Abstract
Caregivers for a family member with dementia experience chronic long-term stress that may benefit from new complementary therapies such as mindfulness-based stress reduction. Little is known however, about the challenges of recruiting and retaining family caregivers to research on mind-body based complementary therapies. Our pilot study is the first of its kind to successfully recruit caregivers for a family member with dementia to a randomized controlled pilot study of mindfulness-based stress reduction. The study used an array of recruitment strategies and techniques that were tailored to fit the unique features of our recruitment sources and employed retention strategies that placed high value on establishing early and ongoing communication with potential participants. Innovative recruitment methods including conducting outreach to health plan members and generating press coverage were combined with standard methods of community outreach and paid advertising. We were successful in exceeding our recruitment goal and retained 92% of the study participants at post-intervention (2 months) and 90% at 6 months. Recruitment and retention for family caregiver interventions employing mind-body based complementary therapies can be successful despite many challenges. Barriers include cultural perceptions about the use and benefit of complementary therapies, cultural differences with how the role of family caregiver is perceived, the use of group-based designs requiring significant time commitment by participants, and travel and respite care needs for busy family caregivers.
Keywords: Recruitment challenges, Participant Retention, Complementary therapies, Chronic stress, Family caregiver
Introduction
Recruiting and retaining family caregivers for a person with dementia to randomized intervention trials remains a significant challenge. [1–2] This may be especially true for interventions examining efficacy for mind-body based complementary therapies designed to address chronic stress, a significant and ongoing problem for caregivers. [3–4] Randomized controlled trials of mind-body based complementary therapies are relatively new with many participant groups and few studies to date describing the components of successful recruitment and retention strategies, or discussing barriers related to research participation. [6] With steady rates of increase in Alzheimer’s disease, providing care for a family member with dementia is becoming increasingly normative [7] and the need for effective interventions for caregiver stress more imperative. Little is known however, about successful strategies for recruiting and retaining family caregivers to research on mind-body complementary therapies.
Recruiting family caregivers to intervention research is a challenge. Caregivers experience significant demands on their time and attention from their caregiving duties and other commitments, often leaving them feeling overwhelmed and making them far less likely to participate in clinical trials. Farran [8] identified long-standing problems in recruiting family caregivers to research, noting early studies used convenience samples and more recent studies identified caregivers through health services users (dementia diagnostic centers, adult day care, and respite programs). This recruiting strategy has helped reach potential study participants, but may be subject to enrollment biases due to non-random (convenience) sampling. Attracting minority participants has also posed a significant challenge as evidenced by the significant lack of minority participation in caregiver research. [9–15] Few studies of complementary and alternative therapies focus on caregivers. We are aware of only three published reports using mind-body complementary therapies for family caregivers, a pilot study of yoga and meditation, [16] and two studies of relaxation therapy. [2,17] All three studies only briefly discuss information related to study recruitment. Waelde and colleagues [16] discuss recruiting 12 caregivers from the community, with 8 of the 12 having previously participated in a study of caregiving. Fisher and Laschinger [17] recruited participants from established caregivers groups in their area. The report by Murphy and colleagues [2] however, is a retrospective study of the factors related to family caregivers’ willingness to participate in a relaxation therapy intervention. The findings were that caregivers often feel overwhelmed and do not recognize or acknowledge their own need for help, or they feel selfish about seeking help for themselves and they need to be ready to seek help when considering participation. They also found that supportive research staff had a large impact on both recruitment and study retention.
With a scarcity of literature on successful methods for recruiting and retaining caregivers to clinical intervention trials focused on complementary and alternative therapies, there is clearly a pressing need for more information in this area. The purpose of this paper is to describe the successful recruitment and retention of caregivers for a family member with dementia to a randomized controlled pilot study of mindfulness-based stress reduction (MBSR), and to discuss the challenges and barriers in recruiting caregivers to intervention trials on mind-body based complementary therapies.
Methods
Background
The Balance Study was a randomized controlled pilot study which examined the feasibility and effectiveness of a MBSR intervention compared to a community caregiver education and support (CCES) program on measures of psychological and physiological distress and caregiver burden in caregivers for a family member with dementia. Each study intervention included eight weekly 2½ hour group sessions, and a 5 hour retreat or wellness day. MBSR participants received mindfulness meditation and yoga, and CCES participants received caregiver education and social support. Participants completed surveys and had blood drawn at points in time: baseline, post-intervention (2 months), and 6 months. They also completed a daily health behaviors calendar to track study adherence to activities, and a subset participated in tracking of their daily blood pressure with a wrist blood pressure cuff. Participants received $175 for completion of all study protocols and participants could apply for additional financial help up to $200 to obtain respite care or travel assistance.
The study was conducted in Bloomington, Minnesota, at HealthPartners Research Foundation (HPRF), a not-for profit research center affiliated with a mixed model health plan in the upper Midwest, during the years 2007 – 2010, with recruitment occurring from 2008–2009. It was reviewed and approved by the HealthPartners Institutional Review Board. HPRF collaborated with two community partners, the Center for Spirituality and Healing (CSH) at the Academic Health Center, University of Minnesota, and Senior Community Services (SCS), a long-standing provider of services to older adults in the Twin Cities Metropolitan area.
Participants
Participants were self-identified family caregivers for a person with dementia living in the community, who themselves contacted the study team after obtaining information about the study. A standardized phone screen was used to determine whether they were eligible for study participation. The inclusion/exclusion criteria were as follows: participants were required to be caring for a family member living in the community with significant cognitive difficulties consistent with the diagnosis of dementia. They needed to score 5 or above on a single-item measure of self-perceived stress (scale 1–10), have no diagnosis of mental illness or psychiatric hospitalizations in the prior 2 years, not be under treatment with anti-convulsion or anti-psychotic medications, not be under treatment for a serious mental health condition, or have had thoughts of harming themselves in the prior 6 months. Inclusion criteria also included being an English-speaking adult able to read the course materials, willing to travel to and attend the 8 week intervention groups, willing to be randomized to either the MBSR or CCES group, and willing to complete the data collection forms and have blood drawn at three points in time. Participants were excluded if they had completed a psycho-educational community caregiver support program, or practiced meditation, yoga, or tai chi within the prior year, since participants should have no prior exposure to the interventions under study prior to randomization.
Recruitment
Potential participants were recruited through a mixture of strategies targeted to an array of sources, some unique to the collaborating institutions. We categorized the sources of recruitment into six groups: (1) health plan outreach, (2) CSH outreach, (3) community outreach, (4) paid advertising, (5) generated press coverage, and (6) word of mouth. Health plan outreach was conducted through HPRF and the Alzheimer’s Research Center at Regions Hospital (ARCRH); this recruiting source allowed us to reach out to caregivers through clinics and health care providers where they, or the person they care for, receive their health care services.
Health plan outreach involved developing targeted communications to physicians, staff, and health plan members using a variety of strategies; these included developing study briefs for posting to internal HealthPartners (HP) electronic newsletters, as well as staff and health plan member websites. Outreach here included use of brochures and flyers in both administrative settings and staff model clinics, in particular inner city clinics with high proportions of minority health plan members. Study staff also presented information at clinic meetings and to HP departments such as Geriatrics and Home Care to increase awareness of the study. ARCRH, in cooperation with the HP Neurology Department, sent a study brochure to the homes of all health plan members who had a primary diagnosis of dementia in the prior year.
The second source of recruitment involved outreach by CSH. As a part of the Academic Health Center at the University of Minnesota, CSH provides education, conducts research, and offers an array of programs on complementary and alternative medicine to the university and broader community. It is well known for its programs and hosts a vibrant website with an array of resources and course listings. Recruitment strategies for CSH involved use of its website, newsletter and posting of brochures and flyers at the Center and throughout the University. The University’s main website also featured a brief report on the study on its all campus website. The Center also conducted outreach through the Minnesota Faith Health Consortium to historically African American churches through contacts with parish nurses, pastors and health ministry coordinators.
Community outreach involved the use of brochures and flyers posted at senior centers, community centers and community groups representing minority groups, such as Lao Family Community of Minnesota and Comunidades Latinas Unidas En Servicio (CLUES). Brochures and flyers were also posted in food coops and other public spaces. We actively worked to develop collaborations with a variety of local social service agencies providing services to seniors including Hennepin County Human Services, the Alzheimer’s Society, local home care agencies, local organizations providing respite care for older adults, and our primary community partner -Senior Community Services of Hennepin County. We hosted information tables at both small and large public gatherings, such as educational seminars for county social workers providing services to seniors, and at community events such as The Elder Care Expo. We placed notices in local community events calendars of small community newspapers. We considered this type of local listing “community outreach” rather than advertising, since it was usually limited to a few sentences of text and was more similar to the use of community postings with brochures and posters.
We also focused on two sources of recruitment involving the media: paid advertising and press coverage. Paid advertisements included the local newspapers; community specific publications, including those directed toward seniors and minorities; and radio advertisements. The radio advertisement we created ran on a local station during programming focused on women’s issues, and our advertisement also ran on a local public station that is directed at a large minority community in North Minneapolis, and is hosted by the Minneapolis Public School district. The study also worked to generate coverage by the press through writing articles on issues related to the caregiver experience such as stress and burden; and highlighting the study within each of the articles. Those articles were published in local community papers, newsletters, and a publication called MN Physician as well as a complementary publication for consumers called Health Care News. One of the main local newspapers also wrote a brief article about the study after seeing information posted on another site.
The last source of recruitment was by word of mouth. Here participants were most often referred to the study by family members, friends or other participants who hoped they might benefit from study participation. The study also received a number of calls from people seeking information on behalf of someone else they thought might be interested or might benefit from the intervention; these calls provided the study with minimal information about potential participants and are grouped together under a category titled “other”.
Minority Recruitment
Following review of the literature on minority recruitment of older adults, the study team held a series of meetings with the directors of community senior centers across the Twin Cities metro area and surrounding suburbs to discuss recommendations for study recruitment, with specific emphasis on minority recruitment. Minority recruitment of older adults is particularly challenging in Minnesota where the estimated percentage of minorities in the older adult population is 4.7%, much lower than other states. [18] The study team also met with Hennepin County Senior Services and their case workers, the visiting home nurse association, community social workers in Dakota County, CLUES – Comunidades Latinas Unidas En Servicio, the Geriatric Division of HealthPartners Medical Group, and local providers of community respite care in low income communities. We also compiled and used a number of resources to direct recruitment efforts to minority communities including the Ethnic Media Directory compiled by the Minnesota Department of Health, The Twin Cities Multicultural Organization contact list compiled by the Office of Institutional Diversity, and a media list on Minnesota Ethnic & Multicultural Media Outlets compiled by the Minnesota Department of Health. We also used a list serve directed to the Asian community that one study team member had personal experience with.
We developed the study recruitment plan with an emphasis on minority recruitment recognizing the hurdles the study would face in this area given the small older adult minority population in Minnesota. As a pilot study however, our recruitment efforts were also constrained by the scope of the study and financial considerations related to grant funding. Advertizing efforts used logos and designs rather than images of older adults where multiple versions of an ad or brochure would need to be created to represent white or minority participants. Hiring additional staff specifically for minority communities, or translating intervention materials and hiring experienced bilingual social workers or MBSR instructors was also out of the scope of this pilot study.
Retention
Retention activities began when participants expressed interest in the study, met the eligibility criteria. At that point information about the orientation meeting was sent to participants and ongoing telephone contact with the study coordinator began. Orientation meetings were held in a group format where the study staff was introduced to help build enthusiasm for the study. Information about randomization assignment was given to participants after this meeting.
When participants consented and enrolled to the study ongoing communication occurred from baseline, across the eight week intervention, and continuing six months following baseline. The study coordinator conducted telephone calls with participants to encourage attendance at groups, as well as participation and practice in the skills they were learning in the program. During the first four weeks of the intervention period the telephone calls were conducted every week, this moved to every other week for the last four weeks of the intervention period. The telephone calls focused on checking in with the participants to answer any questions, address concerns, and encourage participation and practice. Questions regarding specific skills or course materials were directed to the group facilitators. Telephone calls lasted from 5–10 minutes. Following the intervention phase the time period between telephone calls decreased from a biweekly to a monthly basis through the six months of study follow-up.
The study coordinator also maintained ongoing in-person weekly contact with study participants during the intervention. The coordinator provided refreshments and supplies for courses each week and checked-in each study participant to the weekly sessions, as well as the retreat day. If a participant missed a group, the coordinator would follow-up with a phone call to check in with the participant and encourage continued weekly participation and daily practice of course activities.
Results
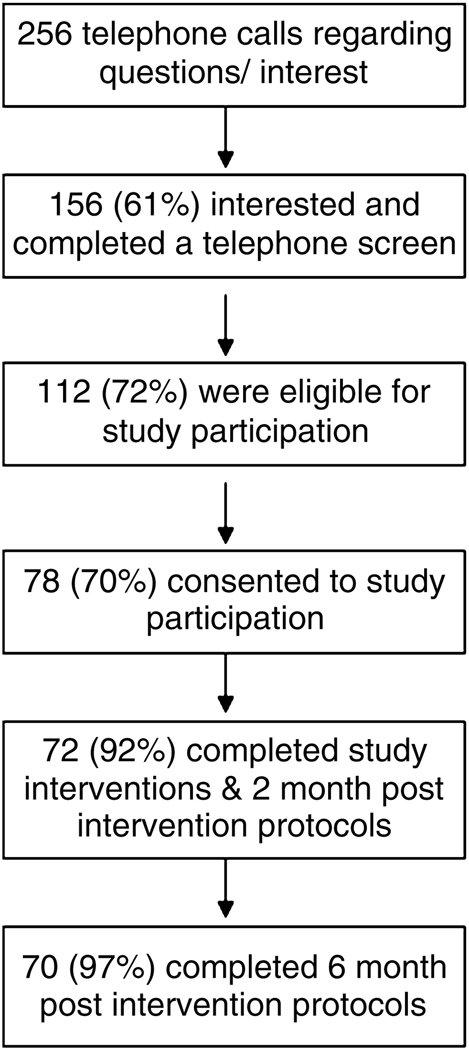
The study was successful in recruiting and retaining study participants in that we recruited 78 caregivers, which exceeded our sample size goal of 60. Furthermore, 72 (92%) completed the study intervention and post-treatment assessment. As can be seen in Figure 1 a total of 256 telephone calls were received about the study; these included potential participants, as well as friends or family seeking information on behalf of someone they knew. Of these, 61% expressed interest in the study and were screened for eligibility criteria. Once eligibility was determined and participants indicated interest in participating in the study they were assigned to a study orientation to complete informed consent, be randomized into a study group, and complete baseline surveys and blood draws. Of the 112 eligible participants, 78 attended a study orientation and consented to participation, 72 completed the interventions and 2 month post-intervention protocols, and 70 completed the 6 month follow-up protocols.
Figure 1.
Flow of Participant Recruitment and Retention
Enrollment and retention success rates for each of the sources of recruitment are presented in Table 1. As can be seen in Table 1, the health plan recruitment strategy had the highest percentage of initial contacts. The top four sources of recruitment however, were approximately equivalent regarding enrollment and accounted for 80% of study enrollees. Paid advertising had a slightly higher percentage of those who screened eligible and overall more closely mirrored health plan percentages than other sources of recruitment. Community outreach and generated press coverage also produced similar percentages of initial contacts, eligible screenings, and those who enrolled. CSH and word of mouth had lower recruitment yields for initial contact, but represented a higher proportion of participants who enrolled and completed the study. The category “unknown” represents a small number of contacts (n=3) for whom incomplete source information was obtained (e.g. where the potential participant could not recall where they had heard about the study).
Table 1.
Source of Recruitment by Enrollment Status
| Source of Recruitment, No. (%) |
Initial contact n=256 |
Screened n=156 |
Eligible n=112 |
Enrolled n=78 |
Post- intervention n=72 |
6 month follow-up n=70 |
|---|---|---|---|---|---|---|
| Health plan | 75 (29.3) | 40 (25.6) | 26 (23.2) | 18 (23.2) | 15 (20.8) | 14 (20.0) |
| Paid advertising | 59 (23.1) | 39 (25.0) | 26 (23.2) | 15 (19.2) | 14 (19.4) | 14 (20.0) |
| Community outreach | 37 (14.5) | 23 (14.7) | 20 (17.9) | 15 (19.2) | 15 (20.8) | 14 (20.0) |
| Press coverage | 32 (12.5) | 24 (15.4) | 20 (17.9) | 15 (19.2) | 14 (19.4) | 14 (20.0) |
| Center for Spirituality | 18 (7.0) | 14 (9.0) | 8 (7.1) | 6 (7.7) | 5 (6.9) | 5 (7.1) |
| Word of mouth | 23 (9.0) | 11 (7.1) | 10 (8.9) | 8 (10.3) | 8 (11.1) | 8 (11.4) |
| Unknown | 12 (4.7) | 5 (3.2) | 2 (1.8) | 1 (1.2) | 1 (1.4) | 1 (1.4) |
Table 2 displays the characteristics of the potential participants and enrollees at key stages of recruitment and retention. It is noteworthy that the composition of the study sample did not change markedly from the pool of individuals who expressed interest in the study through those who continued participation through the 6 month follow-up. Overall participants were predominantly white women in their mid-fifties, approximately three-quarters of whom were adult children of the family member they provided care for. Although the study generated inquiries from minority caregivers, only two minority participants, one American Indian and one Hispanic enrolled and completed the study intervention.
Table 2.
Participant Characteristics at Each Stage of Enrollment and Retention
| Characteristics | Initial Contact | Screened | Eligible | Enrolled | Post- intervention |
6 month follow-up |
|---|---|---|---|---|---|---|
| n | 256 | 156 | 112 | 78 | 72 | 70 |
| Age, M (SD) | 57.7 (11.2) | 56.0* (10.0) | 56.5 (10.1) | 56.8 (9.9) | 56.8 (10.0) | 57.0 (10.0) |
| Female (%) | 82.8 | 85.2 | 86.6 | 88.5 | 88.9 | 90.0+ |
| Race (%) | ||||||
| White | 86.7 | 93.6 | 97.3* | 98.7+ | 98.6 | 98.6 |
| Black/African American | 3.5 | 2.6 | 1.8 | |||
| Asian | 0.8 | 1.3 | ||||
| American Indian | 0.4 | 0.6 | 0.9 | 1.3 | 1.4 | 1.4 |
| Native Hawaiian | 0.4 | 0.6 | ||||
| Other | 1.2 | 0.6 | ||||
| Unknown | 7.0 | 0.6 | ||||
| Hispanic (%) | 2.3 | 1.3+ | 1.8 | 1.3 | 1.4 | 1.4 |
| Non-Hispanic White (%) | 85.2 | 92.3 | 95.5* | 97.4 | 97.2 | 97.1 |
| Relationship (%) | ||||||
| adult child | 63.3 | 73.7* | 75.0 | 74.4 | 73.6 | 72.9 |
| spouse, sibling, friend | 26.2 | 23.7 | 25.0 | 25.6 | 26.4 | 27.1 |
| unknown | 10.6 | 2.6 | ||||
| Months of caregiving, M (SD) | 49.7 (38.4) | 49.2 (38.6) | 48.8 (39.3) | 48.6 (39.5) | 47.2+ (39.2) | |
| Marital status (%) | ||||||
| married | 48.1 | 64.3 | 59.7 | 59.7 | 61.4 | |
| divorced | 10.3 | 12.5 | 12.5 | 12.5 | 11.4 | |
| widowed | 3.2 | 4.5 | 4.2 | 4.2 | 4.3 | |
| never married | 14.1 | 18.8 | 23.6 | 23.6 | 22.9 | |
| unknown | 24.4 | |||||
| Education (%) | ||||||
| high school | 5.8 | 7.1 | 6.4 | 6.9 | 7.1 | |
| some college | 27.6 | 37.5 | 37.2 | 38.9 | 37.1 | |
| college | 24.4 | 31.3 | 34.6 | 31.9 | 32.9 | |
| graduate school | 18.0 | 24.1 | 21.8 | 22.2 | 22.9 | |
| unknown | 24.4 |
p<.10,
p<.05 change in sample composition relative to each stage of enrollment and retention.
Although there was a high degree of variability related to length of providing care in the sample, the majority of study participants were married with high levels of education, and had been providing care to their family member for an average of four years,. This was particularly true for spousal caregivers who represented approximately 25% of the sample and often indicated difficulty in specifying the exact number of years they had been providing care for their spouse. The characteristics of the sample from first contact through eligibility and enrollment show the study sample becoming increasingly female and white, with higher levels of education, and approximately 75% adult children at the time of enrollment.
For those enrolled in the study (n=78), 92% completed the post-intervention protocol and 90% completed the six month follow-up. Session attendance represents another aspect of study retention: the group session attendance rate was 88.1% with 91% of study participants attending at least 6 of the 8 sessions. Attendance at the half- day retreat was 90%; this resulted in a combined group attendance rate of 88%.
Discussion
The use of a variety of recruitment sources and strategies tailored to the unique features of each recruitment source benefitted the clinical trial and enabled us to exceed our recruitment goal. The strategies employed to encourage study retention were successful, with 92% of those enrolling completing the post-intervention study protocols, and 90% the 6 month follow-up. The recruitment design was particularly successful in light of several challenges: first, this was a novel intervention that employed a complementary therapy based in meditation and yoga and used a group-based design which required a significant time commitment. Second, the intervention required travel to a single intervention site and subsequent respite care needs that were difficult, especially for spousal caregivers. And, finally, interaction with potential participants uncovered a lack of identification among families providing elder care with the term ‘caregiver’ and the cultural differences with how this role is perceived.
Research in complementary therapies addresses a wide range of therapeutic modalities, and while some have proposed that participants are willing to engage in this research, [19] others have found that clinical trials for interventions on complementary therapies require greater effort to recruit subjects. [20] The latter was clearly the case for our clinical trial using mindfulness-based stress reduction, which is a type of mind-body complementary therapy. While the use of complementary and alternative medicine in the United States has increased to 38% of adults in recent reports, mind-body therapies account for only a small portion of this, remaining relatively unknown and thus far from the mainstream of acceptability. [21] Perceptions of complementary therapies also vary greatly among racial and ethnic groups. In a recent report Barnes and colleagues found that the lowest use of complementary medicine was among Black and Asian adults. [22] This is reflective of our experience, where despite significant effort we were only able to generate minimal interest from potential minority participants. There are also age differences regarding acceptability of complementary therapies, especially yoga and meditation, with many middle aged and older adults coming of age in a time when such activities were viewed with great skepticism.
One experience from our clinical trial is illustrative of the range of perceptions that adults hold regarding the use of complementary and alternative therapies such as meditation and yoga. Among the telephone calls we received from potential participants regarding interest in the study, were calls from potential participants who were interested in seeking entry only into the active control intervention, the CCES group. The CCES intervention focused on caregiver education and social support and is a well-researched intervention model with successful outcomes. [23–24] However, this type of intervention is also expensive to run and many community groups in our area have abandoned it in favor of support groups, often run by the participants. Of the telephone calls received regarding interest in the CCES group, there were potential participants who were willing to be randomized to the MBSR group, met the criteria, and eventually entered the study. There were also cases where they were not willing to be randomized to a group doing meditation and yoga. So referrals were made to SCS, our community partner for other types of caregiver services. It is highly unusual for a clinical trial to have potential participants seeking entry only into the control intervention arm of the study and is reflective of the challenges of recruiting for clinical trials using mind-body therapies.
Mind-body complementary therapies are also often conducted in a group-based format, presenting additional challenges. For a group-based intervention to be successful, a minimum number of participants must be obtained for each trial arm before an intervention series can start. If recruitment is difficult and uneven, the study runs the risk of losing potential participants as interest wanes, or a caregiver’s situation changes. For example, one of the six participants who withdrew did so when their family member entered a nursing home and three participants’ situations changed making them unable to participate due to events that required more of their time. These types of interventions can also have significant time requirements in terms of weekly groups and retreat attendance and daily practice. [25] As Gallagher-Thompson and colleagues note, time constraints can significantly limit research participation by caregivers in intervention studies. [11] Careful planning and flexibility are necessary and thoughtful discussion with and presentation of information on the affects of stress on physical, mental and emotional health can help caregivers more carefully consider the benefits of study participation.
Time requirements for group-based designs also are incurred through weekly travel to the study site and respite care needs can be a problem especially for spousal caregivers. These have long been a barrier to participation by caregivers in intervention research and disproportionately affect low-income and minority caregivers. [8] Ideally studies would hold intervention groups in areas where they wish to attract participation, limiting participant travel time and costs. Unfortunately, this also raises study costs, and for small studies may not be an option. Respite care involves not only financial costs but also legal and medical issues, since most respite care providers require nurse assessments at enrollment, which can make providing respite care prohibitive for an intervention study. Providing incentives however, can give some assistance with travel and respite care needs. We offered a monetary incentive of up to $175 based on completion of study protocols to all participants to help with respite care and/or travel costs. We recognize this was inadequate in defraying costs for low income participants so we also provided additional assistance of up to $200 through a separate incentive fund designed to encourage participation. The study was limited in the amount of incentives we could offer participants and we recognize this was likely a limitation to participation for low income individuals. We had five participants inquire about the additional assistance, with three requesting and receiving the additional assistance funds.
Finally, and perhaps most importantly, in recruiting and retaining caregivers to intervention research is the language used to identify them and the cultural differences in how this role is perceived. [11] Our community partner SCS, with years of experience serving the needs of caregivers, found that caregivers do not identify with the term “caregiver”; they see themselves through their roles in the family; as daughters, sons, or spouses who are helping their parent, or spouse. The term “caregiver” often holds no meaning for them, or has negative connotations associated with dependency and burden. Language they could identify with, terms that were respectful and acknowledged their long-standing roles within their family structures, was critical. In recruiting caregivers, the terminology used to identify them was as, or more, important than the careful descriptions of the intervention itself. In developing the name of the study we used the phrase “The Balance Study: Balancing Life and Reducing Stress for those Providing Elder Care”, purposefully excluding the term caregiver in the title and all study descriptions. We did however, use the term caregiver in the control group description since we imported this active control intervention from our community partner who had a long history delivering it in the community. The study however, may have benefitted by amending the title to be more consistent with other study material.
The meaning and role of being a caregiver in families also varies greatly by culture and ethnicity. In many cultures the prominence of filial duty and a strong sense of obligation toward aging parents make elder care an expected component of family life. This, combined with strong prohibitions in many cultures regarding discussion of mental or emotional distress or help-seeking outside of the family or community, can make participation in caregiver intervention research seem unacceptable. [11] Careful consideration of cultural differences, collaborations with agencies and community groups serving minorities, as well as careful consideration of language and terminology can help move intervention research toward its goals of inclusiveness and representativeness of all caregivers in the community. [26]
Conclusions
The use of complementary therapies such as mindfulness-based stress reduction to help caregivers manage the long-term chronic stress associated with caregiving holds potential promise for providing an ongoing stress reduction technique that, once learned, can be employed by anyone in a safe, effective, and cost-effective manner. Intervention research is needed to fully test the efficacy of this intervention with caregivers. We have shown that recruiting and retaining caregivers to a randomized controlled intervention study on mind-body complementary therapies can be completed successfully despite the many barriers. Through the use of a wide variety of recruitment sources and techniques, careful attention to language and terminology, and placing a high value on establishing early and ongoing contact with participants, we were successful in exceeding our recruitment goal and retaining participants in the study. In future studies we would employ our lessons learned to focus on our most successful recruitment methods and explore new and hopefully more innovative recruitment techniques as well.
We hope the experience described here will provide insight to others developing the use of innovative and alternative approaches to helping caregivers manage the chronic stress associated with caregiving. More systematic accounts of successful recruitment and retention in clinical trials involving caregivers can help move the field of intervention research, including research on complementary therapies, forward to more successful ends in the coming years.
Acknowledgements
The authors thank the staff who served as recruiters for the study.
Role of the Funding Source
This work was funded by a grant from the National Center for Complementary Medicine, National Institutes of Health [R21 AT003654-01A1]. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM, or the National Institutes of Health.
References
- 1.Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004 May–Jun;12(3):240–249. [PubMed] [Google Scholar]
- 2.Murphy MR, Escamilla MI, Blackwell PH, et al. Assessment of caregivers' willingness to participate in an intervention research study. Res Nurs Health. 2007 Jun;30(3):347–355. doi: 10.1002/nur.20186. [DOI] [PubMed] [Google Scholar]
- 3.Aguglia E, Onor ML, Trevisiol M, Negro C, Saina M, Maso E. Stress in the caregivers of Alzheimer's patients: an experimental investigation in Italy. Am J Alzheimers Dis Other Demen. 2004 Jul–Aug;19(4):248–252. doi: 10.1177/153331750401900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Judge KS, Menne HL, Whitlatch CJ. Stress process model for individuals with dementia. Gerontologist. 2010 Jun;50(3):294–302. doi: 10.1093/geront/gnp162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008 Sep 17;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- 6.Smith CA, Coyle ME. Recruitment and implementation strategies in randomised controlled trials of acupuncture and herbal medicine in women's health. Complement Ther Med. 2006 Mar;14(1):81–86. doi: 10.1016/j.ctim.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Ballard EL. Social work perspectives: issues in caregiver research: the family. Alzheimer Dis Assoc Disord. 1999 Apr–Jun;13 Suppl 1:S88–S92. [PubMed] [Google Scholar]
- 8.Farran CJ. Family caregiver intervention research: where have we been? Where are we going? J Gerontol Nurs. 2001 Jul;27(7):38–45. doi: 10.3928/0098-9134-20010701-11. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher-Thompson D, Rabinowitz Y, Tang PC, et al. Recruiting Chinese Americans for dementia caregiver intervention research: suggestions for success. Am J Geriatr Psychiatry. 2006 Aug;14(8):676–683. doi: 10.1097/01.JGP.0000221234.65585.f9. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher-Thompson D, Singer LS, Depp C, Mausbach BT, Cardenas V, Coon DW. Effective recruitment strategies for Latino and Caucasian dementia family caregivers in intervention research. Am J Geriatr Psychiatry. 2004 Sep–Oct;12(5):484–490. doi: 10.1176/appi.ajgp.12.5.484. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher-Thompson D, Solano N, Coon D, Arean P. Recruitment and retention of latino dementia family caregivers in intervention research: issues to face, lessons to learn. Gerontologist. 2003 Feb;43(1):45–51. doi: 10.1093/geront/43.1.45. [DOI] [PubMed] [Google Scholar]
- 12.Eaves YD. Family recruitment issues and strategies: caregiving in rural African Americans. Nurs Res. 1999 May–Jun;48(3):183–187. doi: 10.1097/00006199-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Amador TK, Travis SS, McAuley WJ, Bernard M, McCutcheon M. Recruitment and retention of ethnically diverse long-term family caregivers for research. J Gerontol Soc Work. 2006;47(3–4):139–152. doi: 10.1300/J083v47n03_09. [DOI] [PubMed] [Google Scholar]
- 14.Fulton P, Tierney J, Mirpourian N, Ericsson JM, Wright JT, Jr, Powel LL. Engaging black older adults and caregivers in urban communities in health research. J Gerontol Nurs. 2002 Feb;28(2):19–27. doi: 10.3928/0098-9134-20020201-07. [DOI] [PubMed] [Google Scholar]
- 15.Chadiha LA, Morrow-Howell N, Proctor EK, et al. Involving rural, older African Americans and their female informal caregivers in research. J Aging Health. 2004 Nov;16(5 Suppl):18S–38S. doi: 10.1177/0898264304268147. [DOI] [PubMed] [Google Scholar]
- 16.Waelde LC, Thompson L, Gallagher-Thompson D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J Clin Psychol. 2004 Jun;60(6):677–687. doi: 10.1002/jclp.10259. [DOI] [PubMed] [Google Scholar]
- 17.Fisher PA, Laschinger HS. A relaxation training program to increase self-efficacy for anxiety control in Alzheimer family caregivers. Holst Nurs Pract. 2001 Jan;15(2):47–58. doi: 10.1097/00004650-200101000-00008. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Census Bureau. Allegany, NY: 2009. [Accessed April 14, 2011]. American FactFinder Fact Sheet: Minnesota. S0102: Population 60 Years and Over in the United States; 2005–2009 American Community Survey 5-Year Estimates. http://factfinder.census.gov/servlet/STTable?_bm=y&-context=st&-qr_name=ACS_2009_5YR_G00_S0102&-ds_name=ACS_2009_5YR_G00_&-tree_id=5309&-redoLog=false&-_caller=geoselect&-geo_id=04000US27&-format=&-_lang=en. [Google Scholar]
- 19.Schneider J, Vuckovic N, DeBar L. Willingness to participate in complementary and alternative medicine clinical trials among patients with craniofacial disorders. J Altern Complement Med. 2003 Jun;9(3):389–401. doi: 10.1089/107555303765551615. [DOI] [PubMed] [Google Scholar]
- 20.Cambron JA. Recruitment and accrual of women in a randomized controlled trial of spinal manipulation. J Manipulative Physiol Ther. 2001 Feb;24(2):79–83. doi: 10.1067/mmt.2001.112567. [DOI] [PubMed] [Google Scholar]
- 21.O'Mathuna DP. Research on Complementary and Alternative Medicine. Research Practitioner. 2007;8(2):61–69. [Google Scholar]
- 22.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008 Dec 10;(12):1–23. [PubMed]
- 23.Acton GJ, Kang J. Interventions to Reduce the Burden of Caregiving for an adult with dementia: A meta-analysis. Res Nurs Health. 2001;24:349–360. doi: 10.1002/nur.1036. [DOI] [PubMed] [Google Scholar]
- 24.Zarit S, Femia E. Behavioral and psychosocial interventions for family caregivers:Characteristics of effective approaches and flaws in study design. AJN. 2008 Sep;108(9 Suppl):47S–53S. doi: 10.1097/01.NAJ.0000336415.60495.34. [DOI] [PubMed] [Google Scholar]
- 25.Kabat-Zinn J. Full Catastrophe Living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- 26.Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. Gerontologist. 2003 Feb;43(1):18–26. doi: 10.1093/geront/43.1.18. [DOI] [PubMed] [Google Scholar]