Abstract
Background
In 1990, Hamada et al. radiographically classified massive rotator cuff tears into five grades. Walch et al. subsequently subdivided Grade 4 to reflect the presence/absence of subacromial arthritis and emphasize glenohumeral arthritis as a characteristic of Grade 4.
Questions/purposes
We therefore determined (1) whether patient characteristics and MRI findings differed between the grades at initial examination and final followup; (2) which factors affected progression to a higher grade; (3) whether the retear rate of repaired tendons differed among the grades; and (4) whether the radiographic grades at final followup differed from those at initial examination among patients treated operatively.
Patients and Methods
We retrospectively reviewed 75 patients with massive rotator cuff tears. Thirty-four patients were treated nonoperatively and 41 operatively.
Results
Patients with Grade 3, 4, or 5 tears had a higher incidence of fatty muscle degeneration of the subscapularis muscle than patients with Grade 1 or 2 tears. In 26 patients with Grade 1 or 2 tears at initial examination, duration of followup was longer in patients who remained at Grade 1 or 2 than in those who progressed to Grade 3, 4, or 5 at final followup. The retear rate of repaired supraspinatus tendon was more frequent in Grade 2 than Grade 1 tears. In operated cases, radiographic grades at final followup did not develop to Grades 3 to 5.
Conclusions
We believe cuff repair should be performed before acromiohumeral interval narrowing. Our observations are consistent with the temporal concepts of massive cuff tear pathomechanics proposed by Burkhart and Hansen et al.
Level of Evidence
Level III, Therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
In 1990, Hamada et al. proposed radiographic classification of massive rotator cuff tears [13]. A tear is defined as massive if it involved the detachment of two or more entire tendons [9] and typically at least the supraspinatus and infraspinatus tendon. The five-grade evolutional classification of Hamada et al. was developed by analyzing radiographic findings of massive rotator cuff tears, in which the grades were presumed to reflect the temporal evolution of rotator cuff tears. Briefly, the acromiohumeral interval (AHI) is maintained in Grade 1 and narrows in Grade 2. Acetabulization (concave deformity of the acromion undersurface) in addition to the Grade 2 narrowing is classified as Grade 3. In Grade 4, narrowing of the glenohumeral joint is added to the Grade 3 features, and Grade 5 comprises instances of humeral head collapse [13].
Subsequently, Walch et al. recognized a group with massive tears that demonstrated glenohumeral narrowing without acromial acetabulization. Thus, they divided Grade 4 of Hamada et al. into two subtypes: Grade 4A, glenohumeral arthritis without subacromial arthritis (acetabulization); and Grade 4B, glenohumeral arthritis with subacromial arthritis (Grade 4 of Hamada et al.). These subtypes allowed for more specific classification of patients [25], and almost all patients could be classified [21]. Furthermore, there appeared to be a correlation between the modified classification of Walch et al. and the Constant-Murley score [6] in 200 patients aged 70 to 101 years [21]. This modified classification has been used for selecting candidates for latissimus dorsi transfer [20].
The degree of fatty degeneration of the supraspinatus and infraspinatus muscles appears to be related to anatomic outcome (ie, retear of a repaired tendon), and the frequency of retears appears to increase with the degree of muscular degeneration of the infraspinatus [12]. Thus, for any categorical classification system intended to reflect severity or temporal progression to be valid, it must be consistent with other factors believed to be related to progression. Furthermore, it would clearly be helpful if retears of repaired tendons could be predicted from preoperative radiographs.
To confirm the temporal evolution of the modified classification, we therefore determined (1) whether patient characteristics and MRI findings differed between the grades at initial examination and at final followup; (2) which factors would affect the progression to a higher grade; (3) whether the retear rate of repaired tendons would be different among the grades; and (4) whether the radiographic grades at final followup would be different from those at initial examination among patients treated operatively.
Patients and Methods
We retrospectively reviewed the cases of 121 patients with massive rotator cuff tears (121 shoulders) involving at least the supraspinatus and infraspinatus tendons from 1980 to 1988 and from 2002 to 2009. Thirty patients declined to participate and 16 were lost to followup because of missing initial radiography data. This left 75 of the 121 patients (62%) for study (Table 1). Fifty-four patients had adequate records and followup and 21 were recalled specifically for this study; data were obtained from direct examination, medical records, MRI, and radiographs. Tendon tears were diagnosed by MRI if available or by ultrasonography (U/S) or arthrography. In patients diagnosed by MRI or U/S (n = 69) (Table 2), the incidence of concomitant subscapularis, teres minor tendon tears, and rupture of the long head of the biceps tendon was examined. In the 41 patients evaluated by T1-weighted images, the degree of fatty muscle degeneration of both the supraspinatus and infraspinatus muscles was evaluated.
Table 1.
Patient characteristics at initial examination (n = 75)
| Grade | Mean age (years) | Gender | Side | ||
|---|---|---|---|---|---|
| Male | Female | Dominant | Nondominant | ||
| Grade 1 | 63.4 | 27 | 16 | 31 | 12 |
| Grade 2 | 65.3 | 20 | 6 | 19 | 7 |
| Grades 3–5 | 81.1 | 3 | 3 | 5 | 1 |
| Grade 3 | 80.3 | 3 | 0 | 2 | 1 |
| Grade 4A, 4B | 83 | 0 | 1 | 1 | 0 |
| Grade 5 | 81.5 | 0 | 2 | 2 | 0 |
| Total | 65.8 | 50 | 25 | 55 | 20 |
Table 2.
Characteristics of torn tendons involving at least the supraspinatus (SSp) and infraspinatus (ISp) tendons (n = 69)
| Grade | Total number | Torn tendons | LHB rupture | ||
|---|---|---|---|---|---|
| SSp + Isp | Concomitant SSc | Concomitant TM | |||
| Grade 1 | 40 | 14 | 12 | 16 | 3 |
| Grade 2 | 23 | 9 | 3 | 13 | 2 |
| Grades 3–5 | 6 | 0 | 4 | 5 | 3 |
| Grade 3 | 3 | 0 | 3 | 2 | 2 |
| Grade 4A, 4B | 1 | 0 | 0 | 1 | 0 |
| Grade 5 | 2 | 0 | 1 | 2 | 1 |
| Total | 69 | 23 | 19 | 34 | 8 |
SSc = subscapularis; TM = teres minor; LHB = long head of the biceps tendon.
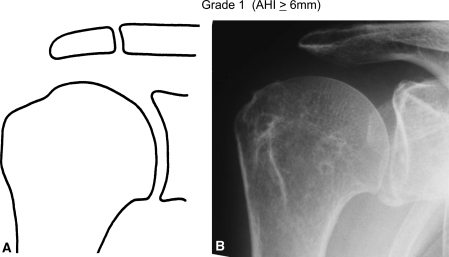
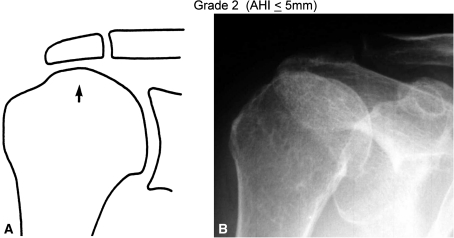
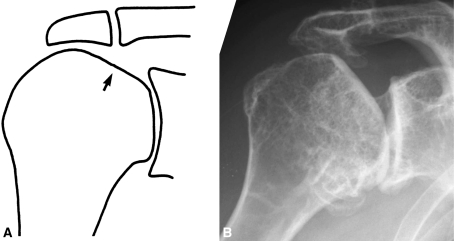
To grade the severity of disease, we used the classification of Hamada et al. as modified by Walch et al. (Table 1). In Grade 1, the AHI is ≥ 6 mm (Fig. 1A–B). In Grade 2, the AHI is ≤ 5 mm (Fig. 2A–B). Grade 3 adds “acetabulization” of the acromion (ie, subacromial arthritis) to the features of Grade 2. In this study, we define “acetabulization” as a concave deformity of the undersurface of the acromion always accompanied by recession of the greater tuberosity and sometimes accompanied by excessive spur formation along the coracoacromial ligament (Fig. 3A–B). Grade 4 shows glenohumeral narrowing (ie, glenohumeral arthritis). In Grade 4A, the AHI is < 7 mm and there is no acetabulization of the acromion (Fig. 4A–B) [24]. In contrast, Grade 4B shows acetabulization of the acromion; in other words, glenohumeral narrowing is seen in addition to Grade 3 features (Fig. 4C–D). Although this classification is based on AP radiographs, glenohumeral narrowing can also be seen on the axillary view. Grade 5 shows humeral head collapse, which is characteristic of cuff tear arthropathy, as initially described by Neer et al. [18] (Fig. 5A–B).
Fig. 1A–B.
Grade 1 cuff tear arthritis is shown (A) schematically and (B) as a plain roentgenogram.
Fig. 2A–B.
Grade 2 cuff tear arthritis is shown (A) schematically and (B) as a plain roentgenogram. The acromiohumeral interval is ≤ 5 mm (arrow).
Fig. 3A–B.
Grade 3 cuff tear arthritis is shown (A) schematically and (B) as a plain roentgenogram. The undersurface of the acromion shows concave deformity (acetabulization) (arrow).
Fig. 4A–D.
Grade 4A cuff tear arthritis is shown (A) schematically and (B) as a plain roentgenogram. The glenohumeral joint space is narrowed (arrow) but there is no acetabulization (C–D). Grade 4B with narrow glenohumeral joint space (arrow) and acetabulization (arrowhead) is shown. The plain roentgenogram (B) was kindly provided by Dr Gilles Walch.
Fig. 5A–B.
Grade 5 cuff tear arthritis (cuff tear arthropathy) is shown (A) schematically and (B) as a plain roentgenogram. Collapse of the humeral head is shown (arrow).
MRI was performed with a 1.5-T system (Signa Horizon LX; GE Healthcare, Milwaukee, WI) using a shoulder coil. Fat-suppressed T2-weighted fast spin-echo images and intermediate-weighted fast spin-echo images (4-mm slice thickness, 0.4-mm slice interval) were obtained in the coronal oblique and transverse planes. The criterion for a full-thickness rotator cuff tear was a fluid-filled gap in the tendon noted on the T2-weighted coronal oblique or transverse images [16]. T1-weighted fast spin-echo images (4-mm slice thickness, 0.4-mm slice interval) were obtained in the sagittal oblique plane parallel to the glenohumeral joint. T1-weighted images on MRI were obtained in 41 of 75 (54.7%) patients at the initial visit. The fatty muscle degeneration in each cuff component was evaluated according to the five-stage classification of Goutallier et al. [11]. Four investigators (KH, KY, TM, YU) reviewed the cases and diagnosed a complete-thickness tear when the tendon was not visible around the tuberosity. All U/S data were obtained in real time with a XarioTM SSA-660A scanner (Toshiba Medical Systems Corp, Otawara, Japan) and a variable high-frequency linear-array transducer PLT-1204AT (7–14 MHz). A full-thickness rotator cuff tear was diagnosed by two investigators (KY, KH) when the rotator cuff was ≤ 4 mm or could not be visualized because of complete avulsion and retraction under the acromion. The AP arthrograms were taken with the shoulder in 30° external rotation, neutral rotation, and 60° internal rotation. In all three positions, the continuous contours of the articular cartilage of the humeral head and the roof of the subacromial bursa without demonstrating the thickness of the cuff were identified [13]. Two investigators (KH, MM) reviewed all arthrograms and made the diagnosis of torn tendons. If the diagnosis differed between observers, a final diagnosis was determined by consensus. As reported previously, the positive predictive value (ratio of massive cuff tears in positive tests) was 0.98 by arthrogram using our original diagnostic method [14], and 0.88 [16] by U/S, and 0.95 by MRI [16]. Two investigators (KH, TM) independently evaluated all MRIs for diagnosing retear of the rotator cuff component [16] and subsequently established the MRI diagnosis by consensus. Sixty-three patients (37 Grade 1, 21 Grade 2, three Grade 3, two Grade 5) were diagnosed by MRI scans. One patient (Grade 1) was diagnosed by both MRI and U/S scans, and five patients (three Grade 1, one Grade 2, one Grade 4A) were diagnosed by U/S scans alone. Six patients (two Grade 1, four Grade 2) were diagnosed by arthrograms alone.
Of the 75 shoulders, 34 (34 patients) were treated nonoperatively by physiotherapy, nonsteroidal anti-inflammatory drugs, or steroid or hyaluronan injections into the subacromial bursa. The mean age of these patients at initial examination was 71.0 years (range, 50–84 years). Twenty-eight of these 34 patients (mean age at initial examination, 69.5 years; range, 50–84 years) were followed for ≥ 2 years (average, 5 years 2 months; range, 2 years to 9 years 11 months) (Table 3). Among the 26 patients with Grade 1 or 2 at initial examination, grading changes at final followup were examined. These patients were divided into two groups: those who remained at Grade 1 or 2 at final followup (n = 17; Group 17) and those progressed to Grade 3–5 at final followup (n = 9; Group 9) (Table 4). Differences in gender, operation on the dominant side, number of torn tendons, long head of biceps tear, active flexion after the acute phase and at final followup, and followup period were determined using the Mann-Whitney U test and all analyses were performed using StatView for Windows Version 5.0 (SAS Institute Inc, Cary, NC).
Table 3.
Progression of grade (n = 28)
| Grade at initial examination | Grade at final followup* | Total | ||||
|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | Grade 4A, 4B | Grade 5 | ||
| Grade 1 | 7 (39.1) | 5 (64.0) | 1 (94) | 2 (113.5) | 15 | |
| Grade 2 | 5 (45.4) | 6 (76.0) | 11 | |||
| Grade 3 | 1 (28) | 1 | ||||
| Grade 4A, 4B | 1 (96) | 1 | ||||
| Grade 5 | ||||||
| Total | 7 | 10 | 7 | 3 | 1 | 28 |
* Number (mean followup period in months).
Table 4.
Number of torn tendons and progression of Grades (G) 1 and 2
| Grade | Mean age (years) | Gender | Side | RC torn tendons | LHB tendon | Mean active flexion | Followup period (months) | |
|---|---|---|---|---|---|---|---|---|
| Male/female | D/non-D | SSp + ISp/more than SSp + ISp | Torn/not torn | After acute phase | At final followup | |||
| G 1 or 2 to G 2 (n = 17; Group 17) | 70.1 | 8/9 | 13/17 | 6/11 | 11/17 | 112.3 | 129.3 | 48.3 |
| G 1 or 2 to G 3, 4, or 5 (n = 9; Group 9) | 67.4 | 6/3 | 9/9 | 1/8 | 8/9 | 118.7 | 125.0 | 86.3 |
| p | 0.517 | 0.429 | 0.263 | 0.357 | 0.357 | 0.875 | 0.78 | 0.017 |
D = dominant side; non-D = nondominant side; RC = rotator cuff; SSp = supraspinatus; ISp = infraspinatus; LHB = long head of the biceps tendon (Mann-Whitney U test).
We treated 41 shoulders (41 patients) operatively: 26 with Grade 1 and 15 with Grade 2 tears. The indications for surgery were: (1) severe shoulder pain for > 2 months under nonoperative treatment; and (2) inability to elevate the arm above the horizontal for > 2 months under nonoperative treatment.. The contraindications for surgery were: (1) Grade 3, 4, or 5 of the Hamada et al. classification; (2) patient uncooperative with postoperative rehabilitation; and (3) contraindications for general anesthesia. The mean age of the patients who underwent surgery was 60.2 years (range, 50–75 years). The minimum followup of the operatively treated patients was 2 years (mean, 2 years 8 months; range, 2 years to 3 years 7 months). During surgery, the tendon stump was pulled distally up to the footprint with the shoulder at 20° elevation in neutral rotation after routine procedures including coracohumeral ligament release, interval slide, circumferential capsulotomy at the proximal edge, and anterior transfer of the teres minor tendon. If the tendon defect could not be closed after these procedures, it was left partially open [2] or closed with interposition of the long head of the biceps tendon or using muscle transfers, as described subsequently. Among the 41 patients treated surgically, primary closure could be performed for 20 of 26 with Grade 1 tears and eight of 15 with Grade 2 tears. Among the 26 patients with Grade 1 tears, primary cuff repair was possible in 20. The remaining six cuff tears were repaired according to the procedures described by Bush [3] (n = 3), Patte et al. [22] (n = 1), and Debeyre et al. [7] (n = 1) or treated with a pectoralis major transfer (n = 1) (Table 5). Among the 15 patients with Grade 2 tears, primary repair was possible in eight. The repair was partial in one patient to restore the force couples [2]. The remaining six cuff tears were repaired using the procedures of Patte et al. (n = 4) and Debeyre et al. (n = 1) or with a latissimus dorsi transfer (n = 1) (Table 5). After surgery, the operated shoulder was immobilized in an abduction splint or cast for 3 weeks. Passive ROM exercise was started 2 days after surgery, active ROM exercise at 6 weeks after surgery, and muscle strengthening exercises at 13 weeks after surgery. The rehabilitation was supervised by a therapist for 6 months and was unsupervised for another 6 months. At initial examination, at yearly followups, and at final followup, shoulder pain, ROM, muscle strength of abduction, and external rotation were evaluated, and three roentgenograms were obtained: the AP view with the shoulder at the side in neutral rotation, the scapular Y view, and the axillary view. Active flexion is believed to be one of the most important factors in activities of daily living [5, 17], and thus those recorded after the acute phase and at final followup were used as a surrogate for clinical function in patients treated nonoperatively. In patients with Grade 1 tears, five patients could not be followed after surgery, but the remaining 36 patients could be evaluated by MRI at 6 months and again at 2 years after surgery.
Table 5.
Surgical procedures
| Grade | Primary cuff repair | Tendon or muscle transfer | Partial repair | ||||
|---|---|---|---|---|---|---|---|
| Bush | Patte | Debeyre | LDT | Pec major T | |||
| Grade 1 | 20 | 3 | 1 | 1 | 0 | 1 | 0 |
| Grade 2 | 8 | 0 | 4 | 1 | 1 | 0 | 1 |
| Total | 28 | 3 | 5 | 2 | 1 | 1 | 1 |
Bush = Bush procedure; Patte = infraspinatus muscle transfer; Debeyre = supraspinatus muscle transfer; LTD = latissimus dorsi transfer; Pec major T = pectoralis major transfer.
We determined differences in patient characteristics (operation on dominant side, gender, age at initial visit), incidence of concomitant tendon tear, and degree of fatty muscle degeneration of rotator cuff components among Grade 1, Grade 2, and Grade 3–5 using multiple analysis of variance using SPSS II Version 17.0 (SPSS, Inc, Chicago, IL). Because Grades 3, 4, and 5 all display arthritic changes radiographically, they were grouped together as Grade 3–5. The mean age of the patients (50 males, 25 females) at initial examination was 65.8 years (range, 50–83 years). Differences in primary closure rates and retear rates between patients with Grade 1 or 2 tears who underwent surgery were evaluated using Fisher’s exact test. The missing data were dealt with as missing values in statistical analysis. The analyses were carried out using StatView for Windows Version 5.0 (SAS Institute Inc).
Results
Patients with Grade 3 to 5 massive cuff rotator tears were older than those with Grade 1 or 2 tears (p = 0.03 and 0.042, respectively) (Table 6). In patients diagnosed by MRI or U/S (n = 69) (Table 2), incidence of concomitant subscapularis or teres minor tendon tears was higher in Grade 3–5 tears than in Grade 1 tears (p = 0.006 and 0.05, respectively) (Table 7). Rupture of the long head of the biceps tendon was also more frequent in Grade 3–5 tears than in Grade 1 or 2 tears (p = 0.005 and 0.017, respectively) (Table 7). In the 41 patients evaluated by T1-weighted images, the degree of fatty muscle degeneration of both the supraspinatus and infraspinatus muscles was higher in Grade 3–5 tears than in Grade 1 (p = 0.005 and 0.015, respectively) and 2 (p = 0.003 and 0.010, respectively) tears. In particular, the degree of fatty muscle degeneration of the subscapularis muscle was higher in Grade 3–5 tears than in Grade 1 or 2 tears (p = 0.000051 or 0.0000668, respectively) (Table 8).
Table 6.
Patient characteristics at initial visit between grades (n = 75)
| Variants | Grade 1 | p | Grades 3–5 | p | Grade 2 | p | Grade 1 |
|---|---|---|---|---|---|---|---|
| Affected side (dominant/nondominant side) | 30/12 | 0.143 | 5/1 | 0.539 | 19/8 | 0.067 | 30/12 |
| Gender (male/female) | 26/16 | 0.712 | 5/1 | 0.821 | 20/7 | 0.295 | 26/16 |
| Age (years) | 64.1 | 0.03 | 81.2 | 0.042 | 65.3 | 0.810 | 64.1 |
Multiple analysis of variance.
Table 7.
Details of tendon tears at initial imaging by grade (n = 69)
| Concomitant tendon tears | Grade 1 (40) | p | Grade 3–5 (6) | p | Grade 2 (23) | p | Grade 1 (40) |
|---|---|---|---|---|---|---|---|
| SSc tendon | 12 | 0.006 | 4 | 0.056 | 3 | 0.184 | 12 |
| TM tendon | 16 | 0.047 | 5 | 0.228 | 13 | 0.205 | 16 |
| LHB | 3 | 0.005 | 3 | 0.017 | 2 | 0.889 | 3 |
SSc = subscapularis; TM = teres minor; LHB = long head of biceps (number of cases) (multiple analysis of variance).
Table 8.
Mean fatty muscle degeneration stage at initial MRI by grade (n = 41)
| Fatty muscle degeneration | Grade 1 (22) | p | Grade 3–5 (5) | p | Grade 2 (14) | p | Grade 1 (22) |
|---|---|---|---|---|---|---|---|
| SSp muscle (19) | 2.3 | 0.005 | 4.0 | 0.003 | 2.2 | 0.798 | 2.3 |
| ISp muscle (22) | 2.3 | 0.015 | 3.8 | 0.010 | 2.4 | 0.703 | 2.3 |
| TM muscle (8) | 1.0 | 0.166 | 1.8 | 0.846 | 1.6 | 0.133 | 1.0 |
| SSc muscle (7) | 0.9 | 0.000051 | 3.2 | 0.0000668 | 0.9 | 0.949 | 0.9 |
SSp = supraspinatus; ISp = infraspinatus; SSc = subscapularis; TM = teres minor (number of cases) (multiple analysis of variance).
Eight of 15 patients with Grade 1 tears who were treated nonoperatively and followed for ≥ 2 years and six of 11 patients with Grade 2 tears progressed to a higher grade in 69.5 and 76.0 months on average, respectively (Table 3). Of the 26 patients with Grade 1 or 2 tears at initial examination, 17 (Group 17) remained at Grade 1 or 2 and nine (Group 9) progressed to Grade 3–5 at final followup. The mean active flexion angles of Groups 17 and 9 did not differ between after the acute phase and at final followup and thus did not deteriorate (Table 4). Duration of followup was longer (p = 0.017) in Group 9 than in Group 17 (Table 4).
Among 21 of the 26 patients with Grade 1 treated surgically six (28.6%) had a supraspinatus tendon retear on followup and two (9.5%) an infraspinatus tendon retear. Of the 15 patients with Grade 2 tears treated surgically 10 (66.7%) had a supraspinatus tendon retear and three (20.0%) an infraspinatus tendon retear. The supraspinatus tendon retear rate was higher (p = 0.041) for Grade 2 than Grade 1, whereas the infraspinatus tendon retear rate was similar (p = 0.63) for these grades.
Among the 20 patients treated operatively (n = 10 each Grades 1 and 2), followup radiographic findings after > 2 years showed for Grade 1, seven remained unchanged and three progressed to Grade 2; for Grade 2, three remained unchanged and seven improved to Grade 1 with no patients progressing to Grade 3–5.
Discussion
To confirm the temporal evolution of the modified classification, we investigated (1) whether patient characteristics and MRI findings differed between the grades at initial examination and final followup; (2) which factors affected progression to a higher grade; (3) whether the retear rate of repaired tendons differed among the grades; and (4) whether the radiographic grades at final followup differed from those at initial examination among patients treated operatively.
Our study has several major limitations. First, the loss of 38% of our patients to followup may have compromised our analysis. Second, the followup period was short for observing radiographic degenerative changes that might take years to develop, and radiographs were not obtained regularly. Important radiographs were sometimes missing and therefore we could not follow the grade of development temporally. These limitations were mainly the result of the retrospective nature of the study and could be improved in a prospective study. Third, we considered only patients with Grade 1 or 2 tears as candidates for surgery, and surgical techniques sometimes varied. Nevertheless, the different procedures used to repair torn rotator cuffs were performed consistently by the same surgical team throughout this study. Fourth, degree of fatty muscle degeneration could not be evaluated as a result of the relatively small patient sample and grouping by classes made for smaller cells, which increase the risk of a Type II error. Nevertheless, we did find differences in key variables.
We found patients with Grade 3–5 tears at initial examination were on average older than those with Grade 1 or 2 tears, although the mean age of patients with Grade 3 tears was similar to that of patients with Grade 4 or 5 tears (statistical analysis could not be performed because of small patient numbers). However, Nové-Josserand et al. [21] reported that patients with tears classed as Grade 3 on (Walch et al.) were younger than patients of all other grades. This difference between their results and ours may result from the small number of patients in our study and the inclusion of patients without massive cuff tears in theirs. In the present study, ruptures of the long head of the biceps tendon were also more frequent in patients with Grade 3–5 tears than in patients with Grade 1 or 2 tears (Table 2). However, Walch et al. [25] reported that arthroscopic biceps tenotomy without rotator cuff repair did not influence the natural progressive changes seen radiographically. These results suggest that such ruptures may be the result of grade progression rather than a specific cause. The active flexion angles did not decrease even after grade progression in our study (Table 4), which could be the result of compensation, including a stable glenohumeral fulcrum [1] and increased reaction force at the glenohumeral joint in abduction [15]. As risk factors for the progression of the modified Hamada classification grade after biceps tenotomy of massive rotator cuff tears, Walch et al. [25] reported teres minor atrophy in patients with severe fatty infiltration of the infraspinatus muscle and fatty infiltration of the subscapularis. We found the incidence of concomitant subscapularis and teres minor tendon tears was higher in patients with Grade 3–5 tears than in those with Grade 1 or 2 tears (Table 2), and the degree of fatty muscle degeneration of the subscapularis muscle was higher for Grade 3–5 tears than in those with Grade 1 or 2 tears (Table 8). Together, these results suggest that the subscapularis could play an important role in progression to Grade 3, 4, or 5. We found that a longer followup period negatively influenced grade progression from Grade 1 or 2 to Grade 3–5, which is consistent with the results of Walch et al. [25].
The reparability of torn rotator cuffs can be evaluated by fatty infiltration on MRI [21, 27] or CT [12] or during surgery. Recently, Gerber et al. [9] reported that the preoperative duration of symptoms was shorter for patients with a retear. By contrast, Walch et al. [25] determined rotator cuff reparability largely from the presence of superior migration of the humeral head on radiographs and/or the presence of fatty infiltration of the rotator cuff musculature. Although various operative procedures were applied in our study, the supraspinatus tendon retear rate was more frequent in Grade 2 (66.7%) than Grade 1 (28.6%). Our observations support those of Walch et al. Although the followup periods were relatively short in the present study, the data suggest that open cuff repair could reduce the risk of grade progression and improve the preoperative radiographic grade, which is consistent with the findings of Nich et al. [19]. After glenohumeral arthritis (Grades 4 and 5) develops, arthrodesis [4, 10], hemiarthroplasty [23, 26], or total shoulder arthroplasty including reverse total shoulder arthroplasty [8] should be considered, because the situation is shifted to articular cartilage degeneration. Much work is still needed to fully elucidate the natural history of massive cuff tear arthritis as well as to refine the treatment indications at each stage of progression.
In summary, we classified 75 massive rotator cuff tears according to a revised radiographic classification. The age of patients with Grade 3–5 tears at initial examination was higher than that of patients with Grade 1 or 2 tears. The degree of fatty muscle degeneration of the subscapularis muscle was higher in Grade 3–5 than in Grade 1 or 2 tears. The duration of followup was the only factor that correlated with progression of Grade 1 or 2 to Grade 3–5. The retear rate of the supraspinatus tendon was more frequent in Grade 2 than Grade 1. Therefore, cuff repair should be performed before AHI narrowing. The results of our study are consistent with the concepts of massive cuff tear pathomechanics previously proposed by Burkhart [1], Hansen et al. [15], and von Eisenhart-Rothe et al. [24]. Nevertheless, isolated glenohumeral arthritis as described by Walch et al. [25] (Grade 4A) may be related to increased glenohumeral reaction forces without a total loss of “stable fulcrum kinematics.”
Acknowledgments
We thank Professor Pascal Boileau for encouraging us to write this article. We also thank Dr Gilles Walch for fruitful e-mail discussions and for allowing us to use his roentgenograms. We dedicate this work to the memory of Emeritus Professor Hiroaki Fukuda.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Shizuoka Red Cross Hospital, Hakone National Hospital, Yamanaka Orthopaedic Clinic, and Tokai University Hospital.
References
- 1.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears A suspension bridge model. Clin Orthop Relat Res. 1992;284:144–152. [PubMed] [Google Scholar]
- 2.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/S0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 3.Bush LF. The torn shoulder capsule. J Bone Joint Surg Am. 1975;57:256–259. [PubMed] [Google Scholar]
- 4.Clare DJ, Wirth MA, Groh GI, Rockwood CA., Jr Shoulder arthrodesis. J Bone Joint Surg Am. 2001;83:593–600. doi: 10.1302/0301-620X.83B4.10681. [DOI] [PubMed] [Google Scholar]
- 5.Codsi MJ, Hennigan S, Herzog R, Kella S, Kelley M, Leggin B, Williams GR, Iannotti JP. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Surgical technique. J Bone Joint. Surg Am. 2007;89(Suppl 2):1–9. doi: 10.2106/JBJS.F.01160. [DOI] [PubMed] [Google Scholar]
- 6.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 7.Debeyre J, Patte D, Elmelik E. Repair of ruptures of the rotator cuff of the shoulder. J Bone Joint Surg Br. 1965;47:36–42. [PubMed] [Google Scholar]
- 8.Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468:1526–1533. doi: 10.1007/s11999-009-1188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 10.González-Díaz R, Rodríguez-Merchán EC, Gilbert MS. The role of shoulder fusion in the era of arthroplasty. Int Orthop. 1997;21:204–209. doi: 10.1007/s002640050151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin M-C. Fatty muscle degeneration in cuff ruptures Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 12.Goutailler D, Postel JM, Lavau L, Bernageau J. Influence of supraspinatus and infraspinatus muscular fatty degeneration on the prognosis of rotator cuff surgical repair [in French] Rev Chir Orthop Reparatrice Appar Mot. 1999;85:668–676. [PubMed] [Google Scholar]
- 13.Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears A long-term observation. Clin Orthop Relat Res. 1990;254:92–96. [PubMed] [Google Scholar]
- 14.Hamada K, Fukuda H, Nakajima T, Mikasa M. Comparative studies of arthrographic and operative findings in rotator cuff tears [in Japanese] Katakannsetsu. 1991;15:141–147. [Google Scholar]
- 15.Hansen ML, Otis JC, Johnson JS, Cordasco FA, Craig EV, Warren RF. Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am. 2008;90:316–325. doi: 10.2106/JBJS.F.00880. [DOI] [PubMed] [Google Scholar]
- 16.Iannotti JP, Ciccone J, Buss DD, Visotsky JL, Mascha E, Cotman K, Rawool NM. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005;87:1305–1311. doi: 10.2106/JBJS.D.02100. [DOI] [PubMed] [Google Scholar]
- 17.Iannotti JP, Hennigan S, Herzog R, Kella S, Kelley M, Leggin B, Williams GR. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am. 2006;88:342–348. doi: 10.2106/JBJS.D.02996. [DOI] [PubMed] [Google Scholar]
- 18.Neer CS, 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65:1232–1244. [PubMed] [Google Scholar]
- 19.Nich C, Mutschler C, Vandenbussche E, Augereau B. Long-term clinical and MRI results of open repair of the supraspinatus tendon. Clin Orthop Relat Res. 2009;467:2613–2622. doi: 10.1007/s11999-009-0917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nové-Josserand L, Costa P, Liotard J-P, Safar J-F, Walch G, Zilber S. Results of latissimus dorsi tendon transfer for irreparable cuff tears. Orthop Traumatol Surg Res. 2009;95:108–113. doi: 10.1016/j.otsr.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Nové-Josserand L, Walch G, Adeleine P, Courpron P. Effect of age on the natural history of the shoulder: a clinical and radiologic study in the elderly [in French] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:508–514. doi: 10.1016/s0035-1040(05)84440-x. [DOI] [PubMed] [Google Scholar]
- 22.Patte D, Debeyre DP, Goutallier D. Rotator cuff repair by muscle advancement. In: Bayley I, Kessel L, editors. Shoulder Surgery. Berlin, Heidelberg, New York: Springer; 1982. pp. 49–50. [Google Scholar]
- 23.Petroff E, Mestdagh H, Maynou C, Delobelle JM. Arthroplasty with a mobile cup for shoulder arthrosis with irreparable rotator cuff rupture: preliminary results and cineradiographic study [in French] Rev Chir Orthop Reparatrice Appar Mot. 1999;85:245–256. [PubMed] [Google Scholar]
- 24.Eisenhart-Rothe R, Müller-Gerbl M, Wiedemann E, Englmeier KH, Graichen H. Functional malcentering of the humeral head and asymmetric long-term stress on the glenoid: potential reasons for glenoid loosening in total shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17:695–702. doi: 10.1016/j.jse.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 25.Walch G, Edwards B, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Yamane S, Suenaga N, Oizumi N, Yamaguchi H, Minami A. A shoulder hemiarthroplasty with a tendon muscle transfer for glenohumeral arthritis associated with severe rotator cuff deficiency [in Japanese] Katakansetsu. 2008;32:465–468. [Google Scholar]
- 27.Yoo JC, Ahn JH, Yang JH, Koh KH, Choi SH, Yoon YC. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2009;25:573–582. doi: 10.1016/j.arthro.2008.12.015. [DOI] [PubMed] [Google Scholar]