Abstract
Background
More than 300 000 joint replacement operations are performed in Germany every year, and the number is rising. In this article, we consider the question of simultaneous bilateral joint replacement at the hips or knees. Such procedures are indicated in patients suffering from bilateral, symptomatic arthrosis.
Methods
The article is based on a selective review of the relevant literature, and on the authors’ own prospective comparative study of simultaneous bilateral hip replacement.
Results
The morbidity and mortality of simultaneous bilateral hip arthroplasty are no different than those of a unilateral procedure. Rehabilitation is easier when both joints are replaced at the same time. Simultaneous bilateral knee arthroplasty has comparable morbidity to a unilateral procedure, but a slightly higher mortality (0.30% vs. 0.14%). Allogenic blood transfusion is more likely to be needed in a bilateral procedure, particularly of the knees. Simultaneous bilateral arthroplasty of either the hips or the knees in one surgical procedure is better than two-staged arthroplasty during a single hospital stay.
Conclusion
Simultaneous bilateral hip arthroplasty is safer for the patient and facilitates rehabilitation, regardless of the patient’s age and ASA status (ASA, American Society of Anesthesiologists). With regard to the knees, there are two additional issues, namely the more frequent need for transfusion and somewhat higher mortality of a simultaneous bilateral procedure. Therefore, we recommend simultaneous bilateral knee arthroplasty only for patients in ASA classes 1 and 2. Simultaneous bilateral arthroplasty of either the hip or knee incurs lower costs than two separate operations.
The Federal Office for Quality Assurance (Bundesgeschäftsstelle Qualitätssicherung, BQS) recorded the implantation of about 158 000 artificial hips and 147 000 artificial knees in Germany in 2008. This shows the significance in terms of numbers of prosthetic implants of these joints. Simultaneous bilateral replacements were not included in this statistic, since they are represented in another diagnosis-related group.
Some patients have the indication for total joint replacement bilaterally. Key criteria that favor simultaneous joint replacement are bilateral severe symptomatic arthrosis and the patient’s wish to have both joints replaced. Improved surgical planning, prosthesis designs that are easier to implant, and muscle-preserving operative techniques (1) make it an obvious choice today to choose a one-stage procedure for bilateral joint wear. The aim of this review article is to assess the advantages and disadvantages of one-stage bilateral joint replacement for the patient. There are no randomized controlled studies comparing one-stage with two-stage bilateral joint replacement, and for this reason the evidence based on the results presented is limited.
Method
This review article is based on a selective literature search on one-stage (simultaneous) hip and knee replacement and on our own experience of bilateral replacement of hip and knee joints. Data from a prospective comparative study of simultaneous hip joint replacement carried out at the Department of Orthopedics, St. Josef Hospital, Wiesbaden, Germany (30 patients treated bilaterally in a one-stage procedure, 30 patients treated on one side only) were also included in the analysis. At the present time, neither Cochrane reviews nor guidelines exist regarding the choice of procedure in patients with bilateral joint wear.
History
The story of prosthetic implants of the large joints starts in the middle of the 20th century (2). As early as 1971, a publication appeared posing the question whether bilateral hip replacement as a single procedure would be advantageous in patients with bilateral coxarthrosis (3). The aim of that study, which included 50 patients who underwent one-stage bilateral procedures, was to find out whether the new treatment method was as successful as unilateral treatment, or even showed advantages for the patient. The primary object of the study was to assess functional results and clinical outcome. The results were very promising. Many publications followed on the subject of one-stage joint replacement in regard to both hips and knees. Recently, some prospective comparative studies have allowed refinement of our knowledge relating to the questions arising in this area of surgery.
Frequency of one-stage joint replacement
Whether one-stage replacement of two joints is offered to the patient usually depends on the surgeon. Hospitals where large numbers of patients are treated offer this option more frequently (4).
In terms of the percentage of patients given one-stage bilateral hip replacement, the largest numbers are reported by the Wrightington Hospital in England. Over a period of 20 years, 13 000 operations were carried out there, 405 of them bilateral (5). This corresponds to 3.1% of the patients and 6.2% of the implants. In the past 3 years (2008 to 2010), 1692 patients received hip replacements at St. Josef Hospital, Wiesbaden, in 62 cases bilaterally. This corresponds to 3.7% of all patients given hip replacements. In North America and Asia, the largest numbers of patients are reported for knee replacements. In a retrospective Korean study, Kim et al. report on 2385 one-stage bilateral knee replacements (6). How often one-stage bilateral operations are carried out worldwide is unknown. Regional differences exist. In South America, unlike in North America and Asia, one-stage bilateral joint replacement is rare. Many publications exist about simultaneous replacement of hips or knees. By contrast, little has been written about how to treat ipsilateral arthrosis of both hip and knee, or arthrosis in all four joints.
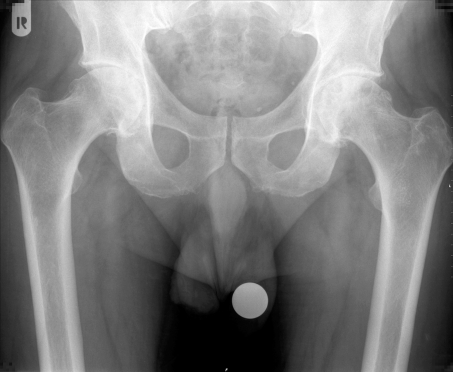
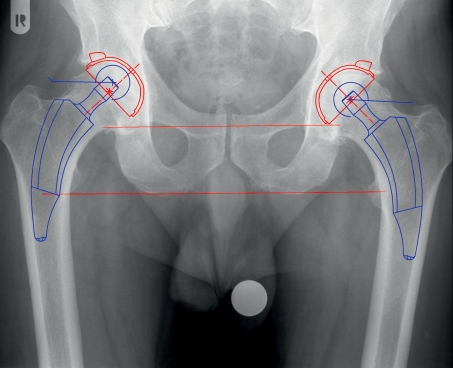
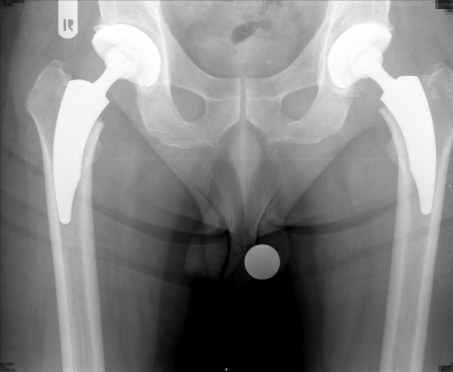
Figure 1 shows a patient with extensive bilateral coxarthrosis who chose to undergo one-stage replacement of both joints. Figure 2 demonstrates the digital preoperative planning, in which the joint prostheses are virtually placed in a large-scale image. Figure 3 shows the joints after the one-stage bilateral total hip replacement.
Figure 1.
Bilateral coxarthrosis of the hip with bilateral extensive loss of cartilage and cyst formation in the femoral heads
Figure 2.
Digital preoperative planning for simultaneous bilateral hip arthroplasty
Figure 3.
Postoperative radiograph after cement-free bilateral hip arthroplasty
Safety of one-stage bilateral joint replacement
Elective total joint replacement is associated with low mortality. Various collective studies have cited mortality rates between 0.14% and 0.3%. All published data relating to one-stage bilateral hip replacement—whether retrospective or in prospective studies—show no difference to unilateral replacement. Moreover, a large retrospective study showed no difference in mortality between patients with a low general surgical risk (ASA score 1 to 2; ASA, American Society of Anesthesiologists) and those with a high surgical risk (ASA score 3 to 4) (7, 8). The ASA scoring of patients in Germany who received joint replacements in 2008 has been published by the BQS (9) and is given in Table 1. However, a (retrospective) study of 450 patients who received bilateral replacements compared to 450 who received unilateral replacements (10), who were operated on between 1970 and 1997, did show a higher incidence of pulmonary embolism (1.6% versus 0.7%). The mortality rate within the first postoperative year, on the other hand, was higher among the patients with unilateral replacement (4% versus 3.1%). Up to 1986 all patients in that study received warfarin prophylaxis; from 1987 onward, prophylaxis was with heparin on the day of surgery only, followed by 325 mg aspirin daily from the first postoperative day. In this respect these data are not comparable with the prophylaxis practiced in Germany, which in accordance with guidelines is done with low-molecular heparin or new oral antithrombotics over the course of 4 weeks.
Table 1. ASA scoring of patients undergoing primary total hip or knee replacement (2008).
| Hip | Knee | |
| ASA 1: Normal healthy patient | 9.6% | 6.0% |
| ASA 2: Patient with mild systemic disease | 59.8% | 59.4% |
| ASA 3: Patient with severe systemic disease that limits activity | 30% | 34.2% |
| ASA 4: Patient with severe, incapacitating systemic disease that is a constant threat to life | 0.6% | 0.5% |
| ASA 5: Moribund patient | 0% | 0% |
Source: BQS Institute for Quality and Patient Safety (BQS-Institut für Qualität und Patientensicherheit), www.bqs-institut.de/
For knee joint replacement, various information is given about the risk to the patient’s life. Here, too, in many studies no difference is observed. In an analysis of all total knee replacements in the USA from 1998 to 2006, the mortality among patients with unilateral replacement was 0.14% versus 0.30% for those with bilateral replacement (p<0.0001) (11). When the second side was operated on later during the same hospital stay (‚two-stage’), morbidity and mortality rose. In a prospective study (12), 70 patients over the age of 70 and who had both knees replaced in one operation were compared to a control group of 312 younger patients who had one knee replaced. Morbidity was comparable; no deaths were seen. The authors do not regard advanced age as a contraindication to one-stage bilateral knee replacement.
A (retrospective) comparison study between patients aged 75 or older (n = 43) and younger patients (n = 136) has also been published for one-stage bilateral hip replacement. In this study, too, no difference was seen (13).
Complication rates
Various complications are possible with total joint replacements, but they are rare. A distinction needs to be made between general complications—chiefly, thromboembolic events—and complications that are specific to the particular operative procedure. Two prospective studies comparing one-stage bilateral and unilateral hip replacement showed no differences between the procedures in terms of fat embolism and respiratory depression (14, 15). An interesting observation (15) was that patients with bone marrow embolism showed significantly lower oxygen saturation values on the first postoperative day than patients who had no embolism (p = 0.017). However, this was true in both patient groups.
Several studies investigating thromboembolic complications of one-stage bilateral hip and knee replacements found no differences in this connection. A meta-analysis of 23 studies that included 2063 bilateral hip replacements (16) found no statistically significant difference (p = 0.365 and p = 0.268). In our own study of a total of 60 patients we saw no thromboembolic complications (17).
Many studies have also found no differences in rates of specific complications (infection, fracture, and luxation). The largest study on one-stage bilateral knee replacement, which retrospectively analyzed 2385 patients operated on bilaterally in one procedure and 719 who underwent unilateral replacement, showed no differences (6). Berend et al. (10) observed deep infection of the implanted hips in 1.4% (bilateral) versus 1.3% of cases. Infection rates today are even lower. Out of more than 1000 implanted hip replacements in the past 2 years, we have seen deep infection in only 0.4% of cases.
Blood loss and transfusion requirements
Obviously, blood loss is greater in simultaneous bilateral operations than in unilateral operations. In our own study (17), with the same mean baseline hemoglobin concentration (14.1 mg/dL) in both groups, mean hemoglobin concentration on the 1st postoperative day was 10.2 mg/dL in the bilaterally operated group compared with 11.0 mg/dL in the unilateral group. Transfusion were given to 4 of the bilaterally operated patients and 2 of the unilaterally operated patients during their hospital stay (Table 2). The higher transfusion rate has also been seen in other prospective studies. Transfusion rates are higher in bilateral knee replacements than in bilateral hip replacements. Peak et al. (18) report having given transfusions to 34% of knee patients versus 20% of hip patients. Transfusion rates increase markedly when joint replacements are carried out as two-stage procedures during a single hospital stay (19).
Table 2. Comparison of bilateral (n = 30) with unilateral total hip replacement (n=30)—data from a prospective study at St. Josef Hospital, Wiesbaden.
| Unilateral | Bilateral | |
| Sex, male/female | 15/15 | 16/14 |
| Mean age (years) | 64 | 62 |
| Mean bodyweight (kg) | 80 | 81 |
| Mean ASA score | 2.0 | 2.1 |
| Duration of hospital stay | 12 | 15 |
| Preoperative Harris Hip Score | 41 | 39 |
| Postoperative Harris Hip Score, 6 weeks after the operation | 91 | 90 |
| Pain VAS before surgery | 7.6 | 7.6 |
| Pain VAS 6 weeks after surgery | 1.0 | 1.1 |
| Preoperative Hb value | 14.1 | 14.1 |
| Hb value on 1st postoperative day | 11 | 10.2 |
| Allogenic blood transfusion (no. of patients) | 2 | 4 |
| Mean operative time (minutes) | 75 | 100 |
| Complications | 0 | 1 postoperative avulsion fracture of the greater trochanter |
| Revisions | 0 | 1 refixation of the avulsion fracture of the greater trochanter |
| Infections | 0 | 0 |
| Thromboembolism | 0 | 0 |
| Gait mobilization (days) | 2.4 | 2.7 |
VAS, visual analog scale: 0 (no pain) to 10 (most severe pain); All patients who underwent one-stage bilateral hip replacement in the St. Josef Hospital between June 2006 and March 2009 were included in the study
Patient acceptance
Many patients do not know that it is possible to have two joints operated on at once. However, after extensive information and advice, most patients choose this procedure. Video recordings of patients walking around on crutches a few days after the operation are helpful in introducing patients to this concept. In our own study, 29 out of the 30 patients who had one-stage bilateral joint replacements said afterward that they would choose this procedure again. Patients often report that they are very satisfied that they chose this option.
Rehabilitation
After a first unilateral operation, patients with bilateral arthrosis still have one joint causing them pain, and, in addition, contractures on the non-operated side impede their rehabilitation. In gait studies, Wykman and Olsson (20) noted that patients with bilateral coxarthrosis were unable to obtain an optimal functional result until after the second hip was replaced. Berend et al. (10) added to this that simultaneous bilateral hip replacement offered better conditions for clinical success, because that fact that both sides had been operated on meant that both sides were equally painful and therefore equally used during rehabilitation, thus preventing the patient from protecting the operated hip in an undesirable way. Even if the hip operated on first does show an excellent functional result, the pain in the contralateral hip means that a final satisfactory outcome will not be obtained until that hip has been replaced as well. Thus, in terms of optimal rehabilitation and patient satisfaction, a one-stage procedure is desirable. Consecutive unilateral joint replacements make considerably greater physical and psychological demands on the patient as well as taking up more time. The overall duration of pain is longer, and the demands of two operations, with anesthesia and its attendant risks, two hospital stays, and two courses of rehabilitation have to be taken into account.
Another advantage of one-stage replacement in patients with bilateral arthrosis is seen in respect of the long-term results. Patients with one-stage bilateral hip replacement had significantly better bending than patients with unilateral or two-stage replacements. The same was noted for parameters quantifying activities of daily living. No differences were seen in relation to abduction and reported pain (21).
Cost issues
Both the length of hospitalization and the rehabilitation period are much shorter for one-stage bilateral joint replacement than for two unilateral procedures. This is noted in all studies, and the authors see a clear cost advantage (7, 19, 22, 23). In our own study (16), patients who underwent one-stage bilateral hip replacement spent an average of 15 days in hospital, whereas those who had unilateral operations stayed for an average of 12 days—that means, for two consecutive operations, hospitalization for 24 days. The following remarks exemplify the differences in cost.
Using the mean values of the state basic case value (Landesbasisfallwert, LBFW) for Hesse and the list of flat-rate case payments from the Institute for the Hospital Remuneration System (Institut für das Entgeltsystem im Krankenhaus, INEK) 2009 (24), a cost–earnings calculation for one-stage bilateral joint replacement was prepared for hospitals. The results are shown in Table 3. The advantage for the cost bearer is significant. For the hospital, the profit is higher for the one-stage procedure, but lower than the sum of two unilateral operations. The costs of inpatient rehabilitation are incurred only once with the one-stage procedure, and in the case of our own patients were only insignificantly higher than for patients who had unilateral operations.
Table 3. Cost–earnings calculation based on the state basic case value (LBFW) for Hesse and the list of flat-rate case payments (INEK) 2009, taken as mean values.
| Bilateral total hip replacement (DRG I36Z) | 2 x Unilateral total hip replacement (DRG I47B) | Difference | |
| LBFW (€) | 2868.50 | 2 × 2868.50 | |
| Relative weight x | 3.344 | 2.366 | – |
| Earnings (€) | 9592.26 | 13 573.74 | 3981.48 |
| INEK costs (€) | – 8765.76 | – 12 406.06 | 3640.30 |
| Profit (€) | 826.5 | 1167.76 | 341.18 |
INEK, Institut für das Entgeltsystem im Krankenhaus (Institute for the Hospital Remuneration System); LBFW, Landesbasisfallwert (state basic case value); DRG, diagnosis-related group
Discussion and recommendation
In almost all studies, simultaneous or one-stage bilateral replacement is compared to unilateral replacement. In patients with bilateral arthrosis, operating at first on only one joint entails the necessity of another unilateral operation. Logically, then, the risks of simultaneous replacement must be compared with the risks of two unilateral replacements, since the patient would have to undergo two of the latter. Looked at this way, simultaneous replacement, especially of the hip, is in many respects the safer procedure. Operating on two joints under the same anesthesia is preferable to a two-stage procedure in which the contralateral side is operated on a few days later during the same hospital stay. In all respects—and especially because of the rise in complications and the increased transfusion rate—the two-stage procedure is inferior to the one-stage procedure and should therefore not be employed. The higher transfusion rate in one-stage bilateral hip joint replacement becomes less significant when it is compared with the transfusion rate for two unilateral procedures, but this problem should be discussed with the patient. The transfusion rate is markedly higher for simultaneous bilateral replacement of the knee. A slightly increased mortality rate is also seen, equal to double the rate seen for unilateral knee replacement (that is, the rate for two unilateral replacements added together). This should be taken into account when contemplating simultaneous replacement.
Patient age is not critical for whether simultaneous joint replacement is indicated. What is important is the ASA score (8). This is referred to in some studies, though estimates vary. We recommend simultaneous replacement to patients with bilateral symptomatic coxarthrosis who have an ASA score of 1 to 3—that is, to over 99% of patients (Table 1). In most cases today, cement-free implants are used. Despite this, owing to improved operative technique and implant design, patients with simultaneous replacements can achieve early full weight bearing. For the knee joint, we are cautious about recommending simultaneous replacement to patients in ASA class 3. The increased transfusion rate also has to be mentioned.
For patients, there is no doubt that one-stage bilateral replacement is advantageous. It means one hospital stay and one course of rehabilitation, both of which are insignificantly longer than after a unilateral procedure. The costs to the patient are lower, and absence from work is shorter. The functional result also argues for the simultaneous route.
Acknowledgments
Translated from the original German by Kersti Wagstaff, MA.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Pfeil J, Siebert WE. Heidelberg, Dordrecht, London, New York: Springer; 2010. Minimal invasive surgery in total hip replacement. [Google Scholar]
- 2.Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br. 1950;32:166–173. doi: 10.1302/0301-620X.32B2.166. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe WL, Charnley J. Bilateral low friction arthroplasty as a single operative procedure. A report of fifty cases. Bull Hosp Joint Dis. 1971;32:198–214. [PubMed] [Google Scholar]
- 4.Hooper GJ, Hooper NM, Rothwell AG, Hobbs T. Bilateral total joint arthroplasty: the early results from the New Zealand National Joint Registry. J Arthroplasty. 2009;24:1174–1177. doi: 10.1016/j.arth.2008.09.022. Epub 2008 Dec 3. [DOI] [PubMed] [Google Scholar]
- 5.David B, Wroblewski BM. Bilateral charnley arthroplasty as a single procedure a report on 400 patients. J Bone Joint Surg Br. 1981;Vol. 63-B:354–356. doi: 10.1302/0301-620X.63B3.7263745. [DOI] [PubMed] [Google Scholar]
- 6.Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91:64–68. doi: 10.1302/0301-620X.91B1.21320. [DOI] [PubMed] [Google Scholar]
- 7.Alfaro-Adrián J, Bayona F, Rech JA, Murray W. One or two-stage bilateral total hip replacement. J Arthroplasty. 1999;14:439–445. doi: 10.1016/s0883-5403(99)90099-2. [DOI] [PubMed] [Google Scholar]
- 8.Cohen MM, Duncan PG. Physical status score and trends in anesthetic complications. J Clin Epidemiol. 1988;41 doi: 10.1016/0895-4356(88)90012-1. [DOI] [PubMed] [Google Scholar]
- 9.BQS Institut für Qualität und Patientensicherheit. www.bqs-institut.de/
- 10.Berend ME, Ritter MA, Harty LD, et al. Simultaneous bilateral versus unilateral total hip arthroplasty an outcome analysis. J Arthroplasty. 2005;20:421–426. doi: 10.1016/j.arth.2004.09.062. [DOI] [PubMed] [Google Scholar]
- 11.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206–1216. doi: 10.1097/ALN.0b013e3181bfab7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Severson EP, Mariani EM, Bourne MH. Bilateral total knee arthroplasty in patients 70 years and older. Orthopedics. 2009;32 doi: 10.3928/01477447-20090501-13. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein MA, Keggi JM, Zatorski LE, Keggi KJ. One-stage bilateral total hip arthroplasty in patients > or = 75 years. Orthopedics. 2002;25:153–156. doi: 10.3928/0147-7447-20020201-19. [DOI] [PubMed] [Google Scholar]
- 14.Cammisa FP, Jr, O’Brien SJ, Salvati EA, Sculco TP, Wilson PD, Jr, Ranawat CS, Pellicci PM, Inglis AE. One-stage bilateral total hip arthroplasty. A prospective study of perioperative morbidity. Orthop Clin North Am. 1988;19:657–668. [PubMed] [Google Scholar]
- 15.Young-Hoo Kim, Oh SW, Kim JS. Prevalence of Fat Embolism Following Bilateral Simultaneous and Unilateral Total Hip Arthroplasty Performed with or without Cement. A Prospective, Randomized Clinical Study. J Bone Joint Surg. 2002;84:1372–1379. doi: 10.2106/00004623-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Tsiridis E, Pavlou G, Charity J, Tsiridis E, Gie G, West R. The safety and efficacy of bilateral simultaneous total hip replacement an analysis of 2063 cases. J Bone Joint Surg Br. 2008;90-B:1005–1112. doi: 10.1302/0301-620X.90B8.20552. [DOI] [PubMed] [Google Scholar]
- 17.Hofmann TN. Simultane bilaterale hüftendoprothetische Versorgung. Inauguraldissertation Medizinische Fakultät der Universität Heidelberg. 2010 [Google Scholar]
- 18.Peak EL, Hozack WJ, Sharkey PF, Parvizi J, Rothman RH. One-stage bilateral total joint arthroplasty: a prospective, comparative study of total hip and total knee replacement. Orthopedics. 2008;31 doi: 10.3928/01477447-20080201-26. [DOI] [PubMed] [Google Scholar]
- 19.Parvizi J, Tarity TD, Ednan Sheikh E, Sharkey PF, Hozack WJ, Rothman RH. Bilateral Total Hip Arthroplasty. One-stage versus Two-stage Procedures Clinical Orthopaedics and related research. 2006;453:137–141. doi: 10.1097/01.blo.0000246529.14135.2b. [DOI] [PubMed] [Google Scholar]
- 20.Wykman A, Olsson E. Walking ability after total hip replacement: a comparison of gait analysis in unilateral and bilateral cases. J Bone Joint Surg Br. 1992;74-B:53–56. doi: 10.1302/0301-620X.74B1.1732266. [DOI] [PubMed] [Google Scholar]
- 21.Yoshii T, Jinno T, Morita S, Koga D, Matsubara M, Okawa A, Shinomiya K. Postoperative hip motion and functional recovery after simultaneous bilateral total hip arthroplasty for bilateral osteoarthritis. J Orthop Sci. 2009;14:161–166. doi: 10.1007/s00776-008-1303-x. [DOI] [PubMed] [Google Scholar]
- 22.Reuben JD, Meyers SJ, Cox DD, et al. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13 doi: 10.1016/s0883-5403(98)90095-x. [DOI] [PubMed] [Google Scholar]
- 23.Bhan S, Pankaj A, Malhotra R. One or two-stage bilateral total hip arthroplasty: a prospective, randomised, controlled study in an Asian population. J Bone Joint Surg Br. 2006;88-B:298–303. doi: 10.1302/0301-620X.88B3.17048. [DOI] [PubMed] [Google Scholar]
- 24.InEK GmbH - Institut für das Entgeltsystem im Krankenhaus. www.g-drg.de/cms/