Abstract
The Global Alliance for Vaccines and Immunization (GAVI), now 10 years old, was established as a successful and innovative public–private partnership to deal with a fundamental inequity. The poorest children in the poorest parts of the world were being denied access to life-saving vaccines simply on the basis of cost. GAVI has been successful in mobilizing significant funding from donors and through innovative financing instruments, immunizing large numbers of children. GAVI has been less successful, at least in the time frames first envisaged, at quickly reducing the prices of new and under-used vaccines to levels affordable by the poorest countries. Vaccines remain some of the most cost effective of public health interventions. As GAVI seeks to introduce a new set of vaccines to tackle major killers such as pneumonia and diarrhoea, and emerging threats such as cervical cancer, it needs to raise significant additional funds. There is no single solution. Multiple and new instruments will be required to raise finance both globally and at the country level, and also to incentivize industry and others to provide vaccines at affordable prices to the poorest countries.
Keywords: vaccines, GAVI, immunization
1. Introduction
The Global Alliance for Vaccines and Immunization (GAVI) works in the poorest countries in the world, the least developed countries according to World Bank classification based on gross domestic product per capita.
GAVI is a highly regarded organization, independently assessed for high impact and value for money [1]. Yet as it celebrates its 10th anniversary and enters its third 5 year strategy period, it is an appropriate moment to reflect on the Alliance's achievements and where it might have achieved more.
GAVI was set up to deal with a fundamental inequity, one that resulted in the children of the richest parts of the world, with the lowest child mortality, benefitting from an increasing range of vaccines while those with the highest mortality, in the poorest parts of the world, had restricted access to the same, more or better vaccines solely for reasons of ‘affordability’ and access to health services. There was an increasing risk that with the perception of a limited market in the developing world, industry in the developed world would increasingly tailor its products to the rich north and that the vaccine industry in emerging market economies would target either traditional vaccines or those designed for a northern market.
GAVI, an innovative public–private partnership, set out to change that paradigm by setting up an alliance of key stakeholders in immunization that included multi-laterals, donors, foundations, developing countries, industry, non-governmental organizations and academia. Without the coordinated collaboration of the United Nations Children's Fund (UNICEF), the World Health Organization (WHO) and the World Bank, with each organization playing to its strengths, the sum of GAVI would not have been greater than the sum of its parts. This was achieved despite the well-known institutional tensions, rivalries and early opposition to the establishment of GAVI.
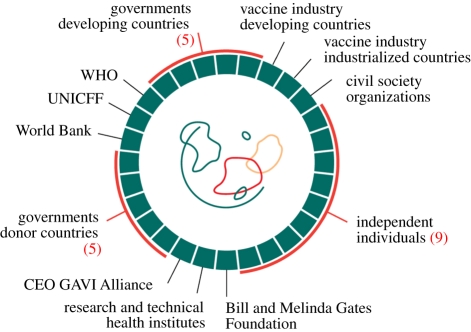
The current board structure of GAVI Alliance is shown in figure 1. Uniquely, for a public–private partnership in health, one-third of the current board includes individuals recruited not only because of their institutional representation but also for their specific skills, in particular, private sector expertise and background. More controversially, for some, the vaccine industry (north and south) was included on the board. As a result, all major stakeholders are partners in the Alliance through its governance structures. As GAVI went through major governance changes, with the combining of two boards in 2009, the consensus was that such an inclusive representation remained appropriate. However, it would be fair to say that the composition and effectiveness of both the previous and the current governance structures, including the presence of industry, have not yet been independently evaluated.
Figure 1.
Structure of the GAVI Alliance board.
Over the past 10 years, GAVI has mobilized significant additional financial support from donors and foundations for immunization, resulting in an annual programme spend of more than US$1 billion. GAVI also recognized the need to evolve from a narrow, vertical and technocratic programme and to work within a broader development model, according to the Paris Principles, with civil society organizations (CSOs deliver up to 65% of health services in some countries), and as a part of integrated maternal and child health services. GAVI determined that accessibility to vaccines delivered through integrated services for women and children depended on functioning health systems that met the needs of the poorest. GAVI could not take on the challenge of poorly functioning health services alone, even when responding to a strong demand from GAVI eligible countries to do more in the area of health system strengthening (HSS). As a consequence, GAVI worked with others to develop a joint programme for HSS launched in 2010 with the World Bank, WHO and the Global Fund to fight AIDS, Tuberculosis and Malaria (GFATM)—the Health Systems Funding Platform. It is too early to assess the success of this approach, but early signs from Nepal and Ethiopia are positive. Funding in this area could usefully focus on the very poorest and improving their access to basic services.
2. Health impact
Vaccines are a powerful tool, with the potential to tackle significant causes of mortality now and in the future. For example, if pneumococcal and rotavirus vaccines were rolled out to full coverage, an additional one million child deaths could be prevented, a significant contribution to Millennium Development Goal 4 (child survival). More than 200 000 women die each year from cervical cancer, mostly in the poorest countries of the world. Numbers are increasing, reflected in a growing cohort of human papilloma virus-infected woman, a trend that could be reversed through effective vaccination and reproductive health programmes for adolescents.
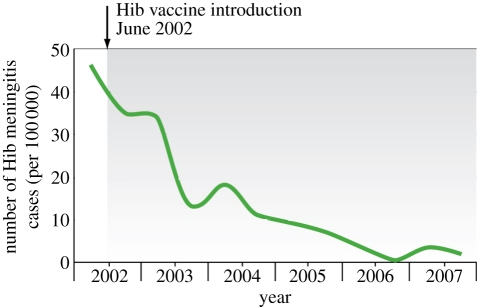
Here, there has been significant progress. By the end of 2010, according to WHO data, GAVI support had resulted in 288 million children being immunized and 5.4 million deaths prevented. Steadily increasing vaccine coverage (nearly 80% diphtheria polio tetanus (DPT) coverage in 2010 is projected by WHO) has resulted in significant impact on disease, for example, on Haemophilus influenzae type b (Hib) meningitis (figure 2) at least in those countries where impact can be measured. Immunization is now closer to universal coverage than most other health interventions, enabling rapid introduction of life-saving new vaccines and presenting an important opportunity to deliver other child and maternal health services. Yet, there are legitimate concerns that, as in other areas of health, the poorest quintile and, in particular, women and female children may not be receiving such benefits. Until all countries, with the support of WHO and UNICEF, monitor and record immunization and other health services by gender and income, it will be hard to ensure such inequalities do not emerge or be perpetuated. The international community will also need to invest more in health systems capability in the areas of surveillance, monitoring and independent verification of programme impact.
Figure 2.
The impact of the introduction of Haemophilus influenzae type b (Hib) conjugate vaccine on the incidence of Hib meningitis in three sentinel hospitals in Uganda [2].
3. Finance
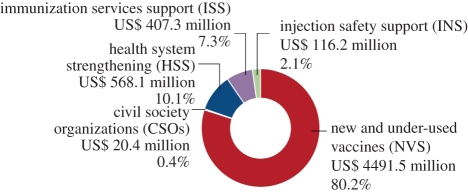
As of mid 2010 (figure 3), GAVI had committed US$5.6 billion to support the poorest countries in the world; 80 per cent of finance had been used for the purchase of new vaccines such as pentavalent vaccine; 2 per cent of resources had been used for injection safety support; 7 per cent for immunization system support and 10 per cent for broader health system strengthening. GAVI mobilized this finance not only through traditional means but also importantly through innovative financing mechanisms, the most notable of which was the Innovative Financing Facility for Immunization (IFFIm). To date, US$2.7 billion has been raised by the IFFIm, through the issuing of bonds securitized by major donors on private capital markets. This enabled GAVI to increase its annual programme spend on a long-term basis. GAVI was able to meet developing countries ambition and create a vaccine market where none was perceived to exist before.
Figure 3.
The financial commitment of the GAVI Alliance (total US$5.6 billion) by category as of July 2010.
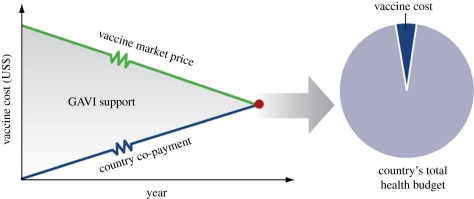
The GAVI model was one that sought not only to raise the necessary volume of finance but also, through long-term predictable finance, to shape the vaccine market, bring new vaccine prices down to affordable levels and to work with countries to mobilize their own resources to co-finance vaccine purchase. Such a long-term vision (15–20 years in the poorest countries) meant that developing countries would in the future be in a position to financially sustain their own new vaccine programmes (figure 4). The critical driver would be new vaccine prices. In this area, GAVI has been only partially successful.
Figure 4.
The GAVI model for making vaccines affordable to poor countries.
The GAVI model assumes that by mobilizing significant finance and generating predictable and measurable demand from developing countries, markets can be ‘shaped’ not only through GAVI's global purchasing power and the impact of new entrants to the market (notably emerging market manufacturers able to compete at a global scale on quality and price), but also through other innovative financial instruments such as the advance market commitment (AMC). The AMC, by legal agreement, binds future donor pledges and then uses those pledges to incentivize industry to produce a specified vaccine with specified impact at an affordable end price for the poorest countries. The first AMC was launched in 2010 for pneumococcal conjugate vaccines, vaccines that have the potential to prevent a leading cause of child mortality. At the same time, this is no free lunch. Countries are expected to co-finance according to their ability to pay. The co-financing programme had a modest start and is currently under revision, but has demonstrated that countries can contribute to programme costs and that countries ‘graduating’ from GAVI support can sustain their programmes. Recent graduates (new emerging middle income economies) include China and its expanded hepatitis B programme, previously GAVI eligible countries in the former eastern European block and in Latin America.
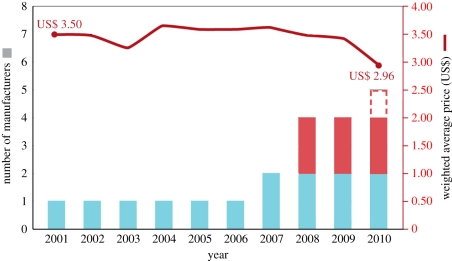
At the same time, it is important that vaccines and vaccine programmes remain an affordable proportion of national health budgets and meet country priorities. For the very poorest countries, vaccine affordability remains unclear. Like other focused programmes, such as those in the area of HIV/AIDS, budgetary distortion remains a real risk and one that GAVI has yet to fully address. Work by the Institute of Health Metrics and Evaluation [3] alerts us to the reality that while some developing countries are using external financial and programme support in addition to their own national health spend, many are not. Countries may choose to reduce or to not increase their own budgetary allocations to health. Development aid in the health sector is fungible. A finding of no surprise to general development specialists, but a fact frequently overlooked by the Health and HIV communities. Despite our best intentions, donor support can and does result in distortions in national priorities. GAVI has now reached a cruising altitude, with a need for constant but sufficient funding but, importantly for donors, not an annually growing budget. Sustaining the cruising attitude allows the GAVI model to function and will allow GAVI and developing countries to sequentially and sustainably introduce new vaccines. GAVI is not a model of a constantly increasing and unsustainable demand for donor support. However, a long-term vision is required. Key to the sustainability of GAVI's model will be vaccine pricing and the influence on that pricing of predictable and sustainable demand. While vaccine prices have come down over time, particularly recently in some areas, this has not happened as quickly as the GAVI founders anticipated. With fewer companies in the field than in the area of pharmaceutical manufacture, high investment costs and vital quality assurance requirements, competition has been slow to emerge and monopoly situations or minimal competition have been the norm. Figure 5 shows, given the long lead times required for vaccine procurement, that it can take 2–3 years before new entrants impact on vaccine pricing.
Figure 5.
The number of manufacturers and the decline in price of pentavalent (DTP, hepatitis B, Hib) vaccine. Dashed line, expected prequalified manufacturers based in emerging markets; red bars, prequalified manufacturers based in emerging markets; light blue bars, prequalified industrialized country manufacturers; solid red line, weighted average price (WAP).
If one thing is clear, it is that there is no single solution. A combination of innovation, as in the AMC, better procurement mechanisms exposed to greater competition,1 improved forecasting on demand, directly working with vaccine manufacturers as in the case of meningococcal vaccine (PATH) and greater effort by large pharma, more might be achieved. It is not the purpose of this paper to go into such issues in detail, but to highlight that more needs to be done and that there is no single solution. It is for this reason that the board has determined that vaccine price reduction should been made a high-order objective for the third phase of GAVI (2011–2015).
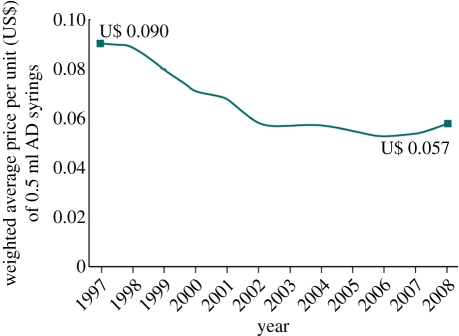
More impressive than a reduction in the price of new vaccines has been the reduction in the price of auto-disable syringes (figure 6). GAVI has always insisted that auto-disable syringes be a part of GAVI programmes, and provided catalytic funding to countries to introduce their procurement. The programme is now phasing out and nearly all GAVI-supported countries independently finance and procure such syringes.
Figure 6.
The cost of auto-disable (AD) syringes used for vaccination [4].
4. Conclusions
In its short life, the GAVI Alliance has accelerated the introduction of new vaccines in the poorest countries, attracted additional funding to the world of vaccines, generated country ownership and led through organizatio nal and programmatic innovation. An early example of innovation was a programme of result-based financing (cash rewards against deliverable performance)—the Immunization Service Support (ISS) programme. Much has been learned about what works and what may not in this area [4], including the challenge of measurement, verification, perverse incentives and the necessary management capacity to make such programmes effective and accountable.
GAVI has demonstrated that it can evolve from a narrow vertical programme, respond to the need and increasing consensus that health systems matter, that integrated maternal and child health services are overall more effective, more efficient, have greater impact and can better respond to the needs and demands of the poorest than vertical programmes. Yet, just as GAVI has demonstrated its proof of concept and is poised to introduce a second generation of life-saving vaccines in the developing world, we find ourselves in the midst of an international financial crisis and generally shrinking aid budgets, notwithstanding notable exceptions such as the UK Department for International Development and Australian Aid. GAVI is challenged to raise sufficient finance to sustain its necessary cruising altitude over the long term.2 Increasingly donor funds will be scrutinized for impact and value for money spent. GAVI is well placed to respond but is not complacent. GAVI has already tightened up on its financial control at the country level. Like the GFATM, GAVI has a zero tolerance for misuse of funds. But the trade off will be to strike a balance between country-driven management and accountability for results, with heavy top-down audit and control outside of national systems.
Resources will need to come from new and existing innovative financing mechanisms, private sector funding but most importantly direct funding from bilateral donors. Funds will need to be efficiently managed. Without sufficient resources children and adults (in the case of cervical cancer and hepatitis) will continue to die in large numbers from entirely preventable causes.
Acknowledgements
The views expressed in this paper are those of the author alone. Dr J.P. Lob-Levyt was CEO of GAVI until October 2010.
Endnote
UNICEF currently procures almost all vaccines on behalf of GAVI-supported countries.
Since the commissioning of this article in 2010, GAVI has successfully met its short to medium term funding targets at its 13 June 2011 London Pledging Conference, and witnessed a partial reduction in some vaccine prices from some companies.
References
- 1.Department for International Development 2011. Multilateral aid review. Ensuring maximum value for money for UK aid through multilateral organizations. See http://www.dfid.gov.uk/documents/publications1/mar/multilateral_aid_review.pdf
- 2.Lewis R., et al. 2008. Action for child survival: elimination of Haemophilus influenzae type b meningitis in Uganda. Bull. World Health Organ. 86, 241–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute for Health Metrics and Evaluation 2010. Financing global health 2010: development assistance and country spending in economic uncertainty. Seattle, WA: IHME.
- 4.CEPA LLP & Applied Strategies 2010. Second GAVI evaluation. See http://www.gavialliance.org/resources/GAVI_Second_Evaluation_Report_Final_13Sep2010.pdf