Abstract
The purpose of this retrospective study was to analyze our experience with mediastinal cysts, emphasizing the clinical presentations and results of surgery.
Thirty-two patients with mediastinal cysts underwent surgery from January 2000 through June 2005. The records of these patients were reviewed for age at presentation, sex, signs and symptoms at presentation, results of the imaging techniques, types of mediastinal cysts, location and size of cysts, types of surgical procedure, length of hospital stay, early postoperative complications, death, and other follow-up information.
The 32 mediastinal cysts comprised 12 bronchogenic, 9 pericardial, 7 thymic, and 2 enteric cysts, together with 2 cystic teratomas. Overall, 14 of the 32 patients with mediastinal cysts were asymptomatic. The surgical approach was thoracotomy in 30 patients and median sternotomy in 2 patients. The mean length of hospital stay was 7.7 ± 2.6 days. All patients were free from recurrence during the mean follow-up period of 4.4 ± 3.3 years.
Surgery for mediastinal cysts is associated with low morbidity and mortality rates and a very low recurrence rate. It offers a definitive diagnosis and cure, avoiding the higher morbidity and mortality risks associated with conservative observation.
Key words: Bronchogenic cyst, mediastinal cyst/complications/diagnosis/radiography/surgery, outcomes, retrospective studies
Cystic lesions of the mediastinum are uncommon, comprising 12% to 18% of all primary mediastinal tumors.1 Unless they attain a large size and cause compressive symptoms, these tumors are generally asymptomatic and are discovered incidentally upon radiologic investigation of some other condition. They are particularly significant because of the difficulty in making a differential diagnosis: they can simulate multiple lesions, both benign and malignant. There is still no consensus on whether the best approach to treatment for mediastinal cysts is a conservative medical one (particularly in application to pericardial and bronchogenic cysts) or a surgical approach.2–4 The objectives of this study were to review the clinical presentations and the results of surgery in patients with mediastinal cysts.
Patients and Methods
The medical records of 32 patients with mediastinal cysts who underwent surgery from January 2000 through June 2005 were studied retrospectively. The records of these cases were analyzed for age, sex, signs and symptoms at presentation, results of the imaging techniques, type of mediastinal cyst, location and size of cyst, type of surgical procedure, length of hospital stay, sequelae during the immediate postoperative period (1st month), death, and follow-up after the 1st postoperative month.
Of 35 cases evaluated at the outset, one case of small and asymptomatic mediastinal bronchogenic cyst was followed clinically but excluded from this study. In addition, 2 cases of bronchogenic cysts in the lung parenchyma were excluded from this study.
Preoperative analysis of the 32 mediastinal cysts that were incorporated into the study included a variety of radiologic and endoscopic diagnostic tests, which were performed in accordance with initial clinical suspicion, cyst location, and the patient's age at presentation. These diagnostic tests included chest radiography (all patients), computed tomography (CT) (n = 23), magnetic resonance imaging (MRI) (n = 8), 2-dimensional echocardiography (n = 6), barium swallow (n = 6), percutaneous fine-needle aspiration under CT guidance (n = 3), esophagoscopy (n = 3), and transesophageal echocardiography (n = 2).
The diagnosis of mediastinal cyst was confirmed surgically in every case. All the patients underwent surgery in our thoracic surgery departments and were reviewed as outpatients at 1 month, 3 months, 1 year, and biannually thereafter.
Results
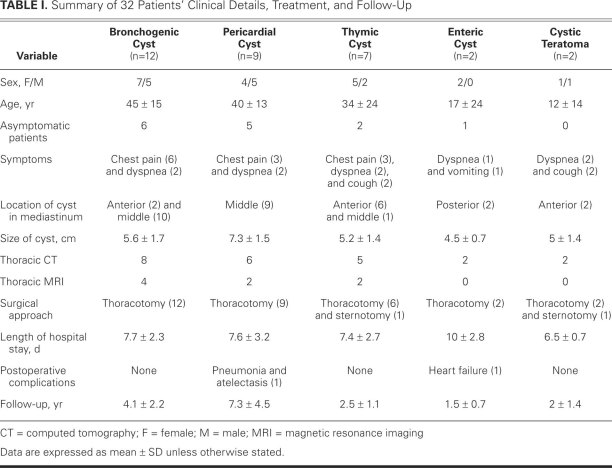
During a span of 4.5 years, 32 mediastinal cysts were treated with surgery. Patients' clinical details, treatments, and duration of follow-up are summarized in Table I. The mean length of hospital stay was 7.7 ± 2.6 days. All patients were free from recurrence during the mean follow-up period of 4.4 ± 3.3 years.
TABLE I. Summary of 32 Patients' Clinical Details, Treatment, and Follow-Up
Bronchogenic Cysts
Six of the 12 patients with bronchogenic cysts were asymptomatic. The most common symptom was chest pain in 6 patients, followed by dyspnea in 2. Chest radiography revealed a mass effect in the anterior-superior mediastinum in all patients. A CT chest scan, performed in 8 patients, revealed round, well-circumscribed masses of water density in the middle mediastinum in 6 patients; similar masses were seen a little higher in the anterior mediastinum in 2 patients. Magnetic resonance imaging helped to clearly define the cystic lesions in the middle mediastinum in the other 4 patients. Compared with the low signal intensity in T1-weighted images, the bright signal intensity in T2-weighted images indicated the cystic content of the mediastinal mass—a characteristic sign that differentiates a solid mediastinal mass. The surgical approach was thoracotomy in all 12 patients.
Pericardial Cysts
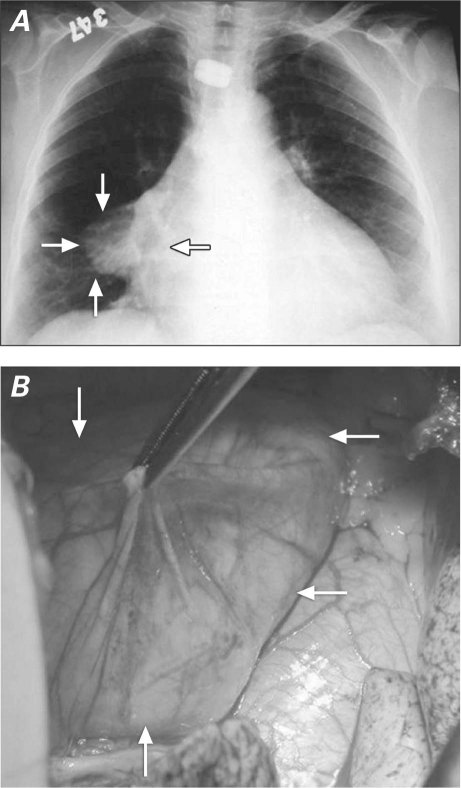
Five of 9 patients with pericardial cysts were asymptomatic; the cyst was an incidental radiologic finding (Fig. 1). Dyspnea or chest pain was the presenting symptom in the other 4 patients with pericardial cysts. Chest radiography in all patients revealed a right paracardial mediastinal tumor. A CT scan performed in 6 patients had revealed thin-walled, sharply defined, oval, homogeneous masses of slightly higher-than-water density, in the right cardiophrenic angle. All 9 patients underwent surgery via right thoracotomy. Pneumonia and atelectasis developed in 1 patient during the postoperative period.
Fig. 1 A) Chest radiograph shows a pericardial cyst (arrows) in the right paracardial area. B) Photograph shows intraoperative appearance of the pericardial cyst (arrows) in the same patient.
Thymic Cysts
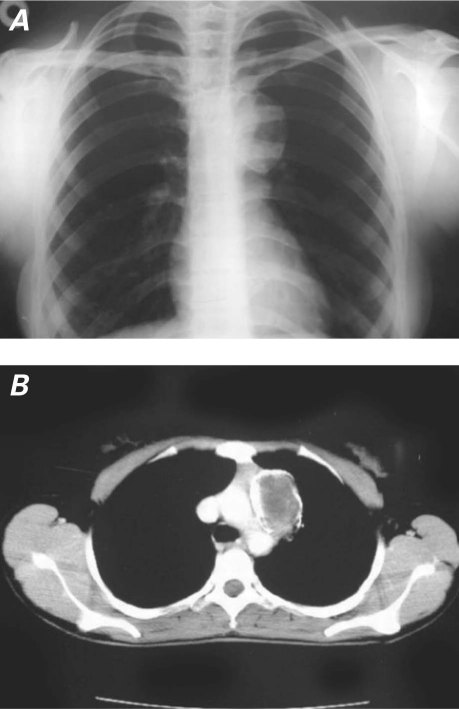
Two of 7 patients with thymic cysts were asymptomatic; 2 presented with dyspnea, 2 with cough, and 3 with angina. Five patients underwent chest CT scans for the evaluation of anterior-superior mediastinal masses detected on chest radiography (Fig. 2). Thymic cysts were located in the anterior mediastinum in 4 patients and in the middle mediastinum in 1 patient. In the remaining 2 patients, MRI showed multilocular masses in the anterior mediastinum, which appeared as a high-intensity area in both T1-weighted and T2-weighted images. In 2 patients, percutaneous fine-needle aspiration under CT guidance was not diagnostic and did not relieve the symptoms. The cysts were resected via thoracotomy in 6 patients and via sternotomy in 1.
Fig. 2 Chest radiograph (A) and computed tomogram (B) show anterior-superior mediastinal masses that were determined upon surgery to be thymic cysts.
Enteric Cysts
One of 2 patients with enteric cyst was clinically asymptomatic. Dyspnea, signs of poor nutrition, and vomiting were present in the other. Preoperative CT scanning confirmed the presence of posterior mediastinal cysts in both patients. The surgical approach was via thoracotomy in both patients. In the postoperative period, the symptomatic patient developed heart failure.
Cystic Teratomas
Dyspnea and cough were the presenting symptoms in the 2 patients with cystic teratoma. In 1 patient, the mediastinal cystic teratoma occupied the entire anterior and left mediastinum and a substantial portion of the left hemithorax. The left-lung parenchyma and mediastinal structures were compressed. Percutaneous fine-needle aspiration under CT guidance was not diagnostic at biopsy, but aspiration of some of the cystic contents partially relieved the patient's symptoms. In the 2nd patient, the cystic teratoma was also located in the anterior mediastinum. The approach was via thoracotomy in 1 patient and via sternotomy in the other. There were no postoperative complications.
Discussion
One controversial aspect of mediastinal cysts concerns appropriate treatment, which ranges from observation to surgical resection.2,3 Many authors have maintained that the treatment of choice is complete excision of the cyst, even in asymptomatic patients, in order to prevent complications and to establish diagnosis.1,5 Ginsberg and colleagues6,7 proposed that small asymptomatic bronchogenic cysts may be monitored with periodic radiography of the chest, whereas enlarging or symptomatic cysts should be removed. We periodically monitored 2 adult patients (not included in this study) who had asymptomatic and incidental bronchogenic cysts of 2 cm in diameter. The cyst progressively increased in size in one of the patients, so we removed it surgically. In the other patient, no progression or symptoms have developed in the 3-year follow-up period. Video-assisted thoracic surgery might be an acceptable surgical procedure for patients with mediastinal cysts, but we had no video-assisted thoracoscopic equipment before 2005.
Despite the value of various noninvasive diagnostic studies, definitive diagnosis is established only by surgical excision and tissue biopsy. Transtracheal and percutaneous cystic aspirations have been proposed as alternatives to operation, but these methods are not widely accepted because of possible cystic recurrence, which carries a substantial morbidity rate.8,9 Many of the patients who do not undergo surgery at diagnosis develop symptoms related to growth of the cyst,10 which means that an operation then involves a higher morbidity and mortality rate, together with a risk of malignancy and development of complications.4 Although complications associated with pericardial cysts are uncommon, serious consequences of enlarged cysts have included hemorrhage,11 spontaneous rupture,12,13 and hemodynamic compromise, including cardiac tamponade.14,15 In light of the potential morbidity associated with complications of pericardial cysts, the potential for cyst recurrence after aspiration alone, and the inability to make a definitive histologic diagnosis in the absence of a tissue sample, many investigators endorse a surgical approach.
Percutaneous fine-needle aspiration may be suggested for histologic diagnosis and possible cure of thymic cysts. However, in 2 of our patients with thymic cysts we found this technique useful neither for cure nor for diagnosis, probably because these cysts were surrounded by dense fibroinflammatory tissue or a thick fibrous capsule. Options other than surgical excision for the treatment of bronchogenic cysts and thymic cysts—including mediastinoscopic aspiration in symptomatic patients—have been reported. However, these methods should be exceptional, reserved as temporary procedures for application to selected patients.1 In our study, 2 of the 7 thymic cysts were asymptomatic, but these patients underwent surgery because the cystic diameters were 5 and 6 cm and cystic thymoma could not be excluded. For cystic teratomas, the standard therapy is complete surgical resection.
There are those who recommend conservative treatment for mediastinal cysts, on the ground that it avoids surgical morbidity and mortality. To the contrary, the prognosis after complete excision is excellent, and the morbidity and mortality rates associated with surgery are low.1,3 In our study sample, there were complications in 2 patients (6%) and no deaths. No patient had a recurrence during the follow-up period of 4.4 ± 3.3 years.
In light of these findings, we conclude that surgery for mediastinal cysts has low morbidity and mortality rates and a very low recurrence rate. It offers a definitive diagnosis and cure, while avoiding the higher morbidity and mortality risks associated with conservative observation. A conservative approach can be considered for small, asymptomatic mediastinal cysts that do not compress adjacent structures, enlarge progressively, display atypical characteristics, or arouse suspicion of malignancy.
Footnotes
Address for reprints: Hidir Esme, MD, Konya Egitim ve Arastirma Hastanesi, Gogus Cerrahisi Klinigi, Meram Yeniyol, 42090 Konya, Turkey
E-mail: drhesme@hotmail.com
References
- 1.Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest 2003; 124(1):125–32. [DOI] [PubMed]
- 2.Kanemitsu Y, Nakayama H, Asamura H, Kondo H, Tsuchiya R, Naruke T. Clinical features and management of bronchogenic cysts: report of 17 cases. Surg Today 1999;29(11):1201–5. [DOI] [PubMed]
- 3.Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: part II. Tumors of the middle and posterior mediastinum. Chest 1997;112(5):1344–57. [DOI] [PubMed]
- 4.Zambudio AR, Lanzas JT, Calvo MJ, Fernandez PJ, Paricio PP. Non-neoplastic mediastinal cysts. Eur J Cardiothorac Surg 2002;22(5):712–6. [DOI] [PubMed]
- 5.Sirivella S, Ford WB, Zikria EA, Miller WH, Samadani SR, Sullivan ME. Foregut cysts of the mediastinum. Results in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg 1985;90(5):776–82. [PubMed]
- 6.Ginsberg RJ, Kirby TJ. Bronchogenic cyst. In: Grillo HC, Austin WG, Wilkins EW Jr, Mathisen DJ, Vlahakes GJ, editors. Current therapy in cardiothoracic surgery. Toronto: B.C. Decker, Inc.; 1989. p. 84.
- 7.Ginsberg RJ, Atkins RW, Paulson DL. A bronchogenic cyst successfully treated by mediastinoscopy. Ann Thorac Surg 1972;13(3):266–8. [DOI] [PubMed]
- 8.Suen HC, Mathisen DJ, Grillo HC, LeBlanc J, McLoud TC, Moncure AC, Hilgenberg AD. Surgical management and radiological characteristics of bronchogenic cysts. Ann Thorac Surg 1993;55(2):476–81. [DOI] [PubMed]
- 9.Sarper A, Ayten A, Golbasi I, Demircan A, Isin E. Bronchogenic cyst. Tex Heart Inst J 2003;30(2):105–8. [PMC free article] [PubMed]
- 10.Patel SR, Meeker DP, Biscotti CV, Kirby TJ, Rice TW. Presentation and management of bronchogenic cysts in the adult. Chest 1994;106(1):79–85. [DOI] [PubMed]
- 11.Borges AC, Gellert K, Dietel M, Baumann G, Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg 1997;63(3):845–7. [DOI] [PubMed]
- 12.Kruger SR, Michaud J, Cannom DS. Spontaneous resolution of a pericardial cyst. Am Heart J 1985;109(6):1390–1. [DOI] [PubMed]
- 13.King JF, Crosby I, Pugh D, Reed W. Rupture of pericardial cyst. Chest 1971;60(6):611–2. [DOI] [PubMed]
- 14.Shiraishi I, Yamagishi M, Kawakita A, Yamamoto Y, Hamaoka K. Acute cardiac tamponade caused by massive hemorrhage from pericardial cyst. Circulation 2000;101(19):E196–7. [DOI] [PubMed]
- 15.Okubo K, Chino M, Fuse J, Yo S, Nishimura F. Life-saving needle aspiration of a cardiac-compressing pericardial cyst. Am J Cardiol 2000;85(4):521. [DOI] [PubMed]