Abstract
To reduce pediatric obesity in clinical settings, multidisciplinary behaviorally-based treatment programs are recommended. High attrition and poor compliance are two difficulties frequently encountered in such programs. A brief, empathic and directive clinical intervention, Motivational Interviewing (MI), might help address these motivational and behavioral issues, ultimately resulting in more positive health outcomes. The efficacy of MI as an adjunct in the treatment of pediatric obesity remains relatively understudied. MI Values was developed to implement within an existing multidisciplinary treatment program for obese, ethnically diverse adolescents, the T.E.E.N.S. Program (Teaching, Encouragement, Exercise, Nutrition, Support). T.E.E.N.S. participants who consent to MI Values are randomized to either MI or an education control condition. At weeks 1 and 10 of T.E.E.N.S. participation, the subset of participants assigned to the MI condition engage in individual MI sessions and control participants view health education videos. All MI sessions are audiotaped and coded to monitor treatment fidelity, which has been satisfactory thus far. Participants complete comprehensive assessments at baseline, 3-and 6-month follow-up. We hypothesize that MI participants will demonstrate greater reductions in Body Mass Index (BMI) percentile, improved diet and physical activity behaviors, better compliance with T.E.E.N.S., and lower attrition than participants in the control group. We present study design and methods for MI Values as well as data on feasibility of recruitment methods and treatment integrity. At study completion, findings will contribute to the emerging literature examining the efficacy of MI in the treatment of pediatric obesity.
Keywords: motivational interviewing, pediatric obesity, values
Introduction
Pediatric obesity is a major public health concern [1] with significant psychological and physiological health consequences [2–5]. Multidisciplinary, lifestyle interventions have demonstrated the greatest, although modest, efficacy to date [6, 7]. To increase effectiveness, strategies to enhance compliance with treatment and reduce attrition (often ≥50% [8]) are needed, as adolescents who adhere to treatment recommendations (i.e., attend ≥75% of intervention sessions) demonstrate sustained reductions in percent overweight [9]. Motivational Interviewing (MI) is a clinical intervention that could enhance treatment effects by increasing internal motivation to change, therefore reducing attrition and increasing compliance with treatment.
MI [10] is a brief, patient-centered counseling technique with utility across multiple behavioral domains [11–14]. People considering health behavior changes typically experience some level of ambivalence, and perceive both advantages and disadvantages to changing their behaviors. MI promotes behavior change by helping patients explore and resolve this ambivalence [10]. An important emphasis of MI is on values, and on increasing congruency between individuals’ value systems and their behaviors [15]. Consistent with humanistic theory, when a behavior/value inconsistency is highlighted, personal distress may increase (i.e., as a result of incongruence between one’s current and ideal selves) [16]. To reduce this distress, individuals will usually seek to achieve consistency between their values and behaviors through behavioral changes. By focusing on values, an individual’s sense of the importance of change is increased. Motivation to change can thus be elicited through helping patients recognize discrepancy between their deeply held beliefs or goals and their current behaviors.
MI interventions with adolescents have been effective in improving multiple health behaviors [17–20], but their utility with adolescent obesity is relatively unknown. Recent reviews have noted growing empirical and theoretical support for MI in the treatment of pediatric obesity [13, 21]. Issues identified in MI research with adolescents, and specifically related to obesity, include inadequate descriptions of MI training and practice, lack of treatment integrity measurement and reporting, and unknown dose necessary for behavior change [22, 23]. Current recommendations are that health professionals integrate MI into existing weight management practices [21, 24]. Further, studies in adult obesity have shown that adding MI early in the intervention process increases adherence and improves outcomes [25], a strategy likely applicable to adolescent obesity treatments as well.
The aim of this report is to provide the rationale and methods for a novel study of MI in the treatment of adolescent obesity. We designed and are currently implementing a study of MI Values, a randomized controlled trial examining the feasibility and efficacy of an adjunct values-based MI intervention. MI Values is implemented within an existing multidisciplinary treatment program for overweight and obese adolescents, the T.E.E.N.S. Program (Teaching Encouragement Exercise Nutrition Support). The MI Values study has three specific aims and two corresponding hypotheses:
-
Implement and evaluate the MI Values intervention for its impact on the main study outcome, adolescent body mass index (BMI) percentile.
We hypothesize that MI participants will demonstrate greater reductions in BMI percentile than participants in an education control treatment arm.
-
Examine the impact of the MI Values intervention on secondary outcomes of dietary intake, physical activity, attrition, and compliance with T.E.E.N.S.
We hypothesize that MI participants will demonstrate better dietary and physical activity behaviors, lower attrition, and higher compliance with the T.E.E.N.S. protocol than participants in an education control group.
-
Explore putative mediators and moderators of treatment effect, including gender and MI mechanisms of action.
We will explore potential mediators and moderators of treatment effect to inform future research.
Methods and Design
Overview of T.E.E.N.S
T.E.E.N.S. is an ongoing multidisciplinary treatment program at a university medical center-based weight management clinic, targeting overweight and obese, primarily African American adolescents and their families (75% African American, 65% female). Participants are eligible if they: 1) are age 11–18 years, 2) have a BMI ≥85th percentile for age and gender [26], 3) have a parent willing to participate, 4) have an identified primary care physician, and 5) have no underlying medical condition which would preclude weight loss through behavioral intervention. Participants are referred from pediatricians, school nurses, or self-referred.
T.E.E.N.S. methods have been previously reported [27–29], but briefly, include three main components: physical activity, dietary intervention, and behavior support. Participants are required to attend the T.E.E.N.S. gym at least three times per week, where they engage in supervised physical activity (strength training and cardiorespiratory exercises). They are encouraged to exercise at the YMCA (complementary memberships given) or other location of their choosing on additional days. Participants and their parent(s) attend biweekly visits with a dietitian, which include nutrition education and personalized nutrition management goals focusing on high-risk eating behaviors (e.g., sugar-sweetened beverage intake). On alternating weeks, participants attend behavioral support visits with psychology doctoral trainees, under the supervision of a licensed clinical psychologist. Behavioral support specialists use primarily cognitive behavioral therapy, including goal-setting strategies, exploring psychological factors associated with obesity, and providing positive reinforcement for behavior changes. Parent groups are also included in the protocol.
T.E.E.N.S. participants and their parents complete standardized assessments at baseline, which are repeated after 3 and 6 months of participation. These assessments, detailed elsewhere [27–29], include measurement of anthropometrics, metabolic profiles, cardiorespiratory fitness, dietary intake, physical activity frequency, and psychosocial functioning (e.g., peer victimization, body image, self-esteem). Study personnel also track participant attrition and attendance at each program component (dietitian, behavior support, and gym). Previous studies have found that participation in T.E.E.N.S. was associated with significant reductions in BMI percentile [28], improved dietary intake [29], and improved cardiovascular fitness [27]; however attrition in this intensive program was high (~55% at 6 months) and strategies to improve compliance to achieve more clinically significant outcomes were needed.
Rationale behind MI Values/Intervention Development
In an effort to improve outcomes, we designed the MI Values intervention for implementation within the T.E.E.N.S. program. MI Values targets the adolescent alone, to enhance his or her autonomy for change as independent from his or her parent(s). This strategy was designed to respect the developmental processes of individuation and identity formation [30], and take into consideration the adolescent’s readiness to change. Thus, while T.E.E.N.S. is a family-based program with significant parental involvement, the MI Values intervention focuses on the adolescent, highlighting self-efficacy and autonomy, and exploring ambivalence, resistance, and internal motivation for change. We will be able to examine if participation in MI Values enhances outcomes in T.E.E.N.S.
Experimental Design
Study procedures for both T.E.E.N.S. and MI Values are approved by the Institutional Review Board of Virginia Commonwealth University. Parents provide written, informed consent and adolescents provide written assent prior to program participation. After consenting to participate in T.E.E.N.S., participants are eligible for MI Values. This consent/assent discussion occurs immediately following the main study consent process.
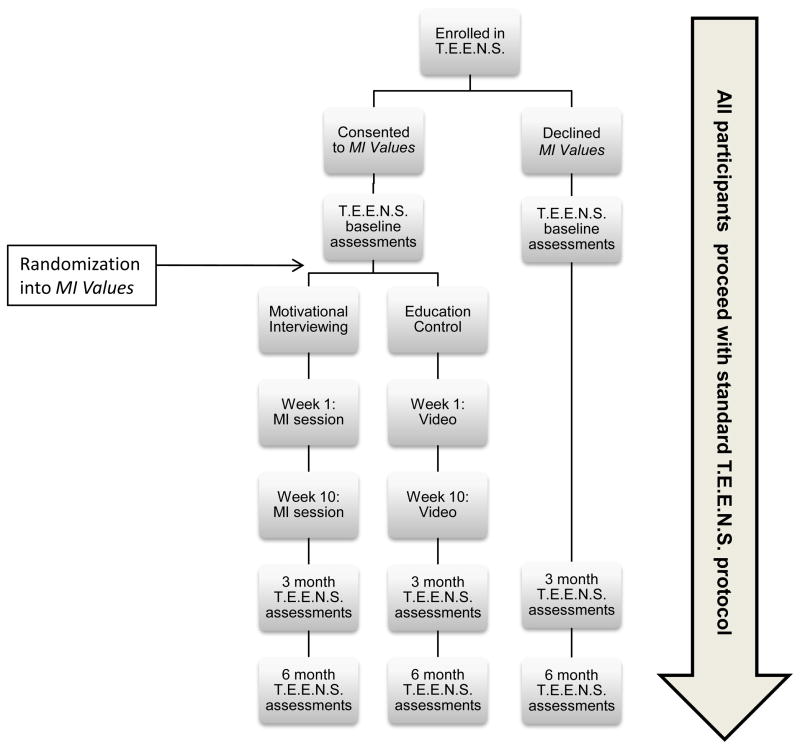
Figure 1 presents an overview of MI Values, embedded within the T.E.E.N.S. program. The MI Values study uses a repeated-measures, pretest-posttest control group design [31]. After enrolling in T.E.E.N.S. and completing baseline assessments, participants are randomized to treatment condition using a random number generator (MI or Education Control). They then complete Session 1 according to treatment condition. Ten weeks after Session 1, participants complete Session 2, also according to treatment condition. All sessions are about 30 minutes long and conducted at the T.E.E.N.S. clinic by trained MI interventionists, independent from T.E.E.N.S. Risk of contamination is low, as only MI Values interventionists are trained in MI and T.E.E.N.S. interventionists (dietitian and behavioral support specialists) are blind to participant treatment condition. To ensure treatment fidelity, all MI sessions are audiotaped and coded by independent raters to measure adherence to MI. All participants, regardless of treatment arm, proceed with treatment as usual (the T.E.E.N.S. protocol, described above). All participants complete follow-up testing at 3 and 6 months, per standard protocol.
Figure 1.
The MI Values Intervention Flowchart
The Intervention: MI Values
MI Condition
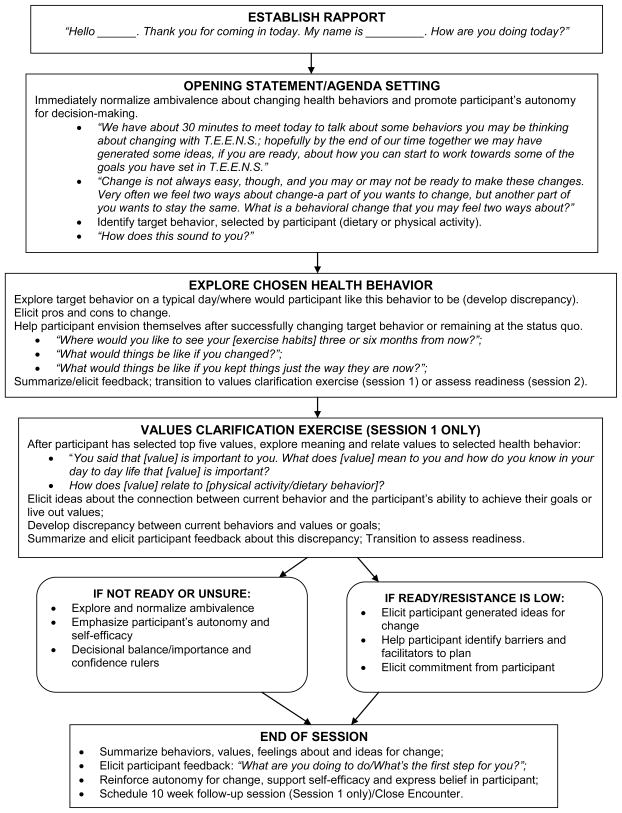
Because MI interventions that follow a treatment manual are less efficacious than those without a manual [32], we did not manualize MI Values; rather, interventionists follow a general roadmap, which includes 1) Establishing Rapport, 2) Agenda Setting, 3) Exploring Target Behavior, 4) Exploration of Values/Goals, 5) Exploration of Ambivalence and Readiness to Change, 6) Negotiating a Change Plan/Eliciting Commitment, 7) Summary. Interventionists are encouraged to be flexible, using the participant as a guide, while being faithful to the clinical style of MI. This general structure is described below and outlined in Figure 2 (note: the values clarification exercise is completed only in Session 1, although values/behavior discrepancy may be addressed in both sessions).
Figure 2.
MI Values Session Roadmap
As part of Session 1, and consistent with the values-focus of MI, participants complete a values-card sort task [33], using 39 value cards adapted for this study [33, 34]. Interventionists present value cards to participants. On each card is written a value and a clarifying statement (See Table 1), with blank cards included if participants wish to add additional values. Participants rank the cards, according to their importance to them, resulting in a selection of their top 5 values. The interventionist encourages exploration of each value and develops discrepancy between the stated value and their selected weight management behavior(s). Participants discuss why their values are important to them, and explore what connection, if any, they see between their ability to live out their values and their selected health behavior. The interventionist throughout is MI-adherent, using open questions, reflections, and affirmations to express empathy, develop discrepancy and support self-efficacy in a non-confrontational, directive manner. While the values clarification exercise is always included in this first session, interventionists follow the roadmap outlined in Figure 2 in their conduct of this MI session, which includes a variety of MI techniques (i.e., exploring readiness to change, eliciting change talk, and/or exploration of target behavior). If appropriate based on participant readiness, behavioral goals are set by the end of this session.
Table 1.
Values and descriptions from values clarification exercisea.
| Value | Description |
|---|---|
| Successful | To have important accomplishments |
| Popular | To be well-liked by others |
| Confident | To feel good about myself and my abilities |
| Independent | To not have to depend on others |
| Family | To have a happy, loving family |
| Relationship with God | To have a good relationship with God |
| Love | To give love and receive love from others |
| Honesty | To be truthful and trustworthy |
| Risk | To take risks and chances in life |
| Fitting In | To be accepted by people |
10 of 39 values presented
In the MI session conducted at week 10 of T.E.E.N.S., the MI Values interventionist explores progress in T.E.E.N.S., follows-up on the values identified in the initial session to examine how congruent current behaviors are with stated values, and elicits participant ideas for change. As in Session 1, the MI interventionist examines participants’ motivation and confidence to make dietary and/or exercise changes. To that end, the interventionist may use a variety of clinical strategies in the encounters, such as importance and confidence rulers or decisional balance. Interventionists use open-ended questions and reflections to further explore ambivalence, with the goal to elicit change talk, resolve ambivalence, highlight autonomy and support self-efficacy for change. Examples of questions (in either MI session) may include:
“You said you are a 5 on the importance ruler. What are the reasons you chose a 5 and not a 4? What would bring you to a 6?”
“What are some things you like [do not like] about your current eating [exercise] habits?”
“What do you think it would be like if you changed [did not change] your eating [exercise] habits?”
“What do you think needs to change?”
“What are your reasons for making a change? What are your reasons for not wanting to change?”
Throughout both MI sessions, the interventionist reflects the participants’ statements, and affirms the participants’ efforts. This non-confrontational strategy differs from typical clinician/patient interactions, in that information is only given if it is directly requested by the patient, and the ideas for change are generated by the patient.
Control Condition
MI Values interventionists proctor two, 30 minute sessions with control participants, also at weeks 1 and 10. This choice of control group: 1) maintains constant contact between groups, and 2) compares MI to an educational intervention [21]. In each session, participants view a health education video, focused on healthy eating and exercise for adolescents. Participants complete a knowledge quiz during/after this video to ensure treatment adherence. The focus on information mirrors the usual care provided in the healthcare setting, which typically involves encouraging patients to make changes based on information and direct persuasion [35]. However, MI assumes that behavior change is elicited by intrinsic motivation, not information alone [10] and that patients do not necessarily want or need advice [36], thus it is not expected that this condition will provide benefit or harm to the participant. We also do not expect significant improvements beyond those elicited by the standard T.E.E.N.S. protocol.
Intervention Fidelity
As described, MI is a complex clinical intervention; thus an important focus in MI Values is on training and supervision to ensure competency and fidelity are maintained. Interventionists participated in a 2-day training conducted by a member of the Motivational Interviewing Network of Trainers (MINT). These workshops have been found to be important, but not sufficient, to establish competent MI interventionists [37]. Thus 30 hours of practice with weekly supervision and feedback of audiotaped sessions was provided until interventionists met or exceeded competency thresholds set in the Motivational Interviewing Treatment Integrity (MITI) Code 3.0 [38] and as judged by an MI expert. The MITI 3.0 [38] is a behavioral coding system that measures adherence to MI. Throughout the intervention, trained raters code randomly selected 20 minute segments of each MI session in a single pass. The MITI 3.0 has two dimensions: behavior counts (e.g., tallies of clinician behaviors: giving information, open and closed questions, simple and complex reflections, MI-adherent and non-adherent behaviors) and global scores (e.g., empathy, direction, collaboration, evocation, and autonomy). Suggested thresholds are provided in the MITI 3.0 for establishing competent interventionists based on behavior counts and global ratings of MI proficiency.
Independent raters were trained to rate MI sessions using the MITI 3.0. This two day (8 hour) training included an overview of intervention fidelity, instruction on how to parse and code clinician utterances and how to use the MITI 3.0. Over 30 hours of group rating sessions were then completed, which included rating pre-scored gold-standard transcripts from motivationalinterviewing.org and comparing team ratings to those provided on this training website. Immediate feedback was given to raters and modifications made. Thirty audiotaped sessions were coded by three independent raters, using the MITI 3.0, to obtain satisfactory intraclass correlations (e.g., ICC = 0.6–1.0), and indicate readiness for study involvement.
To ensure continued interrater reliability, weekly group coding sessions are conducted throughout the study period to ensure rater drift does not occur. Ten percent of all study sessions are independently coded by all raters, to re-establish interrater reliabilities throughout the study duration. MI interventionists meet weekly for supervision with a licensed clinical psychologist, with expertise in MI (M.K.B.), to provide feedback about audiotaped MI sessions and ensure continued competence and adherence to the clinical intervention.
Power Analysis
Power analyses were conducted to determine the needed sample size to assess the main study outcome, BMI percentile. Power calculations indicated that, at a two-sided 5.0% significance level (alpha = 0.05), a sample size of approximately 60 individuals per condition (i.e., MI or control) would have sufficient power to detect a total mean BMI percentile difference of 1.0 between groups. Calculations are based on a power level of 0.80 if the true difference between the conditions is 2.326 times the standard deviation and a 2.0% percentile difference with 0.80 power if the true difference between the conditions is 2.054 times the standard deviation. Given our past experience with recruitment and retention in T.E.E.N.S., we plan to recruit 80 individuals per condition.
Results and Discussion
MI Values strengths include its design (randomized controlled trial), target population (primarily African American adolescents from low socioeconomic status), and emphasis on treatment integrity. As noted, major limitations to the extant literature examining the efficacy of MI in pediatric obesity are the paucity of rigorously designed trials and lack of data on intervention fidelity [21, 23]. Thus, we present and discuss preliminary data on intervention fidelity below.
Intervention Fidelity
Table 2 presents adherence to MI and corresponding competency thresholds, as measured by the MITI 3.0 [38]. Interventionists have exceeded these thresholds, demonstrating MI competency, with the exception of the low ratio of questions to reflections. The questions posed by interventionists in the values clarification exercise in Session 1 may have contributed to this lower ratio. Additionally, it has been suggested that in order to elicit responses, MI with children may involve providers asking more questions, as opposed to stating reflections [21]. We will further investigate these issues upon study completion.
Table 2. MI Values.
Interventionists’ Proficiency with MI Based on the MITI 3.0b
| MITI Domain | Mean Interventionist Rating c |
Competency Threshold | |
|---|---|---|---|
| Session 1 M (SD) | Session 2 M (SD) | ||
| Global Spiritd | 4.36 (0.39) | 4.55 (0.40) | 4 |
| Reflection:Questione | 0.95 (0.33) | 1.11 (0.90) | 2i |
| % Complex Reflectionsf | 79% (0.11) | 76% (0.13) | 50% |
| % Open Questionsg | 83% (0.10) | 83% (0.09) | 70% |
| % MI Adherenth | 100% (0.0) | 100% (0.0) | 100% |
MITI 3.0=Motivational Interviewing Treatment Integrity Code, Version 3.0
Scores based on n=44 interviews at Session 1 and n=31 interviews at Session 2; Average of 2 interventionists presented
Global Spirit = (Evocation + Collaboration + Autonomy)/3
Ratio = Total Reflections/Total Questions
% Complex Reflections = (Complex Reflections/Total Reflections) x100
% Open Questions = (Open Questions/Total Questions) x100
% MI Adherent= MI Adherent/(MI Adherent + MI Non-adherent)
Beginner Proficiency = 1 (1:1 ratio of reflections to questions); Competency 2 = (2:1 ratio of reflections to questions)
Although it has been suggested that 40 hours of rater training is typically required to achieve interrater reliability using the MITI 3.0 [38], no predetermined number of training hours was set. Rather, MI Values raters maintained consistent, satisfactory interrater reliability after 30 hours, and thus initiated study involvement with intraclass correlations (ICCs) all ≥0.80. Weekly group rating identifies and attempts to minimize rater drift. To date, raters have demonstrated adequate to satisfactory ICCs, with ICCs for behavior counts ranging from 0.78–1.00, and ICCs for global scores ranging from 0.50–1.00. Particular attention continues to be given to global scores in group rating sessions. Due to limited ranges on global scales (1.0–5.0) maintaining high ICCs is more challenging than it is for behavior counts, with greater variability and a larger response range. Overall, this model of training and supervision has been effective at maintaining treatment integrity, with areas of improvement identified.
Feasibility of Recruitment
The MI Values study recruits participants from T.E.E.N.S., an intensive treatment program, requiring ≥3x/week participation in program activities for 6-months. Due to the low additional burden of MI Values (two 30-minute sessions, occurring on the same day as another T.E.E.N.S. activity), we anticipated few refusals. To date, 85% of T.E.E.N.S. participants have also consented to the MI Values study. This 15% refusal rate into the adjunct study is higher than expected, and may suggest that some families are feeling overwhelmed by the intensity of T.E.E.N.S. These and other reasons for refusal will be investigated.
This model of recruitment and intervention delivery was designed to present minimal burden on participants. No additional clinic visits are required and all MI Values study sessions take place within the T.E.E.N.S facility, reducing barriers such as unfamiliarity with location or additional travel. Embedding MI Values within T.E.E.N.S. likely contributes to the high attendance rate thus far; of participants who consented to MI Values, 96% completed Session 1 per protocol. Analysis of exit interviews and attendance data will allow for closer examination of the feasibility of this approach.
Analysis of Specific Aims
Investigation of the primary and secondary study outcomes will inform understanding of the efficacy of MI in eliciting reductions in BMI percentile and improvements in treatment compliance, attrition, and dietary and physical activity behaviors, compared to an education control group. We will also be able to explore the mechanisms for change. The detailed process evaluation will allow for discussion of feasibility with respect to participants’ perceptions, ease of administration of the intervention, competence and treatment integrity.
The most effective treatment dose for MI in obesity has not been determined, and might be complicated by the fact that multiple behaviors contribute to obesity. Session timing and frequency in MI Values was informed by 1) research suggesting that MI early in the intervention process is effective [32], and 2) the examination of earlier cohorts of T.E.E.N.S. demonstrating high attrition around 12 weeks. It is possible that the initial MI session should be conducted earlier in T.E.E.N.S., prior to any program activities. For example, in an adult obesity trial, participants who completed orientation sessions, grounded in MI, which explored ambivalence about changing eating and exercise behaviors prior to randomization demonstrated very high (96%) retention at 18-months [25]. These issues should be considered with adolescent obesity trials.
As noted above, another complication inherent in examining MI in obesity is that “obesity” is not a behavior; rather, several behaviors contribute to the development and maintenance of obesity. Thus questions remain about which behavior should be targeted and if MI is equally efficacious for both diet and physical activity. MI Values participants select which behavior to focus on (consistent with the spirit of emphasizing choice and autonomy), which will allow us to begin to answer these questions.
Developmental Considerations
Developmentally, MI has been viewed as an appropriate strategy for counseling adolescents to make health behavior changes. Major tasks of adolescence are individuation and autonomy development, often involving pushing against authority figures and experiencing ambivalence [30]. Because MI is a clinical style that is respectful, non-confrontational, and acknowledges choices, it can be helpful in minimizing resistance. Questions remain about who (i.e., parent, adolescent, or both) should be the target of MI in pediatric interventions [13, 21]. There is some evidence that intervening directly with older obese adolescents is more effective than including their parents [21]. Similarly, a systematic review of lifestyle interventions for the treatment of obesity suggested that parental involvement may be most effective for youth ages 8 years and younger; these data also support intervening directly with adolescents [6]. It is unknown at which age or developmental level MI should be conducted with the parent, the child or adolescent, or both. Considering these developmental tasks, however, MI Values intervenes directly with the adolescent, to instill autonomy and foster adolescents’ growing independence. Further, MI Values occurs within the context of a larger, family-based treatment program, where parents are participating in program activities; thus their exclusion from MI Values was deemed appropriate and still within the recommendations that multidisciplinary obesity treatments include parental involvement [39].
MI Values implements a values clarification exercise using value cards and targeted questions, to develop discrepancy and help build intrinsic motivation for change. Use of this strategy with adolescents is not well examined within the context of an MI intervention, although there is support for its developmental appropriateness. Adolescents are striving to achieve consistency between values, beliefs, and behaviors, as they achieve greater independence from their parents, and seek to develop a sense of coherence in their identity [13]. A clinical intervention which builds on these developmental tasks may thus be effective in eliciting change. However, recent research also suggests that some adolescents have difficulty with this task [34]. Our findings will provide additional data regarding both potential benefits of the MI approach, and use of the values clarification exercise within it.
Cultural Appropriateness
MI’s cultural appropriateness with African American adolescents is not well-examined. This patient-centered, values-based approach appears inherently culturally appropriate, as participants select and express their own values and beliefs. The interventionist then uses the participant’s own words to highlight this value/behavior discrepancy and elicit change talk. Further, a meta-analysis of MI and health behavior change found a larger effect size when MI was used with ethnic minority patients versus White samples [32]. However, additional research is needed on the cultural appropriateness specifically for African American adolescents, which findings from MI Values may help support.
Other Strategies for Improving Compliance/Reducing Attrition
T.E.E.N.S. targets a population in which high attrition is frequently encountered (i.e., 46% uninsured/Medicaid, 75% African American, severely obese [mean BMI = 99th percentile]) [40]. T.E.E.N.S. uses multiple strategies recommended to combat attrition and reduce barriers to participation [8]. These include making repeated contact with participants, implementing a culturally sensitive intervention, flexibility, use of incentives, free and plentiful parking, and easy access via city transportation. Further, consistent with the cognitive behavioral therapy approach, parents provide collaboratively determined reinforcements to participants for meeting interim goals. Thus, the addition of MI to these existing strategies may be helpful in reducing attrition/increasing compliance.
Conclusion
The solution to pediatric obesity will be multi-pronged, and include policy, environmental, and individual level-change. At the individual level, reducing dietary intake and increasing physical activity are essential. Within multidisciplinary treatment programs, strategies to reduce attrition, improve compliance, and enhance outcomes are needed. MI might represent a brief clinical intervention to help meet these needs, by focusing on adolescents’ internal motivation for change, highlighting autonomy, and eliciting reasons for change in a nonconfrontational, collaborative way. The MI Values study will further research in this important area and inform the development of future investigations, building on this MI-based approach to obesity treatment.
Acknowledgments
This study was supported by a grant from the American Cancer Society to MK Bean [PFT-08-144-01-CPPB]. The conduct for this study was also supported by the National Institutes of Health [M01 RR00065 - VCU General Clinical Research Center]. These funding sources had no involvement with the conduct of the research or preparation of the manuscript. We are grateful to Priscilla Powell, MS and Alexis Quinoy, BS for their work as MI Values interventionists, to Alyssa Forcehimes, PhD for facilitating our motivational interviewing training, to Sonya Satterlund, BS, Robert Coltrain, BS, Lauren Almond, and April Hafer for their work as coders, and to Jessye Cohen, MS, for her assistance with the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of High Body Mass Index in US Children and Adolescents, 2007–2008. JAMA: The Journal of the American Medical Association. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Kiess W, Galler A, Reich A, Muller G, Kapellen T, Deutscher J, et al. Clinical aspects of obesity in childhood and adolescence. Obes Rev. 2001;2:29–36. doi: 10.1046/j.1467-789x.2001.00017.x. [DOI] [PubMed] [Google Scholar]
- 3.Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002;40:441–7. doi: 10.1161/01.hyp.0000032940.33466.12. [DOI] [PubMed] [Google Scholar]
- 4.Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, et al. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Public Health. 1992;82:358–63. doi: 10.2105/ajph.82.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 6.McGovern L, Johnson JN, Paulo R, Hettinger A, Singhal V, Kamath C, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93:4600–5. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 7.Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Karlson CW, Rapoff MA. Attrition in Randomized Controlled Trials for Pediatric Chronic Conditions. Journal of Pediatric Psychology. 2009;34:782–93. doi: 10.1093/jpepsy/jsn122. [DOI] [PubMed] [Google Scholar]
- 9.Kalarchian MA, Levine MD, Arslanian SA, Ewing LJ, Houck PR, Cheng Y, et al. Family-Based Treatment of Severe Pediatric Obesity: Randomized, Controlled Trial. Pediatrics. 2009;124:1060–8. doi: 10.1542/peds.2008-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 11.Sindelar HA, Abrantes AM, Hart C, Lewander W, Spirito A. Motivational interviewing in pediatric practice. Curr Probl Pediatr Adolesc Health Care. 2004;34:322–39. doi: 10.1016/j.cppeds.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Dunn AL, Resnicow K, Klesges LM. Improving measurement methods for behavior change interventions: opportunities for innovation. Health Educ Res. 2006;21 (Suppl 1):i121–4. doi: 10.1093/her/cyl141. [DOI] [PubMed] [Google Scholar]
- 13.Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: a review. Arch Pediatr Adolesc Med. 2005;159:1173–80. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- 14.Bisono A, Manuel J, Forcehimes A. Promoting treatment adherence through motivational interviewing. In: O'Donohue W, Levensky E, editors. Promoting Patient Adherence. Thousand Oaks: Sage; 2006. pp. 71–84. [Google Scholar]
- 15.Wagner C, Sanchez F. The role of values in motivational interviewing. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People to Change. 2. New York: Guildford Press; 2002. pp. 284–98. [Google Scholar]
- 16.Rogers CR. Toward a Modern Approach to Values: The Valuing Process in the Mature Person. J Abnorm Psychol. 1964;68:160–7. doi: 10.1037/h0046419. [DOI] [PubMed] [Google Scholar]
- 17.Kelly AB, Lapworth K. The HYP program-targeted motivational interviewing for adolescent violations of school tobacco policy. Prev Med. 2006;43:466–71. doi: 10.1016/j.ypmed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Berg-Smith SM, Stevens VJ, Brown KM, Van Horn L, Gernhofer N, Peters E, et al. A brief motivational intervention to improve dietary adherence in adolescents. The Dietary Intervention Study in Children (DISC) Research Group. Health Educ Res. 1999;14:399–410. doi: 10.1093/her/14.3.399. [DOI] [PubMed] [Google Scholar]
- 19.Channon S, Smith VJ, Gregory JW. A pilot study of motivational interviewing in adolescents with diabetes. Arch Dis Child. 2003;88:680–3. doi: 10.1136/adc.88.8.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knight JR, Sherritt L, Van Hook S, Gates EC, Levy S, Chang G. Motivational interviewing for adolescent substance use: a pilot study. J Adolesc Health. 2005;37:167–9. doi: 10.1016/j.jadohealth.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–33. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Martins RK, McNeil DW. Review of Motivational Interviewing in promoting health behaviors. Clinical Psychology Review. 2009;29:283–93. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Suarez M, Mullins S. Motivational interviewing and pediatric health behavior interventions. J Dev Behav Pediatr. 2008;29:417–28. doi: 10.1097/DBP.0b013e31818888b4. [DOI] [PubMed] [Google Scholar]
- 24.VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: a review of the evidence. Diabetes Educ. 2004;30:404–6. 8–10, 14–6. doi: 10.1177/014572170403000309. passim. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20:439–47. doi: 10.1093/her/cyg139. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Clinical Growth Charts. Available at: http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/clinical_charts.htm.
- 27.Evans RK, Franco RL, Stern M, Wickham EP, Bryan DL, Herrick JE, et al. Evaluation of a 6-month multi-disciplinary healthy weight management program targeting urban, overweight adolescents: effects on physical fitness, physical activity, and blood lipid profiles. Int J Pediatr Obes. 2009;4:130–3. doi: 10.1080/17477160802314997. [DOI] [PubMed] [Google Scholar]
- 28.Wickham EP, Stern M, Evans RK, Bryan DL, Moskowitz WB, Clore JN, et al. Prevalence of the metabolic syndrome among obese adolescents enrolled in a multidisciplinary weight management program: clinical correlates and response to treatment. Metab Syndr Relat Disord. 2009;7:179–86. doi: 10.1089/met.2008.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bean MK, Mazzeo SE, Stern M, Evans RK, Bryan D, Ning Y, et al. Six-Month Dietary Changes in Ethnically Diverse, Obese Adolescents Participating in a Multidisciplinary Weight Management Program. Clinical Pediatrics. doi: 10.1177/0009922810393497. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baer JS, Peterson PL. Motivational interviewing with adolescents and young adults. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People to Change. 2. New York: Guilford Press; 2002. pp. 320–32. [Google Scholar]
- 31.Campbell DT, Stanley JC. Experimental and Quasi-Experimental Designs for Research. Chicago: Rand-McNally; 1963. [Google Scholar]
- 32.Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 33.Miller WR, C'de Baca J. Quantum Change: When Epiphanies and Sudden Insights Transform Ordinary Lives. New York: Guilford Press; 2001. [Google Scholar]
- 34.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13:1739–48. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 35.Tuckett DA, Boulton M, Olson C. A new approach to the measurement of patients' understanding of what they are told in medical consultations. J Health Soc Behav. 1985;26:27–38. [PubMed] [Google Scholar]
- 36.Stott NC, Pill RM. 'Advise yes, dictate no'. Patients' views on health promotion in the consultation. Fam Pract. 1990;7:125–31. doi: 10.1093/fampra/7.2.125. [DOI] [PubMed] [Google Scholar]
- 37.Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A Randomized Trial of Methods to Help Clinicians Learn Motivational Interviewing. Journal of Consulting and Clinical Psychology. 2004;72:1050–62. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- 38.Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. The Motivational Interviewing Treatment Intergrity (MITI) Code: Version 3.0. University of New Mexico, Center on Alcoholism, Substance Abuse, and Addictions; 2007. [Google Scholar]
- 39.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 (Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 40.Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, Santangelo M, et al. Predictors of attrition from a pediatric weight management program. The Journal of Pediatrics. 2004;144:466–70. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]