Abstract
Non-Hodgkin lymphoblastic lymphomas are very uncommon tumors that rarely involve the heart; however, when they do, they typically cause cardiac symptoms. Herein, we describe the case of a young woman who presented with respiratory symptoms. These were caused by a high-grade lymphoblastic lymphoma, which originated in the left inferior pulmonary vein and extended into the left atrium. The tumor was surgically debulked, but it recurred in 1 month, and the patient underwent chemotherapy. Six months later, she had recurrent respiratory symptoms, and echocardiography revealed a persistent mass in the left lower lobar vein. A modified chemotherapy regimen led to complete resolution of the tumor within 2 months. We are unaware of other reports of a primary cardiac non-Hodgkin lymphoblastic lymphoma with this unusual site of origin and rare manifestation of symptoms.
Key words: Antineoplastic combined chemotherapy protocols/therapeutic use; cardiac surgical procedures; chemotherapy, adjuvant; heart atria/pathology; heart neoplasms/complications/diagnosis/drug therapy/pathology; leukemia-lymphoma, adult T-cell/pathology; lymphoma, non-Hodgkin; neoplasm recurrence/local; precursor cell lymphoblastic leukemia-lymphoma/diagnosis/therapy; treatment outcome
Only 1.3% of all primary cardiac tumors are lymphomas.1 Lymphoblastic lymphomas are very rare and constitute approximately 2% of all non-Hodgkin lymphomas.1,2 Lymphoblastic lymphomas typically affect the lymph nodes and rarely involve the heart. Herein, we report the diagnosis and treatment of a primary cardiac lymphoblastic lymphoma that caused respiratory symptoms in an adult woman.
Case Report
In April 2008, a 28-year-old woman presented with a history of exertional dyspnea, a cough of 3 weeks' duration, and sudden-onset hemoptysis. She had no history of angina pectoris. On examination, she was pale, cachexic, hypotensive, and tachycardic, and her superficial thoracic veins were dilated. Chest radiography revealed pericardial effusion and bilateral pleural effusion. Transthoracic echocardiography showed adequate biventricular function, mild mitral regurgitation, moderate-to-severe pericardial effusion, and an intracardiac mass on the posterior left atrial wall. Transesophageal echocardiography showed a 4 × 3-cm left atrial mass that obstructed the pulmonary venous blood flow (Fig. 1). Because of the patient's hemodynamic instability, she was scheduled for emergency cardiac surgery.
Fig. 1 Preoperative transesophageal echocardiography shows a large intracardiac mass (arrow) on the posterior left atrial wall.
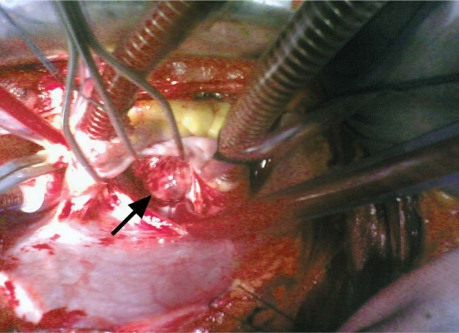
Through a median sternotomy, the pericardial and pleural effusions were drained and sent for cytologic analysis. Cardiopulmonary bypass was started. After a left atriotomy was performed, a large, noncapsulated, multilobular mass was seen in the posterior left atrial cavity (Fig. 2). The mass appeared to originate within the left inferior pulmonary vein (PV), and it occluded and extended into the lumen of that vessel. This also resulted in obstruction of the left superior PV orifice. The right PVs were not involved.
Fig. 2 Photograph during left atriotomy shows a large, noncapsulated, multilobular mass (arrow) in the left atrial cavity.
Because of tumor friability and the luminal invasion of the left inferior PV, en bloc excision was not feasible. The left atrial mass was debulked and sent for histopathologic analysis. Water testing of the mitral valve revealed minimal regurgitation. The left atrial cavity was thoroughly washed, the atriotomy was closed, and the patient was smoothly weaned from cardiopulmonary bypass. Postoperative echocardiography revealed trivial mitral regurgitation and no residual mass in the left atrium. The patient's recovery was uneventful, and she was discharged from the hospital on the 4th postoperative day.
Histopathologic analysis confirmed that the mass was a high-grade lymphoblastic lymphoma with marked anaplastic features, showing hypercellular lymphoblasts with a predominant T-cell phenotype (CD7+, CD3+). These were rich in intermediate-sized hyperchromatic nuclei with inconspicuous nucleoli and increased mitotic figures (Fig. 3). In 1 month, thoracoabdominal computed tomography revealed a residual mass in the patient's left lower lobar vein. The mass extended into the posterolateral aspect of the left atrium and constricted the adjacent left lower lobar bronchus, with consolidation and atelectasis of the left lateral basal segments. Residual inferior tracheobronchial and right basal epicardial nodes were seen. No abdominal pathologic condition was evident. The patient began a chemotherapy regimen of 6 cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone. Six months later, she had recurrent cough, dyspnea, and hemoptysis. Echocardiography revealed a persistent mass in the left lower lobar vein. Modification of the chemotherapy to a 6-cycle regimen of ifosfamide, carboplatin, and etopocide led to complete tumor resolution within 2 months, as confirmed on computed tomography.
Fig. 3 Photomicrograph of the left atrial mass shows hypercellularity of the lymphoblasts, which were rich in intermediate-sized hyperchromatic nuclei with inconspicuous nucleoli and increased mitotic figures (H & E, orig. ×200).
Discussion
To our knowledge, there have been no other reports of an intracardiac non-Hodgkin lymphoblastic lymphoma with this site of origin and presentation of symptoms. Most patients with primary cardiac lymphomas present with cardiac manifestations,3,4 but our patient had primarily respiratory symptoms. This could be attributed to the tumor's unusual origin within the left inferior PV and extension into the left atrium, which led to compression of the adjacent left lower lobar bronchus, pulmonary congestion, and a marked reduction in pulmonary venous return.
Despite surgical debulking of the tumor, it recurred within 1 month. This establishes the aggressiveness and high potential for recurrence of a lymphoblastic lymphoma, especially when treated only by surgical debulking or excision. Although chemotherapy is the main treatment for lymphomas,5 emergent surgical debulking was warranted in our patient, because the large intracardiac mass of unknown type was obstructing pulmonary venous blood flow and causing hemodynamic instability. Postoperative chemotherapy led to complete tumor resolution, which cannot be expected after surgical treatment alone.
Strong suspicion that leads to the early diagnosis of lymphoblastic lymphomas, along with combined surgical and chemotherapeutic treatments, can help in better managing these rare cardiac tumors.
Footnotes
Address for reprints: Amir Mohamed, MD, MSc, Department of Cardiovascular Surgery, Alexandria University, Alexandria 21526, Egypt
E-mail: amigo_cts@yahoo.com
References
- 1.Burke A, Virmani R. Tumors of the heart and great vessels. Fascicle 16, 3rd series. In: Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology; 1996.
- 2.Sweetenham JW, Borowicz M. Lymphoblastic lymphoma. In: Mauch PM, Armitage JO, Coiffier B, Dalla-Favera R, Harris NL, editors. Non-Hodgkin's lymphomas. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 503–13.
- 3.Nascimento AF, Winters GL, Pinkus GS. Primary cardiac lymphoma: clinical, histologic, immunophenotypic, and genotypic features of 5 cases of a rare disorder. Am J Surg Pathol 2007;31(9):1344–50. [DOI] [PubMed]
- 4.Bagwan IN, Desai S, Wotherspoon A, Sheppard MN. Unusual presentation of primary cardiac lymphoma. Interact Cardiovasc Thorac Surg 2009;9(1):127–9. [DOI] [PubMed]
- 5.Sweetenham JW. Treatment of lymphoblastic lymphoma in adults. Oncology (Williston Park) 2009;23(12):1015–20. [PubMed]