Abstract
We have previously described heterotypic peptides from parainfluenza virus that potently inhibit Nipah virus in vitro but are not efficacious in vivo. In contrast, our second-generation inhibitors, featuring a cholesterol moiety, are also efficacious in vivo. The difference between in vitro and in vivo results led us to investigate the basis for this discrepancy. Here, we compare the activities of the compounds in standard laboratory cells and in cells relevant to the natural tropism of Nipah virus, i.e., primary neurons, and show that while our first-generation inhibitors are poorly active in primary neurons, the cholesterol-conjugated compounds are highly potent. These results highlight the advantage of evaluating antiviral potency in cells relevant to natural host target tissue.
TEXT
Nipah virus (NiV) is an emerging virus that was first isolated in Malaysia in 1998-1999 from patients with viral encephalitis and belongs to the henipavirus genus of the paramyxoviridae family (25). The virus is highly pathogenic in humans, with a 40% to 75% mortality rate (reviewed in reference 11), and shows an exceptionally broad host range, with infection occurring predominantly in two cell types: neurons and endothelial cells (3, 7, 26). NiV is an enveloped virus with two surface glycoproteins, G and F, that mediate entry into the host cell. The G protein binds to its cellular receptor: Ephrin B2 or Ephrin B3 (2, 14, 15). As we have shown for other paramyxoviruses, the receptor-bound G protein activates the F protein, which then mediates fusion between the viral and the host cell membranes (18, 19).
NiV has been causing outbreaks with increasing frequency and with well-documented human-to-human transmission (8, 9, 12). Despite the recent development of potential antiviral treatments by us and others, the almost universal failure of in vivo treatments with outstanding in vitro characteristics (5, 6, 20, 24) prompted us to examine potential reasons for this discrepancy. Our method uses the genes encoding envelope glycoproteins derived from a target virus to quickly assess potential reagents that can be used as antivirals (20). Importantly, we then use this method in cells that are biologically relevant to virus infection in the host. We have previously shown that there are considerable differences in the replication characteristics of another paramyxovirus, human parainfluenza virus type 3 (HPIV3), between standard laboratory cells and primary tissues more representative of the natural host system (21). In the current study, we have assessed in vitro antiviral efficacy in primary neurons, an established target tissue for NiV infection in vivo, to determine whether the properties of the natural host cell modulate the effect of antiviral compounds.
Multicycle pseudotyped viral entry assay for NiV in primary neurons.
To mimic multicycle viral infection under BSL2 conditions, we used NiV envelope glycoproteins pseudotyped onto a recombinant vesicular stomatitis virus (VSV) that expresses red fluorescent protein (RFP) but lacks its attachment protein, G, designated VSV-ΔG-RFP-NiV G/F (20). The resulting pseudotyped virus bears the NiV binding and fusion proteins. The infection of target cells is quantified by the production of red fluorescence. This pseudotyped viral entry assay, unlike previous ones (27), simulates multicycle replication because the monolayer cells that express viral glycoproteins will generate additional cycles of pseudotyped particles when infected. In contrast, traditional pseudotyped viral entry assays can assess only one entry event. In the experiment represented in Fig. 1, primary neurons from combined hippocampal, cortex, and ventricular cells from day 18 embryonic Sprague/Dawley rat brains (Neuromics) were digested with 2 mg/ml of papain and then cultured in 96-well plates. After 3 days, cells were transfected with plasmids encoding NiV G/F as well as yellow fluorescent protein (YFP) (to monitor the transfection efficiency). On the following day, these G/F-expressing cells were infected with NiV pseudotyped viruses bearing RFP. Figure 1 shows neurons that have been transfected and infected. Panel A shows the microscopic image with visible light, and panels B and C show fluorescent images of the same field. In panel B, RFP expression indicates infection. In panel C, YFP provides an indication of transfection efficiency. The results show 40% transfection efficiency and intermediate levels of virus infection, essential for sustaining subsequent rounds of replication. In the experiment represented in panel D, primary neurons in 96-well plates, either untransfected or transfected with viral glycoproteins (G/F), were incubated with pseudotyped NiV. The plates were incubated at 37°C for 96 h, and fluorescence was measured. While the maximum difference between untransfected and transfected neurons is seen at lower numbers of PFU, the highest fluorescence intensities are in transfected neurons infected with 12,500 PFU (a multiplicity of infection [MOI] of 0.125). The use of this intermediate number of PFU allows multicycle replication to be evident, sparing the majority of cells from the initial round of infection so that they may be infected during later cycles. As expected in untransfected neurons, the fluorescence intensity is directly proportional to the amount of viral infection (Fig. 1D, squares). The assay is reliably quantitative over a wide range of quantities of PFU/well, from approximately 3,125 to 25,000 PFU, providing a suitable platform with which to evaluate decreases in viral replication in the presence of inhibitors. The differentiation and transfection of primary neurons was performed using previously established protocols (1, 4, 10, 13, 28), and the transfection efficacy was assessed by YFP expression (see also Fig. S1 in the supplemental material).
Fig. 1.
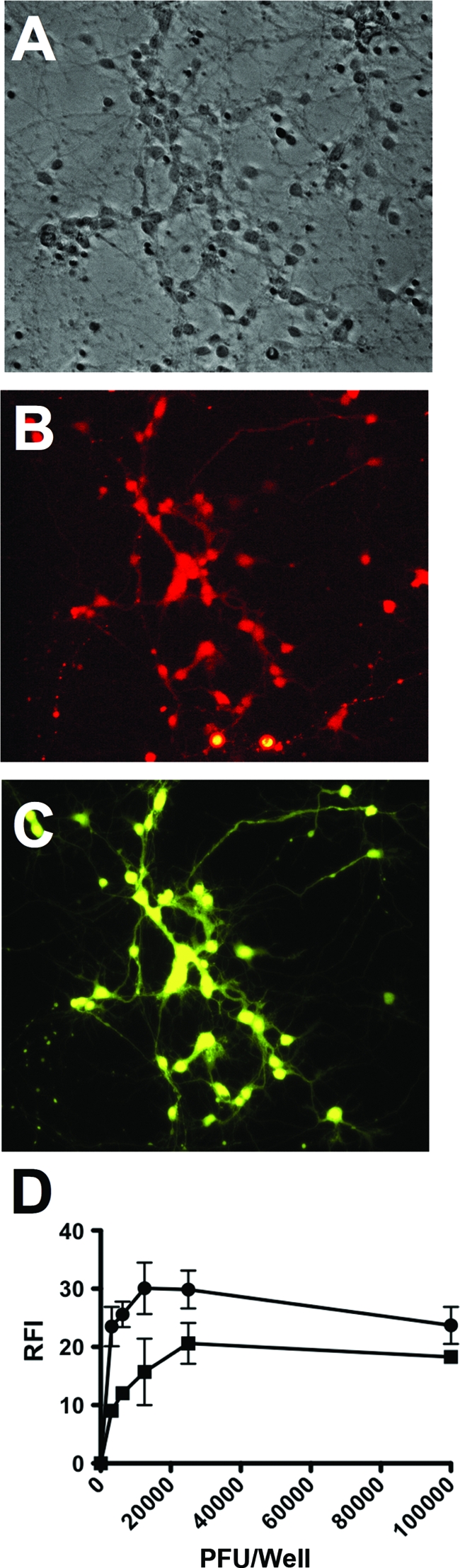
Transfection and infection of primary neurons with pseudotyped NiV. Panel A shows neurons transfected with NiV G/F and then infected with pseudotyped NiV. Panel B shows fluorescence (RFP) in neurons due to infection with RFP-expressing NiV pseudotyped viruses. Panel C shows fluorescence in neurons reflecting transfection with YFP. In panel D, pseudotyped NiV expressing RFP (numbers of PFU/well; x axis) were used to infect transfected (circles) or untransfected (squares) neurons. At 72 h postinfection, the relative fluorescence intensity (RFI) of the RFP was measured (y axis). The data represent 3 replicates, with standard deviations.
Fusion inhibitory standard (unconjugated) peptides are less effective in primary neurons than in 293T monolayer cell cultures.
To determine the impact of host-relevant tissue on antiviral efficacy, we used fusion-inhibitory (HRC) peptides derived from the HRC region of HPIV3 (17, 22, 23) to inhibit G/F-mediated infection in neurons. To investigate why peptide efficacy depends not only on the peptide and the virus but also on the target cell, we employed our cholesterol-conjugated peptide V-PEG4-chol, which is inserted into the target membrane of cells. We recently showed that the addition of a cholesterol group to our antiviral HRC peptides targets these peptides to the membrane, where fusion occurs, dramatically increasing their antiviral effect not only in vitro but also in vivo (21, 23). In the experiment represented in Fig. 2A, primary neurons in 96-well plates were incubated with pseudotyped NiV in medium containing various concentrations of the HPIV3 HRC antiviral peptide with or without cholesterol, shown on the x axis. The plates were incubated at 37°C for 120 h and photographed, and the fluorescence in each well was measured. Specific peptide inhibition of the NiV pseudotyped viruses, but not of the VSV pseudotyped viruses, was observed (see Fig. S2 in the supplemental material). Figure 2B shows quantitative data for the standard (unconjugated) peptide versus the cholesterol-conjugated peptide in neurons infected with NiV, demonstrating an observed 50% inhibitory concentration (IC50) of ∼60 nM for the unconjugated peptide. In distinction from the unconjugated peptide, the cholesterol-conjugated peptide maintained very high efficacy in neurons, with an IC50 of <1 nM in neurons. The differences observed here may be key to understanding the accurate assessment of potential antivirals. These data provide a clear indication that host tissue type modulates antiviral effects for NiV infection also and support our previous observation of large differences in peptide efficacy against HPIV3 infection in human airway epithelial cells (representing the natural host target) and in a standard cell culture (CV-1) line (21). For accurate in vitro assessment of antiviral efficacy, the host cell must be considered and assessment carried out with natural tissue.
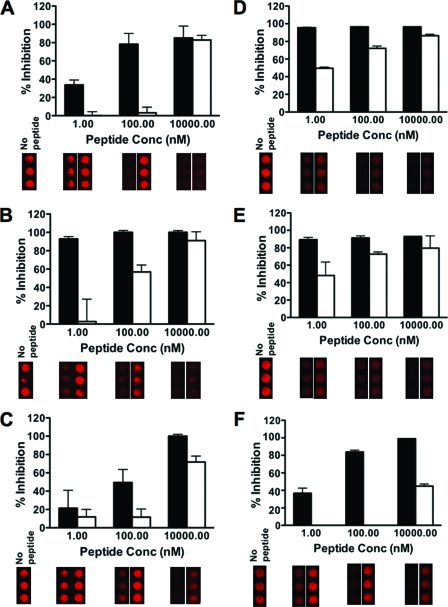
Fig. 2.
Cholesterol-conjugated peptide inhibits NiV infection in primary rat neurons. In panel A, neurons were seeded in a 96-well plate and infected with NiV virions in the presence of the indicated concentrations of HRC peptides at 24 h. At 120 h postinfection, fluorescent pictures of the 96-well plate were taken using a multimode image station Kodak 2000. Panel B shows quantitative data for inhibition of NiV infection by cholesterol-conjugated (black bar) and/or unconjugated (white bar) peptides. The data represent 3 replicates, with standard deviations.
Cholesterol tagging increases antiviral peptide efficacy because the cholesterol-conjugated peptides block viral spread more efficiently than do unconjugated peptides.
In the previous section, we measured the effectiveness of peptides at preventing viral entry. We next asked whether cholesterol-conjugated peptide is also more efficacious at blocking viral spread after initial infection. In the experiment represented in Fig. 3A, we assessed the inhibition of NiV G/F-mediated infection in neurons that were transfected with NiV G/F, using both an unconjugated and a cholesterol-conjugated peptide. The cholesterol-conjugated peptide is much more potent than the unconjugated peptide, supporting our previous observations (21, 23). The significance of the difference in inhibitory effect at 100 nM of the unconjugated peptide in neurons and cell line is a P value of 0.0002, while for the cholesterol-conjugated peptide it is a P value of 0.0107 (see Fig. S3 in the supplemental material). Thus, the difference between the inhibitory efficacy seen in neurons and that seen in monolayer cell line cultures is greater for the unconjugated peptide than for the cholesterol-conjugated peptide. In order to dissect whether the inhibition mediated by both types of peptide occurs during single-cycle or multicycle replication, we tested their efficacy on viral spread after the entry event. To test viral spread, we transfected cells with plasmids encoding the NiV glycoproteins G/F and then infected them with VSVΔG-RFP-VSV G (Fig. 3C). To test viral entry, we transfected cells with plasmid encoding the glycoprotein VSV G and then infected them with VSVΔG-RFP-NiV G/F (Fig. 3B). Our results indicate that both the cholesterol-conjugated and the unconjugated peptides were able to inhibit entry (Fig. 3B); however, only the cholesterol-conjugated peptide effectively inhibited the spread of the virus at low nanomolar concentrations (Fig. 3C). In Fig. 3C, the IC50s are 100 nM for the cholesterol-conjugated peptide and 10,000 nM for the unconjugated peptides. The ability to curtail multicycle replication even after the initial infection is likely to provide an important advantage for antiviral therapy.
Fig. 3.
Cholesterol-conjugated peptide inhibits NiV multicycle replication in primary rat neurons. Neurons were seeded in a 96-well plate and transfected with either NiV G/F (panels A and C) or VSV-G (panel B). At 24 h posttransfection, the cells were infected with NiV (panels A and B) or with VSV pseudotyped virions (panel C) in the presence of the indicated concentrations of peptides. At 120 h postinfection, fluorescent pictures of the 96-well plate were taken using a multimode image station Kodak 2000. 293T cells were seeded in a 96-well plate and transfected with either NiV G/F (panels D and F) or VSV-G (panel E). At 24 h posttransfection, the cells were infected with NiV (panels D and E) or with VSV pseudotyped virions (panel F) in the presence of the indicated concentrations of HRC cholesterol-conjugated peptide (black bar) or unconjugated peptide (white bar). The relative fluorescence intensity (RFI) of the red fluorescent protein (RFP) was quantitated with a Spectramax M5 multimode reader for both the neurons and the 293T cells. Based on the RFI reading, the percentage of inhibition was calculated for neurons (panels A, B, and C) and for the 293T cells (panels D, E, and F). The data represent 3 replicates, with standard deviations.
We then compared these results obtained using neurons with those obtained in a parallel experiment using the 293T cell line. The experiments represented in Fig. 3D, E, and F were performed as described above for neurons (Fig. 3A, B, and C). Similar to the neuron results, the data for 293T cells confirmed that the cholesterol-conjugated peptide is much more potent than the unconjugated peptide and more efficiently blocks viral spread after primary infection.
Our results for primary neurons show both quantitatively (more peptide is required for inhibition of fusion) and qualitatively (a larger difference between tagged and unconjugated peptides is observed) that standard laboratory cell lines do not accurately represent the behavior of peptides and viruses in natural host systems. This assertion is effectively supported by our recent demonstration of in vivo efficacy of cholesterol-conjugated peptides during NiV infection in the golden hamster model (21), while our previous studies using unconjugated peptides in ferrets were largely unsuccessful (M. Porotto and A. Moscona, unpublished data). Why then should the unconjugated peptide work so much less efficiently than the cholesterol-conjugated peptide? The recent demonstration that macropinocytosis may be a mechanism for NiV entry (16) could provide a timely insight. We have previously demonstrated that cholesterol tagging efficiently targets peptides to the cell membrane, even causing them to be inserted into the membranes themselves (23). If macropinocytosis contributes to virus entry, cholesterol-conjugated peptides could follow the virus inside during the entry process while unconjugated peptides may not, considerably enhancing the ability of the tagged peptides to prevent viral fusion.
In summary we report here that antiviral efficacy is intimately related to the target cell, thus providing a novel insight into a perceived discrepancy between in vitro and in vivo efficacies of otherwise promising antiviral candidates. Using an assay system that requires only the genes encoding the envelope glycoproteins derived from the target virus, coupled with a generic VSV pseudotyped virus, we assessed multicycle replication of a BSL4 virus under BSL2 conditions in primary neurons. This strategy allowed us to identify a key factor that may be predictive for in vivo antiviral success. Importantly, we have demonstrated that antiviral efficacies differ greatly between assays conducted with standard laboratory cell lines and those conducted with primary cells representing natural host tissues and that accurate antiviral assessment can be performed only with cells or tissues relevant to natural infection. The interplay between virus and host tissue is critical, not only for pathogenesis but also for antiviral effect.
Supplementary Material
Acknowledgments
We are grateful to Dan and Nancy Paduano for support of innovative research projects, to Ashton Kutcher and Jonathan Ledecky for their support, and to the Friedman Family Foundation for renovation of our laboratories at Weill Cornell Medical College. We acknowledge the Northeast Center of Excellence for Biodefense and Emerging Infections Disease Research's Proteomics Core for peptide synthesis and purification.
The work was supported by NIH (NIAD) Northeast Center of Excellence for Biodefense and Emerging Infectious Disease Research grant U54AI057158 (principal investigator of Center of Excellence grant, W. I. Lipkin), by NIH grant R01AI076335, and by NIH grant R21NS073781.
Footnotes
Supplemental material for this article may be found at http://jvi.asm.org/.
Published ahead of print on 8 June 2011.
REFERENCES
- 1. Arnaud L. T., Myeku N., Figueiredo-Pereira M. E. 2009. Proteasome-caspase-cathepsin sequence leading to tau pathology induced by prostaglandin J2 in neuronal cells. J. Neurochem. 110:328–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonaparte M. I., et al. 2005. Ephrin-B2 ligand is a functional receptor for Hendra virus and Nipah virus. Proc. Natl. Acad. Sci. U. S. A. 102:10652–10657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chua K. B., et al. 1999. Fatal encephalitis due to Nipah virus among pig-farmers in Malaysia. Lancet 354:1257–1259 [DOI] [PubMed] [Google Scholar]
- 4. Counts S. E., Mufson E. J. 2010. Noradrenaline activation of neurotrophic pathways protects against neuronal amyloid toxicity. J. Neurochem. 113:649–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Freiberg A. N., Worthy M. N., Lee B., Holbrook M. R. 2010. Combined chloroquine and ribavirin treatment does not prevent death in a hamster model of Nipah and Hendra virus infection. J. Gen. Virol. 91:765–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Georges-Courbot M. C., et al. 2006. Poly(I)-poly(C12U) but not ribavirin prevents death in a hamster model of Nipah virus infection. Antimicrob. Agents Chemother. 50:1768–1772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goh K. J., et al. 2000. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N. Engl. J. Med. 342:1229–1235 [DOI] [PubMed] [Google Scholar]
- 8. Gurley E. S., et al. 2007. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerg. Infect. Dis. 13:1031–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Homaira N., et al. 2010. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiol. Infect. 138:1630–1636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kandimalla K. K., Scott O. G., Fulzele S., Davidson M. W., Poduslo J. F. 2009. Mechanism of neuronal versus endothelial cell uptake of Alzheimer's disease amyloid beta protein. PLoS One 4:e4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lo M. K., Rota P. A. 2008. The emergence of Nipah virus, a highly pathogenic paramyxovirus. J. Clin. Virol. 43:396–400 [DOI] [PubMed] [Google Scholar]
- 12. Luby S. P., Gurley E. S., Hossain M. J. 2009. Transmission of human infection with Nipah virus. Clin. Infect. Dis. 49:1743–1748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Luo S., Mizuta H., Rubinsztein D. C. 2008. p21-activated kinase 1 promotes soluble mutant huntingtin self-interaction and enhances toxicity. Hum. Mol. Genet. 17:895–905 [DOI] [PubMed] [Google Scholar]
- 14. Negrete O. A., et al. 2005. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 436:401–405 [DOI] [PubMed] [Google Scholar]
- 15. Negrete O. A., et al. 2006. Two key residues in EphrinB3 are critical for its use as an alternative receptor for Nipah virus. PLoS Pathog. 2:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pernet O., Pohl C., Ainouze M., Kweder H., Buckland R. 2009. Nipah virus entry can occur by macropinocytosis. Virology 395:298–311 [DOI] [PubMed] [Google Scholar]
- 17. Porotto M., et al. 2007. Molecular determinants of antiviral potency of paramyxovirus entry inhibitors. J. Virol. 81:10567–10574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Porotto M., Fornabaio M., Kellogg G. E., Moscona A. 2007. A second receptor binding site on human parainfluenza virus type 3 hemagglutinin-neuraminidase contributes to activation of the fusion mechanism. J. Virol. 81:3216–3228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Porotto M., Murrell M., Greengard O., Moscona A. 2003. Triggering of human parainfluenza virus 3 fusion protein (F) by the hemagglutinin-neuraminidase (HN) protein: an HN mutation diminishes the rate of F activation and fusion. J. Virol. 77:3647–3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Porotto M., et al. 2009. Simulating henipavirus multicycle replication in a screening assay leads to identification of a promising candidate for therapy. J. Virol. 83:5148–5155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Porotto M., et al. 2010. Inhibition of Nipah virus infection in vivo: targeting an early stage of paramyxovirus fusion activation during viral entry. PLoS Pathog. 6(10):e1001168 doi: 10.1371/journal.ppat.1001168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Porotto M., et al. 2009. Kinetic dependence of paramyxovirus entry inhibition. J. Virol. 83:6947–6951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Porotto M., et al. 2010. Viral entry inhibitors targeted to the membrane site of action. J. Virol. 84:6760–6768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rockx B., et al. 2010. A novel model of lethal Hendra virus infection in African green monkeys and the effectiveness of ribavirin treatment. J. Virol. 84:9831–9839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang L., et al. 2001. Molecular biology of Hendra and Nipah viruses. Microbes Infect. 3:279–287 [DOI] [PubMed] [Google Scholar]
- 26. Wong K. T. 2000. Emerging and re-emerging epidemic encephalitis: a tale of two viruses. Neuropathol. Appl. Neurobiol. 26:313–318 [DOI] [PubMed] [Google Scholar]
- 27. Yonezawa A., Cavrois M., Greene W. C. 2005. Studies of Ebola virus glycoprotein-mediated entry and fusion by using pseudotyped human immunodeficiency virus type 1 virions: involvement of cytoskeletal proteins and enhancement by tumor necrosis factor alpha. J. Virol. 79:918–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhou X., Dong X. W., Priestley T. 2006. The neuroleptic drug, fluphenazine, blocks neuronal voltage-gated sodium channels. Brain Res. 1106:72–81 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.