Abstract
Background:
We assessed satisfaction and quality of life (QOL) in men with artificial urinary sphincter (AUS) placement.
Methods:
We identified 39 men who had AUS placement. A retrospective chart review was conducted. Validated questionnaires, including the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), Post-Operative Patient Global Impression of Improvement (PGI-I), Incontinence Impact Questionnaire-Short Form (IIQ-SF), and Urogenital Distress Index (UDI-SF), were used to measure patient-reported outcome. Global satisfaction was also assessed.
Results:
At chart review, 34 of 39 questionnaires were assessed for QOL, satisfaction and surgical outcome. Follow-up ranged from 7 to 60 months (median = 24 months). Surgical revisions were required in 6 (17.6%) patients due to infection (1), erosion (1), combined infection and erosion (1), device failure (1) and second cuff placement (2). Quality of life was assessed using the IIQ-SF and UDI-SF, with mean scores of 15.4 and 24.8, respectively; these scores indicated a low negative impact on QOL. The ICIQ-SF mean score was 8.2, well below the worst possible score. The number of men using more than 1 pad per day dropped from 27 preoperatively to 10 postoperatively. Most patients (31/34) described their urinary condition as better, 2 had no change and 1 was worse. Most patients (31/34, 91.2%) would be willing to undergo the procedure again, 2 were undecided, and 1 would not. Similarly, 28 patients (82.4%) would recommend the procedure to a friend, 3 respondents would “with reservation,” 1 respondent was undecided, and 2 would not recommend the AUS placement.
Conclusion:
Treatment of urinary incontinence with the AUS has a positive effect on QOL with high patient satisfaction and reasonably low complication rates.
Introduction
Quality of life (QOL) considerations are integral to the treatment of stress urinary incontinence (SUI) in men. While SUI in men cannot be attributed to any one cause, the condition arises predominantly in patients who have undergone radical prostatectomy. In post-prostatectomy patients, SUI has an incidence of 8% to 77%.1 In 2% to 33% of affected men, symptoms persist for more than 12 months causing up to 10% of this subset to seek surgical intervention.2 Overall, leakage affects QOL enough to prompt 8% to 15% of patients suffering from post-prostatectomy incontinence to seek some form of treatment.3
Available surgical options for the treatment of SUI include injectables, adjustable balloon therapy, slings, and the artificial urinary sphincter (AUS); the AUS is considered the gold standard for treatment.
The AUS is regarded for its particularly high success rates, ranging from 59% to 90%, where success is defined as a continence status of 0 to 1 pads per day.4 While revision rates in the literature appear to be variable (between 17% and 32%), the durability of the AUS has been favourably measured by a “5-year revision-free rate” of 75%, as well as a “probability of device use for 9 years” of 84%.4
The AUS has also been associated with high patient satisfaction and a positive impact on health-related QOL. In the literature, satisfaction rates range from 87% to 90%, remaining high even in the setting of incomplete continence.4
Our study seeks to assess QOL and patient satisfaction in men who received AUS placement for the treatment of SUI at our specific institution.
Methods
Thirty-nine men who had undergone AUS placement at our institution between 2003 and 2008 were identified and asked to self-assess their postoperative QOL. The corresponding demographic and surgical information for these patients was obtained through a retrospective chart review.
To facilitate accurate assessment by patients, we used self-assessment instruments that have been validated in existing studies and amalgamated them into a patient survey (Appendix 1). This survey consisted of 4 existing instruments, the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), Post-Operative Patient Global Impression of Improvement (PGI-I), Incontinence Impact Questionnaire-Short Form (IIQ-SF) and Urogenital Distress Index (UDI-SF).
In addition to assessing QOL, the patient survey measured patient satisfaction with AUS by incorporating an additional set of questions.5 Our survey also sought to determine the extent of protection required by patients against urinary leakage both before and after their procedure.
Beyond efforts to eliminate researcher bias, the survey was designed to be brief (32 questions) and simple to minimize errors stemming from low patient compliance.
Results
Of the 39 questionnaires mailed out, 3 were not returned, 2 were returned incomplete (wrong address) and 34 were returned completed. The ages of the men who responded ranged from 35 to 87, with a mean age of 70.6. The time of follow-up ranged from 7 to 60 months, with a median time of 24.0 months.
Of the 34 men who responded, most were incontinent as a result of undergoing radical prostatectomy with or without radiation (Table 1).
Table 1.
Causes of stress urinary incontinence amongst men in our study population
| Cause | n |
|---|---|
| Radical prostatectomy alone | 24 |
| Radical prostatectomy plus radiation | 6 |
| Radiation plus salvage cryotherapy | 2 |
| Radiation alone | 1 |
| Pelvic fracture | 1 |
| Total | 34 |
Revisions
The overall revision rate was 17.6% (6/34). Complications leading to revision included infection (1), erosion (1), or both (1), as well as device failure (1) (Table 2). Infections occurred 2 to 3 months postoperatively. A second cuff was implanted in 2 patients who were dissatisfied with their level of continence, despite having a well-functioning device and significant improvement from baseline.
Table 2.
Revisions following initial artificial urinary sphincter placement
| Our series (n=34) | In the literature4 | |
|---|---|---|
| Overall | 6 (17.6%) | 8–45% |
| Infection and erosion | 3 (8.8%) | <8% |
| Infection | 1 (2.9%) | |
| Erosion | 1 (2.9%) | |
| Infection + erosion | 1 (2.9%) | |
| Device failure | 1 (2.9%) | 0–53% |
| Second cuff placement | 2 (5.9%) | 3–9% |
All 34 men evaluated in this study had functioning devices at the time of reporting.
Quality of life
The QOL tools used included the ICIQ-SF, IIQ-SF, UDI-SF, and the PGI-I.
Possible ICIQ-SF scores range from 0 to 21, with 0 corresponding to the least possible negative impact on QOL, and 21 being the greatest.6 The median score among our patients at a median follow-up of 24 months was 7.0, indicating a low impact on QOL.
The IIQ-SF and UDI-SF scores range from 0 to 100, and again lower scores correspond with better QOL, while higher scores indicate worse QOL.7 The mean scores for the IIQ-SF and UDI-SF were 15.4 and 24.8, respectively.
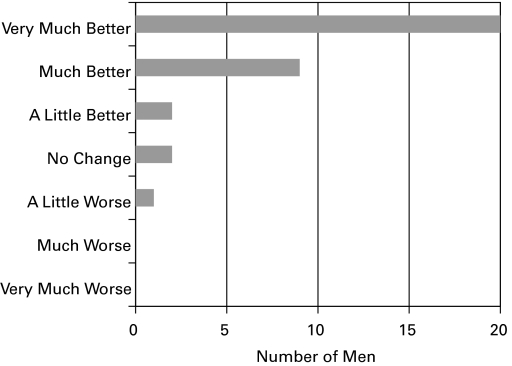
The PGI-I questionnaire data indicate that most patients felt that their urinary condition had changed in a positive manner after the AUS placement (Fig. 1). Among the subset of men requiring a surgical revision, all 6 reported that their urinary condition had improved; 5 out of 6 felt their condition was “very much better” after surgery, and the remaining patient responded that his condition was “much better” following the procedure.
Fig. 1.
Perception of urinary condition amongst men post-artificial urinary sphincter placement.
Patient satisfaction
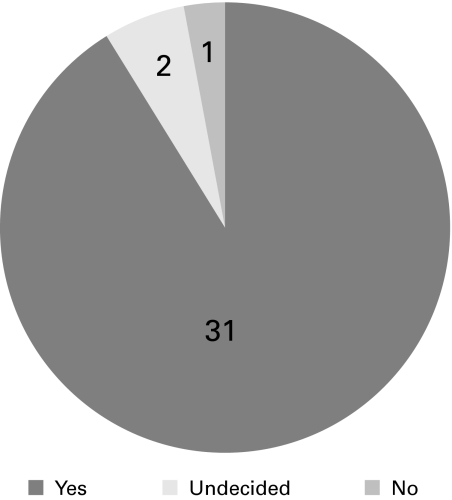
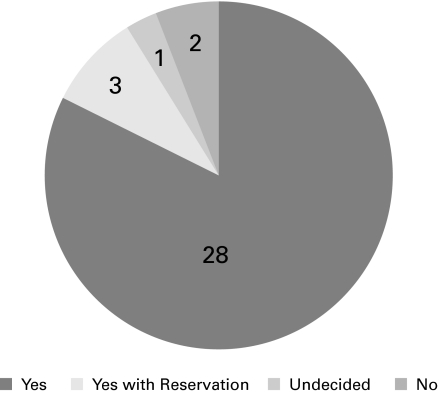
Most patients (31/34) stated that they would have an AUS placed again, knowing what they know now (Fig. 2). Furthermore, most patients (31/34, 91.2%) would recommend the AUS to a friend with the same problem (Fig. 3). Of the 6 men who required revisions, 5 replied that they would be willing to undergo AUS placement again, while 1 would not. Similarly, 5 out of the 6 responded that they would recommend the procedure to a friend, whereas 1 said he would not.
Fig. 2.
Answers to the question: “Knowing what you know now, would you have an artificial urinary sphincter placement again?”
Fig. 3.
Answers to the question: “Would you recommend the artificial urinary sphincter to a friend?”
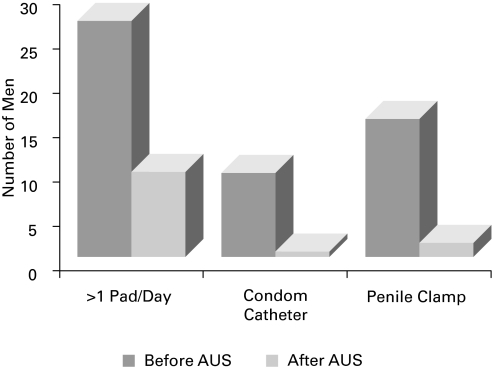
Use of protection against leakage
There is a significant decrease in the usage of all forms of protection against urinary leakage after AUS placement in our study group (Fig. 4).
Fig. 4.
Use of protection against leakage before and after artificial urinary sphincter insertion.
Discussion
The purpose of our study was to determine the effect of the AUS on the QOL of male patients suffering from SUI. We used 4 validated instruments: the IIQ-SF, ICIQ-SF, UDI-SF, and PGI-I. Of these instruments, the ICIQ-SF and the PGI-I have been validated for use in men in particular.8 The UDI-SF and the IIQ-SF were originally validated for use in women.7 Although the validity and reliability of the UDI-SF has not been assessed in men, the IIQ-SF has been tested in men and has demonstrated some validity.9 Regardless, the UDI-SF and the IIQ-SF have been used in the literature to assess QOL in men with incontinence.10,11,12
Although the validity of the each of the 4 instruments used in our survey has been separately established, the validity of using all of them as part of a larger comprehensive survey has not. We cannot accurately predict whether the assimilation of the questionnaires might have affected the individual results, and the literature is lacking to guide us in this regard. To preserve the validity of each instrument to the best of our ability, we designed our survey to maintain the integrity of each individual instrument by keeping it intact and administering it in full. Therefore, no additions or omissions were made, and all questions comprising each instrument were maintained in the order in which they had been originally validated. The results of each instrument were then tabulated separately as described in their original studies. By delivering our survey in this manner, we believe we were able to minimize any potential negative effects on validity.
Our study is limited by its retrospective nature, which may introduce recall bias among participants. Furthermore, preoperative QOL scores from our study population were not available for comparison to postoperative values, which limits our ability to directly determine the impact of treatment.
The IIQ-SF and UDI-SF have been used in other studies to quantify QOL in men with SUI. Haab and colleagues administered questionnaires, including the IIQ-SF and UDI-SF, to 15 patients with pure SUI after prostatectomy who were awaiting AUS insertion to act as the control group.10 The mean scores for this control group on the IIQ-SF and UDI-SF were 83 and 85, respectively. The authors compared the results of the control group to those of the study population (n = 68) and found a statistically significant difference between the 2 groups; QOL and distress, due to incontinence, were less affected in the treatment group.10 Postoperative scores on both tools reported by Haab and colleagues were comparable to scores we obtained in our patient population. Fleshner and Herschorn similarly compared the results of the IIQ-SF in patients who had undergone AUS insertion versus patients who had incontinence post-radical prostatectomy but no treatment, and also found that incontinence had a lesser impact on the patients who had received treatment by way of AUS insertion.11 O’Connor and colleagues administered both tools preoperatively and postoperatively to patients post-radical cystectomy and orthotopic neobladder and also found a statistically significant decrease in patients’ scores following AUS implantation.12
Since we were unable to make a direct comparison between preoperative and postoperative IIQ-SF and UDI-SF scores in our study cohort, we used the PGI-I question to assess how patients had felt their condition had changed postoperatively. Most of our patients felt that their condition had improved as a result of AUS implantation, with 29/34 (85.3%) reporting that they were “very much better” or “much better” after surgery.
The ICIQ-SF data collected from our patients further indicated that the impact of incontinence following AUS insertion was relatively small. Unfortunately, no other studies looking at QOL and AUS have used this particular tool. As a result, there are no values for comparison, and no way to quantify the change in symptoms postoperatively.
Along with considering QOL, we also were interested in assessing patient satisfaction with the device, and whether or not satisfaction was affected by the need for surgical revisions. Rates of satisfaction in our series were very high. More than 90% of patients were willing to undergo the procedure again and were willing to recommend the procedure to a friend. This is similar to the results reported by Litwiller and colleagues and slightly higher than what was reported by Haab and colleagues.5,10 Our revision rates were similar to those reported elsewhere in the literature.4 Our data demonstrated high satisfaction rates even among men requiring surgical revisions, most men reported feeling better off than they were prior to surgery and were satisfied overall.
Lastly, we attempted to quantify the improvement in continence by inquiring about protection usage. We noted that there was a decrease in the need for protection usage across all types of protection (pads, penile clamp, and condom catheters). Other studies have defined social continence or ‘success’ of the procedure as the need for protection not exceeding 1 pad per day.4,10 The most common form of protection used by our study cohort was pads, and the number of men using >1 pad per day prior to surgery dropped significantly. Postoperatively, only 29.4% of men were using >1 pad per day, meaning that 70.6% of men in our study achieved continence based on this definition. While the recording pad use as a determinant of continence suffers from the wide variability in pad types and individual behaviour, the observed changes in usage in our study points to a significant positive impact of AUS placement.
Conclusion
Insertion of the AUS has a strong positive impact on the QOL of men with SUI. We also observed high satisfaction rates with the procedure, even in men requiring revisions. Revision rates in this series are similar to those reported in the literature.
Appendix 1. Quality of life questionnaire
Questions 1–3 pertain to symptoms prior to artificial urinary sphincter (AUS) implantation, 4–32 pertain to symptoms after AUS implantation
|
(Responses for questions 14–26: not at all, slightly, moderately, greatly)Has urine leakage affected your ...
|
Footnotes
This paper has been peer-reviewed.
Competing interests: None declared.
References
- 1.Klinger HC, Marberger M. Incontinence after radical prostatectomy: surgical treatment options. Curr Opin Urol. 2006;16:60–4. doi: 10.1097/01.mou.0000193381.93608.dc. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Litt ER, Ballert KN, et al. Artificial urinary sphincter versus male sling for post-prostatectomy incontinence – what do patients choose? J Urol. 2009;181:1231–5. doi: 10.1016/j.juro.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 3.Comiter CV. Surgery insight: surgical management of postprostatectomy incontinence – the artificial urinary sphincter and male sling. Nat Clin Pract Urol. 2007;4:615–24. doi: 10.1038/ncpuro0935. [DOI] [PubMed] [Google Scholar]
- 4.Herschorn S. The artificial urinary sphincter is the treatment of choice for post-radical prostatectomy incontinence. Can Urol Assoc J. 2008;2:536–9. doi: 10.5489/cuaj.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Litwiller SE, Min KB, Fone PD, et al. Post-prostatectomy incontinence and the artificial urinary sphincter: a long-term study of patient satisfaction and criteria for success. J Urol. 1996;156:1975–80. doi: 10.1016/s0022-5347(01)65408-9. [DOI] [PubMed] [Google Scholar]
- 6.Avery K, Donovan J, Peters TJ, et al. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- 7.Uebersax JS, Wyman JF, Shumaker SA, et al. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodyn. 1995;14:131–9. doi: 10.1002/nau.1930140206. [DOI] [PubMed] [Google Scholar]
- 8.Twiss CO, Fischer MC, Nitti VW. Comparison between reduction in 24-hour pad weight, international consultation on incontinence-short form (ICIQ-SF) score, international prostate symptom score (IPSS), and post-operative patient global impression of improvement (PGI-I) score in patient evaluation after male perineal sling. Neurourol Urodyn. 2007;26:8–13. doi: 10.1002/nau.20333. [DOI] [PubMed] [Google Scholar]
- 9.Moore KN, Jensen L. Testing of the incontinence impact questionnaire (IIQ-7) with men after radical prostatectomy. J Wound Ostomy Continence Nurs. 2000;27:304–12. doi: 10.1067/mjw.2000.110623. [DOI] [PubMed] [Google Scholar]
- 10.Haab F, Trockman BA, Zimmern PE, et al. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of followup. J Urol. 1997;158:435–9. [PubMed] [Google Scholar]
- 11.Fleshner N, Herschorn S. The artificial urinary sphincter for post-radical prostatectomy incontinence: impact on urinary symptoms and quality of life. J Urol. 1996;155:1260–4. [PubMed] [Google Scholar]
- 12.O’Connor RC, Kuznetsov DD, Patel RV, et al. Artificial urinary sphincter placement in men after cystectomy with orthotopic ileal neobladder: continence, complications, and quality of life. Urology. 2002;59:542–5. doi: 10.1016/s0090-4295(01)01655-7. [DOI] [PubMed] [Google Scholar]