Abstract
Background
Reverse total shoulder arthroplasty (RTSA) implants have been developed to treat patients with deficient rotator cuffs. The nature of this procedure’s complications and how these complications should be managed continues to evolve. Fractures of the scapula after RTSA have been described, but the incidence and best methods of treatment are unclear.
Questions/purposes
We therefore (1) determined the incidence and (2) developed a classification system intended to suggest the best choice of treatment.
Patients and Methods
We reviewed the records of 400 patients treated with RTSA over 4.5 years and identified all patients with scapula fractures. We identified three discrete patterns: avulsion fractures of the anterior acromion (Type I); fractures of the acromion posterior to the acromioclavicular joint (Type II); and fractures of the scapular spine (Type III).
Results
Twenty-two patients (5.5%) had fractures. Eight (2.0%) had Type I fractures on the first followup radiographs; these patients were treated nonoperatively with resolution of symptoms. Ten (2.5%) had Type II fractures a mean of 10.8 months after RTSA; seven of the 10 were treated surgically with improvement in their clinical symptoms. Four (1%) had Type III fractures at a mean of 10.3 months; all four fractures were treated with surgical fixation with healing.
Conclusions
Scapula fracture is a relatively common complication of RTSA. Our observations suggest Type I fractures can be observed with a likelihood of symptom relief. For Type II fractures, we recommend acromioclavicular joint resection if stable but open reduction internal fixation if unstable. We believe Type III fractures are best treated with open reduction internal fixation.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The modern reverse total shoulder arthroplasty (RTSA) implant is based on a concept introduced by Grammont and Baulot [3]. The reverse total shoulder is used for patients whose shoulder problems challenge the limitations of conventional total shoulder arthroplasty, including those with cuff tear arthropathy, failed or unstable total shoulder arthroplasties, and failed prosthetic reconstruction of proximal humerus fractures. However, complications with RTSA are common and potentially more serious than those encountered with conventional total shoulder arthroplasty [4]. A recent literature review involving 261 RTSAs with an average duration of followup of 3.1 years found most common complications, in descending order of frequency, were scapular notching, postoperative hematoma, glenosphere dissociation such as baseplate failure or aseptic loosening, glenohumeral dislocation, acromial or scapular fracture, infection, loosening or dissociation of the humeral component, and nerve injury [1].
Although RTSA provides surgeons with an innovative option for treating challenging shoulder disorders, the nature and treatment of the complications continue to evolve. Complications such as scapular notching, glenosphere fixation failure, and joint instability are well described. However, scapula fracture, although a known complication of RTSA, has been rarely reported [2, 9]. One author reported on 60 patients treated with RTSA for deficient rotator cuffs and osteoarthritis [2]. Three scapula fractures in two patients were identified at an average duration of followup of 33 months with an incidence of 5%. One patient with two scapula fractures was treated nonoperatively; one patient had an acromial fracture that was treated surgically. Both of these patients improved. Another investigator published the results of 58 patients treated with RTSA [9]. Four scapula fractures were reported at an average followup of 38 months for an incidence of 6.9%. Two of these fractures were treated operatively and two were treated nonoperatively. None of the fractures led to revision of the implant.
The purposes of our study were to (1) identify the incidence scapula fracture after RTSA; (2) classify these fractures; and (3) describe the likelihood of healing and symptom relief.
Patients and Methods
We retrospectively reviewed the medical records and followup radiographs of all 400 RTSAs performed for rotator cuff tear arthropathy, failed hemiarthroplasty, or failed total shoulder arthroplasty with rotator cuff tear from April 2004 to December 2008. All patients who sustained scapula fractures were included in the study. Contraindications to the procedure were poor deltoid function, active infection, or poor or deficient bone. Patients with Type I fractures were followed for a mean of 40 months, Type II fractures occurred a mean of 10.8 months after arthroplasty and followed posttreatment for a mean of 9.6 months, and Type III fractures occurred a mean of 10.3 months after arthroplasty and followed for a mean of 12.5 months after treatment. No patients with a scapula fracture were lost to followup.
All surgery was performed by one surgeon through a deltopectoral approach and using a DePuy Delta III (Warsaw, IN) in 210 of the cases or Equinoxe (Exactech, Gainesville, FL) implants in 190 cases.
Radiographs were available in all patients at the first postoperative visit (1 week). One of us (AH) independently reviewed all radiographs to retrospectively identify small fractures or avulsions of the acromion. Suspected acromion fractures were then compared with the preoperative radiographs to exclude abnormalities that preceded the surgical procedure.
Patients with clinically apparent acromion or scapular spine fractures that occurred during the followup period were treated with activity modification and observation, open reduction internal fixation, and/or acromioclavicular (AC) joint resection. Analysis of the scapula fractures showed discrete patterns, and a classification scheme was devised to characterize these patterns. All fractures were identified on either postoperative radiographs or CT. Small fractures of the anterior acromion near to or including the footprint of the coracoacromial ligament were classified as Type I fractures. Fractures through the anterior acromion just posterior to the AC joint were classified as Type II fractures. Fractures of the posterior acromion or scapular spine were classified as Type III fractures.
Results
Patients undergoing shoulder arthroplasty were followed at 1 week, 6 weeks, 3 months, 1 year, 2 years, and 5 years. Radiographs (true AP and axillary views) were obtained at 1 week, 3 months, 1 year, 2 years, and 5 years. Patients would come in before a scheduled followup whenever they were experiencing an increase in symptoms such as pain. Type II fractures were seen on average at 10.8 months postarthroplasty with an increase in pain and Type III fractures this occurred at a mean of 10.3 months.
Type I Fractures
Sixteen patients had abnormalities of the anterior acromion on the initial PO radiographs. Comparison to preoperative radiographs suggested three of the abnormalities were not fractures that occurred during the RTSA but were the result of degenerative changes to the acromion that existed before surgery. Five of these irregularities represented previously undiagnosed os acromiale. Eight patients had apparent avulsions occurring at the time of surgery and were classified as Type I fractures (Fig. 1). All eight of the patients with iatrogenic Type I acromion avulsion fractures after RTSA were right-handed; five of these acromion avulsion fractures occurred on right shoulders and three on left shoulders. The mean age was 72.9 years; six patients were female and two were male; the incidence was eight in 400 shoulders (2%). Six of these eight RTSAs were performed for the treatment of rotator cuff tear arthropathy; two had documentation or previous rotator cuff repair, and two had concomitant rheumatoid arthritis. One RTSA was a revision of a failed hemiarthroplasty for the treatment of a proximal humerus fracture, and one was a revision of a failed hemiarthroplasty for the treatment of rotator cuff tear arthropathy.
Fig. 1.
The radiograph shows a Type I scapula fracture.
Initial treatment of patients consisted of supportive care only. However, one patient had greater than expected pain in the AC joint at the first followup appointment. This pain was treated to the patient’s satisfaction with two separate steroid injections into this joint. One shoulder was revised for failure of the glenoid component, whereas one was revised for instability of the joint with osteolysis. Acromion avulsion was not cited as a reason for subsequent interventions in any of these shoulders, and none of the patients reported persistent pain at this location at a minimum followup of 27 months (mean, 40 months; range, 27–54 months).
Type II Fractures
Ten patients who developed pain in the anterior acromion after RTSA had a scapula fracture, identified as Type II, through the acromion just posterior to the AC joint. Nine of these patients were right-handed and one left-handed; seven of these fractures occurred on the side of the patient’s dominant arm, whereas three occurred on the nondominant side. The mean age was 70.4 years; the male to female ratio was 3:7; the incidence was 10 in 400 shoulders (2.5%). Seven of the RTSAs were performed for the treatment of rotator cuff arthropathy, two had documentation of a failed rotator cuff repair, and one had rheumatoid arthritis with rotator cuff deficiency. The remaining three RTSAs were revisions of failed hemishoulder arthroplasties performed for the treatment of proximal humerus fractures. The mean time from RTSA to diagnosis of Type II scapula fracture was 10.8 months (range, 3–33 months).
All 10 patients initially presented for evaluation with point tenderness over the anterior acromion and AC joint. Initial radiographic evaluation was not diagnostic in nine of the 10 patients except to confirm the presence of AC joint arthrosis. One of the 10 patients presented with a displaced fracture of the acromion, whereas three patients had suspected acromial stress fractures that eventually displaced and were clearly demonstrable on plain radiographs. Technetium bone scan ordered for two patients did not diagnose an acromial stress fracture in either case. CT was helpful in establishing the extent of AC joint arthrosis and diagnosing acromial stress fractures (Fig. 2).
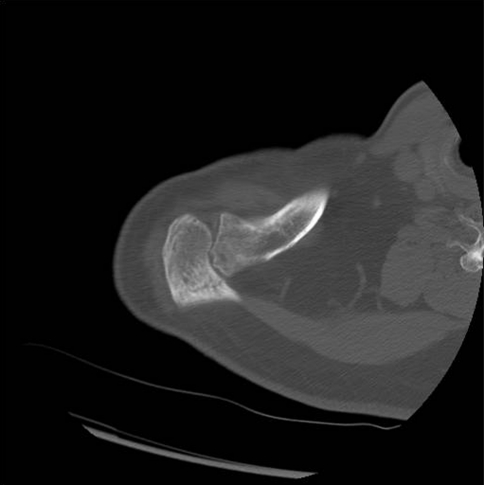
Fig. 2.
The CT scan reveals a Type II acromial stress fracture.
Three of the 10 patients were treated with open reduction internal fixation of their acromial fractures; all three patients had no pain at the fracture site at their most recent followup visit. Three patients were treated with AC joint resection alone because the acromial fractures appeared stable during surgery. One patient was treated with open reduction internal fixation and AC joint resection of his acromial fracture and had stable hardware with no pain at followup. Three patients were observed rather than treated as a result of either low physiological demand or poor health. Two of these patients continued to have persistent pain at the fracture site treated with medication or activity modification. The minimum followup of patients with Type II fractures was 3 months (mean, 9.6 months; range, 3–21 months).
Type III Fractures
Four patients developed pain in the posterior acromion or scapular spine after RTSA and were classified as having Type III scapula fractures. Three of these patients were right-handed and one was left-handed; all four of these fractures occurred on the patient’s nondominant arm. The mean age was 65.8 years; the male to female ratio was 1:3; the incidence was four in 400 shoulders (1.0%). All four RTSAs were performed for the treatment of rotator cuff tear arthropathy; two had documentation of previous failed rotator cuff repair. The mean time from RTSA to diagnosis of scapula fracture was 10.3 months (range, 2–16 months).
All four patients had a history of minor slips and the patient had to grab something to prevent falling, which precipitated the pain and tenderness in the posterior acromion or scapular spine that were ultimately diagnosed as scapula fractures. A displaced scapula fracture was identified on initial radiographs in all four of these cases (Fig. 3). All four patients were treated with open reduction internal fixation. One patient had failure of hardware fixation 2 months after surgery secondary to a fall and was revised; one patient required removal of hardware; all four patients had no pain at the fracture site at a minimum followup of 12 months (mean, 12.5 months; range, 12–13 months). Three-dimensional CT scan suggested these fractures might be the result of a stress riser from the tip of the superior metaglene fixation screw (Fig. 4). In the prosthesis used in this report, the DePuy design has four screw holes to place fixation screws for the metaglene and the Equinoxe design has six holes available. We recommend three or four screws be used to stabilize the metaglene. After obtaining three-dimensional CT scans, it became apparent that the superior screw was a potential stress riser and we recommend that this screw not be used if at all possible.
Fig. 3.
The radiograph shows a Type III scapula fracture.
Fig. 4.
The three-dimensional CT reconstruction displays a Type III fracture arising from the superior metaglene screw.
Discussion
The incidence and treatment of scapula fractures, occurring after RTSA, is not well defined in the literature [5–8]. Scapula fracture was not reported as a complication in four retrospective studies totaling 147 patients undergoing RTSA followed for an intermediate period (mean, 18–69 months) [5–8]. However, scapula fracture is a known complication of RTSA [1]. The purpose of this report is to describe the incidence of the complication in a large series (n = 400) of RTSAs. We have attempted to classify these fractures into a meaningful classification system that may assist surgeons in their treatment of this complication. The healing and symptomatic relief achieved in the patients treated has been included.
We acknowledge limitations of this retrospective study. First, this is a single-surgeon experience and may not represent the experience of all surgeons performing this procedure. Second, only two designs of RTSA implants were used in the patients reported on and may not represent all designs that are currently on the market for this procedure. Third, a prospective randomized study would need to be performed to validate the classification system and treatment recommendations. However this may not be practical as it would require a large number of fractures and require randomizing displaced fractures into nonoperative and operative treatment arms.
We found 22 fractures to the ipsilateral scapula among 400 RTSAs during followup for an incidence of 5.5%. This is similar to the previously reported incidences of 5.0% and 6.9% in two small series [2, 9]. The 22 fractures were classified into three distinct patterns (Types I-III) that may be helpful in directing treatment. The literature on scapula fractures does not generally make a distinction between iatrogenic acromion avulsions caused during RTSA surgery (Type I) and scapular fractures that occur later (Type II and III). We believe these fractures should be considered separate entities.
Type I scapula fractures after RTSA were all small avulsions of the anterior acromion that seemed to occur at the time of surgery, most likely the results of a weakened anterior acromion caused by wear or previous acromioplasty that displaced when deltoid retraction was applied. All were treated nonoperatively and did not have further intervention or patient complaints.
The Type II scapula fractures after RTSA occurred through the acromion just posterior to the AC joint. The pain produced by these fractures developed after the patients had regained their shoulder ROM and was not necessarily associated with a specific traumatic event. All patients with Type II fractures had varying severities of AC joint arthrosis. Arthrosis and stiffness of the AC joint may be an important etiology associated with the development of Type II scapula fractures in patients after RTSA. These fractures propagated from just posterior to the AC joint through the anterior acromion. Normal motion through the AC joint would likely dissipate stresses in this area, but we suggest stiff arthritic AC joints concentrate stresses onto the acromion resulting in a stress fracture over time as the patient regains glenohumeral motion. Resection of the AC joint may dissipate these stresses to allow Type II fractures to heal if stable; if unstable, open reduction internal fixation may be required. Nonoperative management of Type II fractures in patients who are poor surgical candidates should be considered with the knowledge that these fractures may likely displace (Fig. 5). All nondisplaced Type II fractures treated with observation eventually displaced with persistent but tolerable pain. Pain resolved in all surgically treated Type II fractures.
Fig. 5.

The radiograph demonstrates a displaced Type II scapula fracture.
The Type III scapula fractures after RTSA were all displaced fractures of the posterior acromion or scapular spine. All of these patients had a minor traumatic event that precipitated their fractures and were easily diagnosed with plain radiographs. Three of the four Type III fractures appeared to propagate from the tip of the most superiorly placed metaglene screws. These screws appear to act as stress risers. We no longer use the most superior screw hole for fixation of the metaglene. All patients with Type III fractures were treated with open reduction internal fixation with resolution of pain.
In conclusion, the incidence of scapula fractures occurring after RTSA is reported as 5.8%. Our observations suggest the Type I RTSA scapula fracture is a relatively benign complication that can be treated successfully with supportive care. Patients with pain in the anterior acromion after RTSA in which Type II fracture is suspected can best be evaluated with CT to rule out an acromial fracture. We believe AC joint resection should be considered for treating Type II fractures if the fracture appears stable and AC joint resection with open reduction internal fixation in Type II fractures that appear to be unstable. We recommend open reduction internal fixation for treating unstable Type III fractures. We no longer recommend placing the most superior screw for metaglene fixation because this appears to lead to a potential stress riser that may contribute to this fracture of the scapular spine.
Footnotes
One of the authors (LAC) has received royalties and consulting fees from Exactech (Gainesville, FL) for a product related to this study.
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Wright State University Boonshoft School of Medicine, Dayton, OH, USA, and the Medical College of Georgia, Augusta, GA, USA.
References
- 1.Bohsali K, Wirth M, Rockwood C. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 2.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1705–1967. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 3.Grammont P, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 4.Matsen FA, Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. Inst Course Lect. 2008;57:167–174. [PubMed] [Google Scholar]
- 5.Nwakama A, Cofield R, Kavvanagh B, Loehr J. Semiconstrained total shoulder arthroplasty for glenohumeral arthritis and massive rotator cuff tearing. J Shoulder Elbow Surg. 2000;9:302–307. doi: 10.1067/mse.2000.106467. [DOI] [PubMed] [Google Scholar]
- 6.Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg. 2001;10:17–22. doi: 10.1067/mse.2001.110515. [DOI] [PubMed] [Google Scholar]
- 7.Seebaur L, Walter W, Key W. Reverse total shoulder arthroplasty for the treatment of defect arthropathy. Oper Orthop Traumatol. 2005;17:1–24. doi: 10.1007/s00064-005-1119-1. [DOI] [PubMed] [Google Scholar]
- 8.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. J Bone Joint Surg Br. 2004;86:385–388. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 9.Werner C, Stienmann P, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]