Abstract
INTRODUCTION:
Adiponectin is a circulating hormone that is produced exclusively by adipocytes and has anti-inflammatory and anti-atherogenic properties. The hypothesis that there are differences in adiponectin levels between stable and unstable coronary-artery disease patients remains controversial. Furthermore, the potential relationships between the plasma adiponectin level and the inflammatory and non-inflammatory markers (oxidized low density lipoprotein and nitric oxide) in patients with stable and unstable coronary-artery disease relative to normal subjects have not been assessed.
OBJECTIVES:
To assess whether plasma adiponectin levels differ among patients with stable and unstable coronary-artery disease and among control subjects, and to correlate plasma adiponectin level with inflammatory and clinical risk factors (such as oxidized-LDL and nitric oxide) in these patients.
METHODS:
This study included 50 control subjects, 50 stable angina patients and 50 unstable angina patients with angiographically documented coronary-artery disease. Plasma adiponectin and oxidized-LDL levels were determined using an enzyme immunoassay. Plasma nitric oxide, high sensitivity C-reactive protein and lipid profile levels were also measured.
RESULTS:
Plasma adiponectin levels were lower in the unstable angina patients (4.9±1.30 µg/mL) than in the stable angina patients (6.34±1.0 µg/mL) or in the controls (9.25±1.8 µg/mL); these levels were also significantly lower in stable angina patients versus controls (p<0.001). Plasma adiponectin levels were negatively correlated with oxidized-LDL, high sensitivity C-reactive protein, lipid profile and other clinical risk factors but positively correlated with nitric oxide.
CONCLUSION:
Plasma adiponectin levels were found to be lower in both stable and unstable angina patients relative to control subjects, and the correlation between plasma adiponectin and cardiovascular markers is weakened in these patients.
Keywords: Adiponectin, Nitric oxide, Ox-LDL, Stable, Unstable
INTRODUCTION
Adiponectin is a circulating hormone that is produced exclusively by adipocytes1 and has both anti-inflammatory and anti-atherogenic properties.2
Endothelial dysfunction due to reduced nitric oxide (NO) bioavailability is an essential early event in the development, propagation, and clinical expression of atherosclerosis and its complications.3
Oxidized-LDL (Ox-LDL) has a prominent role in the pathogenesis of atherosclerosis,4 and the elevation of ox-LDL levels in atherosclerotic plaques is an important event in the development of atherosclerosis.5 Moreover, elevated ox-LDL contributes to plaque instability and vulnerability.6
Adiponectin may protect the endothelium against the detrimental effects of ox-LDL.7 Low adiponectin levels are associated with high circulating ox-LDL in patients with type 2 diabetes mellitus and coronary artery disease.8
Adiponectin hampers proatherogenic events, such as nuclear factor κB signaling, foam cell formation, and vascular smooth cell migration.9,10 It also promotes NO production by endothelial cells11 and suppresses the proliferation of human aortic smooth muscle cells.12
Decreased levels of adiponectin act as an independent risk factor for coronary artery disease.13 In patients with stable chest pain, low adiponectin levels may contribute to coronary plaque vulnerability and may play a role in the pathophysiology of acute coronary syndrome.14 Also, low plasma adiponectin in patients with stable coronary artery disease is associated with the presence of thin-cap fibroatheroma, which is a criterion for plaque vulnerability.15 Previous studies have demonstrated that low adiponectin levels are an independent predictor of the extent of coronary artery disease and coronary lesion complexity, as determined by coronary angiography.16-18
Despite the aforementioned relationships between adiponectin levels and coronary artery disease, the existence of differences in adiponectin levels between stable and unstable coronary artery disease patients is controversial. In one study of 608 patients with stable angina and 378 patients with unstable angina, conducted by Stefan et al,19 no significant differences in adiponectin levels were observed between the two groups of patients. In contrast, another study found that the plasma levels of adiponectin were significantly lower in patients with unstable angina pectoris relative both to patients with stable angina pectoris and to the control group.20 In addition, in other acute settings (such as acute coronary syndrome and myocardial infarction), plasma adiponectin levels are lower relative to stable coronary artery disease patients.17,21
The relationships between plasma adiponectin levels and the inflammatory and non-inflammatory markers ox-LDL and NO in patients with stable and unstable coronary artery disease relative to normal subjects have not yet been assessed. Furthermore, the differences in adiponectin levels between stable and unstable coronary artery disease patients require further evaluation.
Therefore, in the present study, we sought to assess whether plasma adiponectin levels differ among patients with stable angina, unstable angina, and control subjects, and whether these differences correlate with inflammatory and clinical risk factors, such as ox-LDL and NO.
MATERIALS AND METHODS
Patients
Between 22 November 2009 and 22 May 2010, 150 patients receiving coronary angiograghy following chest pain, clinical manifestations or suspected changes on electrocardiography were selected for inclusion in this study at Isfahan Cardiovascular Research Center in Iran. These subjects included 50 stable angina patients, 50 unstable angina patients, and 50 control subjects. The patient's angiograms were assessed by two experienced cardiologists who were unaware of the disease status of each subject. The position and extent of stenosis for 15 main coronary segments were determined according to the method of Miller et al.22 Coronary artery disease was defined as ≥50% stenosis in at least one main coronary segment. In the majority of the normal subjects, coronary artery obstructions were less than 10%, but a minority of them (15 subjects) presented stenosis of less than 25% in at least one main coronary artery segment. In addition, the control subjects did not have any history or clinical symptoms of cardiovascular disease. Among the patients with significant stenosis, 80 patients (85%) had 50 to 75% stenosis in at least one main coronary artery segment, and 20 patients (20%) had 76 to 85% stenosis in one main coronary artery segment. Furthermore, 85 patients (85%) had single vessel stenosis, 10 patients (10%) had double vessel stenosis and 5 patients (5%) had triple vessel stenosis. All of the patients were evaluated both prospectively at enrollment and retrospectively by review of their clinical history. The unstable angina patients had random and unpredictable angina at rest or sleep along with transient ST-segment shifts and normal creatine kinase MB levels, whereas the stable angina patients had chest pain during physical exertion that was relieved by rest and presented a constant pattern or frequency of chest pain. Patients with myocardial infarction diagnosed on the basis of ST-segment elevation on their electrocardiogram and high levels of creatine kinase MB, lactate dehydrogenase and troponin T were not included in the study.
Information about conventional clinical risk factors, such as smoking, diabetes mellitus, family history of coronary artery disease, hypertension, medication and other necessary data, were obtained through a standardized questionnaire after admission.
Patients with a recent (within 6 months) myocardial infarction, cardiovascular event, surgery (within 3 months), cancer, infection or inflammatory disease were not included in the study. Any patient that underwent any other diagnostic or therapeutic treatment or who experienced a cardiovascular event that might have interfered with the study within one week after the angiography was excluded. Before enrollment, written informed consent was obtained from all of the subjects and approval of the study was provided by the Ethics Committee of Isfahan University Medical Sciences and Isfahan Cardiovascular Research Center (ICRC, a WHO collaborating center).
Biochemical measurements
One week after the angiography, a 12-hour fasting venous blood sample was collected from each patient into a Vacutainer EDTA-tube (BD Vacutainer®, Brocken Bow, NE USA), centrifuged and stored at -70°C until analyses were performed. Plasma adiponectin levels were determined with an enzyme-linked immunosorbent (ELISA) assay kit (Cat. EA-0201, Signosis, Inc.). Ox-LDL was measured with an ELISA kit (Immundiagnostik AG, Bensheim, Germany). Total nitric oxide (NO) was determined by spectrophotometry using a total NO assay kit (Assay designs, Inc., USA). Plasma levels of hsCRP were measured with a highly sensitive latex-enhanced immunoturbidometric assay (Randox laboratory Ltd, Belfast, United Kingdom). Plasma total lipoprotein profiles (total cholesterol, triglycerides, LDL-cholesterol, and HDL-cholesterol) were determined using enzymatic test kits (Pars Azmun Co., Karaj, Iran).
Statistical analysis
All of the statistical analyses were performed using SPSS statistical software version 16.0 (SPSS Inc., Chicago, IL, USA). The sample size was determined by a power analysis based on preliminary results that were obtained in our research center. With a type I error of <0.05 (2-tailed), power (1-β) of 0.80, an expected difference in adiponectin concentration between patients and normal subjects of about 1.4 µg/mL and a standard deviation of about 2.5 µg/mL, a minimum of 49 subjects in each group would be adequate to detect a difference in the plasma adiponectin concentration. Before the statistical analysis, the variables were examined for normal distribution and approved by the Shapiro-Wilk test. The comparison of means for continuous variables among the groups was performed using the unpaired Student's t-test or one-way analysis of variance (ANOVA) with post hoc comparison using the Bonferoni test, and the Chi-square test was applied to the dichotomous variables. Correlations between the plasma concentration of adiponectin and other normally distributed variables were assessed by Pearson's coefficient of correlation (r). Multiple logistic regression analysis was performed to determine the relationship between adiponectin levels and the presence of stable angina or unstable angina. The data are expressed either as mean ± standard deviation or as counts and percentages. A p-value <0.05 was considered to be statistically significant.
RESULTS
The clinical characteristics and biochemical data of the patients are summarized in Table 1. The control subjects were age- and gender-matched with the patients. Cardiovascular risk factors were observed predominantly in the patients. The control subjects were mostly not taking medications. The inflammatory markers hsCRP and ox-LDL were significantly higher in the angina patients relative to the control subjects, and they were higher in the unstable angina patients relative to the stable angina patients. The lipid profiles varied among the three groups, although these differences failed to reach significance, with the exception of LDL-cholesterol, which was significantly higher in the unstable angina patients than in the control subjects (p = 0.009).
Table 1.
Clinical characteristic of the study participants.
| Variable | Controls (n = 50) | Stable angina patients (n = 50) | Unstable angina patients (n = 50) | Controls vs. stable angina patients (p-value) | Controls vs. unstable angina patients (p-value) | Stable angina vs. unstable angina patients (p-value) |
| Age (year) | 58.9±10.3 | 61.2±11.23 | 59.9±10.45 | 0.510 | 0.576 | 0.587 |
| Men | 35 (70%) | 28 (56%) | 32 (64%) | 0.350 | 0.473 | 0.396 |
| BMI (kg/m2) | 26.9±0.6 | 27.8±1.5 | 26.89±1.3 | 0.387 | 0.483 | 0.376 |
| Total Cholesterol (mg/dL) | 178.3±47.0 | 192.9±36.3 | 199.5±55.8 | 0.123 | 0.073 | 0.214 |
| Triglycerides (mg/dL) | 147.4±36.3 | 159.3±80.5 | 161.9±95.6 | 0.112 | 0.073 | 0.231 |
| LDL-cholesterol (mg/dL) | 96.8±27.5 | 109.4±23.8 | 113.5±31.5 | 0.072 | 0.009 | 0.106 |
| HDL-cholesterol (ng/dL) | 46.1±9.5 | 44.7±9.6 | 41.8±11 | 0.108 | 0.099 | 0.444 |
| hsCRP (mg/L) | 1.9±1.3 | 3.2±1.4 | 4.0±1.7 | <0.001 | <0.001 | 0.031 |
| Ox-LDL (ng/mL) | 54.0±19.0 | 85.9±10.17 | 110.0±20 | <0.001 | <0.001 | <0.001 |
| Total NO (µmol/L) | 103.0±21.0 | 74.3±22.0 | 54.5±19.0 | <0.001 | <0.001 | <0.001 |
| Adiponectin (µg/mL) | 9.25±1.8 | 6.34±1.0 | 4.9±1.30 | <0.001 | <0.001 | <0.001 |
| Hypertension | 3(6) | 20(40) | 20(40) | <0.001 | <0.001 | 1.000 |
| Diabetes mellitus | 1(2) | 12(24) | 20(40) | <0.001 | <0.001 | <0.001 |
| Family history of CAD | 10(20) | 20(40) | 30(60) | <0.001 | <0.001 | 0.001 |
| Smoking | 2(4) | 8(16) | 15(30) | <0.001 | <0.001 | <0.001 |
| Statins | 2(4) | 18(36) | 28(56) | <0.001 | <0.001 | <0.001 |
| Aspirin | 0(0) | 28(56) | 32(64) | <0.001 | <0.001 | 0.156 |
| Antiplatelets | 0(0) | 20(40) | 20(40) | <0.001 | <0.001 | 1.000 |
| Nitrates | 0(0) | 15(30) | 15(30) | <0.001 | <0.001 | 1.000 |
Data are expressed as mean ± SD or number (%); BMI, body mass index; LDL-cholesterol, low density lipoprotein-cholesterol; HDL-cholesterol, high density lipoprotein-cholesterol; hsCRP, high sensitivity C-Reactive Protein; NO, nitric oxide; CAD, coronary artery disease.
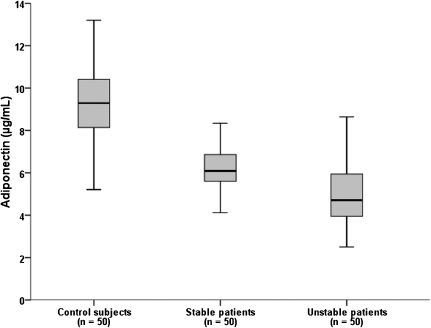
As shown in Figure 1, the plasma adiponectin levels were significantly lower in the unstable angina patients (4.90±1.3 µg/mL) than in the stable angina patients (6.34±1.0 µg/mL) or in the control subjects (9.25±1.8 µg/mL), and they were lower in the stable angina patients than in the control subjects (p<0.001; Table 1).
Figure 1.
Plasma adiponectin levels in unstable angina patients, stable angina patients and control subjects (ANOVA, p<0.001 for all and between groups). n, number of subjects in each group.
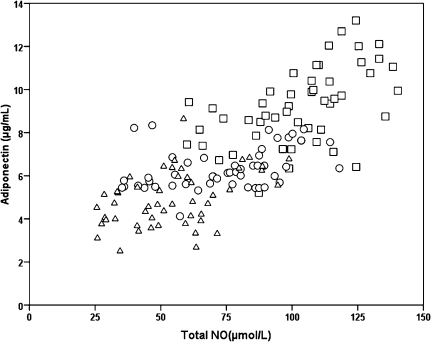
There was a significant inverse relationship between adiponectin and ox-LDL levels in the unstable angina patients (r = -0.447, p = 0.001), stable angina patients (r = -0.379, p = 0.007), and control subjects (r = -0.406, p = 0.003) (Figure 2).
Figure 2.
Correlation between plasma adiponectin and ox-LDL levels in control subjects (□), stable angina patients (○) and unstable angina patients (Δ).
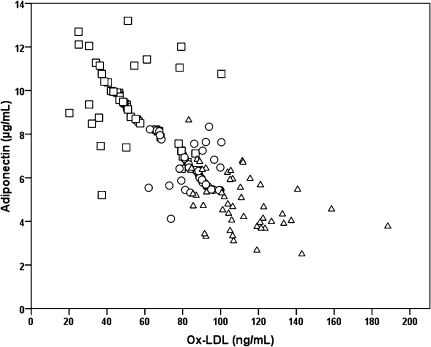
In all of the patients, plasma adiponectin levels correlated positively with plasma total NO levels. The correlations were stronger in the control subjects (r = 0.534, p = 0.01) than in the unstable angina patients (r = 0.448, p = 0.01) or in the stable angina patients (r = 0.405, p = 0.01). Furthermore, total NO levels were significantly higher in the control subjects than in the angina patients, and they were higher in the stable angina patients than in the unstable angina patients (Figure 3).
Figure 3.
Correlation between plasma adiponectin and total NO levels in control subjects (□), stable angina patients (○) and unstable angina patients (Δ).
The angina patients exhibited a trend toward higher levels of cholesterol, triglycerides, LDL-cholesterol, hsCRP and a lower level of HDL-cholesterol compared with the control subjects, but with the exception of hsCRP levels, these differences were not statistically significant (Table 1).
We also assessed the association between plasma adiponectin levels and conventional cardiovascular risk factors among the subjects. These correlations are presented in Table 2. As shown, no significant correlation was found between age, total cholesterol or HDL-cholesterol and adiponectin level.
Table 2.
Bivariate correlations between conventional clinical risk factors and adiponectin levels.
| Variable | Adiponectin (µg/mL) | p-value |
| Age (year) | 0.016 | 0.85 |
| Sex (women)* | 0.310 | 0.01 |
| BMI (kg/m2) | -0.289 | 0.01 |
| Total cholesterol (mg/dL) | -0.200 | 0.05 |
| Triglycerides (mg/dL) | -0.168 | 0.04 |
| LDL-cholesterol (mg/dL) | -0.259 | 0.01 |
| HDL-cholesterol (mg/dL) | 0.155 | 0.05 |
| hsCRP (mg/L) | -0.455 | 0.01 |
| Hypertension* | -0.337 | 0.01 |
| Diabetes mellitus* | -0.332 | 0.01 |
| Family history of CAD* | -0. 278 | 0.01 |
| Smoking* | -0.336 | 0.01 |
| Statins* | 0.236 | 0.04 |
*Point-biserial correlation. BMI, body mass index; LDL-cholesterol, low density lipoprotein-cholesterol; HDL-cholesterol, high density lipoprotein-cholesterol; hsCRP, high sensitivity C-reactive protein; CAD, coronary artery disease.
We did not find a significant difference in plasma adiponectin levels between patients with and without drug therapy. The stable and unstable angina patients did not differ with respect to the extent of coronary artery stenosis or the number of affected arteries. Among all of the subjects, plasma adiponectin levels were higher in women than in men (7.0±2.0 µg/mL vs. 6.7±2.4 µg/mL, p = 0.034).
To look for an independent association of plasma adiponectin level with the presence of stable versus unstable angina, a multiple logistic regression analysis was performed adjusting for age, gender and other clinical risk factors. As shown in Table 3, a low plasma adiponectin level was an independent predictor for both stable and unstable angina (OR = 0.51, p = 0.023; OR = 0.59, p = 0.001, respectively). Other predictors for the presence of stable and unstable angina, respectively, were age (OR = 1.26, p = 0.022; OR = 1.43, p = 0.042), hsCRP (OR = 1.62, p = 0.033; OR = 1.37, p = 0.003), ox-LDL (OR = 1.78, p = 0.014; OR = 2.01, p = 0.038), total NO (OR = 0.61, p = 0.008; OR = 0.76, p = 0.012, negative predictor), statins (OR = 0.64, p = 0.050, negative predictor for stable angina only), and family history of coronary artery disease (OR = 2.02, p = 0.023; OR = 2.17, p = 0.047).
Table 3.
Multiple logistic regression analysis of independent predictors for stable and unstable angina.
| Variable | Stable angina | Unstable angina | ||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age (year) | 1.26(1.35 – 1.63) | 0.022 | 1.43(1.25 – 1.73) | 0.042 |
| Sex (men) | 1.72(1.21 – 2.85) | 0.071 | 1.32(1.17 – 2.64) | 0.118 |
| BMI (kg/m2) | 1.11(0.88 – 2.38) | 0.140 | 1.21(1.12 – 2.28) | 0.154 |
| Total cholesterol (mg/dL) | 1.28(1.02 – 3.55) | 0.055 | 1.38(1.27 – 2.95) | 0.075 |
| Triglycerides (mg/dL) | 1.48(1.24 – 2.33) | 0.063 | 1.11(0.98 – 2.79) | 0.053 |
| LDL-cholesterol (mg/dL) | 2.04(1.32 – 3.07) | 0.056 | 1.92(1.83 – 3.01) | 0.06 |
| HDL-cholesterol (mg/dL) | 0.52(0.47 – 1.29) | 0.057 | 0.74(0.53 – 1.34) | 0.071 |
| hsCRP (mg/L) | 1.62(1.57 – 3.26) | 0.033 | 1.37(1.24 – 2.49) | 0.003 |
| Ox-LDL (ng/mL) | 1.78(1.14 – 2.43) | 0.014 | 2.01(1.74 – 2.27) | 0.038 |
| Total NO (µmol/L) | 0.61(0.38 – 0.74) | 0.008 | 0.76(0.62 – 0.98) | 0.012 |
| Adiponectin (µg/mL) | 0.51(0.34 – 0.73) | 0.023 | 0.59(0.44 – 0.81) | 0.001 |
| Hypertension | 1.88(1.62 – 2.48) | 0.069 | 2.11(1.97 – 2.53) | 0.063 |
| Diabetes mellitus | 1.98(1.67 – 2.14) | 0.054 | 2.47(2.28 – 2.84) | 0.072 |
| Family history of CAD | 2.02(1.56 – 2.49) | 0.023 | 2.17(1.53 – 2.79) | 0.047 |
| Smoking | 1.31(1.18 – 2.59) | 0.220 | 1.37(1.23 – 2.77) | 0.09 |
| Statins | 0.65(0.58 – 0.82) | 0.049 | 0.98(0.87 – 1.13) | 0.106 |
Results are presented for β coefficient. OR, odds ratio; CI, confidence interval; CAD, coronary artery disease. BMI, body mass index; LDL-cholesterol, low density lipoprotein-cholesterol; HDL-cholesterol, high density lipoprotein-cholesterol; hsCRP, high sensitivity C-reactive protein; NO, nitric oxide.
DISCUSSION
To the best of our knowledge, the association between plasma adiponectin level and the cardiovascular risk markers ox-LDL and total NO has not yet been evaluated in stable and unstable angina patients. The findings of the study demonstrate that plasma adiponectin levels are closely associated with the inflammatory markers ox-LDL and total NO in stable and unstable angina patients and that these relationships persist after adjustment for conventional cardiovascular risk factors. Also, this study revealed that plasma adiponectin levels are lower in patients with stable and unstable angina relative to control subjects, and this disparity can be used to identify patients.
Decreased levels of circulating adiponectin have been reported in patients with angiographically documented coronary artery disease.13,20 Our finding that adiponectin was significantly lower in the stable and unstable angina patients relative to the control subjects is in line with the findings of Nakamura et al.20 In another study conducted by Stefan et al, no significant difference in adiponectin levels was found between the stable and unstable angina patients.19 However, a recent study demonstrated that plasma adiponectin levels in patients with acute coronary syndrome are significantly lower than in those with stable coronary artery disease and that low adiponectin levels are correlated with the presence of complex coronary lesions.17 Low adiponectin concentrations in unstable coronary artery disease patients may contribute to coronary plaque vulnerability and thus may play a role in the pathophysiology of acute coronary syndrome.14 Therefore, coronary plaque instability in the acute setting may account for the lower adiponectin levels in our unstable angina patients relative to the stable angina patients. Despite these findings, further studies are required to address the difference in adiponectin levels between stable and unstable angina patients.
Ox-LDL and NO play roles in all stages of coronary artery disease.24,25 Decreased adiponectin levels are an indicator of increased oxidative state in the arterial wall and are associated with high ox-LDL levels in patients with type 2 diabetes mellitus and coronary artery disease.8 In our study, plasma adiponectin was found to be inversely correlated with ox-LDL. This correlation was strongest in the unstable angina patients, weaker in the stable angina patients and weakest in the control subjects, in accordance with the above study. Ox-LDL is a key factor in plaque instability.6 Given the protective effects of adiponectin against plaque vulnerability, the mutual relationship between adiponectin and ox-LDL may become lost during coronary artery disease, especially in the unstable angina patients.
Endothelial dysfunction is a primary event in the pathogenesis of coronary artery disease.3 Adiponectin directly promotes the production of NO by the endothelium.26 Hypoadiponectinemia is associated with endothelial dysfunction in the peripheral arteries.27 In our study, adiponectin levels exhibited a positive correlation with the total NO level. The correlation was weaker in the angina patients than in the control subjects. A beneficial effect of total NO elevation in patients with symptomatic coronary artery disease has been reported.28,29
Our finding of significantly lower total NO levels along with elevated levels of the oxidative markers ox-LDL and hsCRP in the angina patients demonstrates that adiponectin may act through antioxidative and anti-inflammatory mechanisms.
We found inverse associations between adiponectin levels and other conventional cardiovascular risk markers that were in accordance with the results of other studies.30-33
In a multiple logistic regression analysis that adjusted for other cardiovascular risk factors, a low plasma adiponectin level was an independent negative predictor of the presence of stable or unstable angina in the present study, which is in accordance with the findings of Pilz et al.19 The correlation between adiponectin and the risk of coronary heart disease is controversial. Although some studies have reported an inverse relationship between adiponectin level and the risk of coronary artery disease,13,16,19,34 others failed to find a significant relationship.35,36 Differences in the underlying conditions of the study populations may be the cause of the controversy. Altogether, the negative correlations between adiponectin and well-known cardiovascular risk factors in the above literature and in our study highlight the anti-atherogenic effects of elevated adiponectin levels. However, further studies are required to determine the precise nature of this relationship.
Hypoadiponectinemia is an early sign of a complex cardiovascular risk factor leading to the development and progression of atherosclerosis. However, the exact genomic and environmental interactions contributing to hypoadiponectinemia are not fully understood.37 Single nucleotide polymorphisms (SNPs) in the adiponectin gene have been associated with the early onset of coronary artery disease and low adiponectin levels.37,38 Moreover, adipose tissue dysfunction and visceral adiposity have been identified as significant predictors of adiponectin levels.39
There is no definite conclusion regarding the effects of insulin on adiponectin production.40 On the one hand, some in vitro studies have indicated that insulin decreases adiponectin production,41 but in the clinical setting, long-term insulin therapy has failed to increase adiponectin levels.42 On the other hand, in type B insulin resistance, high levels of insulin are accompanied by high levels of adiponectin.43
Oxidative stress44 and proinflammatory cytokines45 suppress adiponectin expression, whereas a Mediterranean diet and exercise increase plasma adiponectin levels.46,47
In our study, body mass index (BMI) and diabetes mellitus, two important cardiovascular risk factors, were negatively associated with plasma adiponectin levels, thereby indirectly corroborating the causal relationships that may exist between adiposity, insulin resistance and hypoadiponectinemia.39,41 Other cardiovascular risk factors, such as hypertension, smoking, family history of coronary disease HDL-cholesterol, triglycerides, and cholesterol, were also inversely associated with plasma adiponectin level, whereas female sex and statin therapy were positively associated with the plasma adiponectin level. According to these findings and to the above literature, the conventional cardiovascular risk factors may affect adiponectin levels, and there may be mutual relationships between adiponectin and the cardiovascular risk factors in the pathogenesis of atherosclerosis.
One limitation of this study is the sample size. Although our results follow a normal distribution, larger samples are frequently used in clinical investigations.
CONCLUSIONS
The findings of this study indicate that plasma adiponectin levels are lower in stable and unstable angina patients than in control subjects. These lower adiponectin levels may facilitate the stratification and identification of stable and unstable angina patients. The correlations found between adiponectin level and both NO and ox-LDL further corroborate the antiatherogenic effects of adiponectin in cardiovascular patients, and the in vivo mechanisms of atherosclerotic progression that are elucidated by these correlations may be useful for disease assessment.
REFERENCES
- 1.Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T, et al. Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin. Implications fpr metabolic regulation and bioactivity. J Biol Chem. 2003;278:9073–85. doi: 10.1074/jbc.M207198200. [DOI] [PubMed] [Google Scholar]
- 2.Han SH, Quon MJ, Kim JA, Koh KK. Adiponectin and cardiovascular disease: response to therapeutic interventions. J Am Coll Cardiol. 2007;49:531–8. doi: 10.1016/j.jacc.2006.08.061. 10.1016/j.jacc.2006.08.061 [DOI] [PubMed] [Google Scholar]
- 3.Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation. 2004;109:III27–32. doi: 10.1161/01.CIR.0000131515.03336.f8. [DOI] [PubMed] [Google Scholar]
- 4.Witztum JL, Steinberg D. Role of oxidized low density lipoprotein in atherogenesis. J Clin Invest. 1991;88:1785–92. doi: 10.1172/JCI115499. 10.1172/JCI115499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yla-Herttuala S, Palinski W, Butler SW, Picard S, Steinberg D, Witztum JL. Rabbit and human atherosclerotic lesions contain IgG that recognizes epitopes of oxidized LDL. Arterioscler Thromb. 1994;14:32–40. doi: 10.1161/01.atv.14.1.32. 10.1161/01.ATV.14.1.32 [DOI] [PubMed] [Google Scholar]
- 6.Vindis C, Escargueil-Blanc I, Elbaz M, Marcheix B, Grazide MH, Uchida K, et al. Desensitization of platelet-derived growth factor receptor-beta by oxidized lipids in vascular cells and atherosclerotic lesions: prevention by aldehyde scavengers. Circ Res. 2006;98:785–92. doi: 10.1161/01.RES.0000216288.93234.c3. 10.1161/01.RES.0000216288.93234.c3 [DOI] [PubMed] [Google Scholar]
- 7.Plant S, Shand B, Elder P, Scott R. Adiponectin attenuates endothelial dysfunction induced by oxidised low-density lipoproteins. Diab Vasc Dis Res. 2008;5:102–8. doi: 10.3132/dvdr.2008.017. 10.3132/dvdr.2008.017 [DOI] [PubMed] [Google Scholar]
- 8.Lautamaki R, Ronnemaa T, Huupponen R, Lehtimaki T, Iozzo P, Airaksinen KE, et al. Low serum adiponectin is associated with high circulating oxidized low-density lipoprotein in patients with type 2 diabetes mellitus and coronary artery disease. Metabolism. 2007;56:881–6. doi: 10.1016/j.metabol.2007.01.018. 10.1016/j.metabol.2007.01.018 [DOI] [PubMed] [Google Scholar]
- 9.Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, et al. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation. 2000;102:1296–301. doi: 10.1161/01.cir.102.11.1296. [DOI] [PubMed] [Google Scholar]
- 10.Ouchi N, Kihara S, Arita Y, Nishida M, Matsuyama A, Okamoto Y, et al. Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation. 2001;103:1057–63. doi: 10.1161/01.cir.103.8.1057. [DOI] [PubMed] [Google Scholar]
- 11.Tsuda K. Adiponectin and nitric oxide production in normotensive and hypertensive men. Clin Exp Pharmacol P. 2007;34:S64–S6. 10.1111/j.1440-1681.2007.04782.x [Google Scholar]
- 12.Arita Y, Kihara S, Ouchi N, Maeda K, Kuriyama H, Okamoto Y, et al. Adipocyte-derived plasma protein adiponectin acts as a platelet-derived growth factor-BB-binding protein and regulates growth factor-induced common postreceptor signal in vascular smooth muscle cell. Circulation. 2002;105:2893–8. doi: 10.1161/01.cir.0000018622.84402.ff. 10.1161/01.CIR.0000018622.84402.FF [DOI] [PubMed] [Google Scholar]
- 13.Kumada M, Kihara S, Sumitsuji S, Kawamoto T, Matsumoto S, Ouchi N, et al. Association of hypoadiponectinemia with coronary artery disease in men. Arterioscler Thromb Vasc Biol. 2003;23:85–9. doi: 10.1161/01.atv.0000048856.22331.50. 10.1161/01.ATV.0000048856.22331.50 [DOI] [PubMed] [Google Scholar]
- 14.Broedl UC, Lebherz C, Lehrke M, Stark R, Greif M, Becker A, et al. Low adiponectin levels are an independent predictor of mixed and non-calcified coronary atherosclerotic plaques. PLoS One. 2009;4:e4733. doi: 10.1371/journal.pone.0004733. 10.1371/journal.pone.0004733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawada T, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, et al. Low plasma adiponectin levels are associated with presence of thin-cap fibroatheroma in men with stable coronary artery disease. Int J Cardiol. 2010;142:250–6. doi: 10.1016/j.ijcard.2008.12.216. 10.1016/j.ijcard.2008.12.216 [DOI] [PubMed] [Google Scholar]
- 16.von Eynatten M, Schneider JG, Humpert PM, Kreuzer J, Kuecherer H, Katus HA, et al. Serum adiponectin levels are an independent predictor of the extent of coronary artery disease in men. J Am Coll Cardiol. 2006;47:2124–6. doi: 10.1016/j.jacc.2006.02.033. 10.1016/j.jacc.2006.02.033 [DOI] [PubMed] [Google Scholar]
- 17.Otsuka F, Sugiyama S, Kojima S, Maruyoshi H, Funahashi T, Matsui K, et al. Plasma adiponectin levels are associated with coronary lesion complexity in men with coronary artery disease. J Am Coll Cardiol. 2006;48:1155–62. doi: 10.1016/j.jacc.2006.05.054. 10.1016/j.jacc.2006.05.054 [DOI] [PubMed] [Google Scholar]
- 18.Selcuk MT, Selcuk H, Temizhan A, Maden O, Saydam GS, Dogan M, et al. Impact of plasma adiponectin levels to the presence and severity of coronary artery disease in patients with metabolic syndrome. Coron Artery Dis. 2008;19:79–84. doi: 10.1097/MCA.0b013e3282f3c40b. 10.1097/MCA.0b013e3282f3c40b [DOI] [PubMed] [Google Scholar]
- 19.Pilz S, Maerz W, Weihrauch G, Sargsyan K, Almer G, Nauck M, et al. Adiponectin serum concentrations in men with coronary artery disease: the LUdwigshafen RIsk and Cardiovascular Health (LURIC) study. Clin Chim Acta. 2006;364:251–5. doi: 10.1016/j.cccn.2005.07.011. 10.1016/j.cccn.2005.07.011 [DOI] [PubMed] [Google Scholar]
- 20.Nakamura Y, Shimada K, Fukuda D, Shimada Y, Ehara S, Hirose M, et al. Implications of plasma concentrations of adiponectin in patients with coronary artery disease. Heart. 2004;90:528–33. doi: 10.1136/hrt.2003.011114. 10.1136/hrt.2003.011114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cavusoglu E, Ruwende C, Chopra V, Yanamadala S, Eng C, Clark LT, et al. Adiponectin is an independent predictor of all-cause mortality, cardiac mortality, and myocardial infarction in patients presenting with chest pain. Eur Heart J. 2006;27:2300–9. doi: 10.1093/eurheartj/ehl153. 10.1093/eurheartj/ehl153 [DOI] [PubMed] [Google Scholar]
- 22.Miller M, Mead LA, Kwiterovich PO, Jr, Pearson TA. Dyslipidemias with desirable plasma total cholesterol levels and angiographically demonstrated coronary artery disease. Am J Cardiol. 1990;65:1–5. doi: 10.1016/0002-9149(90)90017-u. 10.1016/0002-9149(90)90017-U [DOI] [PubMed] [Google Scholar]
- 23.Swingen CM, Seethamraju RT, Jerosch-Herold M. Feedback-assisted three-dimensional reconstruction of the left ventricle with MRI. J Magn Reson Imaging. 2003;17:528–37. doi: 10.1002/jmri.10290. 10.1002/jmri.10290 [DOI] [PubMed] [Google Scholar]
- 24.Miller YI, Choi SH, Fang L, Tsimikas S. Lipoprotein modification and macrophage uptake: role of pathologic cholesterol transport in atherogenesis. Subcell Biochem. 2010;51:229–51. doi: 10.1007/978-90-481-8622-8_8. 10.1007/978-90-481-8622-8_8 [DOI] [PubMed] [Google Scholar]
- 25.Moncada S, Higgs EA. The discovery of nitric oxide and its role in vascular biology. Br J Pharmacol. 2006;147:S193–201. doi: 10.1038/sj.bjp.0706458. 10.1038/sj.bjp.0706458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H, Montagnani M, Funahashi T, Shimomura I, Quon MJ. Adiponectin stimulates production of nitric oxide in vascular endothelial cells. J Biol Chem. 2003;278:45021–6. doi: 10.1074/jbc.M307878200. 10.1074/jbc.M307878200 [DOI] [PubMed] [Google Scholar]
- 27.Tan KC, Xu A, Chow WS, Lam MC, Ai VH, Tam SC, et al. Hypoadiponectinemia is associated with impaired endothelium-dependent vasodilation. J Clin Endocrinol Metab. 2004;89:65–9. doi: 10.1210/jc.2003-031012. [DOI] [PubMed] [Google Scholar]
- 28.Heitzer T, Rudolph V, Schwedhelm E, Karstens M, Sydow K, Ortak M, et al. Clopidogrel improves systemic endothelial nitric oxide bioavailability in patients with coronary artery disease: evidence for antioxidant and antiinflammatory effects. Arterioscler Thromb Vasc Biol. 2006;26:1648–52. doi: 10.1161/01.ATV.0000225288.74170.dc. 10.1161/01.ATV.0000225288.74170.dc [DOI] [PubMed] [Google Scholar]
- 29.Heitzer T, Ollmann I, Koke K, Meinertz T, Munzel T. Platelet glycoprotein IIb/IIIa receptor blockade improves vascular nitric oxide bioavailability in patients with coronary artery disease. Circulation. 2003;108:536–41. doi: 10.1161/01.CIR.0000081774.31064.62. 10.1161/01.CIR.0000081774.31064.62 [DOI] [PubMed] [Google Scholar]
- 30.Shetty GK, Economides PA, Horton ES, Mantzoros CS, Veves A. Circulating adiponectin and resistin levels in relation to metabolic factors, inflammatory markers, and vascular reactivity in diabetic patients and subjects at risk for diabetes. Diabetes Care. 2004;27:2450–7. doi: 10.2337/diacare.27.10.2450. 10.2337/diacare.27.10.2450 [DOI] [PubMed] [Google Scholar]
- 31.Iwashima Y, Katsuya T, Ishikawa K, Ouchi N, Ohishi M, Sugimoto K, et al. Hypoadiponectinemia is an independent risk factor for hypertension. Hypertension. 2004;43:1318–23. doi: 10.1161/01.HYP.0000129281.03801.4b. 10.1161/01.HYP.0000129281.03801.4b [DOI] [PubMed] [Google Scholar]
- 32.Bahia L, Aguiar LG, Villela N, Bottino D, Godoy-Matos AF, Geloneze B, et al. Relationship between adipokines, inflammation, and vascular reactivity in lean controls and obese subjects with metabolic syndrome. Clinics. 2006;61:433–40. doi: 10.1590/s1807-59322006000500010. 10.1590/S1807-59322006000500010 [DOI] [PubMed] [Google Scholar]
- 33.Ozenoglu A, Balci H, Ugurlu S, Caglar E, Uzun H, Sarkis C, et al. The relationships of leptin, adiponectin levels and paraoxonase activity with metabolic and cardiovascular risk factors in females treated with psychiatric drugs. Clinics. 2008;63:651–60. doi: 10.1590/S1807-59322008000500014. 10.1590/S1807-59322008000500014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulze MB, Shai I, Rimm EB, Li T, Rifai N, Hu FB. Adiponectin and future coronary heart disease events among men with type 2 diabetes. Diabetes. 2005;54:534–9. doi: 10.2337/diabetes.54.2.534. 10.2337/diabetes.54.2.534 [DOI] [PubMed] [Google Scholar]
- 35.Lindsay RS, Resnick HE, Zhu J, Tun ML, Howard BV, Zhang Y, et al. Adiponectin and coronary heart disease: the Strong Heart Study. Arterioscler Thromb Vasc Biol. 2005;25:e15–6. doi: 10.1161/01.ATV.0000153090.21990.8c. 10.1161/01.ATV.0000153090.21990.8c [DOI] [PubMed] [Google Scholar]
- 36.Lawlor DA, Davey Smith G, Ebrahim S, Thompson C, Sattar N. Plasma adiponectin levels are associated with insulin resistance, but do not predict future risk of coronary heart disease in women. J Clin Endocrinol Metab. 2005;90:5677–83. doi: 10.1210/jc.2005-0825. 10.1210/jc.2005-0825 [DOI] [PubMed] [Google Scholar]
- 37.Gable DR, Hurel SJ, Humpheries SE. Adiponectin and its gene variants as risk factors for insulin resistance, the metabolic syndrome and cardiovascular disease. Atherosclerosis. 2006;188:231–44. doi: 10.1016/j.atherosclerosis.2006.02.010. 10.1016/j.atherosclerosis.2006.02.010 [DOI] [PubMed] [Google Scholar]
- 38.Filippi E, Sentinella F, Romeo S, Arca M, Berni A, Tiberti C, et al. The adiponectin SNP + 276G> T associates with early onset coronary artery disease and with lower levels of adiponectin in younger coronary artery disease patients (age ≤50 years) J Mol Med. 2005;83:711–9. doi: 10.1007/s00109-005-0667-z. 10.1007/s00109-005-0667-z [DOI] [PubMed] [Google Scholar]
- 39.Kwon K, Jung SH, Choi C, Park SH. Reciprocal association between visceral obesity and adiponectin : in healthy premenopausal women. Int J Cardiol. 2005;101:385–90. doi: 10.1016/j.ijcard.2004.03.050. 10.1016/j.ijcard.2004.03.050 [DOI] [PubMed] [Google Scholar]
- 40.Halleux CM, Takahashi M, Delporte ML, Derty R, Funahashi T, Matsuzawa Y, et al. Secretion of adiponectin and regulation of apM1 gene expression in human visceral adipose tissue. Biochem Biophys Res Commun. 2001;288:1102–7. doi: 10.1006/bbrc.2001.5904. 10.1006/bbrc.2001.5904 [DOI] [PubMed] [Google Scholar]
- 41.Fasshauer M, Klein J, Neumann S, Eszlinger M, Paschke R. Hormonal regulation of adiponectin gene expression in 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2002;290:1084–9. doi: 10.1006/bbrc.2001.6307. 10.1006/bbrc.2001.6307 [DOI] [PubMed] [Google Scholar]
- 42.Imagawa A, Funahashi T, Nakamura T, Moriwaki M, Tanaka S, Nishizawa H. Elevated serum concentration of adipose-derived factor, adiponectin, in patients with type 1 diabetes. Diabetes Care. 2002;25:1665–6. doi: 10.2337/diacare.25.9.1665. 10.2337/diacare.25.9.1665 [DOI] [PubMed] [Google Scholar]
- 43.Semple RK, Soos MA, Luan J, Mtchell Cs, Wilson JC, Gurnell M. Elevated plasma adiponectin in humans with genetically defective insulin receptors. J Clin Endocrinol Metab. 2006;91:3219–23. doi: 10.1210/jc.2006-0166. 10.1210/jc.2006-0166 [DOI] [PubMed] [Google Scholar]
- 44.Kamigaki M, Sakaue S, Tsujino I, Ohira H, Ikeda D, Itoh N. Oxidative stress provokes atherogenic changes in adipokine gene expression in 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2006;339:624–32. doi: 10.1016/j.bbrc.2005.11.059. 10.1016/j.bbrc.2005.11.059 [DOI] [PubMed] [Google Scholar]
- 45.Kim KY, Kim JK, Jeon JH, Yoon SR, Choi I, Yang Y. c-Jun N-terminal kinase is involved in the suppression of adiponectin expression by TNF-alpha in 3T3-L1 adipocytes. Biochem Biophys Res Commun. 2005;327:460–7. doi: 10.1016/j.bbrc.2004.12.026. 10.1016/j.bbrc.2004.12.026 [DOI] [PubMed] [Google Scholar]
- 46.Mantzoros CS, Wiliams CJ, Manson JE, Meigs JB, Hu FB. Adherence to the Mediterranean dietary pattern is positively associated with plasma adiponectin concentration in diabetic women. Am J Clin Nutr. 2006;84:328–35. doi: 10.1093/ajcn/84.1.328. [DOI] [PubMed] [Google Scholar]
- 47.Tsukinoki R, Morimoto K, Nakayama K. Association between lifestyle factors and plasma adiponectin levels in Japanese men. Lipids Health Dis. 2005;4:27. doi: 10.1186/1476-511X-4-27. 10.1186/1476-511X-4-27 [DOI] [PMC free article] [PubMed] [Google Scholar]