Abstract
Air embolism is rare and potentially fatal. Its early recognition and prompt treatment can help to prevent life-threatening sequelae. Herein, we report the case of a 75-year-old man who underwent a computed tomographic-guided lung biopsy of a left-lower-lobe pulmonary nodule. A few minutes after the procedure, he experienced numbness and weakness in his right hand; this lasted for approximately 10 minutes and resolved on its own. Similar symptoms developed in his left hand and subsided in 5 minutes. His speech then became garbled. An urgent computed tomographic scan of the head showed no acute abnormality. Review of the chest computed tomographic scans that were performed during the biopsy revealed 10 cc of air in the left ventricular cavity. The patient was placed on 100% forced inspiratory oxygen and was kept in the Trendelenburg position on his left side. After 4 hours, computed tomography revealed that the air had been absorbed into the circulation. The patient had no residual neurologic deficits. In addition to reporting this case, we discuss possible causes of air embolism and the management of the condition after percutaneous lung biopsy.
Key words: Biopsy, needle/adverse effects/methods; embolism, air/diagnosis/etiology/physiopathology/therapy; lung/pathology; pneumothorax/etiology; posture; tomography, X-ray computed; treatment outcome
An elderly man underwent a percutaneous lung biopsy for evaluation of a pulmonary nodule. Shortly after the procedure, he developed some neurologic deficits. Review of the computed tomographic (CT) scans of the chest showed air in the left ventricular (LV) cavity. Herein, we discuss the case of this patient, possible mechanisms for air embolism in a patient undergoing percutaneous lung biopsy, and the management of systemic air embolism.
Case Report
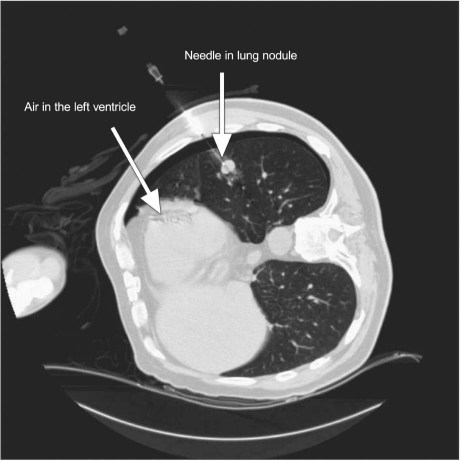
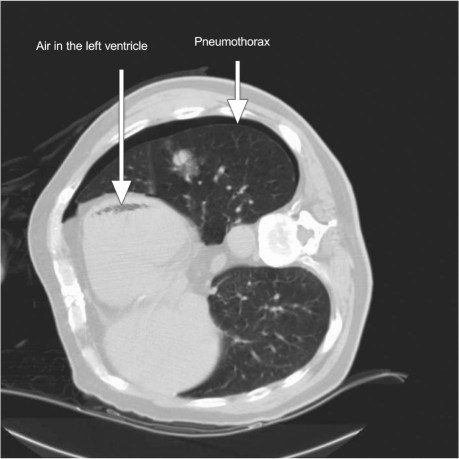
In February 2010, a 75-year-old man underwent a CT-guided lung biopsy of a 1.6-cm left-lower-lobe pulmonary nodule, which had been an incidental finding on chest CT. His medical history was significant for hypertension and melanoma. Under CT guidance, the 19G outer coaxial needle of a Bard® Monopty® disposable core biopsy instrument (Bard Biopsy Systems, part of C.R. Bard, Inc.; Tempe, Ariz) was advanced into the mass in the left lower lobe, and its positioning was confirmed on repeat imaging. The 20G Monopty instrument was advanced coaxially into the mass. Two biopsy cores yielded pigmented tissue. The patient did not cough during the procedure. The biopsy device was removed, and repeat imaging was performed. After the patient was transferred from the CT table to the stretcher, he reported numbness and weakness in his right hand; the condition resolved by itself in 10 minutes. Subsequently, he developed similar symptoms in the left hand, and these subsided in 5 minutes. His speech then became garbled, and he stated that he felt “mysterious.” His blood pressure was 124/72 mmHg and his heart rate was 74 beats/min during this time. An urgent electrocardiogram showed sinus rhythm with no acute ST-T abnormalities, and telemetry revealed no arrhythmias during the patient's period of discomfort. Due to the possibility of transient ischemic attack or evolving stroke, an urgent CT scan of the head was performed; it showed no acute abnormality. Review of the chest CT scans performed during the biopsy revealed 10 cc of air in the LV cavity, along with a small left-sided pneumothorax (Figs. 1 and 2).
Fig. 1 Computed tomogram shows the biopsy needle entering the lung nodule, with associated air in the left ventricle.
Fig. 2 Computed tomogram shows air in the left ventricle and associated left-sided pneumothorax.
The patient was placed on 100% forced inspiratory oxygen and was kept in the Trendelenburg position on his left side, to prevent air from entering the circulation. The cardiology team recommended continuing 100% oxygen and considering hyperbaric oxygen therapy if the patient's symptoms recurred. For 4 hours, he was closely monitored in the emergency department for myocardial ischemia or infarction, arrhythmias, and stroke. A repeat CT scan of the chest showed no air in the LV cavity. The patient was admitted to a telemetry-monitored bed; after an uneventful overnight stay, he was discharged from the hospital with no residual neurologic sequelae.
Discussion
Computed tomographic-guided needle biopsy is a common radiologic procedure that aids the diagnosis of a variety of pathologic pulmonary conditions. Needle biopsy is generally well tolerated, but it is not without risks. Pneumothorax is the most frequent sequela associated with the procedure.1 Air embolism, pulmonary hemorrhage, and death are rare and severe sequelae. Systemic air embolism is a very uncommon and potentially fatal sequela of lung needle biopsy; its reported incidence is 0.07%.2 Peirce3 and Marini and Culver4 showed that needle biopsy of the lung is a much less frequent cause of systemic air embolism than are other procedures, such as cardiac surgery, coronary angiography, and neurosurgery. To our knowledge, 12 cases of simultaneous cerebral and cardiac air embolism have been reported. Our patient's cardiac and cerebral air emboli after a needle biopsy of the lung were not fatal, and his condition improved after conservative treatment.
Aberle and colleagues5 described 3 possible mechanisms for air embolism during needle biopsy of the lung: direct communication between the pulmonary vein and air when the needle is in the pulmonary vein; the formation of a bronchovenous fistula from the needle as it passes through the lung parenchyma; or (in theory) air embolism that reaches the venous circulation through the pulmonary artery. The first 2 mechanisms are plausible precursors of the air embolism in our patient. In addition, physiologic actions (such as the Valsalva maneuver, coughing, or positive-pressure ventilation) may increase air introduction by suddenly elevating intra-alveolar pressures.6 Care should be taken to avoid these influences during biopsy.
It has been speculated that the use of smaller-bore needles is associated with less risk of air embolism than is the use of larger-bore needles.7 During biopsy, promptly replacing the biopsy needle after removing the internal stylet might minimize the chances of air embolism.8
The treatment of systemic air embolism involves administering 100% oxygen through a tightly fitting mask or endotracheal intubation. This facilitates the exchange of oxygen for nitrogen within the air bubble. Positional therapies such as the Trendelenburg and left lateral decubitus position may be helpful, especially if shock is induced by right ventricular failure from air emboli.9,10 Hyperbaric therapy, the mainstay of treatment for symptomatic cases, accelerates the absorption of nitrogen and its replacement with oxygen.11
Summary
We have reported a rare case of simultaneous LV and cerebral air embolism that resulted from a percutaneous CT-guided needle biopsy. Early recognition of this rare and potentially fatal condition is important, because prompt therapy can help to prevent the life-threatening sequelae of air embolism.
Footnotes
Address for reprints: Aniruddha Singh, MD, Department of Medicine, Saint Vincent Hospital, Worcester, MA 01608
E-mail: aniruddha_rajput@rediffmail.com
References
- 1.Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006;59(1):60–4. [DOI] [PubMed]
- 2.Sinner WN. Complications of percutaneous transthoracic needle aspiration biopsy. Acta Radiol Diagn (Stockh) 1976;17 (6):813–28. [DOI] [PubMed]
- 3.Peirce EC. Cerebral gas embolism (arterial) with special reference to iatrogenic accidents. Hyperbaric Oxygen Rev 1980;1 (3):161–84.
- 4.Marini JJ, Culver BH. Systemic gas embolism complicating mechanical ventilation in the adult respiratory distress syndrome. Ann Intern Med 1989;110(9):699–703. [DOI] [PubMed]
- 5.Aberle DR, Gamsu G, Golden JA. Fatal systemic arterial air embolism following lung needle aspiration. Radiology 1987; 165(2):351–3. [DOI] [PubMed]
- 6.Lattin G Jr, O'Brien W Sr, McCrary B, Kearney P, Gover D. Massive systemic air embolism treated with hyperbaric oxygen therapy following CT-guided transthoracic needle biopsy of a pulmonary nodule. J Vasc Interv Radiol 2006;17(8):1355–8. [DOI] [PubMed]
- 7.Lalli AF, McCormack LJ, Zelch M, Reich NE, Belovich D. Aspiration biopsies of chest lesions. Radiology 1978;127(1): 35–40. [DOI] [PubMed]
- 8.Hiraki T, Fujiwara H, Sakurai J, Iguchi T, Gobara H, Tajiri N, et al. Nonfatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest 2007;132(2):684–90. [DOI] [PubMed]
- 9.Muth CM, Shank ES. Gas embolism. N Engl J Med 2000; 342(7):476–82. [DOI] [PubMed]
- 10.Coulter TD, Wiedemann HP. Gas embolism. N Engl J Med 2000;342(26):2000–2. [DOI] [PubMed]
- 11.Leach RM, Rees PJ, Wilmshurst P. Hyperbaric oxygen therapy. BMJ 1998;317(7166):1140–3. [DOI] [PMC free article] [PubMed]