIP Phase III clinical development.(35–37)
Table 3.
Lung deposition for TIP and TIS in healthy volunteers as determined by gamma scintigraphy
| TIP (T-326 Inhaler)(20) | TIS (PARI-LC® Plus)(32) | |
|---|---|---|
| Nominal dose of tobramycin | 80 mg | 300 mg |
| Deposition | ||
| Lung | 34.2% (27 mg) | 9.2% (27 mg) |
| Oropharynx | 43.6% (35 mg) | 16.0% (48 mg) |
| Device | 21.7% (17 mg) | 43.5% (131 mg) |
| Exhaled | 0.2% (0 mg) | 28.3% (85 mg) |
| Total lung deposition | 27.4 mg | 27.3 mg |
| Intersubject variability | 17% | 24% |
The TIP/T-326 Inhaler combination was designed to shorten administration time versus the current nebulized formulation of tobramycin, TIS. Administration times for TIP is under 6 min, which is about 14 min faster than TIS.(9,35) Thus, TIP reduces the time burden by 28 min per day, not including the time required to set up and clean the TIS nebulizer and compressor. As mentioned earlier, most CF patients do not clean their nebulizer as directed, and the majority of nebulizers have been found to be contaminated.(38) The T-326 Inhaler requires minimal cleaning, and no disinfection, and can be disposed of after several uses. Due to the dry nature of the TIP formulation, the T-326 Inhaler has the added convenience that it only needs to be wiped with a dry cloth after each use as it does not come into contact with aqueous solutions, and therefore growth of bacteria is not promoted. It is possible that improved ease of use, reduced administration time, and minimal cleaning requirements may translate into improved patient adherence and therefore potentially improved therapeutic outcomes.
Powder filling and packaging
TIP is filled into hypromellose capsules. Hypromellose was chosen over gelatine due to its decreased tendency to fracture at the low relative humidity storage conditions required to maintain physical stability of the amorphous solid. In order to protect the amorphous TIP from the adverse effects of moisture, the bulk capsules are packaged in coated aluminium blisters. The T-326 Inhaler is also stored in a case between use to prevent moisture uptake by residual powder in the device. Unlike tobramycin and aztreonam inhalation solutions, TIP is kept at room temperature.
The size of the capsule and the achievable powder fill mass for TIP were determined based on the ability of the average pediatric patient (age 6–10 years) to empty the contents of the capsule in a single inhalation.(21)
Clinical development of tobramycin inhalation powder
The early clinical development of TIP included a dose-escalation study to determine the dose of TIP that is pharmacokinetically equivalent, in terms of tobramycin serum and lung exposures, to the approved dose of TIS (TOBI®, 300 mg tobramycin/5 mL preservative-free solution). The dose of TIP that showed comparable systemic tobramycin exposure to 300 mg TIS was four capsules containing a total dose 112 mg tobramycin.(9) Importantly, the serum tobramycin levels were low (approximately 1 μg/mL) relative to systemic levels associated with producing toxicity with intravenous tobramycin (10–12 μg/mL).(39) Based on these data a dose of TIP 112 mg twice daily was chosen for evaluation in Phase III studies.
Two Phase III studies have been performed in patients with CF aged ≥ 6 years. The first study, a randomized, double-blind, placebo-controlled trial in relatively TIS- naïve CF patients, assessed the efficacy and safety of TIP (total dose 112 mg tobramycin) twice daily (28 days on-treatment and 28 days off-treatment) via the T-326 Inhaler. TIP improved FEV1 % predicted versus placebo at day 28 (least squares mean difference = 13.3, p = 0.0016). Importantly, the improvement over placebo was maintained at the end of the first complete cycle (day 56). TIP also reduced sputum Pa density, respiratory-related hospitalizations, and additional antipseudomonal use versus placebo.(36)
The results of the placebo-controlled trial were confirmed in a recently completed Phase III active-comparator trial, which showed that the efficacy of TIP is comparable to the approved dose of TIS.(35) In the same study, a modified Treatment Satisfaction Questionnaire for Medication (TSQM) demonstrated that patients rate TIP as more convenient and satisfying than TIS; mean patient assessments were significantly greater for effectiveness (p < 0.0001), convenience (p < 0.0001), and global satisfaction (p = 0.0018) in the TIP versus TIS treatment group. The favorable results of the modified TSQM is related in part to the ease of use and shorter administration time for TIP (average: 5.6 vs. 19.7 minutes, respectively).(35) TIP was generally well tolerated in both Phase III studies.
Owing to the large amount of powder being delivered to the lungs, there were concerns as to whether TIP would be tolerated in the CF patients.(12) These concerns were largely unfounded, as TIP was well tolerated by most patients in both Phase III studies.(35,36) The safety profile of TIP is similar to that of TIS, with the exception of cough, dysphonia, and dysgeusia, which are higher in patients treated with TIP.(35) Although the incidence of these adverse events was higher for TIP, there was no difference in the treatment satisfaction score for side effects between groups.(35) Importantly, cough does not appear to be related to bronchospasm;(36) rather, a postinhalation reflex to the high powder load may underlie the higher reported cough rate in TIP- versus TIS-treated patients. We speculate that there was a different reporting pattern of cough for TIP versus TIS, as most patients and investigators are experienced with the nebulized administration of tobramycin. Overall, the results of clinical trials to date indicate that TIP is a safe and effective treatment for chronic Pa lung infection in CF patients aged ≥6 years.
Additional applications for pulmosphere technology
PulmoSphere technology was originally developed to treat ventilator associated pneumonia in intubated patients undergoing partial liquid ventilation.(40) The porous particles were designed to effectively stabilize drug suspensions in the fluorinated media used in liquid ventilation. The technology was later applied to the stabilization of suspensions in hydrofluoroalkane propellants,(41) and eventually to dry powder delivery.(18,20,42,43)
PulmoSphere technology is a true “platform,” having demonstrated utility across multiple classes of therapeutics and delivery systems. To date, PulmoSphere formulations have been evaluated in 18 clinical trials. There are currently six drugs under active Investigational New Drug applications in Phase II clinical development or later. These include three anti-infectives: tobramycin(9,20,35,36) and ciprofloxacin(44) to treat chronic Pa infections in CF patients, and amphotericin B to treat invasive pulmonary aspergillosis in immunocompromised patients.(45) Other patient populations with Pa airway infections that may benefit from antimicrobial DPI formulations include non-CF bronchiectasis, chronic bronchitis, and chronic obstructive pulmonary disease (COPD). PulmoSphere formulations (both DPI and metered-dose inhaler) of long-acting muscarinic antagonists, long-acting beta-agonists, and inhaled corticosteroids are in development for treating bronchoconstriction and inflammation in patients with asthma/COPD. Dry powder PulmoSphere formulations are expected to improve lung targeting, and dose consistency for asthma/COPD therapeutics.(18,19) This may ultimately enable improvements in treatment compliance, as poor inhaler technique is a major driver for inconsistent dosing.(18,20)
Beyond the products currently in development, PulmoSphere formulations have shown promise in the delivery of biologicals including peptides, proteins, antibodies,(46) and mucosal vaccines.(47) Additionally, dispersion of porous PulmoSphere particles in hydrofluoroalkane propellants increases delivered dose and improves dose content uniformity versus conventional suspension formulations, which may improve lung delivery efficiency for suspension-based pMDI formulations.(42,43)
Discussion
Aerosol antibiotics for the treatment of Pa form an integral part of the treatment regimen in CF patients with chronic airways infection, although they are currently associated with a high time burden and other inconveniences. Dry powder inhalation with a portable DPI is an attractive alternative to nebulization; and using PulmoSphere technology delivers the high payload of drug to the lungs needed for effective treatment. The PulmoSphere formulation of TIP delivered with the T-326 inhaler has demonstrated safety and efficacy in clinical trials, and has numerous advantages over nebulized antibiotics, including faster delivery, ease of use, portability, reduced need for cleaning, and room temperature storage. It is anticipated that the reduced treatment burden and improved dose consistency afforded by TIP may translate into improved treatment compliance and better therapeutic outcomes for CF patients with Pa airway infections.
Acknowledgments
The authors take full responsibility for the content of the paper. Writing and editorial assistance (funded by Novartis Pharma AG) was provided by Melanie Stephens, ACUMED®, UK.
Author Disclosure Statement
Dr. Geller has relationships with Aires, Aradigm, Bayer, CSL Behring, Discovery Labs, Genentech, Gilead Sciences, Inc., MAP Pharmaceuticals, Mpex, NanoBio, Novartis Pharmaceuticals, Pharmaxis, Philips Respironics, Teva, Talecris, and Vertex. Silvia Heuerding and Jeffry Weers are employees of Novartis Pharmaceuticals.
References
- 1.Emerson J. Rosenfeld M. McNamara S. Ramsey B. Gibson RL. Pseudomonas aeruginosa and other predictors of mortality and morbidity in young children with cystic fibrosis. Pediatr Pulmonol. 2002;34:91–100. doi: 10.1002/ppul.10127. [DOI] [PubMed] [Google Scholar]
- 2.Geller DE. Aerosol antibiotics in cystic fibrosis. Respir Care. 2009;54:658–670. doi: 10.4187/aarc0537. [DOI] [PubMed] [Google Scholar]
- 3.Ramsey BW. Pepe MS. Quan JM. Otto KL. Montgomery AB. Williams-Warren J. VasilJev KM. Borowitz D. Bowman CM. Marshall BC. Marshall S. Smith AL. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. Cystic Fibrosis Inhaled Tobramycin Study Group. N Engl J Med. 1999;340:23–30. doi: 10.1056/NEJM199901073400104. [DOI] [PubMed] [Google Scholar]
- 4.Retsch-Bogart GZ. Quittner AL. Gibson RL. Oermann CM. McCoy KS. Montgomery AB. Cooper PJ. Efficacy and safety of inhaled aztreonam lysine for airway Pseudomonas in cystic fibrosis. Chest. 2009;135:1223–1232. doi: 10.1378/chest.08-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flume PA. O'Sullivan BP. Robinson KA. Goss CH. Rosenblatt RL. Kuhn RJ. Marshall BC. Cystic fibrosis pulmonary guidelines: chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2007;176:957–969. doi: 10.1164/rccm.200705-664OC. [DOI] [PubMed] [Google Scholar]
- 6.Cystic Fibrosis Foundation Patient Registry. Annual Data Report to the Center Directors. Bethesda, MD: Cystic Fibrosis Foundation Patient Registry; 2008. [Google Scholar]
- 7.Briesacher B. Quittner A. Saiman L. Fouayzi H. Sacco P. Quittel L. Adherence to tobramycin inhaled solution and health care utilization. Am J Respir Crit Care Med. 2009;179 [Abstract A1183]. [Google Scholar]
- 8.Sawicki GS. Sellers DE. Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self-management. J Cyst Fibros. 2009;8:91–96. doi: 10.1016/j.jcf.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geller DE. Konstan MW. Smith J. Noonberg SB. Conrad C. Novel tobramycin inhalation powder in cystic fibrosis subjects: pharmacokinetics and safety. Pediatr Pulmonol. 2007;42:307–313. doi: 10.1002/ppul.20594. [DOI] [PubMed] [Google Scholar]
- 10.Saiman L. Garber E. Infection control in cystic fibrosis: barriers to implementation and ideas for improvement. Curr Opin Pulmon Med. 2009;15:626–631. doi: 10.1097/MCP.0b013e328330d974. [DOI] [PubMed] [Google Scholar]
- 11.Geller DE. Pitlick WH. Nardella PA. Tracewell WG. Ramsey BW. Pharmacokinetics and bioavailability of aerosolized tobramycin in cystic fibrosis. Chest. 2002;122:219–226. doi: 10.1378/chest.122.1.219. [DOI] [PubMed] [Google Scholar]
- 12.Weers J. Clark A. Challoner P. High dose inhaled powder delivery: challenges and techniques. In: Dalby RN, editor; Byron PR, editor; Peart J, editor; Suman JD, editor; Farr SJ, editor. Respiratory Drug Delivery IX. Amy Davis Biggs; River Grove, IL: 2004. pp. 281–288. [Google Scholar]
- 13.Zeng XM. Tee SK. Martin GP. Marriott C. Effects of mixing procedure and particle size distribution of carrier particles on the deposition of salbutamol sulphate from dry powder inhaler formulations. Proceedings of Drug Delivery to the Lungs VII; London. 1996. pp. 40–43. [Google Scholar]
- 14.Zeng XM. Martin GP. Marriott C. Particulate Interactions in Dry Powder Formulations for Inhalation. Taylor & Francis; London: 2001. [Google Scholar]
- 15.Clark AR. Borgström L. In vitro testing of pharmaceutical aerosols and predicting lung deposition from in vitro measurements. In: Bisgard H, editor; O'Callaghan C, editor; Smaldone GC, editor. Drug Delivery to the Lung. Marcel Dekker: New York; Chapter 4; 2002. pp. 105–142. [Google Scholar]
- 16.Crowther-Labiris NR. Holbrook AM. Chrystyn H. MacLeod SM. Newhouse MT. Dry powder versus intravenous and nebulized gentamycin in cystic fibrosis and bronchiectasis: a pilot study. Am J Respir Crit Care Med. 1999;160:1711–1716. doi: 10.1164/ajrccm.160.5.9810080. [DOI] [PubMed] [Google Scholar]
- 17.Goldman JM. Bayston SM. O'Connor S. Meigh RE. Inhaled micronised gentamycin powder: a new delivery system. Thorax. 1990;5:939–940. doi: 10.1136/thx.45.12.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duddu SP. Sisk SA. Walter YH. Tarara TE. Trimble KR. Clark AR. Eldon MA. Elton RC. Pickford M. Hirst PH. Newman SP. Weers JG. Improved lung delivery from a passive dry powder inhaler using an engineered PulmoSphere powder. Pharm Res. 2002;19:689–695. doi: 10.1023/a:1015322616613. [DOI] [PubMed] [Google Scholar]
- 19.Weers JG. Bell J. Chan H-K. Cipolla D. Dunbar C. Hickey AJ. Smith IJ. Pulmonary formulations: what remains to be done? J Aerosol Med Pulm Drug Deliv. 2010;(Suppl 2):S5–S23. doi: 10.1089/jamp.2010.0838. [DOI] [PubMed] [Google Scholar]
- 20.Newhouse MT. Hirst PH. Duddu SP. Walter YH. Tarara TE. Clark AR. Weers JG. Inhalation of a dry powder tobramycin pulmosphere formulation in healthy volunteers. Chest. 2003;124:360–366. doi: 10.1378/chest.124.1.360. [DOI] [PubMed] [Google Scholar]
- 21.Borgström L. Olsson B. Thorsson L. Degree of throat deposition can explain the variability in lung deposition of inhaled drugs. J Aerosol Med. 2006;19:473–483. doi: 10.1089/jam.2006.19.473. [DOI] [PubMed] [Google Scholar]
- 22.Weers JG. Tarara TE. Clark AR. Design of fine particles for pulmonary drug delivery. Expert Opin Drug Del. 2007;4:297–313. doi: 10.1517/17425247.4.3.297. [DOI] [PubMed] [Google Scholar]
- 23.Dellamary LA. Tarara TE. Smith DJ. Woelk CH. Adractas A. Costello M. Gill H. Weers JG. Hollow porous particles in metered dose inhalers. Pharm Res. 2000;17:168–174. doi: 10.1023/a:1007513213292. [DOI] [PubMed] [Google Scholar]
- 24.Krafft MP. Riess JG. Weers JG. The design and engineering of oxygen-delivering fluorocarbon emulsions. In: Benita S, editor. Submicron Emulsions in Drug Targeting and Delivery. Harwood Academic Publishers; Amsterdam: 1998. pp. 235–333. [Google Scholar]
- 25.Notter RH. Lung surfactants: basic science and clinical applications. In: Lenfant C, editor. Lung Biology in Health and Disease. Marcel Dekker; New York: 2000. [Google Scholar]
- 26.Tiddens HA. Geller DE. Challoner P. Effect of dry powder inhaler resistance on the the inspiratory flows and volumes of patients with cystic fibrosis of six years and older. J Aerosol Med. 2006;19:456–465. doi: 10.1089/jam.2006.19.456. [DOI] [PubMed] [Google Scholar]
- 27.Standaert TA. Speirs RJ. Rao N. Ung K. Tep V. Lin T. Rourke AM. Challoner P. Young cystic fibrosis patients can effectively use a novel high-payload capsule-based dry powder inhaler with tobramycin powder for inhalation (TPI) Pediatr Pulmonol. 2004;38(Suppl 27):284. [Google Scholar]
- 28.Geller DE. The science of aerosol delivery in cystic fibrosis. Pediatr Pulmonol. 2008;43:S5–S17. [Google Scholar]
- 29.Haynes A. Nakamura J. Heng C. Heuerding S. Thompson G. Malcolmson R. Aerosol performance of tobramycin inhalation powder. In: Dalby RN, editor; Byron PR, editor; Peart J, editor; Suman JD, editor; Farr SJ, editor; Young PM, editor. Respiratory Drug Delivery 2010. Davis Healthcare International Publication; River Grove, IL: 2010. pp. 701–706. [Google Scholar]
- 30.Chrystyn H. Effects of device design on patient compliance: comparing the same drug in different devices. In: Dalby RN, editor; Byron PR, editor; Peart J, editor; Suman JD, editor; Young PM, editor. Respiratory Drug Delivery Europe 2009. Davis Healthcare International Publication; River Grove, IL: 2009. pp. 105–116. [Google Scholar]
- 31.Chodosh S. Flanders JS. Kesten S. Serby CW. Hochrainer D. Witek TJ. Effective delivery of particles with the Handihaler dry powder inhalation system over a range of chronic obstructive pulmonary disease severity. J Aerosol Med. 2001;14:309–315. doi: 10.1089/089426801316970268. [DOI] [PubMed] [Google Scholar]
- 32.Challoner PB. Flora MG. Hirst PH. Klimowicz MA. Newman SP. Schaeffler BA. Speirs RJ. Wallis SJ. Gamma scintigraphy lung deposition comparison of TOBI in the Pari LC Plus nebulizer and the Aerodose inhaler. Am J Respir Crit Care Med. 2001;163:A83. [Google Scholar]
- 33.Newman SP. Hirst PH. Pitcairn GR. Clark AR. Understanding regional lung deposition in gamma scintigraphy. In: Dalby RN, editor; Byron PR, editor; Farr SJ, editor. Respiratory Drug Delivery VI. Interpharm Press; Buffalo Grove, IL: 1998. pp. 9–16. [Google Scholar]
- 34.Clark AR. Beyond the throat: preferred methods of assessing regional distribution in the lung. In: Dalby RN, editor; Byron PR, editor; Peart J, editor; Suman JD, editor; Farr SJ, editor; Young PM, editor. Respiratory Drug Delivery 2010. Davis Healthcare International Publishing; River Grove, IL: 2010. pp. 235–244. [Google Scholar]
- 35.Konstan MW. Flume PA. Kappler M. Chiron R. Higgins M. Brockhaus F. Zhang J. Angyalosi G. He E. Geller DE. Safety, efficacy and convenience of tobramycin inhalation powder in cystic fibrosis patients: the EAGER trial. J Cystic Fibros. 2010 doi: 10.1016/j.jcf.2010.10.003. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Konstan MW. Geller DE. Minić P. Brockhaus F. Zhang J. Angyalosi G. Tobramycin inhalation powder for Pseudomonas aeruginosa infection in cystic fibrosis: the EVOLVE trial. Pediatr Pulmonol. 2010 doi: 10.1002/ppul.21356. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu K. Carter A. Geller DE. Sahasranaman S. Population pharmacokinetics of tobramycin inhalation powder in cystic fibrosis patients. Pediatr Pulmonol. 2010;(Suppl 33):306–307. [Google Scholar]
- 38.Lester MK. Flume PA. Gray SL. Anderson D. Bowman CM. Nebulizer use and maintenance by cystic fibrosis patients: a survey study. Respir Care. 2004;49:1504–1508. [PubMed] [Google Scholar]
- 39.Sweetman SC. Martindale: The Complete Drug Reference. London: Pharmaceutical Press; [Jun 29;2009 ]. (online) [Google Scholar]
- 40.Dickson EW. Heard SO. Tarara TE. Weers JG. Brueggemann BA. Doern GV. Liquid ventilation with perflubron in the treatment of rats with pneumococcal pneumonia. Crit Care Med. 2002;30:393–395. doi: 10.1097/00003246-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 41.Tarara TE. Hartman M. Gill H. Kennedy A. Weers JG. Characterization of suspension-based metered dose inhaler formulations comprised of spray-dried budesonide crystals dispersed in HFA-134a. Pharm Res. 2004;21:1607–1614. doi: 10.1023/b:pham.0000041455.13980.f1. [DOI] [PubMed] [Google Scholar]
- 42.Weers J. Dispersible powders for inhalation applications. Innovat Pharm Tech. 2000;1:114–116. [Google Scholar]
- 43.Weers J. Tarara T. Pulmonary delivery of a fluoroquinolone. 2009 WO/2009/140587. [Google Scholar]
- 44.Lee JD. Kugler AR. Samford LK. Gerety RJ. Eldon MA. Amphotericin B Inhalation Powder (ABIP) is well-tolerated with low systemic amphotericin B exposure in healthy subjects (abstract P118). Program and Abstracts of the 2nd Meeting of Advances Against Aspergillosis; Athens, Greece. 2006. pp. 214–215. [Google Scholar]
- 45.Dellamary L. Smith DJ. Bloom A. Bot S. Guo GR. Deshmuk H. Costello M. Bot A. Rational design of solid aerosols for immunoglobulin delivery by modulation of aerodynamic and release characteristics. J Control Rel. 2004;95:489–500. doi: 10.1016/j.jconrel.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 46.Wang L. Bot S. Smith D. Guo GR. Phillips B. Dellamary L. Bot A. Basic immunological properties of spray-dried lipid microparticles developed for nasal and systemic administration of vaccines. STP Pharma Sci. 2002;12:53–61. [Google Scholar]