Abstract
Background
Longer tenure in methadone treatment has been associated with positive outcomes such as reductions in drug use and crime, HIV seroconversion, and overdose death.
Methods
Retention in treatment was examined for 351 opioid-dependent individuals who had been newly admitted to one of six methadone programs in Baltimore, Maryland. Cox proportional hazards regression was used to predict number of days retained in treatment to 90 days from baseline ASI Composite scores and Treatment Motivation scales. A second analysis predicted days in treatment to 365 days using the same baseline variables plus 3-month Motivation scales, Patient Satisfaction scales, and methadone dose in the 248 individuals who had remained in treatment at least 3 months. Analyses held constant gender, race, age, whether participants had a history of regularly smoking cocaine, whether participants were on parole/probation, and program site.
Results
Retention at 90 days was predicted by female gender, and greater baseline Treatment Readiness (p=.005) but lower Desire for Help (p=.010). Retention at 365 days was predicted by higher baseline ASI Medical Composite scores (p=.037) and lower Legal Composite scores (p=.039), higher 3-month Treatment Satisfaction scores (p=.008), and higher dose (p=.046).
Conclusions
Greater satisfaction with treatment at 3 months was a significant predictor of retention at 12 months, indicating the importance of understanding the role satisfaction plays in determining retention. Greater severity of legal problems was associated with shorter retention, suggesting that program efforts to increase services to criminal justice patients (e.g., legal counseling) may constitute a useful addition to treatment.
Keywords: Opioid addiction, Methadone maintenance, Treatment retention
1. Introduction
The benefits of remaining in methadone treatment for at least 12 months have been well established over the past three decades (Simpson, 1981; Simpson et al., 1997a, 1997b; Hubbard et al., 1989, 1997; Simpson and Joe, 2004). Longer tenure in methadone treatment has been associated with positive patient outcomes, including decreases in drug use (Zhang et al., 2003; Hubbard et al., 1997; Hubbard et al., 2003), criminal activity (Hubbard et al., 2003; Maddux and Desmond, 1997), HIV seroconversion (Metzger et al., 1993; Nathan and Karan, 1989), and overdose death (Gibson et al., 2008; Zanis and Woody, 1998). Unfortunately, premature discontinuation of methadone treatment has remained a serious problem over the decades, as nearly 50% of patients who begin treatment are no longer enrolled in treatment by the end of the first year (Ball and Ross, 1991; Hubbard et al., 1989, 1997; Joe et al., 1999).
Three types of factors can be considered in examining retention in treatment: patient factors, program factors, and community factors. Prior research has established a number of patient-related factors that are associated with longer tenure in treatment, including older age (Saxon et al., 1996; Magura et al., 1998; Deck and Carlson, 2005; Grella et al., 1997; Mertens and Weisner, 2000), female gender (Deck and Carlson, 2005), non-African-American race (Joe et al., 1991, 1998; Saxon et al., 1996), less cocaine use (Grella et al., 1997; Joe et al., 1999; Deck and Carlson, 2005; Saxon et al., 1996); and less alcohol use (Grella et al., 1997; Joe et al., 1999). In addition, higher levels of motivation for treatment (both pre-treatment and during treatment) have been found to be associated with treatment retention (Simpson et al., 1997a, 1997b; Simpson and Joe, 1993; Joe et al., 1998).
Program-related variables have additionally been found to be related to retention in methadone treatment. For example, higher methadone dose has been found to be associated with greater tenure in treatment (Villafranca et al., 2006; Saxon et al., 1996; Magura et al., 1998; Strain et al., 1999; Peles et al., 2008). Greater counselor-patient rapport (Joe et al., 1999; Luborsky et al., 1985; Simpson et al., 1997b) and higher levels of patient satisfaction with the treatment program and counselor (Villafranca et al., 2006; Joe and Friend, 1989) may also be associated with retention in methadone maintenance treatment.
Community-level factors have been less frequently studied than patient- and program- level factors, but have been of increasing interest (Brown et al., 2004) and also appear to play a role in patient retention. There is some indication that involvement in the criminal justice system, such as being on parole or probation or having cases pending at intake (Joe et al., 1998), is associated with less time in treatment (Desmond and Maddux, 1996; Magura et al., 1998; Joe et al., 1998, 1999).
Although prior studies have examined the relationship between personal, treatment, and community factors and retention in methadone treatment, few studies have undertaken a broader evaluation that incorporates factors from all three domains. Thus, the present study seeks to contribute to an understanding of factors related to retention in methadone maintenance treatment by including personal, treatment, and community variables in predicting retention in a sample of methadone patients entering six methadone treatment programs (MTPs) in Baltimore, Maryland, USA. This study includes an analysis of the entire sample (N = 351) of newly-enrolling methadone patients to examine factors associated with treatment termination prior to 90 days because this point has been identified in prior research as the minimum length of time in treatment in order to engage patients for behavior change (Simpson, 1979, 1981). An additional analysis predicting discharge prior to 365 days examined the subsample of those participants (n = 248) who remained in treatment for at least 90 days.
2. Methods
2.1. Participants
The total sample consisted of 351 opioid-dependent individuals entering one of six Baltimore area methadone treatment programs between November 2004 and November 2007, inclusive, who were participants in a larger National Institute on Drug Abuse-funded study of entry and engagement in methadone maintenance treatment. The larger study additionally included a cohort of opioid-dependent individuals not seeking treatment (Schwartz et al., 2008; Kelly et al., 2009) and a qualitative component which examined barriers to treatment entry and retention (Mitchell et al., 2009a; 2009b; Peterson et al., 2010; Reisinger et al., 2009). Eligibility for study participation required participants to be at least 18 years of age and meet the US federal criteria for methadone maintenance treatment at the time of recruitment, which include at least one year of opioid dependence. The study was approved by Friends Research Institute’s Institutional Review Board and all study participants provided written informed consent.
The subsample included only participants who had been enrolled in treatment for at least 90 days and had completed a 3-month follow-up interview, given that 3-month variables were included as predictors in the analysis examining the number of days retained in treatment to 365 days. Of the total sample of 351 participants, 63 participants were no longer in treatment 90 days after admission and, therefore, were necessarily excluded from this latter analysis. Of the remaining 288 participants, 36 were excluded because they did not complete their 3-month follow up interview, and 4 others were excluded due to missing 3-month data. Thus, the final subsample for this analysis consisted of the remaining 248 participants who had complete baseline and 3-month follow-up data and at least 90 days of treatment.
2.2. Measures
Addiction Severity Index (ASI; McLellan et al., 1980, 1985, 1992)
The ASI measures the severity of potential treatment problems in seven areas: alcohol use; drug use; medical; psychiatric; family/social; employment; and legal. Selected ASI items that focus on the past 30-day period are combined within each domain to create seven composite scores ranging from 0 (no problem) to 1 (extreme problem). Study participants were administered the ASI at baseline (treatment entry) to obtain composite scores and the following demographic and background variables used as predictors in the present study: gender, race, age, whether participants were on parole or probation at time of admission, and whether participants reported a history of smoking crack/cocaine.
Treatment Motivation Scale (Joe et al., 2002; Simpson, 2004; Simpson and Joe, 1993; Knight et al., 1994)
This 35-item 5-point Likert measure is taken from the Texas Christian University Client Evaluation of Self and Treatment (CEST) developed by Simpson and colleagues. Three Motivational scales were included in the analysis for the present study: 1) Problem Recognition (PR), a 9-item scale that measures patients’ recognition of problems related to drug use and their perceptions of the severity of these problems; 2) Desire for Help (DH), a 7-item scale that measures patients’ awareness of their need to obtain help for drug problems; and 3) Treatment Readiness (TR), an 8-item scale that measures patients’ degree of commitment to change drug-using behaviors through participation in treatment. Prior studies involving methadone patients have reported these Motivational scales to have coefficient α reliabilities ranging from .71 to .85 (Joe et al., 1998; Simpson et al., 2000). The Motivation scales were administered at baseline and at 3-month follow-up.
Client Evaluation Form (CEF; Simpson, 2004; Joe et al., 2002)
The CEF, also taken from the CEST, is a self-report instrument that assesses treatment engagement and satisfaction (Joe et al., 2002). Participants completed a form consisting of 23 self-rated items answered on a 5-point Likert scale with 5 indicating the most positive rating. Responses were summed to provide scores for two scales of a Patient Satisfaction measure included as predictors in this study: 1) Treatment Satisfaction, a 7-item subscale that measures patients’ overall satisfaction with the treatment program as well as their satisfaction with specific aspects of the program such as location, convenience, staff, and program organization; and 2) Counselor Services, an 11-item subscale that measures patients’ evaluation of their counselors in such areas as dependability, motivation, respect, and encouragement. Prior research involving methadone maintenance patients has shown these scales to be related to retention in treatment (Kelly et al., 2010; Joe and Friend, 1989; Simpson et al., 2000). Coefficient α reliabilities for Treatment Satisfaction and Counselor Services in previous studies of methadone patients have been reported to be .85 and .95, respectively (Joe et al., 2002; Simpson et al., 2000). The CEF was administered to all participants at the 3-month follow-up.
Methadone dosage at 3 months
Participants’ methadone dose on the day their 3-month assessment was due was obtained from treatment program records.
Number of days retained in treatment
Number of days enrolled in the index treatment program through 12 months (maximum number of days = 365) was obtained from the treatment program.
2.3. Statistical analysis
Cox proportional hazards regression was utilized to predict number of days retained in treatment for both the sample of 351 participants and the subsample of 248 participants. Predictor variables for the number of days retained in treatment up to 90 days for the total sample of 351 participants were the seven baseline ASI Composite scores and the baseline Treatment Motivation scales (Problem Recognition, Desire for Help, Treatment Readiness). In order to better isolate the effects of the predictors of interest, the following covariates were included in the model to control for their possible relationship to the number of days in treatment: gender, race, age, history of regularly smoking crack/cocaine (yes/no), and whether participants were on parole or probation (yes/no). Finally, a variable representing program site was included in the statistical model to control for the possible differential effectiveness of the six treatment programs.
Predictor variables for the analysis of number of days retained in treatment to 365 days for the subsample of 248 participants who had at least 90 days of treatment were the seven baseline ASI Composite scores, baseline and 3-month Treatment Motivation scales, 3-month CEF Patient Satisfaction scales (Treatment Satisfaction and Counselor Services), and 3-month methadone dose. The same covariates as in the 90-day retention analysis were likewise employed in this analysis.
3. Results
3.1. Participant characteristics
The sample of 351 participants was 53.3% male, 74.1% African American, and had a mean age of 41.2 years (see Table 1). A third of the sample had a history of smoking cocaine, and just over a quarter were on probation or parole. Eighty-two percent of the sample remained in treatment for at least 90 days, 58.4% remained in treatment for 365 days, and the mean number of days in treatment was 272 (SD = 129; Range = 2 to 365 days). Average methadone dose at 3 months was 86.3 mg (SD = 21.5).
Table 1.
Descriptive statistics
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Total sample (N = 351)
| ||
|
Demographics
| ||
| Gender | ||
| Male | 187 (53.3%) | |
| Female | 164 (46.7%) | |
| Race | ||
| White | 87 (24.8%) | |
| African American | 260 (74.1%) | |
| Native American | 1 (0.3%) | |
| Asian or Pacific Islander | 1 (0.3%) | |
| Other Hispanic | 2 (0.6%) | |
| Age | 41.2 (8.2) | |
|
| ||
|
Baseline variables
| ||
| Smoked crack/cocaine (Lifetime) | 117 (33.3%) | |
| On parole or probation | 93 (26.5%) | |
| Medical composite | .15 (.29) | |
| Employment composite | .82 (.25) | |
| Alcohol composite | .09 (.14) | |
| Drug composite | .32 (.10) | |
| Legal composite | .19 (.22) | |
| Family/Social composite | .07 (.14) | |
| Psychiatric composite | .08 (.17) | |
| Problem Recognition (PR) | 36.1 (5.8) | |
| Desire for Help (DH) | 30.7 (3.4) | |
| Treatment Readiness (TR) | 33.5 (4.2) | |
|
| ||
| Subsample in treatment for at least 90 Days (n = 248)
| ||
|
3-month variables
| ||
| Dose at 3 month due date | 86.3 (21.5) | |
| Treatment Satisfaction | 27.2 (3.9) | |
| Counselor Services | 44.4 (7.2) | |
| Problem Recognition (PR) | 30.8 (7.1) | |
| Desire for Help (DH) | 27.9 (3.9) | |
| Treatment Readiness (TR) | 32.6 (4.3) | |
3.2. Scale psychometric properties
Internal consistency α scores for baseline Problem Recognition, Desire for Help, and Treatment Readiness were .74, .62, and .63, respectively (N = 351). At 3 months, α scores for Problem Recognition, Desire for Help, and Treatment Readiness were .81, .65, and .69, respectively, while for 3-month Patient Satisfaction, internal consistency α was .71 for the Treatment Satisfaction scale and .93 for the Counselor Services scale (n = 248).
3.3. Cox proportional hazards regression analysis
Table 2 shows the results from the Cox proportional hazards regression predicting number of days retained in treatment up to 90 days. Of the demographic covariates, males were significantly more likely to be discharged from treatment prior to 90 days (OR = .42, 95% CI = .22–.78, p = .006). Two of the three baseline Treatment Motivation scales (DH and TR) predicted number of days retained in treatment to 90 days. Participants who showed greater Desire for Help at baseline were less likely to still be in treatment at 90 days (OR = 1.16, 95% CI = 1.04–1.30, p = .010). Conversely, participants who showed greater Treatment Readiness at baseline were more likely to still be in treatment at 90 days (OR = .91, 95% CI = .84–.97, p = .005).
Table 2.
Parameter estimates, confidence intervals, and test statistics from Cox proportional hazards regression analysis predicting number of days retained in treatment to 90 days (N = 349)
| Variable | Odds Ratio | 95% CI (Lower, Upper) | Wald χ2 (df=1) | p |
|---|---|---|---|---|
|
Demographics
| ||||
| Gender | .42 | .22 .78 | 7.56 | .006 |
| Race | .85 | .43 1.68 | .22 | .637 |
| Age | 1.02 | .98 1.06 | 1.07 | .302 |
|
| ||||
|
Baseline variables
| ||||
| Smoked crack/cocaine (Lifetime) | .96 | .54 1.71 | .02 | .897 |
| On parole or probation | .84 | .45 1.58 | .28 | .595 |
| Medical composite | 1.00 | .37 2.67 | .00 | .993 |
| Employment composite | 2.67 | .79 9.06 | 2.49 | .115 |
| Alcohol composite | 1.88 | .27 12.96 | .41 | .520 |
| Drug composite | .94 | .05 18.03 | .00 | .967 |
| Legal composite | 1.80 | .55 5.90 | .95 | .329 |
| Family/Social composite | 1.46 | .18 12.09 | .12 | .727 |
| Psychiatric composite | 1.82 | .34 9.75 | .49 | .482 |
| Problem Recognition (PR) | .98 | .92 1.04 | .63 | .428 |
| Desire for Help (DH) | 1.16 | 1.04 1.30 | 6.59 | .010 |
| Treatment Readiness (TR) | .91 | .84 .97 | 7.78 | .005 |
| Program site | 4.22 | .519 | ||
Note: Test statistic for Race was obtained by collapsing data into two categories: White (n = 87) v. Black/Other (n = 264). N = 349 due to missing data for 2 participants.
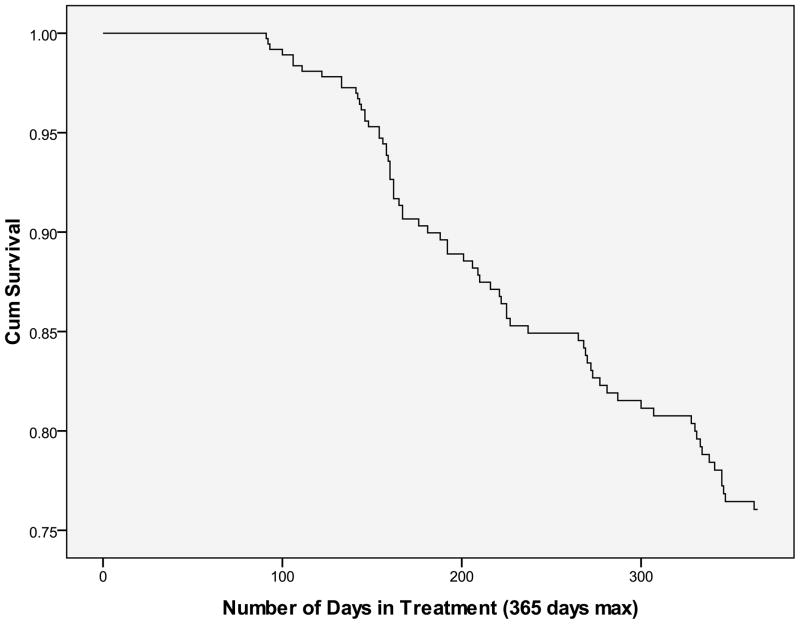
Table 3 shows the results from the Cox proportional hazards regression predicting number of days retained in treatment up to 365 days. None of the demographic covariates significantly predicted days retained in treatment. Of the baseline predictor variables, the ASI Legal and Medical Composites were significant predictors of retention in treatment up to 365 days. Individuals who reported greater legal problem severity were significantly more likely to be discharged from treatment before 365 days (OR = 3.60, 95% CI = 1.03–12.63, p = .045), while individuals who reported greater medical severity were less likely to be discharged prior to 365 days (OR = .31, 95% CI = .10–.93, p = .037). Regarding 3-month predictor variables, Treatment Satisfaction and methadone dose significantly predicted number of days in treatment up to 365 days, indicating that the more satisfied participants were with treatment (OR = .91, 95% CI = .84–.99, p = .024) and the higher the dose (OR = .99, 95% CI = .98–1.00, p = .046), the more likely they were to remain in treatment for 365 days. The survival curve illustrating the number of days participants were retained in treatment over the 12 months is shown in Figure 1.
Table 3.
Parameter estimates, confidence intervals, and tests statistics from Cox proportional hazards regression analysis predicting number of days retained in treatment to 365 days for sample in treatment at least 90 days (N = 248)
| Variable | Odds Ratio | 95% CI (Lower, Upper) | Wald χ2 (df=1) | p |
|---|---|---|---|---|
|
Demographics
| ||||
| Gender | 1.50 | .84, 2.70 | 1.87 | .171 |
| Race | 1.21 | .56, 2.60 | .24 | .628 |
| Age | .98 | .95, 1.02 | 1.08 | .298 |
|
| ||||
|
Baseline variables
| ||||
| Smoked crack/cocaine (Lifetime) | 1.05 | .62, 1.77 | .03 | .867 |
| On parole or probation | 1.12 | .63, 1.97 | .15 | .703 |
| Medical composite | .31 | .10, .93 | 4.33 | .037 |
| Employment composite | 2.43 | .68, 8.65 | 1.89 | .169 |
| Alcohol composite | .24 | .03, 1.95 | 1.78 | .183 |
| Drug composite | 2.90 | .15, 56.82 | .49 | .482 |
| Legal composite | 3.60 | 1.03, 12.63 | 4.00 | .045 |
| Family/Social composite | 3.45 | .56, 21.38 | 1.77 | .184 |
| Psychiatric composite | .72 | .13, 3.96 | .14 | .708 |
| Problem Recognition (PR) | .97 | .92, 1.03 | .79 | .375 |
| Desire for Help (DH) | .99 | .89, 1.11 | .02 | .894 |
| Treatment Readiness (TR) | 1.08 | .99, 1.18 | 3.09 | .079 |
|
| ||||
|
3-month variables
| ||||
| Dose at 3 month due date | .99 | .98, 1.00 | 3.97 | .046 |
| Treatment Satisfaction | .91 | .84, .99 | 5.09 | .024 |
| Counselor Services | 1.00 | .97, 1.04 | .03 | .873 |
| Problem Recognition (PR) | 1.04 | .99, 1.09 | 2.60 | .107 |
| Desire for Help (DH) | .94 | .85, 1.03 | 2.03 | .155 |
| Treatment Readiness (TR) | .98 | .91, 1.04 | .55 | .458 |
| Program site | 5.59 | .348 | ||
Note: Test statistic for Race was obtained by collapsing data into two categories: White (n = 51) v. Black/Other (n = 197).
Figure 1.
Survival curve of number of days retained in treatment over 12 months
4. Supplemental analyses
Supplemental analyses were undertaken as an alternative approach to the Cox regression analyses in order to examine treatment retention as a binary dependent variable, as has been done in some prior studies on methadone treatment retention (Joe et al., 1998, 1999; Simpson and Joe, 2004). In the first supplemental analysis, retention was defined as whether participants remained in treatment for at least 90 days (yes v. no). Logistic regression was conducted using the total sample of 351 participants and the same predictor variables (baseline ASI Composite scores and baseline Motivational scales) and covariates (gender, race, age, whether participants had a history of regularly smoking crack/cocaine, whether participants were on parole or probation, and program site) that were included in the Cox regression analysis. In the second logistic regression model of the same subsample that consisted of the 248 participants who were retained at least 90 days, retention was defined as whether participants remained in treatment for 365 days (yes v. no) and included the same predictor variables and covariates as the Cox analysis (baseline ASI Composite scores, baseline and 3-month Motivational scales, 3-month CEF Patient Satisfaction scales, 3-month methadone dose, program site, gender, race, age, whether participants had a history of regularly smoking crack/cocaine, and whether participants were on parole or probation).
As with the Cox regression analysis, results for the logistic regression showed gender (OR = .37, 95% CI = .19–.72, p = .003), Desire for Help (OR = .84, 95% CI = .74–.95, p = .007), and Treatment Readiness (OR = 1.13, 95% CI = 1.05–1.23, p = .002) to be significant predictors of days in treatment up to 90 days. Regarding retention at 365 days, results for logistic regression showed that greater levels of Treatment Satisfaction predicted retention at 365 days (OR = 1.13, 95% CI = 1.00–1.27, p = .044). However, ASI Legal and Medical Composites and 3-month dose were not significant predictors in this model (all ps > .05) as they were in the survival analysis.
Further analysis of Treatment Satisfaction
Upon finding that Treatment Satisfaction was significant in both the Cox analysis and the logistic regression analysis, two sets of additional Cox analyses were undertaken to examine the items in the scale to determine which were the most important with regard to predicting retention up to 365 days. The seven 5-point Likert items in Treatment Satisfaction scale are: 1) This program location is convenient for you; 2) Program staff here are efficient at doing their jobs; 3) Time schedules for counseling sessions at this program are convenient for you; 4) You get too much personal counseling at this program (reversed item); 5) This program is well-organized and well-run; 6) This program is requiring you to learn responsibility and self discipline; and 7) You are satisfied with this program.
For the first analysis, all seven of the individual scale items replaced the Treatment Satisfaction scale variable (all other predictor variables were the same as in the original such analyses). For the second set of analyses, each of the individual Treatment Satisfaction items replaced the Treatment Satisfaction scale score in seven separate analyses (all other independent variables were again the same as in the original analyses). Results of the first and second additional sets of analyses indicated that the only significant scale item in the Treatment Satisfaction scale was the item “This location is convenient for you” (p < .05 in both cases).
5. Discussion
This multi-site study conducted at six Baltimore-area MTPs examined factors associated with early discharge at two key time points, namely within the first 90 days and 365 days of admission to treatment. Prior research has found that the outcomes of individuals who remain in drug abuse treatment less than 90 days resemble those who received no treatment at all (Simpson, 1981; Simpson and Sells, 1982). Given the importance of a minimum of 90 day treatment retention, we first examined the factors associated with retention in treatment at this key point and found that male gender, having lower scores on the Treatment Readiness scale, and higher scores on the on the Desire for Help scale were associated with greater likelihood of earlier discharge. In a large study of statewide administrative data sets in Oregon and Washington State, Deck and Carlson (2005) also found that men were more likely to drop out of methadone treatment prematurely, although the reasons for this are not clear.
Motivation for treatment has been found to be associated with retention in methadone treatment programs (Booth et al., 2004; Simpson and Joe, 1993; Simpson et al., 1997a, 1997b; Joe et al., 1998). In the present study, higher Treatment Readiness and lower Desire for Help scores at baseline were among the factors predicting retention in treatment at 90 days. One would expect that participants with a higher desire for help at treatment entry would be more likely to be retained in treatment, although it is possible that factors unrelated to the patients’ desire for help might influence treatment retention, including arrest and events that occur during the treatment process.
The factors that were associated with retention over the course of the initial 12 months of methadone treatment for patients who had been in treatment for at least 90 days included lower severity of legal problems and higher severity of medical problems at baseline, as well as higher levels of patient satisfaction and methadone dose measured 3 months after treatment entry. In contrast to prior studies, factors such as age (Grella et al., 1997; Saxon et al., 1996; Magura et al., 1998; Deck and Carlson, 2005; Mertens and Weisner, 2000), gender (Deck and Carlson, 2005), race (Joe et al., 1991, 1998; Saxon et al., 1996), cocaine use (Grella et al., 1997; Joe et al., 1999; Deck and Carlson, 2005); and alcohol use (Grella et al., 1997; Joe et al., 1999) were not found to predict retention.
Participants who reached the 90 day post-admission point and who expressed more satisfaction with treatment were more likely to be retained in treatment at 12 months than patients who expressed less satisfaction with treatment. However, further examination of the items on the Treatment Satisfaction scale revealed that treatment program location was the only significant item in that scale. This finding is not entirely surprising, given the high patient adherence burden of daily reporting to the clinic for observed dosing posed by methadone programs in the US. The ability to earn take-home doses over time in treatment lessens the travel burden, but patients often cannot reduce their reporting schedule for many months or longer. This negative aspect of having to report daily is counterbalanced by safety to patients and to the public engendered by daily administration. In countries such as the United Kingdom, where observed dosing is not required early in treatment, overdose death appears to increase during the dose induction phase (Cornish et al., 2010). This finding is also consistent with previous research in drug-free outpatient programs in the US (Beardsley et al., 2003) and methadone programs in the US (Greenfield et al., 1996) and Iran (Shirinbayan et al., 2010) that found that greater distance between the patients’ home and the clinic was associated with higher drop-out rates. For this reason, patients may benefit from a discussion with staff at admission and during treatment regarding their travel burden and measures to relieve the burden, such as providing take home doses as appropriate, transferring to closer methadone programs, or switching to Suboxone. Mobile methadone programs may also provide more convenient access to daily methadone that would ultimately help in retaining patients (Greenfield et al., 1996).
Consistent with prior research (Booth et al., 2004; Joe et al., 1991; Saxon et al., 1996), the relationship between methadone dose at 3 months and treatment retention was significant. The mean dose in the study at 3 months was 86.3 mg (SD = 21.5), which is well above the recommended minimum dose of 60mgs (Brady et al., 2005; National Institutes of Health, 1997). This speaks well for the efforts of participating programs, as a previous national survey found that average program methadone doses were historically too low, with only 30% of patients receiving 60 mg or more in 1990 and only 65% of patients receiving 60 mg or more by 2000 (D’Aunno and Pollack, 2002).
The finding that a higher ASI Legal Composite score was associated with fewer days retained in treatment is quite important. Previous studies have noted that being on parole or probation was associated with lower treatment retention, possibly due to an increase in subsequent incarceration, which may well have resulted from a violation of probation. However, probation status is not a direct component of the Legal Composite score. It is noteworthy that two of the five items composing the Legal Composite score asked the patient to rate how seriously he or she viewed his or her legal situation and how important legal counseling was to the participant. Given the considerable numbers of MTP patients with legal problems, it is significant that few MTPs provide legal counseling (Berkman and Wechsberg, 2007), a service that MTP patients may want and need. Perhaps if Departments of Public Safety offered alternatives to incarceration for technical violations of MTP patients who do not pose a public safety risk, the likelihood of earlier discharge and “cold turkey withdrawal” from methadone during incarceration (Mitchell et al., 2009b) might be decreased.
Finally, higher ASI Medical Composite scores were associated with greater retention in treatment. This result may be related to the likelihood that individuals with greater medical problem severity may be more likely to qualify for and obtain Medicaid or Medicare. Insured patients are less subject to discharge for inability or unwillingness to pay, factors which have been found to be associated with methadone treatment discharge (Booth et al., 2004; Reisinger et al., 2009).
There are a number of limitations to the present study. The findings may not generalize to other cities in the US with different patient populations or different treatment cultures. One year treatment retention rate for our sample was fairly high (71%), due to the fact that our subsample selection procedure required us to eliminate early discharges from the analysis in order to include 3-month measures of treatment (e.g. mean dose, motivation, and patient satisfaction). Despite our relatively high retention rate, there was adequate variability in the range of number of days in treatment as evidenced by the standard deviation, which was 81.4 days, with number of days in treatment ranging from 91 to 365. Additional variables may also be of significance to patient satisfaction and resulting retention in treatment with particular regard to understudied environmental or community variables. However, program variables merit our special attention because these are more largely under our control and are thereby more subject to change. To the extent we can delineate and employ those variables in the service of patient retention and increased benefit from treatment, we have the potential to increase both patient and community well-being. Finally, the sample sizes in the two proportional hazards regression analyses may be somewhat small given the relatively large number of predictor variables examined. However, results of the supplementary analyses, which utilized different statistical methods and different assumptions and yielded essentially the same results, would suggest that insufficient power to detect an effect of interest was not a reasonable explanation for the failure to find significance. Indeed, using a general linear model approach to estimating power for the analysis in the subsample of 248 participants suggests that, for the statistical model under examination, 80% power would be achieved if the effect size (f2) in the population for any single predictor variable was .035, a value generally associated with a “small” effect size (Cohen, 1977).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ball JC, Ross A. The Effectiveness of Methadone Maintenance Treatment: Patients, Programs, Services, and Outcomes. Springer-Verlag; New York: 1991. [Google Scholar]
- Beardsley K, Wish ED, Fitzelle DB, O’Grady K, Arria AM. Distance traveled to outpatient drug treatment and client retention. J Subst Abuse Treat. 2003;25:279–285. doi: 10.1016/s0740-5472(03)00188-0. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Wechsberg WM. Access to treatment-related and support services in methadone treatment programs. J Subst Abuse Treat. 2007;32:97–104. doi: 10.1016/j.jsat.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Booth RE, Corsi KF, Mikulich-Gilbertson SK. Factors associated with methadone maintenance treatment retention among street-recruited injection drug users. Drug Alcohol Depend. 2004;74:177–185. doi: 10.1016/j.drugalcdep.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Brady TM, Salvucci S, Sverdlov LS, Male A, Kyeyune H, Sikali E, DeSale S, Yu P. Methadone dosage and retention: an examination of the 60 mg/day threshold. J Addict Dis. 2005;24:23–47. doi: 10.1300/J069v24n03_03. [DOI] [PubMed] [Google Scholar]
- Brown BS, O’Grady K, Battjes RJ, Farrell EV. Factors associated with treatment outcomes in an aftercare population. Am J Addict. 2004;13:447–460. doi: 10.1080/10550490490512780. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic Press; New York: 1977. [Google Scholar]
- Cornish R, Macleod J, Strang J, Vickerman P, Hickman M. Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK General Practice Research Database. BMJ. 2010;341:c5475. doi: 10.1136/bmj.c5475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno T, Pollack HA. Changes in methadone treatment practices: results from a national panel study, 1988–2000. JAMA. 2002;288:850–856. doi: 10.1001/jama.288.7.850. [DOI] [PubMed] [Google Scholar]
- Deck D, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two Western States. J Behav Health Serv Res. 2005;32:43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- Desmond DP, Maddux JF. Compulsory supervision and methadone maintenance. J Subst Abuse Treat. 1996;13:79–83. doi: 10.1016/0740-5472(95)02024-1. [DOI] [PubMed] [Google Scholar]
- Gibson A, Degenhardt L, Mattick RP, Ali R, White J, O’Brien S. Exposure to opioid maintenance treatment reduces long-term mortality. Addiction. 2008;103:462–468. doi: 10.1111/j.1360-0443.2007.02090.x. [DOI] [PubMed] [Google Scholar]
- Greenfield L, Brady JV, Besteman KJ, De Smet A. Patient retention in mobile and fixed-site methadone maintenance treatment. Drug Alcohol Depend. 1996;42:125–131. doi: 10.1016/0376-8716(96)01273-2. [DOI] [PubMed] [Google Scholar]
- Grella CE, Wugalter SE, Anglin MD. Predictors of treatment retention in enhanced and standard methadone maintenance treatment for HIV risk reduction. J Drug Issues. 1997;27:203–224. [Google Scholar]
- Hubbard RL, Craddock SG, Anderson J. Overview of 5-year followup outcomes in the drug abuse treatment outcome studies (DATOS) J Subst Abuse Treat. 2003;25:125–134. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychol Addict Behav. 1997;11:261–278. [Google Scholar]
- Hubbard RL, Marsden ME, Rachal JV, Harwood HI, Cavanaugh ER, Ginzburg HM. Drug Abuse Treatment: A National Study of Effectiveness. Chapel Hill; London: 1989. [Google Scholar]
- Joe GW, Broome KM, Rowan-Szal GA, Simpson DD. Measuring patient attributes and engagement in treatment. J Subst Abuse Treat. 2002;22:183–196. doi: 10.1016/s0740-5472(02)00232-5. [DOI] [PubMed] [Google Scholar]
- Joe GW, Friend HJ. Treating process factors and satisfaction with drug abuse treatment. Psychol Addict Behav. 1989;3:53–64. [Google Scholar]
- Joe GW, Simpson DD, Broome KM. Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction. 1998;93:1177–1190. doi: 10.1080/09652149835008. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD, Broome KM. Retention and patient engagement models for different treatment modalities in DATOS. Drug Alcohol Depend. 1999;57:113–125. doi: 10.1016/s0376-8716(99)00088-5. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD, Hubbard RL. Treatment predictors of tenure in methadone maintenance. J Subst Abuse. 1991;3:73–84. doi: 10.1016/s0899-3289(05)80007-0. [DOI] [PubMed] [Google Scholar]
- Kelly SM, O’Grady KE, Brown BS, Mitchell SG, Schwartz RP. The role of patient satisfaction in methadone treatment. Am J Drug Alcohol Abuse. 2010;36:150–154. doi: 10.3109/00952991003736371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly SM, Schwartz RP, O’Grady KE, Mitchell SG, Reisinger HS, Peterson JA, Agar MH, Brown BS. Gender differences among in- and out-of-treatment opioid-addicted individuals. Am J Drug Alcohol Abuse. 2009;35:38–42. doi: 10.1080/00952990802342915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight K, Holcum M, Simpson DD. TCU Psychological Functioning and Motivation Scales: Manual of Psychometric Properties. Institute of Behavioral Research, Texas Christian University; Fort Worth, Texas: 1994. [Google Scholar]
- Luborsky L, McLellan AT, Woody GE, O’Brien CP, Auerbach A. Therapist success and its determinants. Arch Gen Psychiatry. 1985;42:602–611. doi: 10.1001/archpsyc.1985.01790290084010. [DOI] [PubMed] [Google Scholar]
- Maddux JF, Desmond DP. Outcomes of methadone maintenance 1 year after admission. J Drug Issues. 1997;27:225–238. [Google Scholar]
- Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93:51–60. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, O’Brien CP. New data from the Addiction Severity Index: reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Weisner CM. Predictors of substance abuse treatment retention among women and men in an HMO. Alcohol Clin Exp Res. 2000;24:1525–1533. [PubMed] [Google Scholar]
- Metzger DS, Woody GE, McLellan AT, O’Brien CP, Druley P, Navaline H, DePhilippis D, Stolley P, Abrutyn E. Human immunodeficiency virus seroconversion among intravenous drug users in- and out-of-treatment: an 18-month prospective follow-up. J Acquir Immune Defic Syndr. 1993;6:1049–1056. [PubMed] [Google Scholar]
- Mitchell SG, Kelly SM, Brown BS, Reisinger HS, Peterson JA, Ruhf A, Agar MH, O’Grady KE, Schwartz RP. Uses of diverted methadone and buprenorphine by opioid-addicted individuals in Baltimore, Maryland. Am J Addict. 2009a;18:346–355. doi: 10.3109/10550490903077820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SG, Kelly SM, Brown BS, Reisinger HS, Peterson JA, Ruhf A, Agar MH, Schwartz RP. Incarceration and opioid withdrawal: the experiences of methadone patients and out-of-treatment heroin users. J Psychoactive Drugs. 2009b;41:145–152. doi: 10.1080/02791072.2009.10399907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan JA, Karan LD. Substance abuse treatment modalities in the age of HIV spectrum disease. J Psychoactive Drugs. 1989;21:423–429. doi: 10.1080/02791072.1989.10472188. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health (NIH) Effective medical treatment of opiate addiction. JAMA. 1997;280:1936–1943. [PubMed] [Google Scholar]
- Peles E, Linzy S, Kreek M, Adelson M. One-year and cumulative retention as predictors of success in methadone maintenance treatment: a comparison of two clinics in the United States and Israel. J Addict Dis. 2008;27:11–25. doi: 10.1080/10550880802324382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson JA, Schwartz RP, Mitchell SG, Reisinger HS, Kelly SM, O’Grady KE, Brown BS, Agar MH. Why don’t out-of-treatment individuals enter methadone treatment programs? Int J Drug Policy. 2010;21:36–42. doi: 10.1016/j.drugpo.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisinger HS, Schwartz RP, Mitchell SG, Peterson JA, Kelly SM, O’Grady KE, Marrari EA, Brown BS, Agar MH. Premature discharge from methadone treatment: patient perspectives. J Psychoactive Drugs. 2009;41:285–296. doi: 10.1080/02791072.2009.10400539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxon AJ, Wells EA, Fleming C, Jackson TR, Calsyn DA. Pre-treatment characteristics, program philosophy and level of ancillary services as predictors of methadone maintenance treatment outcome. Addiction. 1996;91:1197–1209. doi: 10.1046/j.1360-0443.1996.918119711.x. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Peterson JA, Reisinger HS, Mitchell SG, Wilson ME, Agar MH, Brown BS. In-treatment vs. out-of-treatment opioid dependent adults: drug use and criminal history. Am J Drug Alcohol Abuse. 2008;34:17–28. doi: 10.1080/00952990701653826. [DOI] [PubMed] [Google Scholar]
- Shirinbayan P, Rafiey H, Roshan AV, Narenjiha H, Farhoudian A. Predictors of retention in methadone maintenance therapy: a prospective multi-center study. Sci Res Essays. 2010;5:3231–3236. [Google Scholar]
- Simpson DD. The relation of time spent in drug abuse treatment to posttreatment outcome. Am J Psychiatry. 1979;136:1449–1453. doi: 10.1176/ajp.136.11.1449. [DOI] [PubMed] [Google Scholar]
- Simpson DD. Treatment for drug abuse: follow-up outcomes and length of time spent. Arch Gen Psychiatry. 1981;38:875–880. doi: 10.1001/archpsyc.1981.01780330033003. [DOI] [PubMed] [Google Scholar]
- Simpson DD. A conceptual framework for drug treatment process and outcomes. J Subst Abuse Treat. 2004;27:99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW. Motivation as a predictor of early dropout from drug abuse treatment. Psychother. 1993;30:357–367. [Google Scholar]
- Simpson DD, Joe GW. A longitudinal evaluation of treatment engagement and recovery stages. J Subst Abuse Treat. 2004;27:89–97. doi: 10.1016/j.jsat.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Greener JM, Rowan-Szal GA. Modeling year 1 outcomes with treatment process and post-treatment social influences. Subst Use Misuse. 2000;35:1911–1930. doi: 10.3109/10826080009148245. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Rowan-Szal GA. Drug abuse treatment retention and process effects on follow-up outcomes. Drug Alcohol Depend. 1997a;47:227–235. doi: 10.1016/s0376-8716(97)00099-9. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Rowan-Szal GA, Greener JM. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997b;14:565–572. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Sells SB. Effectiveness of treatment for drug abuse: an overview of the DARP Research Program. An evaluation of drug treatment programs. Adv Alcohol Subst Abuse. 1982;2:7–29. [Google Scholar]
- Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate- vs high-dose methadone in the treatment of opioid dependence: a randomized trial. JAMA. 1999;281:1000–1005. doi: 10.1001/jama.281.11.1000. [DOI] [PubMed] [Google Scholar]
- Villafranca SW, McKellar JD, Trafton JA, Humphreys K. Predictors of retention in methadone programs: a signal detection analysis. Drug Alcohol Depend. 2006;83:218–224. doi: 10.1016/j.drugalcdep.2005.11.020. [DOI] [PubMed] [Google Scholar]
- Zanis DA, Woody GE. One-year mortality rates following methadone treatment discharge. Drug Alcohol Depend. 1998;52:257–260. doi: 10.1016/s0376-8716(98)00097-0. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673–684. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]