Abstract
Background
The lateral femoral cutaneous nerve (LFCN) can be at risk during, for example, the insertion of pins in the anterior superior iliac spine (ASIS) during external fixation of the pelvis, total hip arthroplasty through a direct anterior approach, open surgery for impingement in the hip through an anterior approach, and periacetabular osteotomy. During surgery, the surgeon usually assumes the location of the LFCN by using the ASIS as a landmark.
Questions/purposes
We investigated (1) whether there is any relationship between the LFCN and the ASIS and (2) the anatomy of the LFCN at the lateral border of the psoas major.
Methods
Using 25 formalin-fixed cadavers, we determined the location of the LFCN emergence point as above, same level with, or below the iliac crest (IC). We measured the distances between the LFCN emergence point and the crossing of the IC and psoas major, ASIS, and pubic tubercle. We measured the distances between the ASIS and pubic tubercle (AB) and the ASIS and the point where the LFCN crossed the inguinal ligament (AC) and then calculated AC/AB.
Results
The LFCN was below the IC on 19 sides, at the same level on 13 sides, and above on 12 sides. The distances were −0.98 ± 5.57 cm to the IC, 12.39 ± 2.67 cm to the ASIS, and 17.76 ± 3.33 cm to the pubic tubercle. AB was 13.11 ± 1.08 cm, AC 2.95 ± 2.01 cm, and AC/AB 0.22 ± 0.16.
Conclusions/Clinical Relevance
The LFCN may emerge from the lateral border of the psoas major above or below the IC. The AC/AB ratio can help surgeons to find the LFCN in patients with different body types.
Introduction
The LFCN has received much attention owing to its importance during harvesting of IC bone graft, fixation of acetabular fractures [6], insertion of pins in the ASIS during external fixation of the pelvis, anterior surgical approaches to the hip and pelvis, and ilioinguinal approach to the acetabulum [8]. It also can be affected by tight clothing, obesity, IC disorders [7], limb-length discrepancy [2], pelvic inflammatory disease, toxic neuropathies [16], and surgical interventions such as cardiac catheterization [2], inguinal herniorrhaphy, laparoscopic cholecystectomy [16], and appendectomy [10]. Its best-known clinical disorder is meralgia paresthetica, which is characterized by numbness, burning, or pain over the anterior and lateral aspects of the thigh [15].
The LFCN arises from the dorsal branches of the second and third lumbar ventral rami and emerges from the lateral border of the psoas major (PM), crossing the iliac muscle obliquely toward the ASIS. The LFCN passes behind or through the inguinal ligament (IL), medial to the ASIS and anterior to the sartorius muscle [12].
The LFCN can be damaged along its entire course and cause symptoms. The incidence of meralgia paresthetica has been reported to be between 6.7% and 35% [16]. Because of this relatively high incidence, there are numerous studies regarding the anatomy of the LFCN [1–6, 8, 9, 13–16]. When these studies are examined, it can be seen that most are about the relationship between the LFCN and the structures in the inguinal region. These studies have investigated the distance between the LFCN and the ASIS [5, 6, 8, 9, 15, 16], between the LFCN and the femoral artery [6], the position of the nerve according to ASIS (ie, medial or superolateral) [14], the relationship of the LFCN to the IL (behind, through, or in front of) [15], and the relationship of the LFCN to some fascial planes [3]. One study appeared different by measuring distances between the branches of the lumbar plexus and bony landmarks and imaginary lines at the posterior abdominal wall [17].
In the literature and textbooks, the LFCN is defined as emerging from the lateral side of the PM, but there is limited information about the level of this emergence regarding the IC (ie, above or below the IC). Furthermore, all studies in the literature regarding the relationship between the LFCN and the ASIS measured only the distance between them without considering the individual variations (ie, height, body type) in people. Therefore, we attempted to determine the ratio of the ASIS-LFCN distance to the length of the IL.
In this study, we (1) determined the location of the emergence point of the LFCN at the lateral border of the PM relative to the IC; (2) determined distances of the emergence point of the LFCN to certain bony landmarks, ie, the ASIS and the pubic tubercle (PT); (3) determined the position of the LFCN relative to the IL; and (4) calculated the ratio of the ASIS-LFCN distance to the ASIS-PT distance (ie, length of the IL) to determine whether this ratio is a reliable guide to estimate the position of the LFCN behind the IL.
Materials and Methods
This study was conducted in 25 formalin-fixed cadavers (12 males, 13 females; age range, 36–80 years) at the Istanbul University (10 cadavers) and the University of Cologne (15 cadavers). The course of the LFCN, starting from the point where it left the lateral border of the PM until it passed behind the IL, was examined. The distal course and branching pattern of the LFCN distally to the IL were not studied.
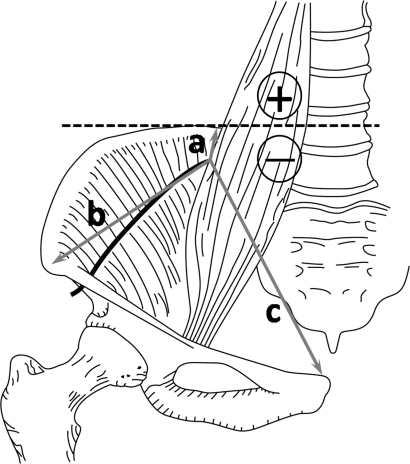
We examined formation of the LFCN at the lateral side of the PM, the existence of an accessory LFCN(s), the course in the greater pelvis, and the relationships with the ASIS and the IL. The measurements were taken in two aspects: intraabdominal and inguinal. The intraabdominal measurements were taken between the point where the LFCN left the lateral border of the PM and the visible medial end (back margin) of the IC (a), the ASIS (b), and the PT (c) (Fig. 1). When the LFCN emerged from the PM above the IC, positive values were given to the LFCN-IC distance; when the LFCN emerged below the IC, negative values were given. In four sides, two branches (possibly the dorsal branches of the ventral rami of spinal nerves) emerged from the lateral border of the PM and united to form the LFCN. In each of those four sides, both branches were measured separately. The intraabdominal (a, b, and c) distances were measurable in 40 sides. In four of those sides, the LFCN emerged as two branches, so 44 measurements were taken in total (Table 1). There were no accessory LFCNs.
Fig. 1.
The intraabdominal measurements of the LFCN are shown: the distance between the emergence point of the LFCN and the IC (a); the distance between the emergence point of the LFCN and ASIS (b); and the distance between the emergence point of the LFCN and the PT (c). (Reproduced with permission of TheJournal of Bone and Joint Surgery-American Volume from Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000;82:746–747.)
Table 1.
Intraabdominal distances of the LFCN to certain bony landmarks
| Institution | Cadaver | Gender | Intraabdominal distances (cm) | |||||
|---|---|---|---|---|---|---|---|---|
| Right | Left | |||||||
| a | b | c | a | b | c | |||
| Istanbul University | 1 | Male | −3.7 | 10.3 | 17 | −1.5 | 9.6 | 17 |
| 2 | Male | −17 | 11.6 | 15.1 | 7.8 | 19.6 | 24.8 | |
| 3 | Male | NA | NA | NA | NA | NA | NA | |
| 4 | Male | 1.9 | 14 | 22 | 4.9 | 17 | 24 | |
| 5 | Male | −24 | 16 | 14 | 9 | 14.2 | 17.5 | |
| 6 | Male | −2.6 | 9.5 | 13.6 | −4 | 9.1 | 12.4 | |
| 7 | Female | 0 | 13 | 18 | 6.6 | 17.1 | 23.8 | |
| 8 | Female | 7.5 | 16.8 | 23.5 | −5.8 | 8.5 | 10.3 | |
| 9 | Female | −3.8 | 9.24 | 16 | NA | NA | NA | |
| 10 | Female | 2 | 13.5 | 19 | 0.8 | 12.5 | 16.5 | |
| University of Cologne | 1 | Male | −2.88 | 10.89 | 22.1 | NA | NA | NA |
| 2 | Male | 0 | 10.27 | 17 | NA | NA | NA | |
| 3 | Male | 0, −3.4 | 13.5, 10.5 | 19.8, 14.5 | NA | NA | NA | |
| 4 | Male | 0 | 12.7 | 18 | 0 | 9.95 | 18.5 | |
| 5 | Male | 3.88 | 17.8 | 23.16 | 0 | 14.2 | 20 | |
| 6 | Male | −2 | 11.17 | 15.4 | NA | NA | NA | |
| 7 | Female | −1.17 | 11.21 | 15.7 | 0, 1.73 | 11.89, 12.92 | 17.5, 18 | |
| 8 | Female | 0 | 12.81 | 14.43 | 0 | 13.17 | 18.3 | |
| 9 | Female | 0, −2.3 | 12.69, 11.9 | 17.28, 16.12 | 2.52 | 14.1 | 20.5 | |
| 10 | Female | −5.67 | 10.5 | 19.3 | NA | NA | NA | |
| 11 | Female | 0 | 12.38 | 17.4 | NA | NA | NA | |
| 12 | Female | −1.85 | 11.92 | 18.6 | 3.4 | 16 | 22.4 | |
| 13 | Female | −4.75 | 8.47 | 14.43 | −3.77 | 9.84 | 15.4 | |
| 14 | Female | NA | NA | NA | 0 | 12.5 | 18.2 | |
| 15 | Female | 0, −3.02 | 11.01, 9.06 | 16.3, 13.83 | −2.09 | 10.12 | 14.61 | |
Intraabdominal measurements were taken between the point where the LFCN leaves the lateral border of the psoas major and the visible medial end (back margin) of the iliac crest (a), the anterior superior iliac spine (b), and the pubic tubercle (c) (Fig. 1); LFCN = lateral femoral cutaneous nerve; NA = not available.
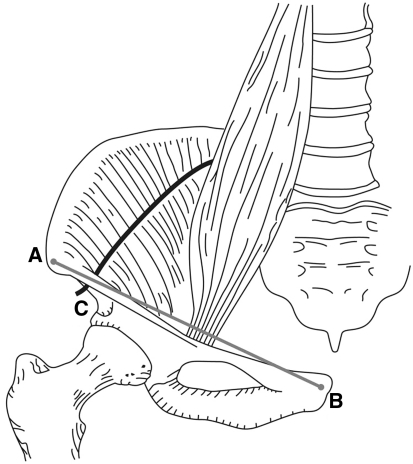
The AB and AC distances were detectable in 42 sides (Table 2). The inguinal measurements were the length of the IL (AB) and the distance between the ASIS and the point where the LFCN crossed the IL (AC) (Fig. 2); by using these two measurements, the AC/AB ratio was calculated. In some cadavers, some measurements of the LFCN could not be performed owing to accidental traumas during the dissections for educational purposes; those nerves were indicated as “NA” in the tables. In the cadavers where the a, b, c and AC and AB distances could be measured on both sides, these distances were compared using the Wilcoxon test. Because of the limited number of specimens, differences between the genders could not be examined.
Table 2.
Inguinal measurements of the LFCN
| Institution | Cadaver | Gender | Inguinal distances (cm) | |||||
|---|---|---|---|---|---|---|---|---|
| Right | Left | |||||||
| AB | AC | AC/AB | AB | AC | AC/AB | |||
| Istanbul University | 1 | Male | 15 | 6.3 | 0.42 | 14.5 | 5.7 | 0.39 |
| 2 | Male | 13.5 | 6.3 | 0.47 | 13.9 | 3.3 | 0.24 | |
| 3 | Male | NA | NA | NA | 12.5 | 3 | 0.24 | |
| 4 | Male | 14 | 3.8 | 0.27 | 13.1 | 2.6 | 0.20 | |
| 5 | Male | 16.2 | 2.7 | 0.17 | 14.8 | 1 | 0.07 | |
| 6 | Male | 13.5 | 2.3 | 0.17 | 12 | 1.5 | 0.13 | |
| 7 | Female | 13.2 | 4.9 | 0.37 | 12.4 | 5.6 | 0.45 | |
| 8 | Female | 13.5 | 2.8 | 0.21 | 12 | 9.2 | 0.77 | |
| 9 | Female | 11.8 | 1.4 | 0.12 | 10.7 | 6.7 | 0.63 | |
| 10 | Female | 11.5 | 2.8 | 0.24 | 12.9 | 2 | 0.16 | |
| University of Cologne | 1 | Male | 14.18 | 3.21 | 0.23 | NA | NA | NA |
| 2 | Male | 13.9 | 5.13 | 0.37 | 13.3 | 0.9 | 0.07 | |
| 3 | Male | NA | NA | NA | 14.12 | 3 | 0.21 | |
| 4 | Male | 13.7 | 2.07 | 0.15 | 13.24 | 5 | 0.38 | |
| 5 | Male | 13.09 | 0.63 | 0.05 | NA | NA | NA | |
| 6 | Male | 12.88 | 1.49 | 0.12 | NA | NA | NA | |
| 7 | Female | 13.02 | 1.44 | 0.11 | 13.41 | 1.53 | 0.11 | |
| 8 | Female | 11.66 | 1.32 | 0.11 | 12.92 | 0.74 | 0.06 | |
| 9 | Female | 13.12 | 1.11 | 0.08 | 12.79 | 0.6 | 0.05 | |
| 10 | Female | 14.07 | 3.63 | 0.26 | NA | NA | NA | |
| 11 | Female | 12.66 | 0.8 | 0.06 | NA | NA | NA | |
| 12 | Female | 12.71 | 1.41 | 0.11 | 13.04 | 1.43 | 0.11 | |
| 13 | Female | 11.79 | 3.36 | 0.28 | 11.09 | 3.08 | 0.28 | |
| 14 | Female | NA | NA | NA | 14.08 | 3.98 | 0.28 | |
| 15 | Female | 12.07 | 0.74 | 0.06 | 12.8 | 1.01 | 0.08 | |
Inguinal measurements were the length of the inguinal ligament (AB) and the distance between the anterior superior iliac spine and the point where the LFCN crosses the inguinal ligament (AC) (Fig. 2); by using these two measurements, the AC/AB ratio was calculated; LFCN = lateral femoral cutaneous nerve; NA = not available.
Fig. 2.
The inguinal measurements of the LFCN are shown: the distance between the ASIS and the LFCN (AC) and the distance between the ASIS and the PT (AB). (Reproduced with permission of TheJournal of Bone and Joint Surgery-American Volume from Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000;82:746–747.)
Results
The emergence point of the LFCN was above the IC (Fig. 3) in 12 (27%) sides, at the same level with the IC (Fig. 4) in 13 sides (30%), and below the IC (Fig. 5) in 19 sides (43%) (Table 1).
Fig. 3.
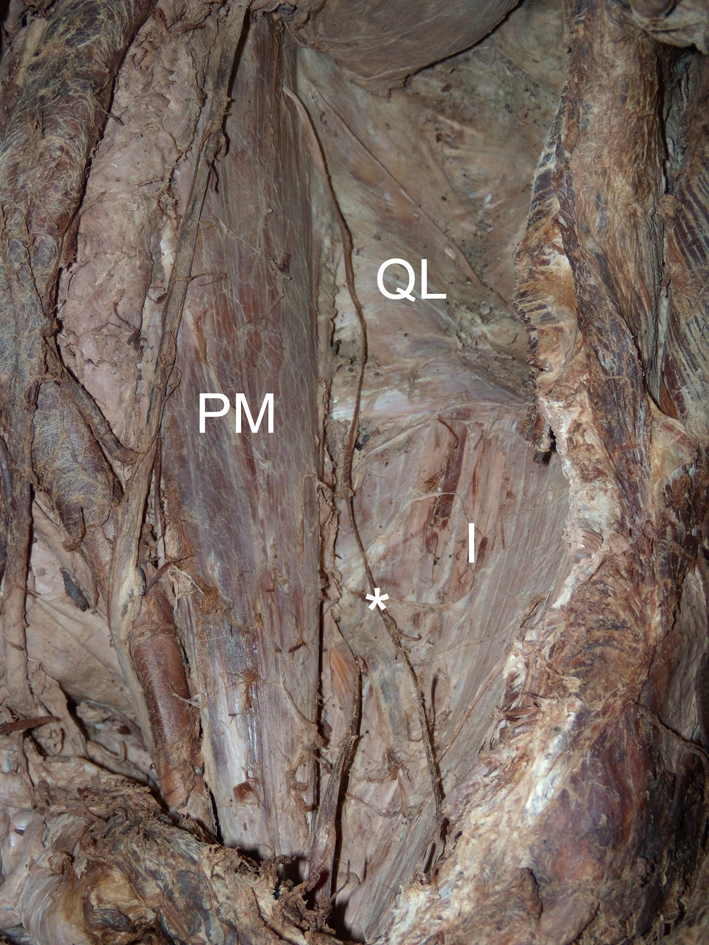
An example of the LFNC emerging above the IC (left side) is shown. In this case, the LFCN emerges through the PM instead of behind the muscle. * = LFNC; QL = quadratus lumborum muscle; PM = psoas major muscle; I = iliacus muscle.
Fig. 4.

An example of the LFNC emerging at the same level with the IC (right side) is shown. * = LFNC; QL = quadratus lumborum muscle; PM = psoas major muscle; I = iliacus muscle.
Fig. 5.

An example of the LFNC emerging below the IC (left side) is shown. * = LFNC; QL = quadratus lumborum muscle; PM = psoas major muscle; I = iliacus muscle.
The mean ± SD distances were −0.98 ± 5.57 cm between the LFCN emergence point and the IC, 12.39 ± 2.67 cm between the LFCN emergence point and the ASIS, and 17.76 ± 3.33 cm between the LFCN emergence point and the PT (Table 1). In the cases where the LFCN emerged above the IC (n = 12), the mean distance between the LFCN emergence point and the IC was 4.34 ± 2.77 cm and, in the cases below (n = 19), 5.02 ± 5.72 cm. For the cadavers in which both sides could be measured, no difference was found between sides for any of the intraabdominal measurements (p = 0.31 for a; p = 0.42 for b; and p = 0.09 for c) (Table 3).
Table 3.
Comparison of intraabdominal measurements between sides
| Parameter | a (right) | a (left) | b (right) | b (left) | c (right) | c (left) |
|---|---|---|---|---|---|---|
| Number | 19 | 19 | 19 | 19 | 19 | 19 |
| Mean (cm) | −1.60 | 1.05 | 12.39 | 12.84 | 17.14 | 18.24 |
| SD (cm) | 7.98 | 4.02 | 2.49 | 3.11 | 3.03 | 3.91 |
| Minimum (cm) | −24.00 | −5.80 | 8.00 | 8.50 | 14.00 | 10.30 |
| Maximum (cm) | 13.82 | 9.00 | 18.00 | 19.60 | 24.00 | 24.80 |
| Range (cm) | 37.82 | 14.80 | 9.00 | 11.10 | 10.00 | 14.50 |
| Median (cm) | 0.00 | 0.00 | 11.92 | 12.92 | 16.30 | 18.00 |
| z Value* | −1.02 | 0.81 | −1.72 | |||
| p Value | 0.31 | 0.42 | 0.09 | |||
Intraabdominal measurements were taken between the point where the lateral femoral cutaneous nerve leaves the lateral border of the psoas major and the visible medial end (back margin) of the iliac crest (a), the anterior superior iliac spine (b), and the pubic tubercle (c) (Fig. 1); *Wilcoxon signed-rank test.
All LFCNs in our specimens passed medial to the ASIS and behind the IL (neither through a slit on the IL nor through the iliac bone) as a single trunk. The mean AC was 2.95 ± 2.01 cm (3.09 ± 2.32 cm for the left sides, 2.71 ± 1.73 cm for the right sides). The mean AB was 13.11 ± 1.08 cm (12.98 ± 1.04 cm for the left sides, 13.23 ± 1.13 cm for the right sides). The mean AC/AB was 0.22 ± 0.16 (0.24 ± 0.20 for the left sides, 0.20 ± 0.12 for the right sides). For the cadavers in which both sides could be measured, no difference was found between sides for any of the inguinal measurements (p = 0.61 for AC and p = 0.49 for AC/AB) (Table 4).
Table 4.
Comparison of inguinal measurements between sides
| Parameter | AC (right) | AC (left) | AC/AB (right) | AC/AB (left) |
|---|---|---|---|---|
| Number | 17 | 17 | 17 | 17 |
| Mean | 2.93 cm | 3.19 cm | 0.22 | 0.24 |
| SD | 1.79 cm | 2.54 cm | 0.13 | 0.21 |
| Minimum | 0.70 cm | 0.60 cm | 0.06 | 0.05 |
| Maximum | 6.30 cm | 9.20 cm | 0.47 | 0.77 |
| Range | 5.60 cm | 8.60 cm | 0.41 | 0.72 |
| Median | 2.70 cm | 2.30 cm | 0.17 | 0.16 |
| z Value* | −0.52 | −0.69 | ||
| p Value | 0.61 | 0.49 | ||
Inguinal measurements were the length of the inguinal ligament (AB) and the distance between the anterior superior iliac spine and the point where lateral femoral cutaneous nerve crosses the inguinal ligament (AC) (Fig. 2); by using these two measurements, the AC/AB ratio was calculated; *Wilcoxon signed-rank test.
We found most (84%) of the LFCNs were 5 cm or less from the ASIS (Table 5). In one side (Table 2, cadaver 8 of Istanbul University series), the AC distance was 9.2 cm. In 89% of the 42 sides, the AC/AB ratio was less than 0.40 (Table 6).
Table 5.
ASIS-LFCN distances, numbers, and percentages
| ASIS-LFCN distances | Number |
|---|---|
| 0–10 mm | 7 (17%) |
| > 10–20 mm | 11 (26%) |
| > 20–30 mm | 8 (19%) |
| > 30–40 mm | 7 (17%) |
| > 40–50 mm | 2 (5%) |
| > 50–60 mm | 3 (7%) |
| > 60–70 mm | 3 (7%) |
| > 90–100 mm | 1 (2%) |
| Total | 42 (100%) |
ASIS = anterior superior iliac spine; LFCN = lateral femoral cutaneous nerve.
Table 6.
AC/AB ratios, numbers, and percentages
| AC/AB ratio | Number |
|---|---|
| 0–0.09 | 9 (21%) |
| 0.10–0.19 | 12 (29%) |
| 0.20–0.29 | 12 (29%) |
| 0.30–0.39 | 4 (10%) |
| 0.40–0.49 | 3 (7%) |
| 0.60–0.69 | 1 (2%) |
| 0.70–0.79 | 1 (2%) |
| Total | 42 (100%) |
AB = length of the inguinal ligament; AC = distance between the anterior superior iliac spine and the point where the lateral femoral cutaneous nerve crosses the inguinal ligament.
Discussion
During the relevant surgical procedures, the surgeon usually assumes the location of the LFCN by using the ASIS as a landmark. In this study, we investigated the exact location of the emergence point of the LFCN relative to IC, ASIS, PT, and the relative position of the nerve behind the IL.
There are two limitations to this study. One is the insufficient number of cadavers; this small number was increased by some missing nerves attributable to accidental trauma during the educational dissections. In addition, this limitation further prohibited us from calculating the differences between genders, and we could calculate only the differences between sides. The other limitation is that only embalmed cadavers were used in the study. The standard embalming procedures could change tissue properties, and measurements from the cadavers might not fully correlate with measurements from living subjects.
In some anatomy texts, the LFCN is described as “emerging from the lateral side of the PM, just above the IC” [1, 11]. During our dissections, we observed the situation was actually different. Little information is available regarding the exact level of this emergence relative to the IC. In our series, the emergence point of LFCN was above the IC in 12 (27%) sides. In such cases where the LFCN travels unexpectedly high in the retroperitoneum, the nerve can be injured during operations such as laparoscopic cholecystectomy [18]. The mean distance between the LFCN and the IC (including above and below cases) was −0.98 ± 5.57 cm in this study. In the literature, we found only one study [17] in which the distance between the LFCN and the IC was measured. In their study, Tubbs et al. [17] found all LFCNs left the lateral border of the PM below the IC and the mean distance was 5 ± 1.2 cm (range, 4–7 cm). In our series, the mean value of below cases (n = 19) was 5.02 ± 5.72 cm, indicating our findings are parallel to those of Tubbs et al. [17]. We could not find any published study regarding the distances between the LFCN emergence point and the ASIS and the PT. In our study, the mean distances were 12.39 ± 2.67 cm and 17.76 ± 3.33 cm, respectively. We believe these distances may be helpful for laparoscopic and open procedures of the abdomen.
Owing to the relatively high incidence (range, 6.7%–35%) [16] of meralgia paresthetica, the inguinal anatomy of the LFCN has been the subject of numerous studies [1–6, 8, 9, 13–16]. In most of the studies, researchers measured the distance between the ASIS and LFCN to define safe zones for operations in this region [5, 6, 8, 9, 13, 15, 16]. In our study, the mean ASIS-LFCN distance was 2.95 ± 2.01 cm (range, 0.6–9.3 cm) (3.09 ± 2.32 cm for the left sides, 2.71 ± 1.73 cm for the right sides), and we did not find any LFCNs passing lateral to the ASIS. This finding is consistent with some previous studies [5, 6, 9, 15–17] (Table 7). However, other studies [1, 4, 13, 14] have reported the LFCN passing lateral to the ASIS in different percentages (range, 2.9%–13%). Carai et al. [3] reported the LFCN passed through a canal in the iliac bone in 4.4% of their cases. In our study, the ASIS-LFCN distance was 4 cm or less in 79% of the cases, whereas Mischkowski et al. [13] reported 94.2%.
Table 7.
Comparison of the ASIS-LFCN distance between studies
| Study | ASIS-LFCN distance (cm) | ||
|---|---|---|---|
| Mean | SD | Range | |
| Dias Filho et al. [5] (2003) | 0.7 | 1 | 0–4 |
| Doklamyai et al. [6] (2008) | 1.6 | 0.3 | 0–6.2 |
| Grothaus et al. [8] (2005) | 3.6 | 2 | 0.6–7.3 |
| Hospodar et al. [9] (1999) | 2.04 | NA | 0.3–4.6 |
| Mischkowski et al. [13] (2006) | 1.46 | NA | NA |
| Ropars et al. [15] (2009) | 2.11 | NA | 0.5–5.6 |
| Sürücü et al. [16] (1997) | 1.52 | 0.84 | 0–3.21 |
| Tubbs et al. [17] (2005) | 1.5 | 0.8 | 0.5–3.5 |
| Current study (total) | 2.95 | 2.01 | 0.6–9.2 |
| Current study (left sides) | 3.09 | 2.32 | 0.6–9.2 |
| Current study (right sides) | 2.71 | 1.73 | 0.6–6.3 |
ASIS = anterior superior iliac spine; LFCN = lateral femoral cutaneous nerve; NA = not available.
There have been attempts to define different landmarks to localize the position of the LFCN behind the IL [6]. We believe ratios, not distances, should be considered. People have different body types and dimensions. Measuring the ASIS-LFCN distance does not take into account the relative position of the LFCN behind the IL. We calculated the AC/AB ratio to determine whether this ratio can define a certain relationship between the LFCN and the ASIS. Our mean AC/AB ratio was 0.22 ± 0.16 (0.24 ± 0.20 for the left sides, and 0.20 ± 0.12 for the right sides), and the AC/AB ratio for most (89%) of the LFCNs was less than 0.40. Our results suggest this ratio could be helpful in defining the position of the LFCN behind the IL.
Our findings indicate the LFCN may emerge from the lateral border of the PM not only below the IC but also above it in 27% of the cases. However, in 89% of the cases, the LFCN was found behind the lateral 40% of the IL. We suggest this finding may be helpful to surgeons in localizing the LFCN behind the IL in different patients whose bodies and body measurements may be different. We believe our results enrich the anatomic knowledge of the exact location of the LFCN relative to some bony landmarks and the IL. These findings may have potential relevance to everyday clinical surgical practice.
Acknowledgments
We thank Penbe Cagatay and Sevim Purisa for help with statistical work.
Footnotes
One or more of the authors (MÜ) have received funding from Scientific Research Projects Coordination Unit of Istanbul University (Project Number UDP-4021).
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Istanbul University and University of Cologne.
References
- 1.Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100:600–604. doi: 10.1097/00006534-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Atamaz F, Hepgüler S, Karasu Z, Kilic M. Meralgia paresthetica after liver transplantation: a case report. Transplant Proc. 2005;37:4424–4425. doi: 10.1016/j.transproceed.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 3.Carai A, Fenu G, Sechi E, Crotti FM, Montella A. Anatomical variability of the lateral femoral cutaneous nerve: findings from a surgical series. Clin Anat. 2009;22:365–370. doi: 10.1002/ca.20766. [DOI] [PubMed] [Google Scholar]
- 4.Ridder VA, Lange S, Popta JV. Anatomical variations of the lateral femoral cutaneous nerve and the consequences for surgery. J Orthop Trauma. 1999;13:207–211. doi: 10.1097/00005131-199903000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Dias Filho LC, Valença MM, Guimaraes Filho FA, Medeiros RC, Silva RA, Morais MG, Valente FP, França SM. Lateral femoral cutaneous neuralgia: an anatomical insight. Clin Anat. 2003;16:309–316. doi: 10.1002/ca.10106. [DOI] [PubMed] [Google Scholar]
- 6.Doklamyai P, Agthong S, Chentanez V, Huanmanop T, Amarase C, Surunchupakorn P, Yotnuengnit P. Anatomy of the lateral femoral cutaneous nerve related to inguinal ligament, adjacent bony landmarks, and femoral artery. Clin Anat. 2008;21:769–774. doi: 10.1002/ca.20716. [DOI] [PubMed] [Google Scholar]
- 7.Ducic I, Dellon AL, Taylor NS. Decompression of the lateral femoral cutaneous nerve in the treatment of meralgia paresthetica. J Reconstr Microsurg. 2006;22:113–118. doi: 10.1055/s-2006-932505. [DOI] [PubMed] [Google Scholar]
- 8.Grothaus MC, Holt M, Mekhail AO, Ebraheim NA, Yeasting RA. Lateral femoral cutaneous nerve: an anatomic study. Clin Orthop Relat Res. 2005;437:164–168. doi: 10.1097/01.blo.0000164526.08610.97. [DOI] [PubMed] [Google Scholar]
- 9.Hospodar PP, Ashman ES, Traub JA. Anatomic study of the lateral femoral cutaneous nerve with respect to the ilioinguinal surgical dissection. J Orthop Trauma. 1999;13:17–19. doi: 10.1097/00005131-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kavanagh D, Connolly S, Fleming F, Hill AD, McDermott EW, O’Higgens NJ. Meralgia paraesthetica following open appendicectomy. Ir Med J. 2005;98:183–185. [PubMed] [Google Scholar]
- 11.Keegan JJ, Holyoke EA. Meralgia paresthetica: an anatomical and surgical study. J Neurosurg. 1962;19:341–345. doi: 10.3171/jns.1962.19.4.0341. [DOI] [PubMed] [Google Scholar]
- 12.Mahadevan V. Pelvic girdle and lower limb. In: Standring S, ed. Gray’s Anatomy: The Anatomical Basis of Clinic Practice. 40th ed. Edinburgh, UK: Churchill Livingstone Elsevier; 2009:1382.
- 13.Mischkowski RA, Selbach I, Neugebauer J, Koebke J, Zöller JE. Lateral femoral cutaneous nerve and iliac crest bone grafts: anatomical and clinical considerations. Int J Oral Maxillofac Surg. 2006;35:366–372. doi: 10.1016/j.ijom.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000;82:746–747. doi: 10.2106/00004623-200005000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Ropars M, Morandi X, Huten D, Thomazeau H, Berton E, Darnault P. Anatomical study of the lateral femoral cutaneous nerve with special reference to minimally invasive anterior approach for total hip replacement. Surg Radiol Anat. 2009;31:199–204. doi: 10.1007/s00276-008-0433-3. [DOI] [PubMed] [Google Scholar]
- 16.Sürücü HS, Tanyeli E, Sargon MF, Karahan ST. An anatomic study of the lateral femoral cutaneous nerve. Surg Radiol Anat. 1997;19:307–310. doi: 10.1007/BF01637599. [DOI] [PubMed] [Google Scholar]
- 17.Tubbs RS, Salter EG, Wellons JC, 3rd, Blount JP, Oakes J. Anatomical landmarks for the lumbar plexus on the posterior abdominal wall. J Neurosurg Spine. 2005;2:335–338. doi: 10.3171/spi.2005.2.3.0335. [DOI] [PubMed] [Google Scholar]
- 18.Yamout B, Tayyim A, Farhat W. Meralgia paresthetica as a complication of laparoscopic cholecystectomy. Clin Neurol Neurosurg. 1994;96:143–144. doi: 10.1016/0303-8467(94)90048-5. [DOI] [PubMed] [Google Scholar]