Abstract
Many observational coding schemes have been offered to measure communication in health care settings. These schemes fall short of capturing multiple functions of communication among providers, patients, and other participants. After a brief review of observational communication coding, the authors present a comprehensive scheme for coding communication that is (a) grounded in communication theory, (b) accounts for instrumental and relational communication, and (c) captures important contextual features with tailored coding templates: the Siminoff Communication Content & Affect Program (SCCAP). To test SCCAP reliability and validity, the authors coded data from two communication studies. The SCCAP provided reliable measurement of communication variables including tailored content areas and observer ratings of speaker immediacy, affiliation, confirmation, and disconfirmation behaviors.
Understanding communication processes in health care transactions is fundamental to advancing the understanding of how people access, obtain, and use health care services. At its core, communication in medicine is a goal-oriented process (Feldman-Stewart, Brundage, Tishelman, & Team, 2005; Hack, Degner, & Parker, 2005). Providers and patients use communication to learn about health-related risks, appraise possible changes in behavior, assess and take action about symptoms, and make decisions about treatment for illness. These interactions can be directly or indirectly influenced by illness severity, the presence of families or friends, and other sources of health information. They can occur between two individuals or include numerous participants. Consistent with much everyday communication, people experience health communication interactions as a rich process that reflects multiple goals, beliefs, attitudes, and preferences (Step & Finucane, 2002).
Development of tools for accurate measurement of communication is in its infancy. Many such tools are based on traditional linguistic structures and are primarily descriptive of verbal content during a consultation or interview (Cecil, 1998; Shaikh, Knobloch, & Stiles, 2001). Observational schemas have developed some complexity over the years, but few depict process-based explanations and predictions of outcomes. Process models of communication are fundamental to understanding interactional behaviors and outcomes because they can account for static and dynamic factors (Bales, 1976; Berger & Calabrese, 1975; L. E. Rogers & Escudero, 2004). These types of communication models include individual, joint, and situational contributions to communication transactions as they unfold.
An important feature of communication process perspectives is the idea that communicators, through verbal and nonverbal communication, can convey multiple layers of messages. Early communication theorists conceptualized this idea as the content and relational levels of communication (Watzlawick, Beavin, & Jackson, 1967). In this sense, communication can be understood as providing two streams of meaning: one that regards the denotative content of a message and another that reflects the affective tone, and therefore the relational quality of the interactants. An observational scheme that captures both these streams of meaning may reveal important relationship dynamics than that revealed by a single analytic approach.
This article describes a computerized program to facilitate the analysis of health care conversations, the Siminoff Communication Content and Affect Program (SCCAP). Because health transactions are widely variable in form and function, this new program is designed to be adaptable to the goals and patterns of diverse health care contexts. The SCCAP builds on other well-known observational systems but emphasizes verbal and nonverbal communication behaviors drawn from the communication research literature. Specifically, the program captures the following: (a) task-driven information exchange among multiple interaction partners, (b) the affective and relational communication activities of all communicators, and (c) the social-influence tactics used in health care settings that contribute to decision making. Data are reported from initial tests using two different health communication settings: tissue donation telephone requests and oncologist-cancer patient treatment decision making. These different health care contexts tested the flexibility and adaptability of the SCCAP to capture multiple health communication scenarios.
Existing Observer Communication Measurement Systems
Most methodologies designed for studying face-to-face interactions can be traced to interaction process analysis for observing small groups (Bales, 1976). On the basis of the assumption that interactions have identifiable regularities, Bales defined a standard set of categories along socioemotional tasks. These categories were further delineated as positive or negative communication activities, such as asking questions or antagonism. The interaction process analysis further used group communication theory to frame interaction, and subjective coding was rooted in the coder’s empathic ability.
The interaction process analysis provided a foundation for the Roter Interaction Analysis System, perhaps the most ubiquitous of communication coding schemes used in health communication research today (Roter & Larson, 2001). The system was designed to describe physician–patient interaction in terms of content and context of routine dialogue during medical care. General functions of the medical interview provide categories for coding physician–patient communication behavior. The first two categories, data gathering and educating/counseling, reflect general medical interview tasks. The second two categories, relationship building and partnership, are more affective in tone and reflect a broad conceptualization of nonverbal communication. This relational dimension of the Roter Interaction Analysis System accounts for a comparatively small segment of data and is often excluded from analyses or operationalized differently from study to study.
The Roter Interaction Analysis System has influenced the development of many communication coding schemes, including the SCCAP. Most of these offer twists on coding the content of the interaction but tend to minimize other communication functions. Gillotti, Thompson, and McNeilis (2002) used communication competence theory to create the Coordination and Competence System, which offers an approach to measuring participant responsiveness firmly grounded in conversational alignment. The Coordination and Competence System provides an excellent description of information exchange (i.e., “fit”), but stops short of capturing the affective component of relationship building. The Medical Interaction Process System accounts for some communicated affect via ratings of each utterance for “feeling” (Ford, Hall, Ratcliffe, & Fallowfield, 2000), but does not ground this activity in theoretical explanations of relational development. Dent, Brown, Dowsett, Tattersall, and Butow, (2005) revised an earlier coding scheme, the CN-LOGIT (Butow, Dunn, Tattersall, & Jones, 1995), to create the CanCode system, which includes ratings of discrete emotional content (e.g., anxious, sad) as well as various medical interview functions, similar to those in the Roter Interaction Analysis System. Although these coding systems are more descriptive of content than past coding schemes, these observational methods still lack systematic explanation and integration in the communication process.
One exception, an observational scheme developed by Street and colleagues, better captures the interrelationships of communication content and affect. This approach, similar to the Roter Interaction Analysis System, positions patient participation as a central mechanism for linking physician communication and measurable outcomes (Street, Gordon, Ward, Krupat, & Kravitz, 2005; Street & Millay, 2001). This coding scheme moves closer to fulfilling what Rimal described as “a typology of participation” (p. 96, Frankel, 2001).
We designed a program that adds to this approach by (a) using relational communication theory to conceptualize the affiliative function of communication; (b) using qualitative analysis to create tailored templates; (c) creating measures of patient participation that include content, behavior and affect dimensions; and (d) acknowledging the persuasive function of many health care communications. Further, the SCCAP provides assessment of the communication activity of family or caregivers directly within the structure of the medical interview. Most important, the SCCAP captures the dynamic nature of transactional communication by allowing specific content to be connected to verbal and nonverbal relational codes. The rich data provided by the SCCAP will enable researchers to make nuanced predictions of medical care outcomes affected by provider–patient communication.
Relational Communication in Health Communication Coding and SCCAP
Relational communication enables people to make affective interpersonal connections, yet few schemes allow for coding detailed affective information crucial to relationship development (Dillard, 1998; Duggan & Parrott, 2001; Jones & Guerrero, 2001; Mehrabian, 1972; Peters, Kipkus, & Diefenbach, 2006). Comprehensive coding of relational information depends heavily on coder nonverbal sensitivity, which is highly variable, often resulting in low intercoder reliability (Keeley-Dyreson, Burgoon, & Bailey, 1991). However, communication researchers have shown that coding single nonverbal cues (e.g., smile, eye contact) is less meaningful than coding clusters of cues that suggest an affective quality (e.g., affiliation, dominance) (D.B. Buller, Strzyzewski, & Hunsaker, 1991). The SCCAP was designed to provide a frame for all of these affective sources of information within a functional framework that can sequence interaction across a real-time process.
Further, coding systems should be able to adapt to the contextual and practical circumstances and conditions of the health criterion under study. For example, many interactions, particularly among older adults and those with life-threatening illness, occur within triads or even small family groups. Therefore, it is important for coding schemes to be able to be used with more than two interactants, a feature built into the SCCAP. In general, our aim for the SCCAP was to capture theoretically derived features of communication that have also been shown to be salient and relevant in health care settings. These include the ability to code (a) discrete content/task information, (b) relational and affective elements of interactions, and (c) tag data to speakers and specific communication functions.
Communication Theory Used to Construct the SCCAP
Using transactional communication models as a guide, we considered two primary domains, communication content and relationship messages, to reflect interrelated cognitive and affective processes operating in health care communication transactions. Content denotes generally agreed upon meanings in the shared (i.e., verbal) language of the interactants, and forms the instrumental or information exchange portion of the communication. The relational communication domain reflects identifiable affective qualities of interaction, embedded in verbal messages and nonverbal cues expressed by the interactants (Andersen, Guerrero, & Jones, 2006; J. K. Burgoon & Hale, 1987; J. K. Burgoon & Le Poire, 1999; Guerrero, Farinelli, & McEwan, 2009).
Although theorists have offered several perspectives of relational communication, we focused on confirmation, vocal immediacy, and the more global construct of affiliation as important communication indicators of relationship (Andersen, Guerrero, Buller, & Jorgensen, 1998; Jones & Guerrero, 2001; Kiesler & Auerbach, 2003; L. E. Rogers & Farace, 1975; Watzlawick et al., 1967; Wilmot, 1980). These constructs reflect relational qualities derived from interpersonal theory and validated by research. Further, these constructs can be observed and measured with vocalic cues associated with speech. First, confirmation theory is used to conceptualize verbal relational messages in the SCCAP.
Confirmation and Disconfirmation
Relational communication theorists define confirmation as the metacommunicative process through which a person’s self-definitions are accepted, acknowledged, or endorsed by others (Laing, Phillipson, & Lee, 1966; C. R. Rogers, 1957). Conversely, disconfirmation is the metacommunicative process by which a person’s self definitions are denied, avoided, or otherwise invalidated. Perceived confirmation and disconfirmation are experienced as psychological outcomes to certain types of messages and can influence the trajectory of the transaction (Cissna & Sieburg, 1981; Ruesch & Bateson, 1951; Watzlawick et al., 1967). Confirmation perceptions have been shown to predict relational satisfaction and trust (Beatty & Dobos, 1992; Weger & Metts, 2005). Using a previously validated typology as a guide, we listened to audiotapes of health care interactions and identified the following confirmation messages as especially salient to health care interactions: approval, reassurance, clarification, acknowledgement, shared laughter, apology, and offers of service (Sieburg, 1985). Disconfirmation elements included the following: ambiguity, indifference, tangents, irrelevancies, disparagement, and one-sided laughter.
Immediacy
Immediacy is a way of referencing the degree of psychological closeness expressed in a person’s communication with another (P. A. Andersen et al., 2006). Immediacy may be cued by vocal warmth, interpersonal touch, reduced physical distance, using a conversant’s name, or other person-centered references (Jones & Guerrero, 2001). These cues have been distinctly connected to relationship perceptions such as dominance, formality, and intimacy (J. K. Burgoon & Le Poire, 1999).
It follows that perceived immediacy appears to play an important role in the affective perceptions of communicative partners (Richmond & McCroskey, 2000). For example, relational outcomes such as perceived comforting, liking, and satisfaction have been attributed to higher levels of immediacy (Jones & Guerrero, 2001; Richmond, Heisel, Smith, & McCroskey, 2001). Immediacy has also been empirically linked to other, more task oriented communication outcomes including perceptions of communicative effectiveness, credibility, influence, and some forms of learning (Johnson & Miller, 2002; Witt, 2004; Witt, Wheeless, & Allen, 2004). Immediacy is operationalized in the SCCAP through observer perceptions of vocalic cues that indicate clear and inclusive speech. These cues signify connection, responsiveness, and inclusion.
Affiliation
Affiliation is widely recognized as a universal dimension of interpersonal behavior that has long been associated with health outcomes, particularly patient satisfaction (see Kiesler & Auerbach, 2003, for review). Affiliative behavior includes activities performed to gain friendship and prevent isolation, which is an important means of coping under stressful conditions (Wirth & Schultheiss, 2006). As a relational perception, affiliation reflects acceptance, nonjudgement, encouragement, and compassion (M. Buller & Buller, 1987; Garrity, 1981; Indvik & Fitzpatrick, 1986). Communicatively, this may be expressed nonverbally through a variety of cues (e.g., smiling, nodding, close distance), including vocalic features such as sympathetic or encouraging tone of voice (Kiesler & Auerbach, 2003). Affiliation is coded in SCCAP with a set of affective qualities that reflect a friendly and supportive tone of voice.
Social Influence
Interpersonal influence “involves the symbolic effort of preserving or creating thoughts, emotions, or behaviors in others” (p. 427, J. P. Dillard, Anderson, & Knobloch, 2002). Although much research exists about persuasive message production in general, less is available that pertains to social influence attempts in health care contexts. However, in either general or role specific contexts, the argument can be considered the fundamental unit of purposive speaking (Campbell, 1996).
Arguments generally consist of a proposition or are claim backed by some sort of evidence (e.g., statistical, anecdotal). Although arguments that feature statistical evidence are more powerful than anecdotal evidence in producing cognitive reactions and overall message processing, contemporary persuasion theory provides conditions for the effectiveness of both (Kopfman, Smith, Ah Yun, & Hodges, 1998; Petty & Cacioppo, 1986). These cognitive reactions can frequently be expressed in the form of counterargument, that is, a refutation to the original argument. Health care recipients do not always agree with clinician recommendations and this dynamic may reveal much about their shared interaction. Successful use of refutations can neutralize reservations or build resistance to recommendations (Boster, Levine, & Kazoleas, 1993; Kazoleas, 1993; Winkel & Huismans, 1986). SCCAP coding includes identification and description of persuasive arguments and any corresponding refutation from any speaker.
Another form of social influence is compliance gaining, that is, strategic social influence attempts that target a specific behavior change (Cody, Woelfel, & Jordan, 1983; Marwell & Schmitt, 1967). The SCCAP uses positive (e.g., esteem) and negative compliance messages (i.e., guilt) because of their specificity and potential relevance to a wide variety of medical interactions (Birkimer, Johnston, & Berry, 1993; Vangelisti, Daly, & Rudnick, 1991), and also codes for strategies that may be a function of the medical system (e.g., foot in the door), or strategies evidenced in previous research (e.g., threat; Birkimer et al.; D. B. Buller & Street, 1991; J. K. Burgoon et al., 1987; M. Burgoon et al., 1990; Dillard, 1991; Ferrari & Leippe, 1992; Klingle & Burgoon, 1995; Massi Lindsey, 2005; O’Keefe, 2002).
In general, SCCAP coding accounts for additional messages that occur in conjunction with task-defined instrumental content during medical communication transactions. This coding scheme fills previous gaps in observational medical interaction coding by integrating important relational and social-influence constructs within an empirically grounded explanation of communication processes. Figure 1 provides a schematic description of the SCCAP. Content themes represent categories of instrumental information relative to the visit while the observer ratings represent expressed affect that provides relational meaning. Communication types translate instrumental and relational meaning into communication acts that lead to hypothesized communication outcomes.
Figure 1.
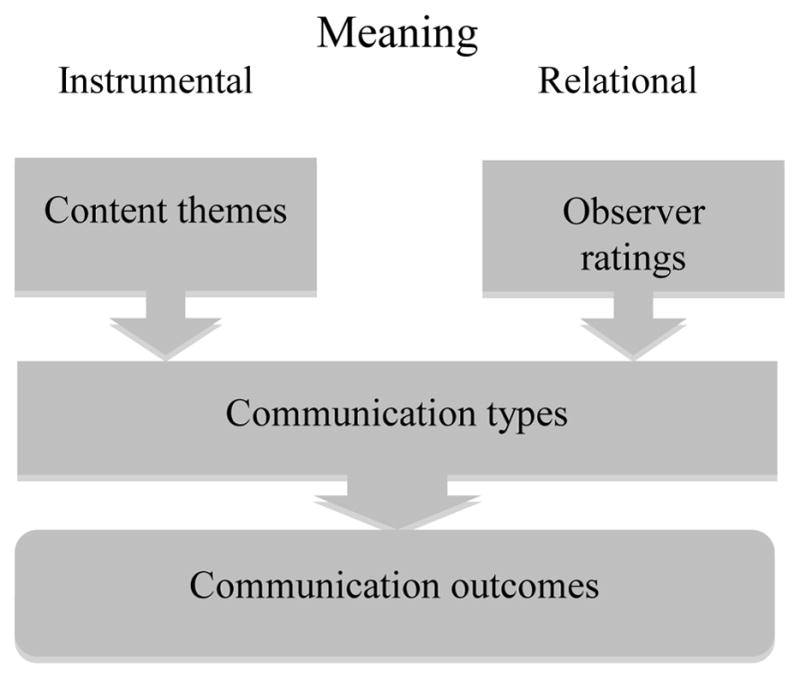
Schematic description of the Siminoff Communication Content & Affect Program.
Primary Elements and Development of the SCCAP Program
The SCCAP was initially developed as a paper and pencil instrument. Once this version was completed and tested, a computerized application was developed. The SCCAP application can be used across computer operating systems (Windows, Macintosh, and Linux). The program functions with a user-friendly point and click interface with drop down menus, text boxes, or counters.
SCCAP is an application designed to accomplish coding of verbal conversations from audio. The audio portion is not integrated into the SCCAP; the researcher listens to and uses his or her audio data directly from his or her own audio equipment. This is advantageous because transcription is costly and time consuming. Nevertheless, researchers can choose to transcribe and use the written transcription to aid in the coding process if they so choose. The SCCAP program is designed for audio only, rather than audio and video. Although nonverbal communication presents a multitude of observable cues audio retains nonverbal vocal inflections that impart meaning to the spoken words. Some researchers have argued that inclusion of kinesic information does not necessarily add significant explanatory power to coding only vocalic information (Dent et al., 2005) and that vocal cues are a more reliable and valid channel for coding nonverbal cues (DePaulo, Rosenthal, Eisenstat, Rogers, & Finkelstein, 1978; Haskard, DiMatteo, & Heritage, 2009). Other recent work (Penner et al., 2007; Riddle et al., 2002) has indicated that nonverbal, observable behaviors have much to add to an understanding of a particular communication. However, recording of nonverbal data requires videotaping, which is often expensive or impracticable. Therefore, to maximize feasibility, reliability, and coding parsimony, our version of SCCAP is audio only. The flexibility of the program is such that future versions could include additional nonverbal coding sections (e.g., kinesics).
The program opens and runs from a main menu that offers several coder activities. These reflect three general sets of data. The first set, content themes, includes those activities that constitute the task or instrumental aspect of most medical transactions (e.g., providing treatment information). Content themes are delineated into general categories and then further refined into discrete communication behaviors or events (e.g., discuss treatment, side effects). Coders click each event or activity as it occurs in the interaction and the program automatically records speaker, topic, message form (statement or question) and sequence. The unit of analysis that the SCCAP developers have used to test the program is an utterance, that is, the smallest definable unit of meaning. We trained all coders to identify an utterance with accuracy and calculated reliability scores on that basis. However, the idea of the SCCAP was to provide researchers with as much flexibility as possible. Researchers need to choose their own unit of speech analysis as dictated by their theoretical framework and research questions. A highly focused research question examining specific content might only code every instance of a specific content item. Conversely, a study taking a holistic or linguistic approach might need to code every utterance. Researchers can decide how much communication data they need and use the program to obtain their desired level of detail as long as the coding unit of analysis is clearly defined and the coding is consistent.
The second set consists of communication types. These are the aspects of communication that indicate relational information or influence attempts. Within this group are nested additional menus for recording question types. Content themes and communication types are coded at the same time. As the coder assigns a specific content theme to an utterance, she toggles to another coding screen that offers a menu of various communication types. After coding, communication types can be analyzed as discrete entities or by how they are associated with the content codes.
The third set consists of observer speech and affect ratings, including emotions (e.g., anger, sadness) and more composite affect (e.g., composure). Coders are trained to observe nonverbal vocalic cues likely to indicate affective qualities of interaction (Frijda, 1989). Speech ratings include those cues associated with the immediacy construct, such as speech rate and timber (Bradac, Bowers, & Courtright, 1979; Kearney, 1994). Coders rate each participant after listening to and coding content aspects of the interaction. Each of these primary data sets—content themes, communication types, and speech/affect ratings—are subsequently described in more detail.
Content Themes
Content themes reflect commonly occurring communication functions in most health interactions (Cole & Bird, 2000). The underlying assumption is that information exchange is a primary function of the interaction between providers and patients. Therefore, the utility of the program lies in being able to code exactly who exchanges what information, how frequently, and in what sequence. The content themes include introduction, purpose of visit, medical history, disease information, prognosis information, treatment information, clinical trials, logistics, preferences and values, psychosocial information, emotional, procedural directives, and closing. The program allows the researcher to add as many or as few sub-themes as desired under each content heading. Researchers may use all or only some of the content themes in the SCCAP program, depending on the health care context under study, the level of detail required or theoretical predictions. Table 1 defines each major content theme domain.
Table 1.
Siminoff Communication Content & Affect Program content themes
| Content theme | Coding definition |
|---|---|
| Introduction | Nonmedical talk in first moments of consult, light chat, greetings |
| Purpose | Stated or implied outcomes, objectives, or goals for the consult |
| Care logistics | How future medical tasks (e.g., treatment, imaging) will unfold, be performed, or take place |
| Disease | Talk of patient’s identified current or chronic disease, including disease specific symptoms |
| Treatment | Any aspect or type of disease treatment, including side effects, complementary and alternative medicine, no treatment |
| Preferences and values | Expression of any interactant’s opinions or attitudes about past, current, or future medical care |
| Procedures | Directives for progressing through current consult (e.g., physical exam) |
| Medical history | Review of past and current medical issues, family history, comorbidities, symptoms |
| Clinical trials | Describe, offer, discuss aspects of clinical trials |
| Psychosocial | Talk about lifestyle, work, cultural, spiritual, or economic issues; also, small talk that occurs after introduction |
| Emotional | Discussion or expression of emotional state, anxiety, gratitude, fears, frustrations |
| Prognosis | Discussion of future disease state or outcomes |
As the content themes are coded, the program logs each categorized utterance as it occurs in a real time sequence. Because of this ongoing sequencing, content themes are coded at the same time as the second primary group of variables, communication and question types. This approach is consistent with a transactional view of communication that recognizes simultaneous streams of content and relational communication during interactions.
Communication Types
The second coding group, communication types, encompasses those utterances that fulfill relational and social-influence functions of provider–patient communication. As the coder clicks content subtheme codes, he or she can also access a communication types menu from a sidebar on the screen. This menu offers options for confirming and disconfirming messages, arguments and refutations, and compliance strategies. Table 2 defines these relational message types.
Table 2.
Definitions of communication types
| Communication behavior | Definition | Example |
|---|---|---|
| Influence | ||
| Argument | Factual statements made in support of a desired goal, often accompanied by evidence | May indicate experience/expertise (from what I’ve seen …), reference to value system (best interest to …), inference from evidence (lab result indicates …). |
| Refutation | Discounting information to something that has been said | Factual responses offered by provider in order to dispel myth(s) held by patient. |
| Altruism | Reference to helping others, being unselfish, or generous to secure a course of action | “Future patients will benefit from your participation.” |
| Esteem | Referencing others’ positive perceptions if the interactant complies | “I’m sure your husband would be happy if you….” |
| Guilt | Point out negative consequences of thoughts or actions; includes drawing attention to an existing inconsistency or past expressed thought or action | “That’s not a healthy attitude to take. You said you were going to be optimistic.” |
| Foot in the door | Small request followed by a larger one | “As long as you’re willing to accept palliative relief, then we can discuss hospice.” |
| Threat | Statement indicating negative consequences if one does not follow the other’s recommendation | “If you don’t quit smoking, this is just going to get worse.” |
| Relational Confirmation | ||
| Approval | Message indicating that other is doing the correct thing | “That’s a good idea”; “I appreciate you[r] being straightforward.” |
| Reassurance | Supportive response directed to expressed fears, concerns, or anxiety | “It will be OK”; “Don’t worry, I have faith in you.” |
| Clarification | Statements repeated or paraphrased to ensure understanding | “I’m not sure what you mean. Can you explain some more?”; “So what you’re saying is …” |
| Acknowledgement | Statement that expresses normalcy of beliefs or behaviors | “Lots of people would feel that way.” |
| Concern | Recognition of the other’s emotional state or other psychosocial issue; the spirit of identification with another is present | “I know this has been a long process for you”; “I realize that these options may sound confusing.” |
| Laughter (+) | Jokes or moments of laughter shared by interactants | |
| Apology | Expression of regret or nonverbal indication of compassion | “I’m sorry you’re burdened by this”; “I’m sorry, I didn’t mean to upset you.” |
| Offer of service | Provider offers service, above and beyond the normal scope of responsibility | Provider calls or arranges for social work rather than have nurse do it. |
| Disconfirmation | ||
| Disapproval | Communicated rejection of other’s values, beliefs, thoughts, or opinions, including sarcastic or defensive statements | “No, I don’t want to discuss it”; “It’s too soon to discuss this”; “You can’t be serious.” |
| Ambiguity | Unclear expression with more than one possible meaning | “Well it is and it isn’t”; “I agree 100%, but I must say …” |
| Indifference | Failure to respond appropriately to the other’s message by disconnecting from the topic verbally or nonverbally | Talk-overs, prolonged silence, overelaboration, monologue that doesn’t stop even with interruption, side conversations with others |
| Tangential | Recognition of an incidental piece of the previous communication, but misses or disconnects from the other’s main intent | “Yes, that’s interesting but what I want to focus on …”; “Sure, sure, now lets talk about …”; “Mm-hmm, that reminds me that we need to discuss …” [new topic] |
| Irrelevant | Incomplete, loose, or rambling responses, or complete disconnection from topic or other’s version of events | Topic switch without explanation or recognition |
| Disparaging | Demeaning remark or put down that focuses on the person rather than message | “Don’t be silly”; “You’re making this harder than you need to …” |
| Laughter (−) | Jokes or moments of laughter that are nervous, derisory, not shared | |
Question forms are also embedded within the communication types section of the SCCAP. Questioning is a fundamental mode of active information seeking and is particularly important in health care conversations (Berger & Calabrese, 1975). Therefore, several question descriptors are available to indicate the function of a question (e.g., seek understanding, service), topic (e.g., economic, spiritual concerns), and whether the question was open- or closed ended. Questions can also be entered verbatim into a space provided for further analysis. Similar to other elements of the program, frequency and sequencing data for questioning is automatically calculated for each speaker during the course of the interview.
Observer Ratings
The third SCCAP coding group is the observer ratings section. These include third party observations of primarily nonverbal communication behaviors, such as vocal immediacy, composure, and expressed affect. Ratings are completed for as many health care providers, patients or others who contribute to the conversation. Immediacy cues include vocal expressiveness, speech rate, extemporaneous tone, vocal clarity, vocal encouragement, and inclusive pronoun use (e.g., we, our). Each item is rated on a scale of 1 to 7, with higher scores indicating optimum quantities.
Although research has identified a variety of communication skills specific to health transactions (e.g., questioning, listening, empathy), few focus on the qualitative features of communication that indicate closeness, warmth, and connection. These cues are fundamental to relationship development and have been associated with building rapport and increased patient disclosure and participation (Duggan & Parrott, 2001; Street et al., 2005; Zandbelt, Smets, Oort, Godried, & de Haies, 2007). Positive (i.e., compassionate, involved, sincere, friendly, animated, expressive) and negative (i.e., sadness, anger) emotion items relevant to health contexts were scaled 0–6, with high scores representing higher quantities of that emotion.
The observer rating section of the main menu concludes with menus that enable description of decisions made during the interaction. For each decision discussed, the coder provides verbatim transcription and indication of decision options, option clarity, chosen option, and option discussed most.
SCCAP Reliability and Validity
A first test of the SCCAP used conversational data obtained from 420 early stage breast cancer patients discussing adjuvant therapy decisions with their medical oncologists. The data was originally collected for a study of a decision aid (Siminoff, Gordon, Silverman, Budd, & Ravdin, 2006). Two coders were trained in SCCAP procedures and content categories as well as social influence and relational communication theory. This first coding attempt examined the ability of coders to reliably identify all utterances in these conversations. Reliability averaged .92 (range = .80 to .95) for conversations averaging 55 minutes each.
A second and more detailed examination of SCCAP was used to code communication in a sample of 1,200 requests for tissue from the families of deceased patients. The parent study was designed to understand how consent for tissue donation is obtained. Audiotapes of these conversations were obtained from 16 tissue banks in the United States and include next of kin who chose to donate as well as those who refused donation. Audiotapes were accessed after permission was obtained from deceased patients’ families. Five coders were originally trained to use the SCCAP application and reliability was assessed with a sample of 50 of the 1,200 audiotapes, randomly assigned to two coders who independently rated each audiotape.
The mean total number of utterances per consultation for Coder A was 177.30 (SD = 152.12), whereas the mean number for Coder B was 184.55 (SD = 152.70), Cronbach’s α =.998, p < .001. Interrater reliability for each content category, examining the tissue requester and next of kin utterances combined, ranged from 0.92 to 1.00 (see Table 3). For tissue requester communication, the interrater correlations ranged from 0.84 to 1.00. For next of kin communication, the interrater correlations ranged from 0.82 to 0.99. We also examined difference scores between Coder A and Coder B and these are presented in Table 4 and also indicate excellent interrater reliability.
Table 3.
Tissue donation study interrater correlations
| Major domain (# subtopics) | Tissue requester | Next of kin | Category |
|---|---|---|---|
| Introduces self | 0.97 | 0.95 | 0.99 |
| Intro topics | 0.93 | 0.91 | 0.94 |
| Today’s call | 0.98 | 0.96 | 0.97 |
| Donation decision | 0.84 | 0.82 | 0.93 |
| Tissues | 0.97 | 0.97 | 0.98 |
| Basic donation info | 0.98 | 0.98 | 0.98 |
| Consent form | 0.99 | 0.98 | 0.99 |
| Use of donated tissue | 0.98 | 0.95 | 0.98 |
| Psychosocial donation info | 0.97 | 0.97 | 0.97 |
| Medical history | 1.00 | 0.98 | 1.00 |
| Social history | 1.00 | 0.99 | 1.00 |
| Other | 0.92 | 0.90 | 0.92 |
Table 4.
Tissue donation study interrater difference scores of code frequency
| Tissue requester
|
Next of kin
|
|||
|---|---|---|---|---|
| Median | Range | Median | Range | |
| Introduces self | 1 | −3 to 3 | 0 | −3 to 1 |
| Intro topics | 0 | −9 to 2 | 0 | −2 to 6 |
| Today’s call | 0 | −4 to 8 | 0 | −7 to 5 |
| Donation decision | −4 | −14 to 0 | −2 | −10 to 0 |
| Tissues | −1 | −5 to 4 | 0 | −3 to 2 |
| Basic donation info | 0 | −9 to 14 | 0 | −9 to 11 |
| Consent form | 0 | −1 to 1 | 0 | 0 to 1 |
| Use of donated tissue | 0 | −6 to 4 | 0 | −2 to 4 |
| Psychosocial donation info | 0 | −12 to 3 | 0 | −12 to 5 |
| Medical history | 0 | −3 to 3 | 0 | −5 to 5 |
| Social history | 0 | −2 to 3 | 0 | −2 to 4 |
| Other | 1 | −5 to 9 | 1 | −5 to 10 |
Further examination of the SCCAP’s ability to enable prediction of an outcome of interest was conducted. Using all 1,200 coded tissue conversations, we tested predictors on family consent to tissue donation. As we originally hypothesized, we found that more requester affect was positively associated with consent to donation (31.1% vs. 29.1%; p < .001). Specifically, requesters who exhibited more involvement, sincerity, friendliness, and verbal expressiveness were more successful at obtaining consent to donation. Requesters who used disconfirmation were more likely to encounter family refusal of donation than consent (29.8% vs. 22.8%; p < .01). We also found that families were significantly more likely to consent when the requester did not cut off the family member when speaking (81.5% vs. 18.5%; p < .001) and when family members disclosed personal information about themselves (80.9% vs. 19.1%; p < .001).
Another test of the validity of the results obtained by SCCAP analysis was obtained by coding conversations between early stage breast cancer patients and their medical oncologists (Step, Rose, Albert, Cheruvu, & Siminoff, 2009). The sample consists of 39 oncologists, 180 patients, and 137 patient family members. Table 5 shows how much talk surrounded each function of the oncology interviews. Consistent with other health communication coding schemes (Frankel, 2001; Roter & Hall, 1993), medical management talk dominated the interaction. Also consistent with other studies (Frankel; Roter & Hall; Siminoff, Graham, & Gordon, 2006), oncologists talked more than patients about all topics with the exception of care logistics (i.e., how to get care). Psychosocial content (i.e., topics concerning, the patient’s lifestyle) and emotional topics were discussed but heavily dominated by oncologists.
Table 5.
Content category codes, by participant (N = 8,819)
| Content category | Oncologist (n = 39)
|
Patient (n = 180)
|
Family (n = 137)
|
Total
|
||||
|---|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | Frequency | % | |
| Introduction | 306 | 5.2 | 59 | 2.8 | 16 | 1.9 | 381 | 4.0 |
| Purpose | 17 | 0.4 | 9 | 0.3 | 1 | 0.1 | 27 | 0.3 |
| Care logistics | 314 | 5.3 | 579 | 27.8 | 239 | 29.3 | 1,132 | 12.8 |
| Disease | 672 | 11.3 | 307 | 12.0 | 99 | 12.1 | 1,078 | 12.2 |
| Treatment | 569 | 9.3 | 509 | 24.2 | 241 | 29.4 | 1,319 | 14.9 |
| Preferences and values | 270 | 4.5 | 133 | 6.3 | 47 | 5.7 | 450 | 5.0 |
| Procedures | 27 | 0.5 | 5 | 0.2 | 0 | 0 | 32 | 0.3 |
| Medical history | 2,616 | 44.2 | 159 | 7.5 | 44 | 5.3 | 2,819 | 31.9 |
| Clinical trials | 21 | 0.4 | 34 | 1.6 | 23 | 2.7 | 78 | 0.8 |
| Psychosocial | 803 | 13.7 | 98 | 4.1 | 37 | 4.4 | 938 | 10.6 |
| Emotion | 189 | 3.2 | 17 | 0.8 | 6 | 0.6 | 212 | 2.0 |
| Prognosis | 121 | 1.9 | 165 | 7.7 | 67 | 8.1 | 353 | 4.0 |
| Total | 5,925 | 67.2 | 2,074 | 23.5 | 820 | 9.3 | 8,819 | 98.8 |
Note. Percentages represent total for speaker.
Relational messages initiated by clinicians are shown in Table 6. Most relational messages occurred in the form of reassurance, followed by shared laughter and acknowledgement. Expressed empathy and disconfirming messages were infrequent. Disapproval was the most common disconfirming message followed by irrelevant or tangential comments. Confirming messages far outnumbered disconfirming messages and are characterized mainly by reassurance and acknowledgement of the patient’s expressed thoughts or feelings. Third-party observer ratings of clinicians indicated high fluency (M = 6.15, SD = 0.50) but low affiliation (M = 3.95, SD = 0.84).
Table 6.
Oncologist relational messages (n = 1245)
| Confirmation | Frequency (%) | Disconfirmation (n = 70) | Frequency (%) |
|---|---|---|---|
| Reassurance | 352 (28.3) | Disapproval | 28 (40.0) |
| Shared laughter | 294 (23.6) | Indifference | 10 (14.3) |
| Acknowledgement | 211 (16.9) | Irrelevant | 9 (12.9) |
| Approval | 180 (14.5) | Tangential | 8 (11.4) |
| Offer of service | 139 (11.2) | Disparagement | 7 (10.0) |
| Empathy | 57 (4.6) | Laughter (−) | 4 (5.7) |
| Repetition | 12 (1.0) | Ambiguous | 4 (5.7) |
Conclusions
Researchers across many disciplines have only begun to unpack the complexity of communication among clinicians, patients, and their families. Methodologies for analyzing clinician–patient communication should tap into the transactional nature of communication, combine qualitative and quantitative approaches, and adopt a contextual, or ecological approach to understanding the encounter. Moreover, no communication coding scheme explicitly differentiates between what is observed and what is relevant and important to the patient. For example, we have only begun to understand what types of communication, affectively and informationally, are important to patient decision making. Studies that use the SCCAP, like any other coding system, need to collect separate outcome data to assess this critically important outcome of communication research. The SCCAP is unique, however, because it is adaptive to multiple health communication contexts, which offers great flexibility to observational studies of health communication.
An important feature of the SCCAP is that it also offers measures of relational communication tied exclusively to communication theory. This provides a means of describing sequenced cognitive and affective communication behaviors that can be analyzed at individual, dyadic, or group levels. We are currently planning analysis of the location and sequence of confirming and disconfirming communication to explore those effects on consult duration and patient participation in patient-physician encounters. This will allow us to find out whether physicians’ consistent use of relational messages (i.e., across content domains) has the same effect on select patient outcomes as does strategic use of relational messages (i.e., in response to patient concerns).
Building any coding scheme is a challenging endeavor and this one is no exception. Although reliability is generally high, training to obtain adequate reliability is lengthy, generally 2–4 weeks. Researchers should consider training challenges carefully when designing content templates. Longer coder training will be required for more nuanced content templates. The SCCAP allows each element to be independently analyzed and researchers are free to tailor what parts of the programs are useful for their research question.
Another important caveat is the need to use large samples in order to control subject differences within clinician samples. Observation research in medical contexts typically features multiple patients for each clinician in the sample. It is important to offset potential errors by systematic random sampling of clinicians in multilevel designs or controlling for random effects of clinician communication styles in analyses. Future work should offer examples of how sequenced data can be used, as well as how SCCAP can be used to model more complex communication processes.
Clinician–patient communication transactions are at the heart of medical care. Observational coding of behavior is a vitally important method of capturing evidence-based social processes. It is crucial that health communication scholars use a more interdisciplinary body of research findings to inform measurement. The SCCAP coding program offers a means of capturing large amounts of interaction data that can be used to explain communication process and predict outcomes. More important, it is a theoretically grounded instrument capable of producing content and relational level data from all encounter participants. The SCCAP represents an advancement in our ability to observe and measure a broad spectrum of interactive behaviors that constitute health communication.
Acknowledgments
Results presented in this article are supported by a grant from the Agency for Healthcare Research and Quality, Understanding Consent to Tissue Donation (R01 HS-13152), Principal Investigator Laura A. Siminoff.
Contributor Information
LAURA A. SIMINOFF, Department of Social and Behavioral Health, Virginia Commonwealth University, Richmond, Virginia, USA
MARY M. STEP, Case Western Reserve University, Cleveland, Ohio, USA
References
- Andersen PA, Guerrero LK, Buller DB, Jorgensen PF. An empirical comparison of three theories of nonverbal immediacy exchange. Human Communication Research. 1998;24:501–535. [Google Scholar]
- Andersen PA, Guerrero LK, Jones SM. Nonverbal behavior in intimate interactions and intimate relationships. In: Manusov V, Patterson ML, editors. The Sage handbook of nonverbal communication. Thousand Oaks, CA: Sage; 2006. pp. 259–277. [Google Scholar]
- Bales RF. Interaction process analysis: A method for the study of small groups. Chicago: University of Chicago Press; 1976. [Google Scholar]
- Beatty MJ, Dobos JA. Relationship between sons’ perceptions of fathers’ messages and satisfaction in adult son–father relationships. The Southern Communication Journal. 1992;57:277–284. [Google Scholar]
- Berger CR, Calabrese RJ. Some explorations in initial interactions and beyond: Towards a developmental theory of interpersonal communication. Human Communication Research. 1975;1:99–112. [Google Scholar]
- Birkimer JC, Johnston PL, Berry MM. Guilt and help from friends: Variables related to healthy behavior. Journal of Social Psychology. 1993;133:683–692. doi: 10.1080/00224545.1993.9713923. [DOI] [PubMed] [Google Scholar]
- Boster FJ, Levine T, Kazoleas E. The impact of argumentativeness and verbal aggressiveness on strategic diversity and persistence in compliance-gaining behavior. Communication Quarterly. 1993;41:405–414. [Google Scholar]
- Bradac JJ, Bowers JW, Courtright JA. Three language variables in communication research: Intensity, immediacy, and diversity. Human Communication Research. 1979;5:257–269. [Google Scholar]
- Buller DB, Street RL., Jr The role of perceived affect and information in patients’ evaluations of health care and compliance decisions. Southern Communication Journal. 1991;56:230–237. [Google Scholar]
- Buller DB, Strzyzewski KD, Hunsaker FG. Interpersonal deception II: The inferiority of conversational participants as deception detectors. Communication Monographs. 1991;58:25–40. [Google Scholar]
- Buller M, Buller D. Physicians’ communication style and patient satisfaction. Journal of Health & Social Behavior. 1987;28:375–388. [PubMed] [Google Scholar]
- Burgoon JK, Hale JL. Validation and measurement of the fundamental themes of relational communication. Communication Monographs. 1987;54:19–41. [Google Scholar]
- Burgoon JK, Le Poire BA. Nonverbal cues and interpersonal judgments: Participant and observer perceptions of intimacy, dominance, composure, and formality. Communication Monographs. 1999;66:105–124. [Google Scholar]
- Burgoon JK, Pfau M, Parrott R, Birk T, Coker R, Burgoon M. Relational communication, satisfaction, compliance-gaining strategies, and compliance in communication between physicians and patients. Communication Monographs. 1987;54:307–324. [Google Scholar]
- Burgoon M, Parrott R, Burgoon JK, Birk T, Pfau M, Coker R. Primary care physicians’ selection of verbal compliance-gaining strategies. Health Communication. 1990;2:13–27. [Google Scholar]
- Butow PN, Dunn SM, Tattersall MHN, Jones QJ. Computer-based interaction analysis of the cancer consultation. British Journal of Cancer. 1995;71:1115–1121. doi: 10.1038/bjc.1995.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell KK. The rhetorical act. 2. Belmont, CA: Wadsworth; 1996. [Google Scholar]
- Cecil DW. Relational control patterns in physician–patient clinical encounters: Continuing the conversation. Health Communication. 1998;10:125–149. doi: 10.1207/s15327027hc1002_2. [DOI] [PubMed] [Google Scholar]
- Cissna KN, Sieburg E. Patterns of interactional confirmation and disconfirmation. In: Wilder-Mott C, Weakland J, editors. Rigor and imagination: Essays from the legacy of Gregory Bateson. New York: Praeger; 1981. pp. 253–282. [Google Scholar]
- Cody MJ, Woelfel ML, Jordan WJ. Dimensions of compliance-gaining situations. Human Communication Research. 1983;9:99–113. [Google Scholar]
- Cole SA, Bird J. The medical interview: The three-function approach. 2. St. Louis, MO: Mosby; 2000. [Google Scholar]
- Dent E, Brown R, Dowsett S, Tattersall M, Butow P. The cancode interaction analysis system in the oncological setting: Reliability and validity of video and audio tape coding. Patient Education & Counseling. 2005;56:35–44. doi: 10.1016/j.pec.2003.11.010. [DOI] [PubMed] [Google Scholar]
- DePaulo BM, Rosenthal R, Eisenstat RA, Rogers PL, Finkelstein S. Decoding discrepant nonverbal cues. Journal of Personality & Social Psychology. 1978;36:313–323. [Google Scholar]
- Dillard JP. The current status of research on sequential-request compliance techniques. Personality & Social Psychology Bulletin. 1991;17:283–288. [Google Scholar]
- Dillard JP. The role of affect in communication, biology, and social relationships. In: Andersen PA, Guerrero LK, editors. Handbook of communication and emotion: Research, theory, applications, and contexts. San Diego, CA: Academic Press; 1998. pp. xvii–xxxii. [Google Scholar]
- Dillard JP, Anderson J, Knobloch L. In: Interpersonal influence. 3. Knapp Mark L, Daly John A., editors. Thousand Oaks, CA: Sage; 2002. pp. 423–474. [Google Scholar]
- Duggan AP, Parrott RL. Physicians’ nonverbal rapport building and patients’ talk about the subjective component of illness. Human Communication Research. 2001;27:299–311. [Google Scholar]
- Feldman-Stewart D, Brundage MD, Tishelman C, Team SC. A conceptual framework for patient–professional communication: An application to the cancer context. Psycho-Oncology. 2005;14:801–811. doi: 10.1002/pon.950. [DOI] [PubMed] [Google Scholar]
- Ferrari JR, Leippe MR. Noncompliance with persuasive appeals for a prosocial, altruistic act: Blood donating. Journal of Applied Social Psychology. 1992;22:83–101. [Google Scholar]
- Ford S, Hall A, Ratcliffe D, Fallowfield L. The Medical Interaction Process System (MIPS): An instrument for analysing interviews of oncologists and patients with cancer. Social Science and Medicine. 2000;50:553–566. doi: 10.1016/s0277-9536(99)00308-1. [DOI] [PubMed] [Google Scholar]
- Frankel RM. Cracking the code: Theory and method in clinical communication analysis. Health Communication. 2001;13:101–110. doi: 10.1207/S15327027HC1301_09. [DOI] [PubMed] [Google Scholar]
- Frijda NH. The functions of emotional expression. In: Forgas JP, Innes JM, editors. Recent advances in social psychology: An international perspective. Amsterdam: Elsevier; 1989. pp. 205–217. [Google Scholar]
- Garrity T. Medical compliance and the clinician–patient relationship: A review. Social Science & Medicine. 1981;15:215–222. doi: 10.1016/0271-5384(81)90016-8. [DOI] [PubMed] [Google Scholar]
- Gillotti C, Thompson T, McNeilis K. Communicative competence in the delivery of bad news. Social Science and Medicine. 2002;54:1011–1023. doi: 10.1016/s0277-9536(01)00073-9. [DOI] [PubMed] [Google Scholar]
- Guerrero LK, Farinelli L, McEwan B. Attachment and relational satisfaction: The mediating effect of emotional communication. Communication Monographs. 2009;76:487–514. [Google Scholar]
- Hack TF, Degner LF, Parker PA. The communication goals of cancer patients: A review. Psycho-Oncology. 2005;14:831–845. doi: 10.1002/pon.949. [DOI] [PubMed] [Google Scholar]
- Haskard K, DiMatteo M, Heritage J. Affective and instrumental communication in primary care interactions: Predicting the satisfaction of nursing staff and patients. Health Communication. 2009;24:21–32. doi: 10.1080/10410230802606968. [DOI] [PubMed] [Google Scholar]
- Indvik J, Fitzpatrick M. Perceptions of inclusion, affiliation, and control in five interpersonal relationships. Communication Quarterly. 1986;34:1–13. [Google Scholar]
- Johnson SD, Miller AM. A cross-cultural study of immediacy, credibility and learning in the U.S. and Kenya. Communication Education. 2002;51:280–292. [Google Scholar]
- Jones SM, Guerrero LK. The effects of nonverbal immediacy and verbal person centeredness in the emotional support process. Human Communication Research. 2001;27:567–596. [Google Scholar]
- Kazoleas D. The impact of argumentativeness on resistance to persuasion. Human Communication Research. 1993;20:118–137. [Google Scholar]
- Kearney P. Verbal immediacy behaviors. In: Rubin R, Palmgreen P, Sypher H, editors. Communication research measures: A sourcebook. New York: Guilford Press; 1994. pp. 81–85. [Google Scholar]
- Keeley-Dyreson M, Burgoon JK, Bailey W. The effects of stress and gender on nonverbal decoding accuracy in kinesic and vocalic channels. Human Communication Research. 1991;17:584–605. [Google Scholar]
- Kiesler DJ, Auerbach SM. Integrating measurement of control and affiliation in studies of physician–patient interaction: The interpersonal circumplex. Social Science & Medicine. 2003;57:1707–1722. doi: 10.1016/s0277-9536(02)00558-0. [DOI] [PubMed] [Google Scholar]
- Klingle RS, Burgoon M. Patient compliance and satisfaction with physician influence attempts: A reinforcement expectancy approach to compliance-gaining over time. Communication Research. 1995;22:148–187. [Google Scholar]
- Kopfman JE, Smith SW, Ah Yun JK, Hodges A. Affective and cognitive reactions to narrative versus statistical evidence organ donation messages. Journal of Applied Communication Research. 1998;26:279–300. [Google Scholar]
- Laing RD, Phillipson H, Lee AR. Interpersonal perception: A theory and method of research. New York: Springer; 1966. [Google Scholar]
- Marwell G, Schmitt DR. Dimensions of compliance-gaining behavior: An empirical analysis. Sociometry. 1967;30:350–364. [Google Scholar]
- Massi Lindsey LL. Anticipated guilt as behavioral motivation: An examination of appeals to help unknown others through bone marrow donation. Human Communication Research. 2005;31:453–481. [Google Scholar]
- Mehrabian A. Nonverbal communication. Chicago: Aldine Atherton; 1972. [Google Scholar]
- O’Keefe DJ. Guilt as a mechanism of persuasion. In: Dillard JP, Pfau M, editors. The persuasion handbook: Developments in theory and practice. Thousand Oaks, CA: Sage; 2002. pp. 329–344. [Google Scholar]
- Penner L, Orom H, Albrecht T, Franks M, Foster T, Ruckdeschel J. Camera-related behaviors during video recorded medical interactions. Journal of Nonverbal Behavior. 2007;31:99–117. [Google Scholar]
- Peters E, Kipkus I, Diefenbach MA. The functions of affect in health communications and in the construciton of health preferences. Journal of Communication. 2006;56:S140–S162. [Google Scholar]
- Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 19. New York: Academic Press; 1986. pp. 123–205. [Google Scholar]
- Richmond VP, Heisel AD, Smith RS, McCroskey JC. Nonverbal immediacy in the physician/patient relationship. Communication Research Reports. 2001;18:211–216. [Google Scholar]
- Richmond VP, McCroskey JC. The impact of supervisor and subordinate immediacy on relational and organizational outcomes. Communication Monographs. 2000;67:85–95. [Google Scholar]
- Riddle D, Albrecht T, Coovert M, Penner L, Ruckdeschel J, Blanchard C, et al. Differences in audiotaped versus videotaped physician-patient interactions. Journal of Nonverbal Behavior. 2002;26:219–239. [Google Scholar]
- Rogers CR. The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting Psychology. 1957;21:95–103. doi: 10.1037/h0045357. [DOI] [PubMed] [Google Scholar]
- Rogers LE, Escudero V. Theoretical Foundations. In: Rogers LE, Escudero V, editors. Relational communication: An interactional perspective to the study of process and form. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 3–21. [Google Scholar]
- Rogers LE, Farace R. Analysis of relational communication in dyads: New measurement procedures. Human Communication Research. 1975;1:222–239. [Google Scholar]
- Roter DL, Hall JA. Doctors talking with patients/patients talking with doctors: Improving communication in medical visits. Westport, CT: Auburn House Paperback; 1993. [Google Scholar]
- Roter DL, Larson S. The relationship between residents’ and attending physicians’ communication during primary care visits: An illustrative use of the Roter Interaction Analysis System. Health Communication. 2001;13:33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- Ruesch J, Bateson G. Communication: The social matrix of society. New York: Norton; 1951. [Google Scholar]
- Shaikh A, Knobloch LM, Stiles WB. The use of a verbal response mode coding system in determining patient and physician roles in medical interviews. Health Communication. 2001;13:49–60. doi: 10.1207/S15327027HC1301_05. [DOI] [PubMed] [Google Scholar]
- Sieburg E. Family communication: An integrated systems approach. New York: Gardner Press; 1985. [Google Scholar]
- Siminoff LA, Graham G, Gordon N. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Education & Counseling. 2006;62:355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Gordon NH, Silverman P, Budd T, Ravdin PM. A decision aid to assist in adjuvant therapy choices for breast cancer. Psycho-Oncology. 2006;15:1001–1013. doi: 10.1002/pon.1040. [DOI] [PubMed] [Google Scholar]
- Step MM, Finucane MO. Interpersonal communication motives in everyday interactions. Communication Quarterly. 2002;50:93–109. [Google Scholar]
- Step MM, Rose JH, Albert JM, Cheruvu VK, Siminoff LA. Modeling patient-centered communication: Oncologist relational communication and patient communication involvement in breast cancer adjuvant therapy decision-making. Patient Education & Counseling. 2009;77:369–378. doi: 10.1016/j.pec.2009.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: Why some patients are more involved than others. Medical Care. 2005;43:960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Millay B. Analyzing patient participation in medical encounters. Health Communication. 2001;13:61–73. doi: 10.1207/S15327027HC1301_06. [DOI] [PubMed] [Google Scholar]
- Vangelisti AL, Daly JA, Rudnick JR. Making people feel guilty in conversations: Techniques and correlates. Human Communication Research. 1991;18:3–39. [Google Scholar]
- Watzlawick P, Beavin JH, Jackson DD. The pragmatics of human communication. New York: Norton; 1967. [Google Scholar]
- Weger H, Metts S. Disconfirming communication and self-verification in marriage: Associations among the demand/withdraw interaction pattern, feeling understood, and marital satisfaction. Journal of Social & Personal Relationships. 2005;22:19–31. [Google Scholar]
- Wilmot WW. Dyadic communication. 2. Reading, MA: Addison Wesley; 1980. [Google Scholar]
- Winkel FW, Huismans SE. Refutational messages on donor cards: A test of boomerang effects. Psychological Reports. 1986;59:899–910. [Google Scholar]
- Wirth M, Schultheiss O. Effects of affiliation arousal (hope of closeness) and affiliation stress (fear of rejection) on progesterone and cortisol. Hormones & Behavior. 2006;50:786–795. doi: 10.1016/j.yhbeh.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Witt PL. An initial examination of observed verbal immediacy and participants’ opinions of communication effectiveness in online group interaction. Journal of Online Behavior. 2004;2(2) Retrieved December 10, 2010 from http://www.behavior.net/JOB/v2n1/witt.html.
- Witt PL, Wheeless LR, Allen M. A meta-analytical review of the relationship between teacher immediacy and student learning. Communication Monographs. 2004;71:184–207. [Google Scholar]
- Zandbelt LC, Smets EM, Oort FJ, Godried MH, de Haies HC. Patient participation in the medical specialist encounter: Does physicians’ patient-centered communication matter? Patient Education & Counseling. 2007;65(3):309–406. doi: 10.1016/j.pec.2006.09.011. [DOI] [PubMed] [Google Scholar]


