Abstract
The development of genomic and proteomic tools has enabled studies that begin to characterize the molecular targets of an effective host immune response to Mycobacterium tuberculosis, including understanding the specific immune responses associated with tuberculosis (TB) disease progression, disease resolution, and the development of latency. One application of such tools is the development of diagnostic reagents and assays useful as a test of cure. Such a test could be of considerable importance for the evaluation of new therapeutics. We and others have previously described immunodominant proteins of M. tuberculosis, including both vaccine and diagnostic candidates. In the present study, we describe the changes in immune responses to a panel of 71 M. tuberculosis antigens in six patients during the course of therapy. The levels of six cytokines were measured in 24-h whole-blood assays with these antigens, revealing that gamma interferon (IFN-γ), tumor necrosis factor (TNF), and interleukin-10 (IL-10) were differentially regulated in response to a subset of antigens. Therefore, measuring the production of these three cytokines in response to a panel of carefully selected M. tuberculosis proteins during the course of TB therapy might be a promising path toward the development of a test of cure and warrants further validation in larger cohorts of pulmonary TB patients.
INTRODUCTION
Tuberculosis (TB) caused by Mycobacterium tuberculosis complex bacilli is one of the leading causes of death worldwide (42). Upon exposure to M. tuberculosis, 30 to 40% of close contacts will develop TB infection, of whom 5% would be expected to develop active disease within a 24-month period while the other 95% enter a state of controlled latent TB infection (LTBI), which can reactivate later in life following decreased immunocompetence of the host. T cells, both CD4+ and CD8+, and the cytokines gamma interferon (IFN-γ) and tumor necrosis factor (TNF) play important roles in the prevention of active disease and the control of LTBI, as demonstrated by gene-knockout animal models and human subjects with mutations affecting the expression of these two cytokines (17).
The traditional diagnosis of active TB disease relies on positive identification of acid-fast bacilli (AFB) in a sputum smear or M. tuberculosis identified in culture and is supported by delayed-type hypersensitivity reactions to intradermal injection of M. tuberculosis-specific and nonspecific purified protein derivative (PPD). The tuberculin skin test (TST) utilizes PPD and has a number of drawbacks, notably that TST cross-reacts with the Mycobacterium bovis vaccine strain bacillus Calmette-Guérin (BCG) and other environmental mycobacteria, increasing the number of false positives (37). As IFN-γ is required for a T helper 1 (Th1) response to M. tuberculosis, this cytokine has been measured ex vivo in serum (35, 39), sputum (35), bronchoalveolar lavage fluid (4), pleural effusions of TB patients (21, 25), or culture supernatants of peripheral blood mononuclear cells (PBMC) after in vitro stimulation with M. tuberculosis antigens (2, 18, 40). IFN-γ responses to antigen stimulation are easily induced in PBMC or whole blood and can be detected using simple technologies, such as enzyme-linked immunosorbent assay (ELISA) or enzyme-linked immunosorbent spot assay (ELISPOT), since IFN-γ is not labile and is usually produced in measurable quantities. Differences in the levels of IFN-γ measured in culture supernatants of stimulated lymphocytes from TB patients and controls varied considerably depending on the study and were inconclusive as a diagnostic tool (40), probably due to nonstandardized sample handling and variable duration of stimulation with M. tuberculosis antigens (13).
More recently, standardized short (<24 h) peripheral blood T-cell IFN-γ responses to three M. tuberculosis-specific antigens, early secreted antigenic target 6 (ESAT-6), culture filtrate protein 10 (CFP-10), and antigen TB7.7 (Rv2654), have been investigated for the management of TB. Two assays, the ELISPOT assay T-SPOT.TB (Oxford Immunotec, Oxford, United Kingdom) that uses PBMC and the ELISA QuantiFERON-TB gold (Cellestis, Victoria, Australia) that uses whole blood, measure IFN-γ responses to overlapping ESAT-6/CFP-10 peptides and ESAT-6/CFP-10/TB7.7, respectively, in less than 24 h. It was reported that the number of ESAT-6/CFP-10-specific IFN-γ-producing cells in circulating PBMC reflects bacterial load and the relative risk for pathology and illness. While both assays have advanced the diagnosis of latent TB infection, their utility in monitoring immune responses during the course of chemotherapy for active TB disease and in correlating IFN-γ levels after antigen stimulation with the decrease in bacterial load has yet to be confirmed (12). The results obtained to date from a small number of studies using these two assays are controversial for both active TB and LTBI. Some of these studies report decreased IFN-γ responses to specific mycobacterial antigens (1, 8, 10, 20, 26, 28, 33, 34, 36) during and after chemotherapy, while others have shown persistently positive or even stronger responses with chemotherapy (3, 16, 31, 38, 41, 43). Decreases in IFN-γ responses to CFP-10 during treatment appeared to correlate better with reduction in bacterial loads than analogous responses to ESAT-6 or ESAT-6 and CFP-10 combined (9, 14, 27). Host immune responses to M. tuberculosis antigens during therapy are complex, dynamic events that will likely require the measure of more than one parameter—cytokine and/or antigen. It has been suggested that the IFN-γ/IL-10 ratio might be used to successfully predict the development of active disease after exposure to TB (24). In addition, Eum et al. recently showed that the regulation of TNF during therapy might be better than IFN-γ in predicting sputum conversion at 6 months (15).
The identification of surrogate markers of bacterial clearance in TB patients receiving chemotherapy is important for a number of reasons, including early diagnosis of treatment efficacy, prevention of relapse due to incomplete cure, and as endpoints in clinical trials evaluating new tuberculosis medications (22). The objective of this study was to identify in pulmonary TB patients surrogate markers for successful response to therapy by characterizing the dynamic of cytokine responses to a large array of M. tuberculosis antigens before, during, and after completion of treatment. For that purpose, cytokines associated with Th1, Th2, and Th17 were analyzed. The levels of IFN-γ, TNF, interleukin-10 (IL-10), IL-5, IL-2, and IL-17 were characterized in whole blood after <24 h of stimulation with PPD, M. tuberculosis lysate (MtbL), ESAT-6, and 70 additional recombinant M. tuberculosis proteins, including both secreted and latency antigens.
MATERIALS AND METHODS
Study subjects.
TB patients (n = 6), recruited at the TB Control Program, Public Health—Seattle & King County (Seattle, WA), were assessed for cytokine profiles during therapy using M. tuberculosis antigen-stimulated whole-blood cultures. The study was approved by the Human Subjects Review Committee of the University of Washington, and written informed consent was obtained from each study subject. All six patients were diagnosed with active pulmonary TB by sputum culture, were PPD positive (indurations of >10 mm), and were negative for human immunodeficiency virus (HIV) and hepatitis B and hepatitis C viruses. Four patients had a history of BCG vaccination, one did not, and the status of one patient was unknown. The mean age was 32.8 years (range, 19 to 49), and the male/female ratio was 5:1. Each patient was given the standard 6 months of directly observed therapy (DOT) for TB, which consisted of a combination of at least two of the following drugs: isoniazid, rifampin, ethambutol, pyrazinamide or rifamate (a combination of isoniazid and rifampin). Each patient was initially treated with standard short-course therapy according to the guidelines of the American Thoracic Society and Centers for Disease Control and Prevention (7), consisting of a 2-month intensive phase with four drugs (isoniazid, rifampin, ethambutol, and pyrazinamide) and 4 months of isoniazid and rifampin. One patient (TBC-04) harbored a multidrug-resistant M. tuberculosis strain that was resistant to both isoniazid and rifampin and was treated with an alternative regimen for 18 months. All patients had converted to culture negative at the end of the treatment and were considered adequately treated. In addition, healthy PPD-negative subjects (n = 7) with no history of BCG vaccination were included as controls.
Reagents.
M. tuberculosis PPD (lot P A0814-1) was obtained from Mycos Research LLC (Loveland, CO). Phytohemagglutinin (PHA) was purchased from Sigma (Sigma-Aldrich, St. Louis, MO). Target M. tuberculosis recombinant His-tagged proteins were prepared in Tris buffer as previously described (5), and all showed residual endotoxin levels of <100 endotoxin units (EU)/mg of protein.
Whole-blood assay.
At the time of enrollment in the study, patients had been started on chemotherapy for <2 weeks. Blood samples were drawn into heparinized Vacutainers (BD Biosciences, San Jose, CA) between the hours of 10 a.m. and 2 p.m. at the initial visit (time zero [T0]) and at 2 weeks (T0.5) and 1, 3, 6, 9, and 12 months (T1, T3, T6, T9, and T12) thereafter. Blood (20 ml) was diluted 1:1 with sterile RPMI 1640 (Invitrogen) tissue culture medium. Diluted blood (450 μl/well) was plated in 48-well tissue culture plates within 2 h of collection. Blood cultures were stimulated with 50 μl/well of Tris buffer, 10 μg/ml PPD, 10 μg/ml PHA, 10 μg/ml MtbL, or 10 μg/ml of each recombinant protein of M. tuberculosis (Table 1) for 20 to 22 h at 37°C in 5% CO2. Culture supernatants were harvested and stored for later use in separate polypropylene plates as three 100-μl aliquots at −80°C.
Table 1.
Categories of selected M. tuberculosis antigens
| Category | Antigens |
|---|---|
| Secreted/membrane | Rv0125, Rv0153c, Rv0164, Rv0390, Rv0455c, Rv0496, Rv0577, Rv0733, Rv0909, Rv1411, Rv1511, Rv1626, Rv1827, Rv1860, Rv1926c, Rv1980c, Rv1984c, Rv2031, Rv2220, Rv2873, Rv2875, Rv3029c, Rv3881, Ag85B |
| PE/PPE protein family | Rv0915, Rv1789, Rv1818c, Rv2608, Rv3478 |
| EsX protein family | Rv0287, Rv1793, Rv3619, Rv3620c, ESAT-6 |
| Database | Rv0952, Rv1009, Rv1174, Rv1211, Rv1253, Rv1270c, Rv1288, Rv1884c, Rv2389c, Rv2450, Rv3204, Rv3407 |
| Latency | |
| Growth in macrophage | Rv0467, Rv0523c, Rv0655, Rv0716, Rv1099, Rv1397c, Rv1410c, Rv1569, Rv1589, Rv1590, Rv3541c, Rv3587 |
| Hypoxia | Rv1240, Rv1738, Rv1813c, Rv2032, Rv2428, Rv2558, Rv2624c, Rv2626c, Rv2801c, Rv3044, Rv3129c, Rv3130, Rv3810 |
Cytokine determination by Luminex.
Supernatants were filtered through 1.2-μm and 0.2-μm filters to remove possible M. tuberculosis bacilli. The filtrates were analyzed for IL-2, IL-5, IL-10, IL-17, IFN-γ, and TNF cytokine production using a customized human 6-plex Procarta cytokine assay kit (Affymetrix, Santa Clara, CA), following the directions of the manufacturer. Samples were read on a Luminex 200 (Luminex Corporation, Austin, TX) machine powered by the MasterPlex Software Suite program and analyzed using the MasterPlex QT 3.0 (MiraiBio, Inc., Alameda, CA) quantification software in order to obtain cytokine concentration values. The sensitivities and ranges of the assays were determined by running a dose-response curve of a reference standard for each cytokine from the manufacturer on each plate.
Data analyses.
All data were analyzed by using MasterPlex QT 3.0 and Microsoft Excel. Antigen-specific cytokine responses are shown after subtraction of the spontaneous cytokine secretion that occurs in the absence of a stimulant. A macro was written with Microsoft Excel to convert cytokine levels from pg/ml or fold change to colored heat maps. Comparison of the levels of IFN-γ and IL-10 or those of TNF and IL-10 were provided as differences rather than ratios to account for zero values where present. Intra-assay variation was initially calculated for each cytokine at the T0 and T6 time points on duplicate wells of cells stimulated with PHA, PPD, ESAT-6, or antigen 85B (Ag85B). The intra-assay cytokine variation averaged 1.1 ± 0.3 (mean ± standard deviation [SD]; range, 1.0 to 1.5). There were no statistically significant differences observed between stimulants or cytokines, as determined using a 1-way analysis of variance (ANOVA) test. A cutoff for fold-change cytokine expression compared to the expression at T0 was considered different when greater than the absolute value of 2 (averagevariation + 3 × SDvariation).
RESULTS
To explore whether changes in cytokine responses to defined M. tuberculosis antigens would provide a surrogate marker for sputum smear and culture conversion, whole blood was obtained from six pulmonary TB subjects during the course of chemotherapy. The blood samples were stimulated for 24 h with an extensive panel of 71 single M. tuberculosis proteins, including ESAT-6 and Ag85B, and PPD. The levels of cytokines associated with Th1/effector (IFN-γ and TNF), memory (IL-2), regulatory (IL-10), Th2 (IL-5), and Th17 (IL-17) cells were measured in culture supernatant with the Luminex technology.
Profile of cytokine responses to M. tuberculosis antigens at initiation and end of therapy.
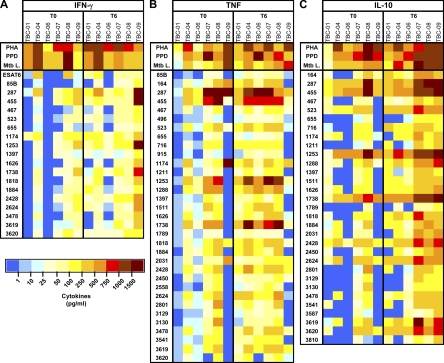
Whole-blood cells' cytokine responses to M. tuberculosis antigen stimulation were initially compared at the beginning (T0) and end (T6) of therapy (see Fig. S1 in the supplemental material). While the six cytokines were upregulated in all patients in response to PHA stimulation, indicating that active disease did not inhibit cytokine responses, only IFN-γ, TNF, IL-10, and IL-2 were increased in response to PPD and MtbL. Furthermore, cytokine responses to single M. tuberculosis antigens were mostly restricted to IFN-γ, TNF, and IL-10. Based on these observations, we focused our analyses on a subset of M. tuberculosis antigens that induced antigen-specific cytokine responses of >25 pg/ml in four of six patients (67%) at T6 for one or more of the latter three cytokines (Fig. 1). Nineteen, 33, and 31 M. tuberculosis antigens met these criteria for IFN-γ (Fig. 1A), TNF (Fig. 1B), and IL-10 (Fig. 1C), respectively. Interestingly, among these M. tuberculosis antigens, 17 upregulated all three cytokines, 12 more were associated with increases in TNF and IL-10 responses, and one was associated with IFN-γ and TNF responses. When concentrations of effector (IFN-γ and TNF) versus regulatory (IL-10) cytokines were compared, the IL-10 levels were generally higher than the IFN-γ and TNF levels for most M. tuberculosis antigens and TB subjects at both T0 and T6, resulting in net negative values (Table 2). In addition, there was a trend for a greater IL-10 than IFN-γ response detected at T6 compared to their levels at T0 (T6 value < T0 value).
Fig. 1.
Heat map of whole-blood cytokine responses to a subset of M. tuberculosis antigens recognized by two-thirds of the subjects. Whole blood was obtained from six TB patients at time 0 (T0) and 6 months (T6) of antibiotic treatment and stimulated with Tris buffer, PHA, PPD, MtbL, or an individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ, TNF, and IL-10 were measured using multiplexing ELISA. Antigen-specific cytokine concentrations are represented in a heat map from blue (>1 pg/ml) to dark brown (>1,500 pg/ml).
Table 2.
Differences between plasma levels of IFN-γ effector and IL-10 regulatory cytokines with stimulation by various M. tuberculosis antigens
| Cytokine pair measured and M. tuberculosis antigen used | Amt of IFN-γ or TFN − amt of IL-10 (pg/ml) in patient at indicated time pointa |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TBC-01 |
TBC-04 |
TBC-06 |
TBC-07 |
TBC-08 |
TBC-09 |
|||||||
| T0 | T6 | T0 | T6 | T0 | T6 | T0 | T6 | T0 | T6 | T0 | T6 | |
| IFN-γ − IL-10 | ||||||||||||
| PHA | 580 | 1182 | −761 | −556 | −223 | 456 | −261 | 4380 | −542 | −565 | −2933 | −3350 |
| PPD | 600 | 110 | 3714 | 1895 | −331 | −462 | −1166 | −1046 | 49 | −1781 | −641 | −1412 |
| MtbL | 620 | 315 | 4402 | 1726 | −25 | −187 | −612 | −915 | 551 | −1327 | −428 | −1380 |
| ESAT-6 | 7 | 69 | 324 | 179 | 0 | 0 | −2 | −19 | 250 | 8 | 16 | 36 |
| Ag85B | 0 | 0 | 24 | 25 | 0 | 0 | 5 | −71 | −58 | −91 | 23 | 15 |
| Rv0287 | −139 | −387 | −76 | −46 | −488 | −249 | −498 | −1400 | −853 | −1209 | 58 | 82 |
| Rv0455 | −114 | −406 | −243 | −491 | −594 | −445 | −993 | −1703 | −1030 | −1608 | −107 | −267 |
| Rv0467 | −62 | −83 | 20 | −15 | 0 | −86 | −116 | −156 | −76 | −163 | 65 | −132 |
| Rv0523 | −84 | −356 | −200 | −367 | −174 | −317 | −553 | −779 | −232 | −574 | 86 | −438 |
| Rv0655 | 0 | 6 | 11 | 27 | 0 | −19 | 3 | −109 | −24 | −165 | 5 | −69 |
| Rv1174 | −18 | 204 | −44 | 83 | 0 | −125 | −267 | −418 | 65 | −147 | 105 | −117 |
| Rv1253 | −35 | −395 | −549 | −783 | −647 | −624 | −801 | −1417 | −1136 | −1668 | −203 | −189 |
| Rv1397 | −42 | −90 | 32 | 5 | 0 | −20 | −64 | −239 | −83 | −247 | 15 | −54 |
| Rv1626 | −37 | −175 | −84 | −193 | 0 | −151 | −215 | −381 | −127 | −381 | 75 | −245 |
| Rv1738 | −88 | −519 | −410 | −570 | −286 | −630 | −662 | −1575 | −831 | −1981 | −351 | −473 |
| Rv1818 | −50 | −178 | 85 | −184 | 0 | −115 | −918 | −823 | −164 | −297 | 50 | −85 |
| Rv1884 | −24 | −85 | −62 | −54 | 0 | −23 | −568 | −241 | −328 | −621 | 80 | −82 |
| Rv2428 | −130 | −182 | −250 | −378 | −72 | −459 | −289 | −775 | −217 | −461 | −75 | −319 |
| Rv2624 | −57 | −298 | −226 | −334 | 0 | −256 | −322 | −789 | −352 | −671 | 13 | −170 |
| Rv3478 | 0 | −80 | −146 | −44 | 0 | −55 | −215 | −316 | −30 | −222 | 51 | −42 |
| Rv3619 | −24 | −173 | −137 | −264 | 0 | −234 | −254 | −905 | −393 | −443 | 63 | −312 |
| Rv3620 | −79 | −302 | 28 | −295 | 0 | −246 | −163 | −869 | −190 | −583 | −180 | −749 |
| TNF − IL-10 | ||||||||||||
| PHA | 33 | −233 | −3643 | −6254 | −358 | 111 | 1226 | 1274 | −889 | −1074 | −376 | −2192 |
| PPD | −58 | 29 | −50 | 130 | −305 | 257 | −729 | −1007 | −606 | −1190 | 1199 | −1373 |
| MtbL | −18 | −39 | −126 | −213 | −250 | −234 | 76 | −1045 | −295 | −1064 | 2989 | −883 |
| Ag85B | 0 | 20 | 10 | 59 | 1 | 30 | 0 | −60 | −24 | −49 | 0 | −161 |
| Rv0164 | −38 | −248 | 64 | 30 | 11 | 0 | −348 | −332 | −58 | −201 | 564 | −382 |
| Rv0287 | −132 | −186 | 21 | 1114 | −338 | 730 | −799 | −444 | 35 | −539 | 862 | −761 |
| Rv0455 | −106 | −213 | −21 | 343 | −466 | 264 | −1284 | −879 | −2 | −696 | −463 | −1238 |
| Rv0467 | −59 | −39 | 89 | 91 | 3 | −41 | −148 | −32 | 20 | −4 | 0 | −249 |
| Rv0496 | 1 | 11 | 5 | 35 | 1 | 39 | 0 | 31 | −3 | −49 | 0 | −77 |
| Rv0523 | −78 | −256 | −55 | −81 | −151 | −199 | −713 | −594 | −45 | −310 | 31 | −639 |
| Rv0655 | 1 | 37 | 3 | 18 | 0 | 17 | 0 | −118 | 18 | −115 | 0 | −155 |
| Rv0716 | −18 | −163 | 31 | −5 | 1 | 14 | −377 | −150 | −35 | −73 | 0 | −169 |
| Rv0915 | 0 | 9 | 15 | 71 | 0 | 30 | −31 | 14 | −8 | −22 | 0 | −194 |
| Rv1174 | −72 | 102 | 21 | 122 | 12 | −66 | −423 | −218 | 48 | 0 | 1463 | 29 |
| Rv1211 | 1 | −65 | 69 | 129 | 3 | 15 | −123 | −56 | 14 | −55 | 0 | −295 |
| Rv1253 | −34 | −174 | −173 | 625 | −553 | −133 | −1130 | −471 | −236 | −80 | −528 | −1280 |
| Rv1288 | −36 | −84 | 52 | 197 | 53 | 439 | −317 | −201 | 98 | 3 | −40 | −869 |
| Rv1397 | −41 | −76 | 12 | 54 | 5 | 126 | −84 | −202 | −22 | −140 | 0 | −217 |
| Rv1511 | −58 | −127 | 40 | 90 | 14 | 207 | −140 | −179 | −24 | −167 | 0 | −312 |
| Rv1626 | −34 | −125 | 26 | −7 | 12 | −80 | −301 | −156 | −43 | −139 | 0 | −569 |
| Rv1738 | −82 | −203 | −164 | 404 | −238 | −108 | −924 | −779 | −293 | −922 | −613 | −1283 |
| Rv1789 | 1 | 32 | 26 | 31 | 2 | 45 | −148 | −11 | −24 | −68 | 0 | −140 |
| Rv1818 | −49 | −74 | 75 | 39 | 15 | 12 | −1119 | −573 | 136 | −25 | 103 | −376 |
| Rv1884 | −24 | −91 | −54 | 220 | 36 | 116 | −848 | −179 | −7 | −227 | 0 | −259 |
| Rv2031 | −38 | 31 | −56 | −28 | 9 | −28 | −382 | −345 | 3 | −81 | 597 | −385 |
| Rv2428 | −122 | −83 | −72 | 51 | −47 | −282 | −440 | −482 | 32 | −180 | −226 | −739 |
| Rv2450 | −41 | 32 | 65 | −81 | 8 | 8 | −262 | −88 | −3 | −144 | 0 | −520 |
| Rv2558 | 0 | 21 | 4 | 25 | 0 | 59 | 0 | −233 | 39 | −87 | 0 | −140 |
| Rv2624 | −54 | −51 | −99 | 48 | 15 | −94 | −462 | −621 | −68 | −200 | −132 | −682 |
| Rv2801 | 2 | −134 | 69 | 113 | 24 | 20 | −457 | −234 | −52 | −159 | 0 | −206 |
| Rv3129 | 1 | 11 | 10 | 70 | 4 | 4 | −186 | −365 | 23 | −67 | 0 | −140 |
| Rv3130 | 1 | 8 | 18 | 96 | 12 | 12 | −676 | −171 | 110 | −26 | 0 | −217 |
| Rv3478 | 2 | −23 | −73 | 146 | 13 | −2 | −303 | −36 | 11 | −24 | 0 | −315 |
| Rv3541 | −48 | −110 | 15 | 64 | 9 | 104 | −199 | −244 | 2 | −114 | 0 | −304 |
| Rv3619 | −21 | −128 | −58 | 108 | 10 | −131 | −338 | −733 | 27 | −212 | 0 | −667 |
| Rv3620 | −78 | −271 | 26 | −123 | 13 | −276 | −171 | −825 | −174 | −583 | −209 | −856 |
Whole blood was obtained from six TB patients at time zero (T0) and 6 months (T6) of antibiotic treatment and stimulated with individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ or TNF and IL-10 were measured using multiplexing ELISA. A negative value indicates a higher level of IL-10 than of IFN-γ or TNF.
Kinetics of cytokine responses to M. tuberculosis antigens during chemotherapy.
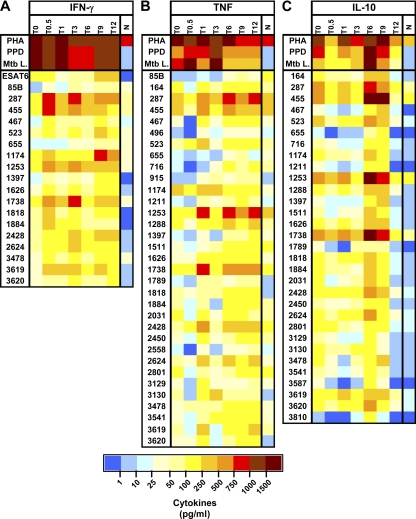
Whole-blood samples were obtained at T0, T0.5 (2 weeks), and T1, T3, T6, T9, and T12 (months) after the initiation of therapy and stimulated for 24 h with the subset of stimulating M. tuberculosis antigens identified in the experiments discussed above (Fig. 1). Plasma levels of IFN-γ, TNF, and IL-10 were measured and averaged for the six patients at each time point. For IFN-γ, the cytokine level associated with each single M. tuberculosis antigen was either maintained or increased at all the other time points except T0 (Fig. 2 A). This observation is of particular interest as it suggests that blood cells from TB subjects already become more responsive to antigen-specific stimulation within 2 weeks after starting on antibiotics. In comparison, IFN-γ levels measured from blood cells of PPD-negative healthy controls were low (<50 pg/ml, except for Rv0287 and Rv0455). The TNF levels in response to M. tuberculosis antigen stimulation seemed generally higher at the later time points, T6 through T12 (Fig. 2B), with the exception of Rv0287, Rv0455, Rv1174, Rv1253, Rv1288, Rv1738, and Rv2428, which induced strong TNF responses at all time points, as well as in healthy controls. Responses to these M. tuberculosis antigens in healthy controls are probably due to homology with and exposure to environmental nontuberculous mycobacteria. Likewise, the highest IL-10 responses were generally observed at T6 and T9, with Rv0287, Rv0455, Rv1253, and Rv1738 inducing IL-10 levels of >500 pg/ml (Fig. 2C). At T12, however, the IL-10 responses resemble those of healthy controls. It appears that secretions of TNF and IL-10 have both more similar kinetics and more reactive M. tuberculosis antigen subsets than those of IFN-γ and IL-10.
Fig. 2.
Kinetics of whole-blood cytokine responses to a subset of M. tuberculosis antigens. Whole blood was obtained from six TB patients at time 0 (T0), 2 weeks (T0.5), and 1 (T1), 3 (T3), 6 (T6), 9 (T9), and 12 months (T12) of antibiotic treatment and from seven PPD-negative healthy controls (N) and stimulated with Tris buffer, PHA, PPD, MtbL, or an individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ, TNF, and IL-10 were measured using multiplexing ELISA. At each time point, data from the six subjects were averaged for a given in vitro stimulation and color coded depending on cytokine concentration.
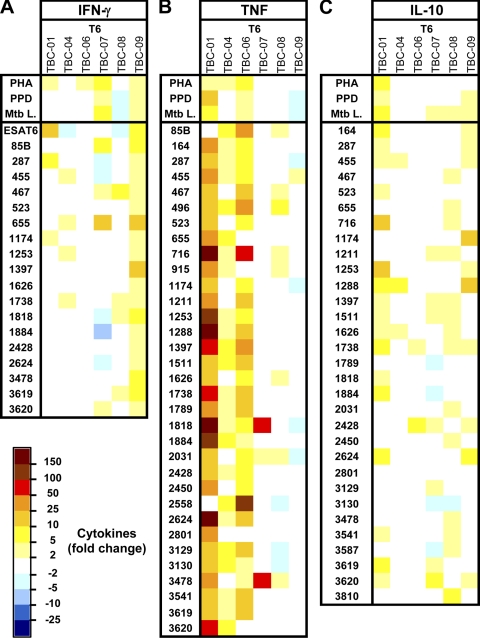
Quantitative changes in cytokine responses to M. tuberculosis antigens during chemotherapy.
In the experiments discussed above, we identified a subset of 36 M. tuberculosis antigens inducing IFN-γ, TNF, and/or IL-10 responses in the blood of two-thirds of the TB subjects. We further examined whether cytokine response(s) to some of these M. tuberculosis antigens changed during the course of therapy (Fig. 3 and Fig. S2).
Fig. 3.
Fold changes in cytokine responses to a subset of M. tuberculosis antigens 6 months into antibiotic therapy. Whole blood was obtained from six TB patients at time 0 (T0) and 6 months (T6) of antibiotic treatment and stimulated with Tris buffer, PHA, PPD, MtbL, or an individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ, TNF, and IL-10 were measured using multiplexing ELISA. Increases (positive fold change) or decreases (negative fold change) in cytokine responses at T6 compared to the data at T0 are shown and color coded based on intensity.
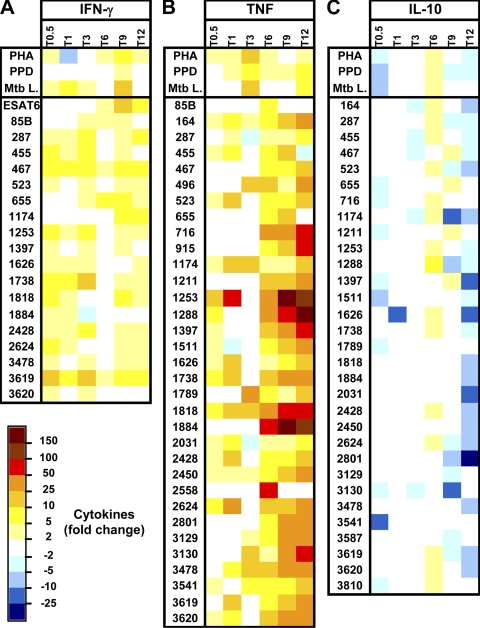
The fold changes in IFN-γ, TNF, and IL-10 responses to the subset of 36 M. tuberculosis antigens over the period from T0 to T6 were first calculated for each subject. Among the 19 M. tuberculosis antigens selected, IFN-γ responses to latency antigens Rv467, Rv655, and Rv1738 were upregulated (2- to 25-fold) in 50% of the TB subjects (Fig. 3 A). Similarly, at T6, 25 of the 33 M. tuberculosis antigens initially selected induced increased TNF levels (2- to 150-fold) (Fig. 3B), and 8 of 31 increased IL-10 responses (2- to 25-fold) (Fig. 3C) in 50% of the TB subjects. Finally, a subset of 8 M. tuberculosis antigens did induce positive changes at T6 for at least two cytokines in ≥50% of the patients (Table 3) and might be pursued further as a test of cure. While cytokine responses to some antigens were downregulated at T6 compared to their levels at T0, the occurrence was rare and never occurred in more than one-third of the subjects. Finally, fold changes in cytokine levels during the course of therapy were averaged for the six subjects and presented as a group response at the different time points tested. IFN-γ responses to Rv0467, Rv1738, and Rv3619 were already upregulated 5- to 25-fold at T0.5, while responses to ESAT-6, Ag85B, Rv0655, and Rv1174 increased at T3 or later (Fig. 4 A). TNF responses to all but three antigens were upregulated at T6 and further increased at T9 and/or T12 (Fig. 4B). In addition, 2- to 10-fold changes in TNF responses to Rv0164, Rv1818, and Rv2425 were already occurring at T0.5. Finally, IL-10 responses to most antigens were downregulated, especially at T12 (Fig. 4C).
Table 3.
Increase in IFN-γ, TNF, and IL-10 responses to a subset of M. tuberculosis antigens
| Antigen | % of patients with positive cytokine responsea |
||
|---|---|---|---|
| IFN-γ | TNF | IL-10 | |
| Rv287 | 33 | 50 | 33 |
| Rv455 | 33 | 67 | 50 |
| Rv467 | 50 | 50 | 17 |
| Rv523 | 17 | 33 | 17 |
| Rv655 | 50 | 33 | 17 |
| Rv1174 | 33 | 33 | 17 |
| Rv1253 | 33 | 50 | 33 |
| Rv1288 | 0 | 50 | 50 |
| Rv1397 | 17 | 50 | 50 |
| Rv1511 | 0 | 50 | 50 |
| Rv1626 | 17 | 50 | 50 |
| Rv1738 | 50 | 50 | 67 |
| Rv1818 | 33 | 67 | 17 |
| Rv1884 | 17 | 50 | 17 |
| Rv2428 | 17 | 50 | 50 |
| Rv2624 | 17 | 50 | 33 |
| Rv3478 | 17 | 67 | 17 |
| Rv3619 | 33 | 50 | 33 |
| Rv3620 | 33 | 33 | 50 |
Percentage of patients with positive fold-change cytokine responses to a subset of M. tuberculosis antigens 6 months into antibiotic therapy. Whole blood was obtained from six TB patients at time zero (T0) and 6 months (T6) of antibiotic treatment and stimulated with individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ, TNF, and IL-10 were measured using multiplexing ELISA. Antigens marked in boldface induced positive changes at T6 for at least two cytokines in ≥50% of the patients.
Fig. 4.
Fold changes in cytokine responses to a subset of M. tuberculosis antigens at different times during antibiotic treatment. Whole blood was obtained from six TB patients at time 0 (T0), 2 weeks (T0.5), and 1 (T1), 3 (T3), 6 (T6), 9 (T9), and 12 months (T12) of antibiotic treatment and stimulated with Tris buffer, PHA, PPD, MtbL, or individual recombinant M. tuberculosis protein for 24 h at 37°C. Plasma levels of IFN-γ, TNF, and IL-10 were measured using multiplexing ELISA. Increases (positive fold change) or decreases (negative fold change) in cytokine responses at the different time points compared to the data at T0 were calculated. For each time point and in vitro stimulation, data from the six subjects were averaged and color coded based on intensity.
DISCUSSION
The identification of surrogate markers of bacterial clearance in pulmonary TB patients receiving chemotherapy is a critical step toward early assurance of treatment success and identification of patients at risk of relapse and subsequent transmission of TB to others following short-course TB therapy. These biomarkers may also serve as a surrogate endpoint in clinical trials evaluating new TB medications. In this longitudinal study, we demonstrated that whole-blood cytokine production patterns from pulmonary TB patients vary during standard TB treatment. Blood culture stimulation with a set of 71 recombinant M. tuberculosis proteins and complex antigen mixtures (PPD and MtbL) resulted predominantly in Th1 (IFN-γ and TNF) and regulatory (IL-10) cytokine responses; the levels of Th2 (IL-5)-, Th17 (IL-17)-, and memory (IL-2)-associated cytokines were low to undetectable for most antigens in all subjects. IFN-γ, TNF, and/or IL-10 changes in expression profiles during chemotherapy were associated with a subset of the M. tuberculosis antigens tested.
Diagnosis of active TB relies on clinical criteria, patient history, chest radiography, TST, and confirmation by sputum smear or AFB culture positivity. However, an unexpectedly high number of individuals can be sputum positive (and therefore potentially infectious) without any apparent symptoms, whereas many patients who have significant symptoms remain sputum negative, thus calling this simple definition into question. The recent development of short standardized IFN-γ release assays (QuantiFERON-TB Gold and T-SPOT.TB) based on recall responses to ESAT-6 and/or CFP-10 M. tuberculosis antigens offers new possibilities for the early diagnosis of active TB in adults (11, 32). The use of IFN-γ release assays in assessing treatment efficacy in adults and children, however, has yielded conflicting results, with some studies reporting good correlations between bacterial loads and IFN-γ responses (mainly to CFP-10) (9, 14, 20, 26, 27, 36), while other studies did not (3, 16, 31, 38, 41, 43). Our study confirms the lack of reliability of ESAT-6 as a single marker because only two patients (TBC-04 and TBC-08) of the six tested showed a moderate IFN-γ response to this antigen at T0, while all patients had moderate to strong cytokine responses to M. tuberculosis-specific (PPD and MtbL) and nonspecific (PHA) stimulations. TBC-04 showed an initial increase in IFN-γ 2 weeks into therapy, consistent with previous observations (20), and both TBC-04 and TBC-08 showed further-reduced IFN-γ responses to ESAT-6 from T1 to T6 but returned to T0 levels at T12. A similar kinetic was reported by Dominguez et al. (14). Among the four other patients, one never responded to ESAT-6, and the three others showed mild increases at T3 and onward. It is unclear why these four patients had poor correlations between the presence of bacteria and IFN-γ responses to ESAT-6, but this observation is consistent with the considerable interindividual variation reported across studies in terms of percentage of responders and rate of decline of the response (14). When taken collectively, our data indicate that there are no differences in IFN-γ responses to ESAT-6 during the first 3 months of treatment, followed by a moderate increase thereafter. Furthermore, our screening of 70 additional M. tuberculosis antigens revealed that for a majority of patients, none of these antigens was associated with IFN-γ declines during the course of treatment, while a small subset of antigens (the 15 antigens Ag85B, Rv0287, Rv0455, Rv467, Rv523, Rv0655, Rv1174, Rv1253, Rv1626, Rv1738, Rv1818, Rv1884, Rv2428, Rv2624, and Rv3619) induced higher IFN-γ recall responses at T6 in ≥67% of TB patients. Patient responses to latency antigens were generally low, as previously observed by Leyten et al. (29), except for Rv1738. The relative discrepancy between our Rv1738 data and Leyten's might be explained by the use of whole blood instead of PBMC or by a more restricted definition of TB patients. Antigen stimulation of whole blood has the advantage of capturing the totality of the cellular response compared to that seen in PBMC, where loss of low-frequency cells during the purification process cannot be ruled out. Altogether, these observations suggest that increased rather than decreased IFN-γ responses to a selected subset of M. tuberculosis antigens might better correlate with bacterial load and treatment efficacy. Furthermore, antigen stimulation of whole-blood cultures is a simple method that does not require labor-intensive PBMC purification and that might be more suitable in resource-limited laboratory settings. Nevertheless, further characterization of the T-cell response to these 15 M. tuberculosis antigens and phenotypic analyses at the single-cell level might provide additional information on whether higher IFN-γ responses are associated with increased frequencies of blood antigen-specific circulating effector T cells.
In this study, we hypothesized that short (<24 h) in vitro blood stimulations will target circulating effector rather than memory cells. Consistent with this hypothesis, the levels of IL-2 measured in response to all single M. tuberculosis antigens were low (<100 pg/ml). Positive-control cultures incubated with the mitogen PHA showed elevated levels of IL-2 (500 to 1,500 pg/ml) at all time points, indicating that the lack of IL-2 responses to M. tuberculosis antigens were not due to an overall low T-cell response or cytokine detection problem. The IL-5 and IL-17 levels, as a measure of Th2 and Th17 cell responses, respectively, were also low (<100 pg/ml) for all M. tuberculosis antigens, including PPD and MtbL, in agreement with observations from Hussain et al. (23). As for IL-2, we found IL-5 and IL-17 responses to PHA stimulation (250 to 1,500 pg/ml and 100 to 1,000 pg/ml, respectively). However, PHA-driven IL-2, IL-5, and IL-17 responses were not consistently modulated during the course of therapy. Therefore, the measure of IL-2, IL-5, and IL-17 expression patterns in response to M. tuberculosis antigens or PHA stimulation was not predictive of sputum conversion and therapy outcome.
The ratios of IFN-γ/IL-2 (6, 30) and IFN-γ/IL-10 (24) have also been used with some success in the diagnosis of active TB and/or assessment of therapy outcome. In addition, Eum et al. recently demonstrated that whole-blood TNF levels in response to culture filtrate proteins were uniquely correlated with sputum conversion in patients treated for multidrug-resistant TB (15). However, they reported a decrease in TNF in sputum-negative patients at 6 months, while we observed an increase. Similarly, Harari et al. reported that subjects with active TB had elevated frequencies of antigen-specific (ESAT-6 and CFP-10) TNF-positive CD4 T cells that decreased upon completion of antibiotic treatment (19). The reasons for this difference are still unclear, but it might be related to the M. tuberculosis antigens tested in their and our study. Nevertheless, TNF, IL-10, and IFN-γ responses to M. tuberculosis antigens were the most dynamic and likely to better predict therapy outcomes.
In summary, our results suggest that a subset of defined M. tuberculosis antigens can be used to monitor IFN-γ, TNF, and IL-10 expression patterns associated with sputum conversion in pulmonary TB patients during chemotherapy. However, the sample size in the present study is too small to make a definitive conclusion, and this hypothesis will have to be validated in larger patient cohorts. These studies (i) confirm the relevance of IFN-γ, TNF, and IL-10 expression profiles as an immune signature associated with reduction in bacterial load and (ii) define novel M. tuberculosis antigens with diagnostic potential. Early detection of treatment failure has significant implications for TB control programs, as it may allow the identification of TB patients whose clinical courses need to be reviewed for nonadherence, malabsorption of medications, poor penetration of TB drugs to the affected sites, or drug-resistant TB. Conversely, accurate diagnostics may allow for shortening treatment in early responders and a focusing of resources on patients with a higher likelihood of poor outcome in order to limit the chance of relapses. Accurate biomarkers are urgently needed as surrogate endpoints in clinical trials for evaluating tuberculosis medications, especially phase 2 trials.
ACKNOWLEDGMENTS
This work was supported by National Institutes of Health grant AI-044373 (S.G.R.).
We are thankful to Gregory C. Ireton for discussion and selection of M. tuberculosis antigens, to Jeffrey Guderian, Raodoh Mohamath, Garrett Poshusta, and Jackie Whittle for protein expression and purification, to Qiong Pan and the clinical staff of the TB Control Program, Public Health—Seattle & King County, to Anna Marie Beckmann for regulatory affairs, to Randall F. Howard for reviewing the manuscript, and to Rick Sorensen for heat map display programming.
Footnotes
Supplemental material for this article may be found at http://cvi.asm.org/.
Published ahead of print on 29 June 2011.
REFERENCES
- 1. Aiken A. M., et al. 2006. Reversion of the ELISPOT test after treatment in Gambian tuberculosis cases. BMC Infect. Dis. 6:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Al-Attiyah R., et al. 2006. Cytokine profiles in tuberculosis patients and healthy subjects in response to complex and single antigens of Mycobacterium tuberculosis. FEMS Immunol. Med. Microbiol. 47:254–261 [DOI] [PubMed] [Google Scholar]
- 3. Al-Attiyah R., Mustafa A. S., Abal A. T., Madi N. M., Andersen P. 2003. Restoration of mycobacterial antigen-induced proliferation and interferon-gamma responses in peripheral blood mononuclear cells of tuberculosis patients upon effective chemotherapy. FEMS Immunol. Med. Microbiol. 38:249–256 [DOI] [PubMed] [Google Scholar]
- 4. Barry S. M., Lipman M. C., Bannister B., Johnson M. A., Janossy G. 2003. Purified protein derivative-activated type 1 cytokine-producing CD4+ T lymphocytes in the lung: a characteristic feature of active pulmonary and nonpulmonary tuberculosis. J. Infect. Dis. 187:243–250 [DOI] [PubMed] [Google Scholar]
- 5. Bertholet S., et al. 2008. Identification of human T cell antigens for the development of vaccines against Mycobacterium tuberculosis. J. Immunol. 181:7948–7957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Biselli R., et al. 2010. Detection of interleukin-2 in addition to interferon-gamma discriminates active tuberculosis patients, latently infected individuals, and controls. Clin. Microbiol. Infect. 16:1282–1284 [DOI] [PubMed] [Google Scholar]
- 7. Blumberg H. M., et al. 2003. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am. J. Respir. Crit. Care Med. 167:603–662 [DOI] [PubMed] [Google Scholar]
- 8. Carrara S., et al. 2004. Use of a T cell-based assay for monitoring efficacy of antituberculosis therapy. Clin. Infect. Dis. 38:754–756 [DOI] [PubMed] [Google Scholar]
- 9. Chee C. B., et al. 2007. Latent tuberculosis infection treatment and T-cell responses to Mycobacterium tuberculosis-specific antigens. Am. J. Respir. Crit. Care Med. 175:282–287 [DOI] [PubMed] [Google Scholar]
- 10. Dheda K., et al. 2007. Interpretation of Mycobacterium tuberculosis antigen-specific IFN-gamma release assays (T-SPOT.TB) and factors that may modulate test results. J. Infect. 55:169–173 [DOI] [PubMed] [Google Scholar]
- 11. Dheda K., Udwadia Z. F., Huggett J. F., Johnson M. A., Rook G. A. 2005. Utility of the antigen-specific interferon-gamma assay for the management of tuberculosis. Curr. Opin. Pulm. Med. 11:195–202 [DOI] [PubMed] [Google Scholar]
- 12. Diel R., Loddenkemper R., Nienhaus A. 2010. Evidence-based comparison of commercial interferon-gamma release assays for detecting active TB: a metaanalysis. Chest 137:952–968 [DOI] [PubMed] [Google Scholar]
- 13. Doherty T. M., et al. 2005. Effect of sample handling on analysis of cytokine responses to Mycobacterium tuberculosis in clinical samples using ELISA, ELISPOT and quantitative PCR. J. Immunol. Methods 298:129–141 [DOI] [PubMed] [Google Scholar]
- 14. Dominguez J., et al. 2009. T-cell responses to the Mycobacterium tuberculosis-specific antigens in active tuberculosis patients at the beginning, during, and after antituberculosis treatment. Diagn. Microbiol. Infect. Dis. 63:43–51 [DOI] [PubMed] [Google Scholar]
- 15. Eum S. Y., et al. 2010. Association of antigen-stimulated release of tumor necrosis factor-alpha in whole blood with response to chemotherapy in patients with pulmonary multidrug-resistant tuberculosis. Respiration 80:275–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ferrand R. A., Bothamley G. H., Whelan A., Dockrell H. M. 2005. Interferon-gamma responses to ESAT-6 in tuberculosis patients early into and after anti-tuberculosis treatment. Int. J. Tuberc. Lung Dis. 9:1034–1039 [PubMed] [Google Scholar]
- 17. Flynn J. L., Chan J. 2001. Immunology of tuberculosis. Annu. Rev. Immunol. 19:93–129 [DOI] [PubMed] [Google Scholar]
- 18. Handzel Z. T., et al. 2007. Increased Th1 and Th2 type cytokine production in patients with active tuberculosis. Isr. Med. Assoc. J. 9:479–483 [PubMed] [Google Scholar]
- 19. Harari A., et al. 2011. Dominant TNF-alpha+ Mycobacterium tuberculosis-specific CD4+ T cell responses discriminate between latent infection and active disease. Nat. Med. 17:372–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Herrmann J. L., et al. 2009. Temporal dynamics of interferon gamma responses in children evaluated for tuberculosis. PLoS One 4:e4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hirsch C. S., et al. 2001. Augmentation of apoptosis and interferon-gamma production at sites of active Mycobacterium tuberculosis infection in human tuberculosis. J. Infect. Dis. 183:779–788 [DOI] [PubMed] [Google Scholar]
- 22. Horne D. J., et al. 2010. Sputum monitoring during tuberculosis treatment for predicting outcome: systematic review and meta-analysis. Lancet Infect. Dis. 10:387–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hussain R., et al. 2002. Cytokine profiles using whole-blood assays can discriminate between tuberculosis patients and healthy endemic controls in a BCG-vaccinated population. J. Immunol. Methods 264:95–108 [DOI] [PubMed] [Google Scholar]
- 24. Hussain R., Talat N., Shahid F., Dawood G. 2007. Longitudinal tracking of cytokines after acute exposure to tuberculosis: association of distinct cytokine patterns with protection and disease development. Clin. Vaccine Immunol. 14:1578–1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jalapathy K. V., Prabha C., Das S. D. 2004. Correlates of protective immune response in tuberculous pleuritis. FEMS Immunol. Med. Microbiol. 40:139–145 [DOI] [PubMed] [Google Scholar]
- 26. Katiyar S. K., Sampath A., Bihari S., Mamtani M., Kulkarni H. 2008. Use of the QuantiFERON-TB Gold In-Tube test to monitor treatment efficacy in active pulmonary tuberculosis. Int. J. Tuberc. Lung Dis. 12:1146–1152 [PubMed] [Google Scholar]
- 27. Kobashi Y., et al. 2009. Transitional changes in T-cell responses to Mycobacterium tuberculosis-specific antigens during treatment. J. Infect. 58:197–204 [DOI] [PubMed] [Google Scholar]
- 28. Lalvani A., et al. 2001. Enumeration of T cells specific for RD1-encoded antigens suggests a high prevalence of latent Mycobacterium tuberculosis infection in healthy urban Indians. J. Infect. Dis. 183:469–477 [DOI] [PubMed] [Google Scholar]
- 29. Leyten E. M., et al. 2006. Human T-cell responses to 25 novel antigens encoded by genes of the dormancy regulon of Mycobacterium tuberculosis. Microbes Infect. 8:2052–2060 [DOI] [PubMed] [Google Scholar]
- 30. Millington K. A., et al. 2007. Dynamic relationship between IFN-gamma and IL-2 profile of Mycobacterium tuberculosis-specific T cells and antigen load. J. Immunol. 178:5217–5226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pai M., et al. 2007. Sensitivity of a whole-blood interferon-gamma assay among patients with pulmonary tuberculosis and variations in T-cell responses during anti-tuberculosis treatment. Infection 35:98–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pai M., Riley L. W., Colford J. M., Jr 2004. Interferon-gamma assays in the immunodiagnosis of tuberculosis: a systematic review. Lancet Infect. Dis. 4:761–776 [DOI] [PubMed] [Google Scholar]
- 33. Pathan A. A., et al. 2001. Direct ex vivo analysis of antigen-specific IFN-gamma-secreting CD4 T cells in Mycobacterium tuberculosis-infected individuals: associations with clinical disease state and effect of treatment. J. Immunol. 167:5217–5225 [DOI] [PubMed] [Google Scholar]
- 34. Ribeiro S., et al. 2009. T-SPOT.TB responses during treatment of pulmonary tuberculosis. BMC Infect. Dis. 9:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ribeiro-Rodrigues R., et al. 2002. Sputum cytokine levels in patients with pulmonary tuberculosis as early markers of mycobacterial clearance. Clin. Diagn. Lab. Immunol. 9:818–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sauzullo I., et al. 2009. In vivo and in vitro effects of antituberculosis treatment on mycobacterial interferon-gamma T cell response. PLoS One 4:e5187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Snider D. E., Jr 1985. Bacille Calmette-Guerin vaccinations and tuberculin skin tests. JAMA 253:3438–3439 [PubMed] [Google Scholar]
- 38. Ulrichs T., Anding R., Kaufmann S. H., Munk M. E. 2000. Numbers of IFN-gamma-producing cells against ESAT-6 increase in tuberculosis patients during chemotherapy. Int. J. Tuberc. Lung Dis. 4:1181–1183 [PubMed] [Google Scholar]
- 39. Vankayalapati R., et al. 2003. Serum cytokine concentrations do not parallel Mycobacterium tuberculosis-induced cytokine production in patients with tuberculosis. Clin. Infect. Dis. 36:24–28 [DOI] [PubMed] [Google Scholar]
- 40. Veenstra H., et al. 2007. Changes in the kinetics of intracellular IFN-gamma production in TB patients during treatment. Clin. Immunol. 124:336–344 [DOI] [PubMed] [Google Scholar]
- 41. Vekemans J., et al. 2001. Tuberculosis contacts but not patients have higher gamma interferon responses to ESAT-6 than do community controls in The Gambia. Infect. Immun. 69:6554–6557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. WHO 2007. Global tuberculosis control: surveillance, planning, financing, vol. 376. World Health Organization, Geneva, Switzerland [Google Scholar]
- 43. Wu-Hsieh B. A., et al. 2001. Long-lived immune response to early secretory antigenic target 6 in individuals who had recovered from tuberculosis. Clin. Infect. Dis. 33:1336–1340 [DOI] [PubMed] [Google Scholar]