Abstract
Objective The present study prospectively examined the development of child PTSD symptoms (PTSS) and the impact of caregiver PTSS on child PTSS following injury. Methods One hundred and eighteen ED patients and their caregivers were interviewed in-hospital and 2- and 6-weeks posttrauma. Structural equation modeling and hierarchical linear regressions examined the development of PTSS. Results A model combining child and caregiver 2-week PTSS into one latent family PTSS variable provided the best fit to the data. Child in-hospital avoidance symptoms predicted higher levels of 2-week family PTSS. Two-week family PTSS predicted child 6-week PTSS. Post hoc analyses revealed an interaction between in-hospital caregiver avoidance symptoms and child reexperiencing symptoms in predicting 6-week child PTSS. Conclusions Results highlight the dynamic development of child PTSS. Different symptom clusters may be related to higher PTSS at differing times posttrauma and may inform the development of time-sensitive methods of assessment and intervention for injury victims.
Keywords: children, pediatric injury, PTSD
Each year one in four children receives medical care for an injury, resulting in millions of emergency department (ED) visits and hospitalizations (Center for Disease Control and Prevention, 2010; National Safe Kids Campaign, 2004). Traumatically injured children report high rates of behavioral and emotional dysfunction following relatively minor injuries (Basson et al., 1991), underscoring the importance of examining pediatric medical traumatic stress (Kazak et al., 2006; National Child Traumatic Stress Network, 2010). Reported rates of posttraumatic stress disorder (PTSD) in children and their caregivers due to pediatric injury range from 10% to 30% (Kahana, Feeny, Youngstrom, & Drotar, 2006; Kenardy, Spence, & Macleod, 2006; Winston, Kassam-Adams, Garcia-Espana, Ittenbach, & Cnaan, 2003). Many more of these children experience subthreshold levels of PTSD (DeVries et al., 1999; Kassam-Adams & Winston, 2004; Levi, Drotar, Yeates, & Taylor, 1999). Patients with subthreshold PTSD often endorse similar levels of impairment as those meeting full PTSD criteria (Stein, Walker, Hazen, & Forde, 1997). Further, examining continuous PTSD symptoms (PTSS) has proven to be more broadly applicable to patients and families than psychiatric diagnoses (Kazak et al., 2006).
Researchers have conceptualized models to help guide the identification of at-risk children and inform the design of interventions associated with pediatric medical traumatic stress (Kazak et al., 2006; Le Brocque, Hendricks, & Kenardy, 2010; Winston, Kassam-Adams, Garcia-Espana, Ittenbach, & Cnaan, 2003). However, these models differ as to how child PTSS develop over time and as to whether the impact of acute caregiver PTSS is considered. The present study prospectively examined the development of child PTSS and the impact of caregiver PTSS on the development of acute child PTSS.
Different theoretical models propose distinct and oftentimes contradictory patterns of symptom development following a traumatic event. For instance, in adult trauma victims, it has been hypothesized that initial hyperarousal symptoms can lead to the development of “overconsolidated” memories (Pitman, Orr, Lowenhagen, Macklin, & Altman, 1991) or could interfere with the emotional processing of the event, leading to the development of other PTSS (Ehlers & Clark, 2000). Other models focusing on acute responses to trauma have focused on intrusive posttraumatic cognitions (Best, Streisand, Catania, & Kazak, 2001; Kazak, Alderfer, Rourke, Simms, Streisand, & Grossman, 2004; Keppel-Benson, Ollendick, & Benson, 2002; Scheeringa & Zeanah, 1995). Following a trauma, children can experience emotionally upsetting memories and intrusive thoughts that can be elicited by trauma reminders and increase their distress (Meiser-Stedman, 2002). Activation of these intrusive memories may result in elevated levels of arousal, cognitive distortions, and altered behaviors (Meisser-Stedman, 2002), leading victims to avoid traumatic thoughts, images, and cues. As such, one may experience an oscillation between intrusive and avoidant states. Avoidance symptoms may then impair one’s emotional processing of traumatic memories, thereby leading to an exacerbation of PTSS (Meiser-Stedman, 2002).
In sum, research suggests time-dependent processes through which PTSS may develop. Theoretical and empirical evidence implicates the importance of early hyperarousal symptoms in predicting victims who are most likely to develop PTSS. However, in the subsequent days and weeks posttrauma, evidence highlights the role of reexperiencing and avoidance symptoms in leading to persistent PTSS. Although results support this process in adults, there is limited research concerning the course of PTSS development in children (Bryant, Salmon, Sinclair, & Davidson, 2007; Le Brocque Hendricks, & Kenardy 2010). Furthermore, child posttraumatic responses are likely influenced by their parents’ responses (e.g., Barakat et al., 1997; Keppel-Benson et al., 2002; Ostrowski, Christopher, & Delahanty, 2007); therefore, it is crucial for models of childhood PTSS to take a more family systems perspective.
Traumatic medical events impact children entrenched within families (Kazak et al., 2006). Parents are often traumatized by their child’s injury either through direct exposure to the child’s trauma, having to cope with the child’s distress, or because of their own feelings of guilt and hopelessness (Landolt, Vollrath, Ribi, Gnehm, & Sennhauser, 2003). Elevated caregiver distress may result in a caregiver being less available to the child during the early posttraumatic period. Furthermore, parent PTSS due to a child’s trauma were more strongly related to child PTSS than general parental distress (Nugent, Ostrowski, Christopher, & Delahanty, 2007), suggesting specific risk afforded by parent PTSS. While the majority of studies have examined the impact of overall parental PTSS on child posttraumatic adjustment, some have found that parental avoidance symptoms (e.g., not talking about the child’s trauma or avoidance of trauma-related cues and/or activities) may have the greatest negative impact on the child’s adjustment (Ostrowski, Christopher, & Delahanty, 2007). Caregiver avoidance may not allow a child to confront and resolve his/her own anxieties, which may increase sensitivity to future traumatic events and maintenance of psychological symptoms (Best, Streisand, Catania, & Kazak, 2001; Smith, Perrin, Yule, & Rabe-Hesketh, 2001).
Given the interrelationships between parent and child PTSS, and recognizing that these relationships may differ over time, the present study prospectively examined the dynamic interplay between caregiver and child responses immediately posttrauma and during the acute phase of recovery. Prospective studies assessing traumatic responses in both the child and caregiver may aid in the development of effective screening methods to identify children at greatest risk for PTSS, and may inform symptom-specific interventions to prevent/buffer the development of PTSS (Le Brocque, Hendricks, & Kenardy, 2010). It was hypothesized that child in-hospital symptoms of hyperarousal would have the greatest predictive value with respect to 2- and 6-week overall child PTSS. In addition, higher caregiver in-hospital and 2-week PTSS were hypothesized to predict higher levels of subsequent child PTSS and significantly interact with child in-hospital hyperarousal symptoms in predicting PTSS. We also examined the impact of caregiver avoidance symptoms on child 6-week PTSS, but due to the relatively small sample size, these analyses were considered exploratory.
Method
Participants
Participants were children aged 8–18 years who visited a Midwestern Children’s Hospital ED for nonabuse-related injuries and their primary caregivers. All participants were released from the ED within 8 hr (mean: 3.46 hr; range 1–8 hr). Patients with a chronic mental illness, evidence of pervasive developmental disorders or mental retardation were excluded.
Of the 120 families approached and screened, 118 agreed to participate (98% acceptance rate). Eighty percent (n = 94) of the original sample was retained at the 2-week follow-up and 84% (n = 99) of the original sample was retained for the 6-week time point. Reasons for dropout included inability to contact participants (n = 15) and disinterest in continuing with the study (n = 9). No differences were found in terms of demographics and PTSS at any time point between children and caregivers who did and did not complete the follow-ups (all p’s > .10). Additional demographic data are presented in Table I.
Table I.
Demographics and Descriptive Information
| Total sample | Boys | Girls | |
|---|---|---|---|
| Caucasian (n) | 92 | 64 | 28 |
| African American (n) | 26 | 8 | 18 |
| Age [M (SD); range] | 12.17 (3.03); 8–18 | 11.66 (2.94); 8–17 | 12.77 (2.93); 8–18 |
| Injury severity score [M (SD); range] | 7.36 (5.05); 1–22 | 8.24 (5.71); 1–22 | 5.90 (3.34); 1–16 |
| Types of injury (n) | |||
| Motor vehicle accidents (MVA) | 60 | 32 | 28 |
| Sports injury | 29 | 19 | 10 |
| Falls | 19 | 8 | 19 |
| Physical assault | 12 | 7 | 5 |
Measures
Demographics
Caregivers answered several questions concerning basic demographic information, such as child age, gender, and family income.
PTSS
Given the difficulty inherent in conducting interviews in-hospital during the acute aftermath of a child’s trauma, we assessed in-hospital child and caregiver PTSS due to the child’s injury with the self-report Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997). The 22-item IES-R has been validated in children ≥8 years and adults (e.g., Stallard, Velleman, & Baldwin, 1999). Total PTSS scores and subscale scores were computed. For the child, Cronbach’s α’s were .87 for total PTSS scores, .85 for reexperiencing, .85 for avoidance, and .72 for hyperarousal symptoms. For the caregiver, Cronbach’s α’s were .94 for total PTSS scores and .88 for avoidance symptoms.
At follow-up, child PTSS were assessed using the Clinician Administered PTSD Scale—Children and Adolescents (CAPS-CA; Nader et al., 1996), while caregivers were administered the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995). Caregivers and children were interviewed in separate rooms to prevent their responses from influencing each other. Subthreshold criteria were met, if the participant endorsed at least one symptom from each symptom cluster. This definition has been used in numerous studies in both adults (Stein et al., 1997) and children (Daviss et al., 2000; Nugent et al., 2007; Ostrowski et al., 2007). Given low rates of diagnostic levels of PTSD, the majority of analyses were conducted on continuous CAPS/CAPS-CA total scores. Cronbach’s α for total CAPS-CA score in the present study was .90 and for the CAPS was .85.
Medical information
Length of stay, time of admit and discharge, ISS scores, medications, blood alcohol content, and chronic diseases were recorded from medical charts.
Procedure
The human subjects review boards of Akron Children’s Hospital and Kent State University approved the following procedures. Trained research assistants approached potential participants to assess whether the child met DSM-IV-TR diagnostic criterion A (assessed via four questions inquiring if the child experienced threat to his/her life and if the child responded with fear, horror, or helplessness). Caregivers and children aged ≥10 years were provided with a detailed written consent form with age-appropriate grammar. The study was described verbally to children under the age of 10 years, who were asked for their assent.
In-hospital assessment
The in-hospital assessment included gathering demographic and contact information. Caregivers also gave authorization for release of medical information from the child’s medical chart. Finally, children and caregivers completed the IES-R.
Two- and six-week follow-up
Follow-up sessions were conducted at 2- and 6-weeks posttrauma in the participants’ homes and involved the assessment of caregiver and child PTSS. The 2-week time point was included as it represents a meaningful medical time point; many injury patients return for clinic visits to check progress ∼2 weeks following treatment. Primary care providers can play an important role in recognizing ongoing or escalating symptoms of PTSD that may not be apparent to others (Kazak et al., 2006). The 6-week time point was chosen as it allows for sufficient time to pass posttrauma to meet the duration criterion for a diagnosis of PTSD. At each time point, the CAPS-CA (Nader et al., 1996) was administered to the child and the CAPS (Blake et al., 1995) to the caregiver with the child’s trauma as the targeted index event. These interviews are considered the gold standard for assessing child and adult PTSD.
Statistical analyses
Preliminary analyses
Preliminary analyses were run in Statistics Package for the Social Sciences Version 17 (SPSS 17; SPSS 2009). Initial one-way analyses of variance (ANOVAs) and Pearson-product moment correlations were conducted to determine whether child PTSS levels differed by demographic variables.
Hypothesized model
Structural equation modeling (SEM; AMOS Version 7.0) was used to allow for the examination of the simultaneous effects of child and caregiver in-hospital PTSS on child posttraumatic distress. The proposed model was hypothesized to reflect the temporal development of child PTSS following pediatric injury by depicting the impact of child in-hospital PTSD symptom clusters and caregiver overall in-hospital PTSS on the development of child and caregiver 2-week total PTSS and child 6-week total PTSS. Due to concerns of low statistical power resulting from a small sample size, only those variables that were related to child 2- and 6-week PTSS were included in the model. Covariance matrices and ML estimates were used as the method of estimation for all models tested.
Empirical research suggests that sample size adequacy is best measured by the ratio of subjects-to-estimated parameters (n:q) and complexity of the model rather than by sample size in an absolute sense (MacCallum, Widaman, Zhang, & Hong, 1999) with some suggesting that the ratio of number of cases per model parameter (n:q) be at least five when using ML estimation under reasonable distributional conditions (see Jackson, 2001, 2003). We believe that, given the lack of research examining the development of child PTSS and the longitudinal nature of our data set, the current model provides an excellent opportunity to provide preliminary evidence for the impact of acute child and caregiver PTSS on subsequent child PTSS.
Post hoc analyses
Hierarchical linear regression analyses were conducted examining the impact of caregiver in-hospital avoidance and child in-hospital PTSD symptom clusters on the development of child 6-week PTSS.
Results
Demographics
ISS (range 1–22; mean = 7.35), age, family income, race, and type of injury were not related to child PTSS at any time point (all p’s > .09). Given this, and that inclusion of these demographic variables did not alter results, these variables were not entered into the hypothesized model.
Two-weeks following the child’s admission, 17 (18%) children endorsed at least subthreshold levels of PTSS. Fifteen percent (n = 15) of the children met at least subthreshold criteria for PTSD at the 6-week follow-up. Caregiver and child PTSS were significantly correlated at each time point (in-hospital: r = .44, p ≤ .001; 2-weeks posttrauma: r = .34, p ≤ .001; 6-weeks posttrauma: r = .26, p ≤ .02; see Table II for descriptive information).
Table II.
PTSD Symptom Descriptive Information
| Variables |
Mean (SD); range |
|
|---|---|---|
| Child | Caregiver | |
| In-hospital (IES-R) | ||
| Total | 21.81 (15.16); 0–64 | 13.14 (15.49); 0–76 |
| Reexperiencing | 6.49 (6.22); 0–23 | 4.30 (5.74); 0–28 |
| Avoidance | 8.83 (6.27); 0–25 | 4.98 (5.81); 0–24 |
| Hyperarousal | 6.56 (5.30); 0–21 | 3.85 (4.88); 0–24 |
| 2-week CAPS-CA/CAPS | ||
| Total | 17.84 (12.59); 0–43 | 11.50 (12.53); 0–57 |
| Reexperiencing | 3.43 (3.77); 0–14 | 5.05 (5.84); 0–29 |
| Avoidance | 4.39 (4.81); 0–20 | 1.40 (2.81); 0–13 |
| Hyperarousal | 6.66 (5.03); 0–20 | 3.29 (3.73); 0–14 |
| 6-week CAPS-CA/CAPS | ||
| Total | 17.70 (15.96); 0–51 | 9.43 (3.51); 0–46 |
| Reexperiencing | 3.77 (3.78); 0–12 | 3.36 (2.06); 0–10 |
| Avoidance | 6.09 (7.67); 0–23 | 2.00 (1.06); 0–14 |
| Hyperarousal | 5.59 (3.85); 0–10 | 2.53 (2.72); 0–10 |
Note. IES-R = impact of event scale—revised; Weiss & Marmar, 1997; CAPS-CA = clinician administered PTSD scale for children and adolescents; Nader et al., 1996; CAPS = clinician administered PTSD scale; Blake et al., 1995.
Development of child overall PTSS
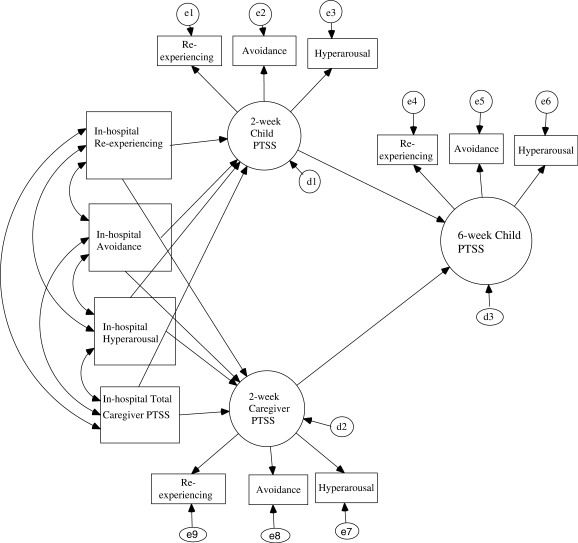
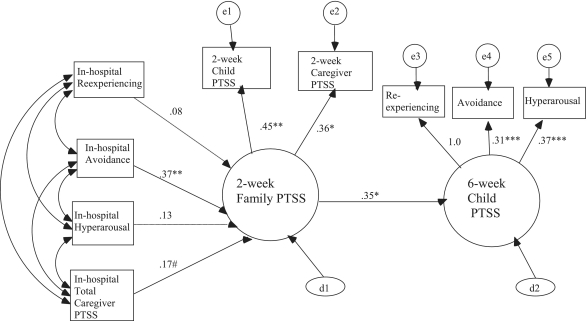
Preliminary examination of the data revealed that all assumptions of SEM were met. In accordance with the two-step approach in examining model fit (Kline, 2005), we first examined the hypothesized model (see Figure 1) as a measurement model. Results suggested a poor fit to the data [χ2 (24, N = 118) = 84.78, p < .001, CFI = .89, NNFI = .80, RMSEA = .15, confidence interval (CI) 95% CI = 0.11–0.18]. All indicators loaded substantially onto their respective factors (all p’s < .001). However, inspection of the model revealed that the estimated factor covariance between 2-week child and caregiver PTSS was very high (p < .001) suggesting that these factors were not distinct. Based on these results, the measurement model was respecified such that 2-week child and caregiver PTSS were merged to create a 2-week “family PTSS” latent variable with caregiver and child CAPS/CAPS-CA scores as indicators. The respecified model was a better fit to the data [χ2 (4, N = 118) = 5.98, p = .20, CFI = .99, NNFI = .97, RMSEA = .06, 95% CI = 0.00–0.16]. The measurement model was then specified as a hybrid model in which in-hospital child PTSS clusters and caregiver total PTSS were hypothesized to predict 2-week family PTSS and 6-week child PTSS (see Figure 2). Results revealed a good fit to the data [χ2 (20, N = 118) = 31.20, p = .05, CFI = .94, NNFI = .93, RMSEA = .06, 95% CI = 0.00–0.11]. Higher levels of child in-hospital avoidance symptoms predicted higher levels of 2-week family PTSS (p ≤ .01) and in-hospital caregiver total PTSS marginally predicted 2-week family PTSS (p = .06). Inspection of the pathways leading from 2-week family PTSS to child 6-week PTSS revealed a significant positive effect (p ≤ .05). A correlation matrix of all model variables is provided as a Supplementary Table I.
Figure 1.
Hypothesized Model of Child PTSS Development Following Pediatric Injury.
Figure 2.
Revised Model of Child PTSS Development Following Pediatric Injury. Note. PTSS = Posttraumatic stress symptoms. Path loadings are standardized coefficients. [χ2 (20, N = 118) = 31.20, p = .05, CFI = .94, NNFI = .93, RMSEA = .06, 95% CI = 0.00–0.11].
#p = .06, *p < .05, **p < .01.
In order to fully test the hypothesized model, pathways leading from in-hospital PTSS to child 6-week PTSS were included. Results from the revised model suggested an adequate fit [χ2 (16, N = 118) = 29.02, p = .02, CFI = .93, NNFI = .91, RMSEA = .08, 95% CI = 0.03–0.13] suggesting that the partially mediated model was a better fit. Results remained the same as the original model [i.e., higher levels of child in-hospital avoidance symptoms predicted higher levels of 2-week PTSS (p ≤ .05), and 2-week PTSS positively predicted 6-week PTSS (p ≤ .05)], with the exception that in-hospital caregiver PTSS did not significantly predict 2-week family PTSS or 6-week child PTSS (all p’s > .12).
Exploratory analyses
After controlling for gender and ISS, hierarchical linear regression analyses revealed that in-hospital caregiver avoidance symptoms interacted with in-hospital child reexperiencing symptoms to predict 6-week child PTSS [ΔR2 = .05, p ≤ .05; F(5, 82) = 2.40, p < .05; t = 2.20, p < .05]. Decomposition of the interaction suggested that high levels of caregiver avoidance symptoms and high levels of child reexperiencing symptoms predicted 6-week child PTSS. However, the slopes of the individual regression lines were nonsignificant (p = .09). Caregiver in-hospital avoidance symptoms did not significantly interact with in-hospital child avoidance or hyperarousal symptoms to predict child 6-week PTSS (all p’s > .09).
Discussion
The present study prospectively examined the development of child PTSS over time following pediatric injury while also examining the impact of caregiver PTSS on child posttraumatic adjustment. Consistent with prior literature (Murray, Kenardy, & Spence, 2008), child injury victims admitted to the ED endorsed moderate rates of PTSS that may be overlooked by medical professionals and may undermine child recovery and development. Interestingly, our hypothesized model did not fit the data well, but rather a re-specified model combining caregiver and child 2-week PTSS was a better fit to the data. Contradictory findings have been found regarding the association between caregiver and child PTSS and have been confounded by the use of multiple reporters on child symptoms (e.g., child self-report, parents, teachers, nurses). The current study suggests that 2-week child and/or caregiver posttraumatic distress might reflect general levels of symptoms experienced by the family unit, and that the assessment of family stress during the acute phase of responding to a child's trauma may add more to our understanding of child symptom development than assessing PTSS in one individual. Future research is needed to further examine the interplay between child and caregiver posttraumatic distress within 1 month posttrauma and the interactions between symptoms experienced by children and their family members. Additional studies should also examine how age and gender of the child further impacts these relationships.
Contrary to prior studies implicating early psychological and physiological hyperarousal as a predictor of subsequent PTSS in adults and children (Delahanty, Nugent, Christopher, & Walsh, 2005; Kassam-Adams, Garcia-Espana, Fein, & Winston, 2005; Schell, Marshall, and Jaycox, 2004), the present model revealed that elevated levels of child in-hospital avoidance symptoms significantly predicted 2-week family PTSS. Further, post hoc analyses revealed an interaction between in-hospital caregiver avoidance and child reexperiencing symptoms in predicting 6-week child PTSS. More specifically, a child was more likely to suffer from persistent PTSS when the caregiver experienced high levels of avoidance and the child endorsed high levels of reexperiencing. However, the slopes of the regression lines were nonsignificant, necessitating the viewing of this finding with caution. Future research with a larger sample size that will afford more statistical power is needed to either replicate or refute the current findings.
Implications for the treatment of PTSD symptoms in children
The current study highlights the importance of examining both the child’s and caregiver’s traumatic responses to fully understand the development and maintenance of child posttraumatic distress. Similar to prior studies, the present study demonstrates the importance of early reexperiencing symptoms in the development of child PTSS (Meiser-Stedman, 2002). It appears that caregiver avoidance symptoms concurrent with child reexperiencing symptoms may further increase a child’s risk for subsequent PTSS. Child reexperiencing symptoms may force caregivers to confront the child’s distress and make it difficult for caregivers to contain their own and their child’s anxieties, which may intensify the child’s own intrusions. Caregivers may then engage in avoidance strategies to help the child cope. However, caregiver avoidance symptoms may not allow for the identification and processing of the child’s distress (Best, Streisand, Catania, & Kazak, 2001; Smith, Perrin, Yule, & Rabe-Hesketh, 2001). Results underscore the importance of cognitive-behavioral family interventions that address both cognitive and avoidance symptoms in children and their caregivers in the treatment of child PTSS following pediatric injury.
Limitations and areas for future research
The present study is limited by a relatively small sample size which may have resulted in low statistical power. Furthermore, the sample consisted of mild to moderately injured participants and were primarily Caucasian and the present results may not generalize to more severely injured children or diverse populations. In addition, different measures of PTSD were used at baseline and at follow-up. Given the difficulties in administering structured interviews in-hospital, the current study used self-report measures to assess in-hospital PTSS. While this may limit the internal validity of the assessments, prior research has found high correlations between the CAPS and IES-R and has used the IES-R to predict subsequent PTSD as assessed by the CAPS (Turnbull, Campbell, & Swann, 2001).
The current study focused on the impact of pediatric injury but was unable to differentiate what aspect of the injury was the most traumatic. Child victims of traumatic injury experience “on-going” trauma from the point of injury through the subsequent medical procedures. These medical procedures could be conceptualized as additional potentially traumatizing experiences or as a continuation of the initial trauma (Kazak et al., 2006). Further, traumatic medical events can also vary in their type and intensity. Although type (intentional versus unintentional) and severity of injury were not significantly related to child PTSS in the current sample, this may be due to insufficient power and unequal representation of different injury mechanism subgroups. Intentional or interpersonal trauma often involves increased guilt and increased risk for PTSD. Future research in a larger sample of mixed trauma victims may find differential risk for PTSS is afforded by different types or severity of injury (Le Brocque et al., 2010).
The present study suggests that regardless of the type of injury, avoidance symptoms resulting from the child’s injury may increase a child’s risk for subsequent distress. Avoidance symptoms of PTSD have been found to be related to, but not identical to, avoidant coping in both child and adult studies (Bryant & Harvey, 1995; Ullman, Townsend, Filipas, & Starzynski, 2007). Further, avoidant coping may be a mechanism through which PTSD symptoms develop (Pacella et al., manuscript under review). Although not measured in the present study, children may model caregiver coping styles in order to minimize their own levels of distress (Fivush, 1998). Given that posttraumatic coping processes are crucial in shaping emotional outcomes after traumatic events (Bryant & Harvey, 1995), future research should examine the impact of avoidant coping during the days, weeks, and months following the child’s trauma.
The present study also focused primarily on early PTSS as predictors. While research has demonstrated that early PTSS can negatively impact child psychosocial development, research has identified a number of other variables that predict the development of more persistent PTSS. Given prior research demonstrating physiological differences between children who do and do not experience PTSS following pediatric injury (Delahanty, Nugent, Christopher, & Walsh, 2005; Kassam-Adams, Garcia-Espana, Fein, & Winston, 2005; Ostrowski, Christopher, vanDulmen, & Delahanty, 2007), future studies should examine biopsychological variables in models of child posttraumatic distress development.
Further, due to concerns of power, the current study focused specifically on in-hospital symptoms of PTSD on the impact of subsequent total 2- and 6-weeks posttrauma. Rather than examining total symptoms, future research is needed examining the development of specific PTSD symptom clusters over time as these studies may shed light on timing of symptom development and inform the content of early preventive interventions. In addition, inclusion of additional family members may also assist in the identification of child and family risk and resilience factors.
A better understanding of the relationship between early PTSS and persistent posttraumatic distress in pediatric injury victims can increase medical professionals’ ability to assess child trauma victims’ mental health needs and provide appropriate services. The present study highlights the importance of assessing posttraumatic symptoms in children and their caregivers following a child’s injury. Findings suggest that children and/or caregivers may need additional follow-up mental health care if they are reporting symptoms of avoidance or re-experiencing in the acute aftermath of a traumatic injury.
Funding
National Institute of Mental Health (grant R34 MH073014, in part).
Conflicts of interest: None declared.
Supplementary Material
References
- Barakat L P, Kazak A E, Meadows A T, Casey R, Meeske K, Stuber M L. Families surviving childhood cancer: A comparison of posttraumatic stress symptoms with families of healthy children. Journal of Pediatric Psychology. 1997;22:843–859. doi: 10.1093/jpepsy/22.6.843. [DOI] [PubMed] [Google Scholar]
- Basson M, Guinn J, Mc Elligott J, Vitale R, Brown W, Fielding L. Behavioral disturbances in children after trauma. Journal of Trauma. 1991;31:1363–1368. doi: 10.1097/00005373-199110000-00008. [DOI] [PubMed] [Google Scholar]
- Best M, Streisand R, Catania L, Kazak A E. Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. Journal of Pediatric Psychology. 2001;26(5):299–307. doi: 10.1093/jpepsy/26.5.299. [DOI] [PubMed] [Google Scholar]
- Blake D D, Weathers F W, Nagy L M, Kaloupek D G, Gusman F D, Charney D S, Keane T M. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bryant R A, Harvey AG. Processing threatening information in post-traumatic stress disorder. Journal of Abnormal Psychology. 1995;104:537–554. doi: 10.1037//0021-843x.104.3.537. [DOI] [PubMed] [Google Scholar]
- Bryant R A, Salmon K, Sinclair E, Davidson P. The relationship between acute stress disorder and posttraumatic stress disorder in injured children. Journal of Traumatic Stress. 2007;20(6):1075–1079. doi: 10.1002/jts.20282. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. Childhood Injury Report. 2010, June. Retrieved from http://www.cdc.gov/ [Google Scholar]
- Daviss W, Mooney D, Racusin R, Ford J, Fleischer A, McHugo G. Predicting posttraumatic stress after hospitalization for pediatric injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(5):576–583. doi: 10.1097/00004583-200005000-00011. [DOI] [PubMed] [Google Scholar]
- Delahanty D L, Nugent N R, Christopher N C, Walsh M. Initial urinary epinephrine and cortisol levels predict acute PTSD symptoms in child trauma victims. Psychoneuroendocrinology. 2005;30(2):121–128. doi: 10.1016/j.psyneuen.2004.06.004. [DOI] [PubMed] [Google Scholar]
- De Vries A, Kassam-Adams N, Cnaan A, Sherman-Slate E, Gallagher P R, Winston F K. Looking beyond the physical injury: Posttraumatic stress disorder in children and parents after pediatric traffic injury. Pediatrics. 1999;104:1293–1299. doi: 10.1542/peds.104.6.1293. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark D. A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Fivush R. Children’s recollections of traumatic and nontraumatic events. Development and Psychopathology. 1998;10(4):699–714. doi: 10.1017/s0954579498001825. [DOI] [PubMed] [Google Scholar]
- Jackson D L. Sample size and the number of parameter estimates in maximum likelihood confirmatory factor analysis: A Monte Carlo investigation. Structural Equation Modeling. 2001;8:205–223. [Google Scholar]
- Jackson D L. Revisiting sample size and number of parameter estimates: Some support for the N:q hypothesis. Structural Equation Modeling. 2003;10(1):128–141. [Google Scholar]
- Kahana S Y, Feeny N C, Youngstrom E A, Drotar D. Posttraumatic stress in youth experiencing illnesses and injuries: An exploratory meta-analysis. Traumatology. 2006;12:148–161. [Google Scholar]
- Kassam-Adams N, Garcia-Espana J, Fein J A, Winston F K. Heart rate and posttraumatic stress in injured children. Archives of General Psychiatry. 2005;62(3):335–340. doi: 10.1001/archpsyc.62.3.335. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Winston F K. Predicting child PTSD: The relationship between ASD and PTSD in injured children. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):403–411. doi: 10.1097/00004583-200404000-00006. [DOI] [PubMed] [Google Scholar]
- Kazak A E, Alderfer M, Rourke M T, Simms S, Streisand R, Grossman J R. Posttraumatic Stress Disorder (PTSD) and Posttraumatic Stress Symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology. 2004;29(3):211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- Kazak A E, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer M, Rourk M. An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology. 2006;31(4):343–355. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- Kenardy J, Spence S, Macleod A. Screening for risk of persistent posttraumatic morbidity in children following traumatic injury. Pediatrics. 2006;118:1002–1009. doi: 10.1542/peds.2006-0406. [DOI] [PubMed] [Google Scholar]
- Keppel-Benson J M, Ollendick T H, Benson M J. Post-traumatic stress in children following motor vehicle accidents. Journal of Child Psychology and Psychiatry. 2002;43(2):203–212. doi: 10.1111/1469-7610.00013. [DOI] [PubMed] [Google Scholar]
- Kline R B. Principles and practice of structural equation modeling. New York, NY: The Guilford Press; 2005. [Google Scholar]
- Landolt M A, Vollrath M, Ribi K, Gnehm H E, Sennhauser F H. Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry. 2003;44(8):1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- Le Brocque R M, Hendricks J K, Kenardy J A. The course of posttraumatic stress in children: Examination of recovery trajectories following traumatic injury. Journal of Pediatric Psychology. 2010;35(6):646–655. doi: 10.1093/jpepsy/jsp050. [DOI] [PubMed] [Google Scholar]
- Levi R, Drotar D, Yeates K, Taylor G. Posttraumatic stress symptoms in children following orthopedic or traumatic brain injury. Journal of Clinical Child Psychology. 1999;28:232–243. doi: 10.1207/s15374424jccp2802_10. [DOI] [PubMed] [Google Scholar]
- MacCallum R C, Widaman K F, Zhang S, Hong S. Sample size in factor analysis. Psychological Methods. 1999;4:84–99. [Google Scholar]
- Meiser-Stedman R. Towards a cognitive–behavioral model of PTSD in children and adolescents. Clinical Child and Family Psychology Review. 2002;5:217–232. doi: 10.1023/a:1020982122107. [DOI] [PubMed] [Google Scholar]
- Murray B L, Kenardy J A, Spence S H. Brief report: Children's responses to trauma- and nontrauma-related hospital admission: A comparison study. Journal of Pediatric Psychology. 2008;3(4):435–440. doi: 10.1093/jpepsy/jsm078. [DOI] [PubMed] [Google Scholar]
- Nader K O, Kriegler J A, Blake D D, Pynoos R S, Newman E, Weather F. White River Junction, VT: National Center for PTSD; 1996. Clinician administered PTSD scale, child and adolescent version (CAPS-CA) [Google Scholar]
- National Child Traumatic Stress Network. Medical events and traumatic stress in children and families. 2010 June. Retrieved from: http://www.nctsnet.org. [Google Scholar]
- National Safe Kids Campaign. Injury facts: Childhood injury. 2004. Retrieved from: http://www.safekids.org. [Google Scholar]
- Nugent N R, Ostrowski S A, Christopher N, Delahanty D L. Parental posttraumatic stress symptoms as a moderator of child’s acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. Journal of Pediatric Psychology. 2007;32(3):309–318. doi: 10.1093/jpepsy/jsl005. [DOI] [PubMed] [Google Scholar]
- Ostrowski S A, Christopher N, Delahanty D L. Brief Report: The impact of maternal posttraumatic stress disorder symptoms and child gender on risk for persistent posttraumatic stress disorder symptoms in child trauma victims. Journal of Pediatric Psychology. 2007;32(3):338–342. doi: 10.1093/jpepsy/jsl003. [DOI] [PubMed] [Google Scholar]
- Ostrowski S A, Christopher N C, van Dulmen M H M, Delahanty D L. Acute child and mother psychophysiological responses and subsequent PTSD following a child’s traumatic event. Journal of Traumatic Stress. 2007;20(5):1–11. doi: 10.1002/jts.20286. [DOI] [PubMed] [Google Scholar]
- Pacella M L, Irish L, Ostrowski S A, Sledjeski E, Fallon W, Spoonster E, Delahanty DL. Avoidant coping as a mediator between peritraumatic dissociation and posttraumatic stress symptoms. Journal of Traumatic Stress. manuscript under review doi: 10.1002/jts.20641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman R K, Orr S P, Lowenhagen M J, Macklin M L, Altman B. Pre-Vietnam contents of posttraumatic stress disorder veterans’ service medical and personnel records. Comprehensive Psychiatry. 1991;32(5):416–422. doi: 10.1016/0010-440x(91)90018-8. [DOI] [PubMed] [Google Scholar]
- Scheeringa M, Zeanah C. Symptom expression and trauma variables in children under 48 months of age. Journal of Infant Mental Health. 1995;16:259–270. [Google Scholar]
- Schell T L, Marshall G N, Jaycox L H. All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology. 2004;113(2):189–197. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- Smith P, Perrin S, Yule W, Rabe-Hesketh S. War exposure and maternal reactions in the psychological adjustment of children from Bosnia-Hercegovina. Journal of Child Psychology and Psychiatry. 2001;42:395–404. [PubMed] [Google Scholar]
- Stallard P, Velleman R, Baldwin S. Psychological screening of children for post-traumatic stress disorder. Journal of Child Psychology and Psychiatry. 1999;40(7):1075–1082. [PubMed] [Google Scholar]
- Stein M B, Walker J R, Hazen A L, Forde D R. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Turnbull S J, Campbell E A, Swann I J. Post-traumatic stress disorder symptoms following a head injury: Does amnesia for the event influence the development of symptoms? Brain Injury. 2001;15(9):775–785. doi: 10.1080/02699050110034334. [DOI] [PubMed] [Google Scholar]
- Ullman S E, Townsend S M, Filipas H H, Starzynski L L. Structural models of the relations of sexual assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31:23–37. [Google Scholar]
- Weiss D, Marmar C. The impact of event scale–revised. In: Wilson T, Keane J, editors. Assessing psychological trauma and PTSD. New York: Guildford Press; 1997. pp. 399–411. [Google Scholar]
- Winston F K, Kassam-Adams N, Garcia-España F, Ittenbach R, Cnaan A. Screening for risk of persistent posttraumatic stress in injured children and their parents. Journal of the American Medical Association. 2003;290(5):643–649. doi: 10.1001/jama.290.5.643. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.