We report a case on a neonate with congenital epulis rarely detected on the anterior ventral surface of the tongue.
Introduction
Congenital epulis of the newborn, also known as congenital granular cell tumour, or Neumann's tumour, is a rare benign tumour.1 The neoplasm occurs more frequently in the alveolar ridge of the maxilla near the canine than in the mandibular alveolus and has rarely been reported on the tongue.2–8 This lesion occurs 10 times more frequently in female infants than male infants suggesting hormonal involvement during embryonic development.1 However, the exact etiology and pathogenesis remain unknown.9 Congenital epulis may be sessile or pedunculated, normally coloured or reddish, vary in size from several millimetres to a few centimetres in diameter, be single or multiple, and may interfere with respiration or feeding.1,8,9 Histologically, the tumour mass comprises large, round cells with abundant eosinophilic granular cytoplasm, and round or oval lightly basophilic nuclei.5,7 Diagnosis is often made postnatally during neonatal care. However, prenatal diagnosis is critical in determining the route of delivery as well as planning early multidisciplinary postnatal management as the mass may obstruct the airway during the perinatal period.10 The recommended treatment is prompt surgical excision, although spontaneous regression has been reported in a few cases.11
Case report
In this report, we describe a rarely reported case of congenital epulis detected on the anterior ventral surface of the tongue. A newborn girl was seen immediately after delivery with a mass protruding from her mouth. She weighed 3880 g at birth and was delivered at full term via Caesarean section. The pregnancy was normal and the prenatal ultrasound reports showed no abnormalities. No family history of hereditary diseases was discovered. Upon physical examination, a tumour mass obtruding from the oral cavity, measuring 2 × 1 × 0.6 cm, that was pink, pedunculated and attached at the anterior ventral surface of the tongue was detected (Figure 1). The mass prevented normal closure of the mouth, although respiration was normal. Because the mass partially interfered with breastfeeding, a nasogastric tube was used for breastfeeding.
Figure 1.
Appearance of a mass protruding from the mouth
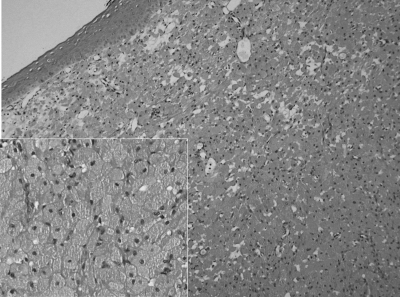
Excluding the mass, a general physical examination, including laboratory tests, did not reveal other abnormalities. On the second day after birth, the tumour was completely resected by surgical excision following local anaesthesia. The intraoperative and postoperative courses were uneventful. The newborn recovered with no complications, and breastfeeding was initiated the same day of the operation. Histological examination was performed using 3 µm-thick sections cut from formalin-fixed paraffin-embedded tissue blocks and stained with hematoxylene and eosin. A microscopic analysis revealed large sheets of cells with no particular cellular arrangement under a normal squamous mucosa (Figure 2). The lesional cells were polygonal or rounded, with nuclei ranging from small and dark to large with some vesicular chromatin. No notable nuclear atypia was observed. Immunostaining (Biotin-Streptavidin detection system, Ventana Benchmark XT) with S-100 (Scytek, Clone: 4C4.9) did not show any positivity, and CD34 (Scytek, Clone: QBEND/10) staining emphasized a prominent vascularity. These findings were interpreted as being sufficient to diagnose ‘granular cell tumour’.
Figure 2.
Histological aspects of the tumour: Sheets of cells with no particular cellular arrangement (H&E; 100x). Inlet (H&E x400): Typical large polygonal granular cells without nuclear atypia
The one-month follow-up period did not reveal any resulting abnormalities in the baby.
Discussion
Congenital epulis, or granular cell tumour, is a rare intra-oral tumour of newborns. It is generally not associated with any other abnormality of the teeth or other congenital abnormalities.11 In this report, there were no other congenital abnormalities present in the newborn. As predicted by the fact that there is a female predilection for congenital epulis,1 this report documents the case of a female newborn. The diagnosis of a large congenital epulis is often made at birth, as in our patient. Diagnosis is also made during systematic examination of the newborn immediately after birth, when the tumour is small. The upper maxillary location is the most frequent location but the mandibular region, and in rare cases the tongue, can also be involved.2 A Medline search revealed only eight documented cases of congenital epulis reported with similar histological appearance on the tongue.2–8 In four cases, a solitary lesion was observed on the tongue,2,4,6,8 similar to the present case, and in the other four cases, a tongue lesion occurred simultaneously with a lesion on the alveolar gingival.3,5,7 Only one reported case occurred in a male newborn.6 Cussen and MacMahon8 previously reported the lesion on the tip of the tongue, Atterbury and Vazirani6 reported one case on the anterior dorsum surface of the tongue. The case presented in this paper was diagnosed with a mass on the anterior ventral surface of the tongue, similar to six other case reports.2–5,7 Some prenatal conditions, such as polyhdramniosis, have been described with congenital epulis. Postnatally, feeding and respiration problems in addition to difficulty closing the mouth have been reported.10 In the present case, there was no polyhdramniosis or problem with respiration, although the lesion interfered with feeding because of the size of the tumour.
Sonographic prenatal diagnosis of congenital abnormalities is an important tool in the management of pregnancy, delivery and postnatal treatment of the affected newborn. Prenatal ultrasonographic diagnosis of congenital epulis is possible after the 25th week of intrauterine life.10 However, the present case showed no abnormalities in the prenatal ultrasound reports.
Management involves surgical removal of the congenital epulis under local or general anaesthesia,9 as spontaneous regression of the lesion is only rarely reported.11 The treatment selected for our case was surgical excision under local anaesthesia to alleviate problems the infant was having with feeding and with closure of the mouth.
A differential diagnosis of masses in the oral cavity of newborns must be made for hemangioma, lymphangioma, fibroma, granuloma, rhabdomyosarcoma and osteogenic and chondrogenic sarcomas because the treatment modalities differ for each case.9 In the present case, the clinical diagnosis of congenital epulis was further confirmed by histopathological examination. However, some congenital lesions occur predominantly on the tongue. Choristoma and hamartoma are well-known congenital, tumour-like masses comprising an overgrowth of normal cells that are located predominantly on the posterior dorsum of the tongue.12 Leiomyomatous hamartoma has the appearance of congenital epulis and is often seen on the median anterior alveolar ridge and the tip of the tongue.13
We conclude that rare congenital epulis on the tongue must be differentially diagnosed by histological examination and then must be surgically excised promptly if there is any stress on fear of airway obstruction or feeding.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
SMK
Contributorship
All authors contributed equally
Acknowledgements
None
Reviewer
Robert Insall
References
- 1.Godra A, D'Cruz CA, Labat MF, Isaacson G Pathologic quiz case: a newborn with a midline buccal mucosa mass, congenital gingival granular cell tumour (congenital epulis). Arch Pathol Lab Med 2004;128:585–6 [DOI] [PubMed] [Google Scholar]
- 2.Senoo H, Iida S, Kishino M, Namba N, Aikawa T, Kogo M Solitary congenital granular cell lesion of the tongue. Oral Pathol Oral Radiol Endod 2007;104:e45–8 [DOI] [PubMed] [Google Scholar]
- 3.Dixter CT, Konstat MS, Giunta JL, Schreirer E, White GE Congenital granular-cell tumour of alveolar ridge and tongue. Report of two cases. Oral Surg Oral Med Oral Pathol 1975;40:270–7 [DOI] [PubMed] [Google Scholar]
- 4.Ophir D, Lifschitz B, Mogilner BM Congenital granular cell tumour of the tongue. Head Neck Surg 1987;9:250–2 [DOI] [PubMed] [Google Scholar]
- 5.Yavuzer R, Ataoglu O, Sari A Multiple congenital epulis of the alveolar ridge and tongue. Ann Plast Surg 2001;47:199–202 [DOI] [PubMed] [Google Scholar]
- 6.Atterbury RA, Vazirani SJ Granular-cell myoblastoma of the newborn; report of a case. Oral Surg Oral Med Oral Pathol 1957;10:1037–40 [DOI] [PubMed] [Google Scholar]
- 7.Loyola AM, Gatti AF, Pinto DS Jr, Mesquita R Alveolar and extra-alveolar granular cell lesions of the newborn: report of case and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:668–71 [DOI] [PubMed] [Google Scholar]
- 8.Cussen LJ, MacMahon RA Congenital granular-cell myoblastoma. J Pediatr Surg 1975;10:249–53 [DOI] [PubMed] [Google Scholar]
- 9.Merrett SJ, Crawford PJ Congenital epulis of the newborn: A case report. Int J Paediatr Dent 2003;13:127–9 [DOI] [PubMed] [Google Scholar]
- 10.Williams RW, Grave B, Stewart M, Heggie A Prenatal and postnatal management of granular cell tumours: a case report. Br J Oral Maxillofac Surg 2009;47:56–8 [DOI] [PubMed] [Google Scholar]
- 11.Ritwik P, Brannon R, Musselman R Spontaneous regression of congenital epulis: a case report and review of the literature. J Med Case Reports 2010;4:331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chou LS, Hansen LS, Daniels TE Choristomas of the oral cavity: a review. Oral Surg Oral Med Oral Pathol 1991;72:584–93 [DOI] [PubMed] [Google Scholar]
- 13.de la Rosa-Garcia E, Mosqueda-Taylor A Leiomyomatous hamartoma of the anterior tongue: report of a case and review of the literature. Int J Paediatr Dent 1999;9:129–32 [DOI] [PubMed] [Google Scholar]