Abstract
Social Security is the most important and effective income support program ever introduced in the United States, alleviating the burden of poverty for millions of elderly Americans. We explored the possible role of Social Security in reducing mortality among the elderly. In support of this hypothesis, we found that declines in mortality among the elderly exceeded those among younger age groups following the initial implementation of Social Security in 1940, and also in the periods following marked improvements in Social Security benefits via legislation and indexing of benefits that occurred between the mid-1960s and the early 1970s. A better understanding of the link between Social Security and health status among the elderly would add a significant and missing dimension to the public discourse over the future of Social Security, and the potential role of income support programs in reducing health-related socioeconomic disparities and improving population health.
Keywords: Social Security, income support, social epidemiology, health policy
Introduction
Low socioeconomic position, measured variously in terms of poverty, income, wealth, education, or occupation, has been repeatedly linked to a greater burden of disease and death in the United States and other countries.1–4 While this has been one of the most consistent findings in social and epidemiological research for decades, it is surprising that the major social programs that were designed to ease the burden of poverty or otherwise improve economic wellbeing of the US population have only rarely been examined with respect to health and disease.5–7
Social Security (specifically, Old Age and Survivor Insurance) is the single most important and effective income support program ever introduced in the United States. It has been credited with alleviating the burden of poverty for millions of Americans, particularly for the elderly.8 Recent census data indicate that over 40 per cent of the US population aged 65 years or older is kept out of poverty by Social Security.9 Supplemental Security Income (SSI), which provides cash or benefits to low-income elderly people, has also helped to improve the economic status of the poorest stratum of Social Security beneficiaries.
Most public attention to the Social Security system from the media and politicians focuses on the system’s long-range financial problems. Some economists and policymakers have been pushing for cuts in Social Security benefits as a way of addressing our long-term federal budget deficits. The National Commission on Fiscal Responsibility and Reform established by President Obama to address the nation’s long-term fiscal crisis, has, for example, recommended steps to alter Social Security by lowering benefits and raising payroll taxes.10 Legislation introduced in early 2010 by Representative Paul Ryan (Republican, Wisconsin), titled the ‘Roadmap for America’s Future Act of 2010’, would reduce future Social Security benefits and raise the age before benefits could be obtained.11 Far less attention has been paid to the program’s unsurpassed record of reducing poverty and providing a safety net among the elderly. Still less attention considers the possible effect on the public’s health.
Our study explores the potential impact of Social Security on mortality among the elderly in the United States. We hope it will call attention to the likely relationship between major socioeconomic programs – such as Social Security – and the public’s health. Our goal is to broaden the perspectives of those in health, economics, social policy, and research regarding ways of improving population health and reducing health-related disparities.
Social Security and the Economic Wellbeing of the Elderly
The economic wellbeing of the elderly has improved dramatically since World War II.12–14 Poverty fell from 35.2 per cent for persons aged 65 and older in 1959 (the first year official statistics were tabulated) to 9.7 per cent in 2008.15 This compares with children, for example, whose poverty rates fell far less – from 27.3 to 19 per cent over the same time period. As early as the 1940s, the average monthly Social Security benefit accounted for 16 to 17 per cent of median family income for those aged 65 and older. (The percentage of income generated by Social Security benefits is estimated here by dividing the median Social Security benefit by the median family income in current dollars for each year.) This proportion rose to 28 per cent in 1950, when Congress mandated the first in a series of benefit increases. With the help of additional mandated increases, which improved the real income of the elderly substantially during the 1960s and early 1970s, and the indexing of benefits to inflation, begun in 1975, Social Security benefits now account for 28 to 38 per cent of median income among the elderly.16
An early attempt to quantify the economic status of the elderly was conducted by Marjorie Shearon of the Social Security Board’s Bureau of Research and Statistics immediately before the introduction of monthly Social Security benefits and published in 1938.17 Forty years later, the Social Security Administration published a comparative analysis, tracking the economic progress of the population aged 65 years and older.18 It found, for example, that in 1937, 47.5 per cent of the non-institutionalized elderly had no income whatsoever (presumably relying entirely on friends, relatives, and charity). By 1978, the group reporting no income dropped dramatically to only 1.5 per cent. The single most important factor accounting for this change was Social Security benefits, followed by a distant second, the growth of private pensions.
At present, more detailed evidence describes the role of Social Security in alleviating the burdens of poverty and providing a safety net for retirees. Social Security remains a key source of income for most of its recipients. In 2008, more than half (63.9 per cent) of the beneficiaries aged 65 years or older received 50 per cent or more of their total income from their monthly Social Security checks. For a third of elderly beneficiaries (34.2 per cent), it provided 90 per cent or more of their income.19,20 In addition, the reliance of the elderly on private, defined benefit retirement plans has declined dramatically.21
Statistics on poverty are no less compelling. Nearly 44 per cent of the elderly are kept out of poverty by Social Security.9 This impact on poverty is more substantial than all other government programs combined. According to one study, nine of every 10 elderly people lifted from poverty by government benefit programs, including state and local cash assistance programs, are lifted out by Social Security.22
Finally, it can be argued that Social Security improves the social and economic status of the elderly in at least two dimensions: (1) level of current income, and (2) freedom to exit from unpleasant or onerous work and/or increase the amount of leisure time. The introduction of Social Security accelerated retirement at younger ages. In 1942, for example, approximately 48 per cent of men and 9 per cent of women aged 65 years or older participated in the labor force.23 Although the figures for women have not changed as much over the years (13.3 per cent as of 2008), the percentage of men working past 65 has declined significantly to 21.5 per cent in 2008.22
Social Security and Health of the Elderly
Analysts have observed that socioeconomic disparities in health and mortality are large in infancy and early childhood, diminish through very early adulthood, widen dramatically through middle and early old age, and then diminish in old age.24 There are multiple potential causes of diminishing socioeconomic disparities in health and mortality in the oldest age group, but few have been carefully evaluated. Some evidence suggests that differential rates of mortality by socioeconomic status at younger ages are not the primary explanation.25 Particularly in the United States, one plausible cause of reduced health disparities is that the population aged 65 years or older is the only one that has a substantial social welfare safety net – both income support via Social Security since 1940 and later universal health insurance via Medicare (the Federal program of health insurance for the elderly) since 1965.
Despite the important role of income support provided by Social Security and the well-known relationship between socioeconomic status and health, surprisingly little research has tried to demonstrate a link between Social Security benefits and health consequences. The major exception is the work of Jere Behrman, Robin Sickles, and Paul Taubman.26 They found that an additional $1000 of Social Security benefits lowered the mortality hazard by 10–20 per cent. Given their study sample and design (heads of households from the Retirement History Survey who were 58–63 in 1969 with 10 years of mortality follow-up), they concluded that this reduction in mortality was a function of the inverse relationship between income and mortality. As the level of Social Security benefits is related to one’s career earnings history, the additional $1000 of benefits reflects higher lifetime earnings. They also found that SSI has an even larger impact on mortality than Social Security benefits, which they attributed to the fact that SSI goes exclusively to the poor and near-poor elderly.
In contrast, Snyder and Evans examined the impact of differing levels of Social Security benefits on mortality.27 As a result of the changes made in the 1970s to lower costs of the program, for beneficiaries with identical earning histories, those born before 1 January 1917 received a higher benefit compared to those born after this date. Their study showed that the beneficiaries with lower payments were more likely to work and had lower mortality rates after age 65 years. Their results seem to suggest that source of income was as important as amount of income. They conclude that the time spent working decreased social isolation, a co-factor in mortality, suggesting that work had a positive health impact. One critique of their study is that their results measured the effect of increases for those beneficiaries who were wealthier and healthier and did not reflect the impact on the poorer elderly. Handwerker pointed out that mortality differences observed by Snyder and Evans occurred even before this cohort began collecting Social Security benefits.28
More recently, Herd et al studied the changes in SSI benefits and changes in disability for beneficiaries aged 65 years and older.6 They conclude that higher SSI benefit levels reduced disability in this group and their results remained robust regardless of the disability measure used (self-reported health condition or census Activities of Daily living (ADL) measure) and whether or not beneficiaries also received Medicaid (state programs to pay for medical care used by the indigent) payments for medical services. In addition, a preliminary analysis of the old-age assistance program from 1930 to 1955 by Balan-Cohen demonstrates an inverse relationship between income support for the poor elderly and mortality.5 These findings affirm that income policies have potential for improving health outcomes among the elderly.
A few studies in other nations have considered the effect of state pension programs on health. One, in South Africa, looked at the impact of expanded pension payments to older people.29 In households where incomes were pooled with other earners, self-reported health (including psychological health) of adults was improved, children living in the households were taller, and overall nutrition and sanitation were improved. Another study looked at the effect of the 1996 pension crisis on Russian households, where almost one-third of pensioners went without benefits for a prolonged period of time.30 What was the health impact? The authors found that poverty rates doubled, nutrition standards decreased, and pensioners who received no payments were 5 per cent more likely to die in the 2 years immediately following the crisis. In a more recent study looking at the impact of pension reform in China, the authors found that as ‘pension wealth declines, households reduce their expenditures on education and health for children’.31 Finally, in an analysis of 18 OECD countries, Norström and Palme found that old-age pensions had a significant inverse impact on all-cause mortality among the elderly.32 In other words, the existence of public pension income affects household consumption and may have an indirect effect on health outcomes. On balance, the few available data about the role of Social Security and public pensions on the health of the elderly are consistent with our hypothesis that Social Security in the United States has resulted in improvements in the health of the elderly.
Methods
The purpose of our analysis is to evaluate more directly the hypothesis that Social Security has improved the health and longevity of the elderly population and hence contributed to overall improvements in population health over the last seven decades. We model ‘exposure’ to Social Security for those aged 65 years plus, specifically to Old-Age and Survivors Insurance benefits, capturing program effects among age groups, and over time within age groups. We model overall and non-infectious disease mortality as functions of age and time period using piecewise linear regression. According to Andersson et al, ‘Linear segmented regression analysis is a partly controlled design where the trend before the event of interest is used as a control period and can be controlled by the use of a comparison area or group that was not affected by the policy studied’.33 This approach allows us to consider pre- and post-policy temporal trends. The limitations in our approach include the challenge of ‘separating the effect of time from that of the policy, accounting for heterogeneity in the policy effect’.34 Mortality decline is assumed to be linear over time.35 Wald tests were used to determine the significance of differences in declines of mortality rates. Our residual plots show no signs of autocorrelation.
We test our hypothesis in two specific ways. If the data support the hypothesis that Social Security has a positive impact on health of the elderly, we would observe:
A steeper decline in mortality in the elderly compared with younger age groups during the time period that followed the initial implementation of Social Security in 1940.
A steeper decline in mortality in the elderly compared with younger age groups in the time period that followed the legislated improvements in Social Security benefits and then after indexing of Social Security benefits that occurred between the mid-1960s and the early 1970s.
Data sources
Age group-specific mortality rates from all causes and from infectious diseases for the years 1900 through 1996 were provided by Gregory Armstrong at the Centers for Disease Control and Prevention (CDC). These data were used in a published analysis of trends in infectious disease mortality in the United States during the twentieth century.36 Total population counts for each age grouping in each year were also provided. The age groups represented in the original data are infants (less than 1 year old), children (ages 1 to 4 years), 10-year age groupings from age 5 through 84 years, and older than age 84 years. As infants, children, and young adults are not relevant for testing our hypotheses, the age groups younger than 45 years were excluded. Thus, for our analyses, we constructed 10-year age-groupings from age 45 to age 74 years (45–54 years, 55–64 years, and 65–74 years) and a grouping for everyone older than 74 years. The oldest group was calculated by combining the original CDC data for 75 to 84 year olds and those 85 years and older, using a population-weighted average for the two subgroups.
Mortality data were grouped by calendar years into five ‘eras’: 1900–1939, 1940–1954, 1955–1969, 1970–1984, and 1985–1996. The eras were defined by our study hypotheses that highlight two crucial periods around which we should observe shifts in mortality patterns: 1940–1954, the period following the introduction of monthly Social Security benefits (1940) and 1970–1984, which reflected a period of substantial growth in the amount of Social Security benefits received. Similarly, our analyses and results will focus on these same two crucial periods. The years 1900–1939 are the ‘control’ period before the Social Security program was initiated; 1955–1969 is an era in which Social Security existed but did not grow substantially; and finally we distinguish 1985–1996 because of the new impact of HIV disease on infectious disease mortality.
Non-infectious disease mortality rates were calculated as the all-cause mortality rate minus the infectious disease mortality rate.
Statistical analyses
To test Hypotheses 1 and 2, we first graphed age-specific mortality rates over time for each age group and conducted piecewise linear regression analyses to test the statistical significance of observed differences in rates of change for the two crucial periods of interest (1940–1954 and 1970–1984) compared with the other eras for the two age groups under 65 years, compared with the two age groups 65 years and older.
We then modeled the logarithm of the all-cause and non-infectious disease mortality rates assuming that separate rates of decline might be found for each age group and all time trends were piecewise, log-linear. When the natural logarithm of mortality rate is regressed against time, as in these models, the slope of the regression line is an estimate of the average annual relative change in the untransformed rate variable. For example, a regression coefficient associated with a year that equals –0.02 can be interpreted as an average annual decline of 2 per cent in the untransformed mortality rate. Wald tests were used to compare the rates of change for each of the four outcomes (all-cause mortality, non-infectious disease mortality, and their respective log transformations) for each age group with that of the next youngest age group in each era and to compare the rates of change for each era with that of the previous era in each age group. We include results for both the log-transformed and untransformed mortality data, as there is some contention as to which provides the best evidence, especially from a policy perspective.37
Results
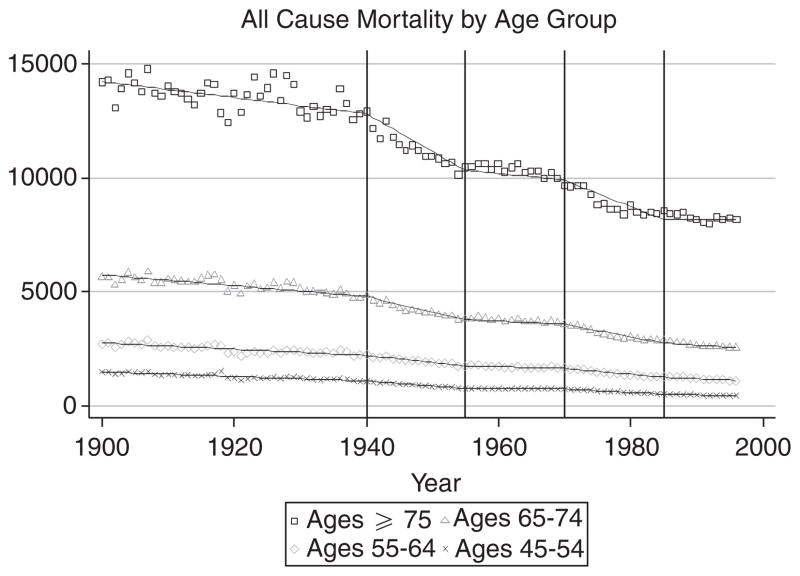
Figure 1 shows age-specific mortality over the study period for four age groups, 45–54 years, 55–64 years, 65–74 years, and 75–84 years. These data suggest that the rate of mortality decline was approximately steady before 1940 for all four age groups, but just after that year there was marked deceleration of mortality among both age groups 65 years and older compared with the two age groups younger than 65 years. This steeper decline in mortality in the over-65 year groups compared with younger people in the period that followed the initial implementation of Social Security in 1940 is consistent with our hypothesis. As elderly mortality declines could have been simply due to economic growth, we conducted additional sensitivity analyses that included controls for gross domestic product growth over this time period; our results did not substantially change from what is presented below.
Figure 1.
All-cause mortality by age group, the United States, 1900–1997 deaths per 100 000 population.
The greater rate of decline since 1940 does not appear to have been uniform over the entire post-1940 period. Rather, in both of the two age groups 65 years and older, there was a sharp deceleration of mortality in both the 1940–1954 and 1970–1984 eras, with sharpest rate of decline in the first half of both of these intervals. These steeper declines in mortality in the over-65 age group compared to the younger age groups specifically in the periods that followed the initial implementation of Social Security (1940) and the marked improvements in benefits, indexing of Social Security and increased enrollment (beginning in the late 1960s), are also consistent with our hypothesis.35
Linear regression analyses of these data confirmed that, although mortality rates for all age groups fell throughout the entire study period, the 65 years and older groups experienced a statistically significant greater decline in mortality after 1940 compared with the earlier period (see Figure 2). This is in stark contrast to the groups younger than 65 years, whose mortality rate declines before and after 1940 remained virtually the same. Furthermore, the rates of mortality decline for these younger age groups were modest and not statistically different across the time periods.
Figure 2.
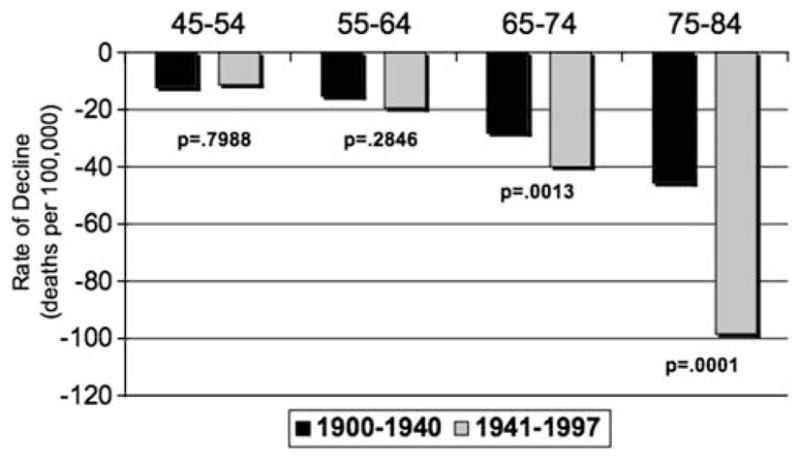
Results of linear regression analysis comparing average annual mortality decline for pre- and post-1940 eras for each of four age groupings: all-cause mortality by age group, the United States, 1900–1997.
Table 1 illustrates the rates of decline in mortality for each age group and era for each of the four outcomes (all-cause mortality, non-infectious disease mortality, and their respective log transformations). The first of the three columns in each era represents either the average annual absolute decline in mortality rates or the log average annual decline in mortality rates for each age group. The log average annual decline can be interpreted as an annual percent decline, for example for the age group 65–74 years in the era 1940–1954, there was an average annual decline of 1.49 per cent in the mortality rate. The second column is the P-value associated with a Wald test of the statistical significance of the difference between declines in mortality rates in that era and the preceding one (for example, 1900–1939), thus representing an era-to-era comparison within each age group. The third column is the P-value associated with a Wald test of the statistical significance of the difference between declines in mortality rates of that age group with that of the next youngest age group within a particular era (for example, 55–64 years). As expected, larger reductions in average annual absolute mortality rates are consistently observed in the groups aged 65 years and older compared with those younger than 65 years with the one exception of non-infectious disease mortality for those ≥75 in 1930–1939. This latter group (≥75) clearly had a significant drop in infectious disease mortality during this time period as well.
Table 1.
Decline in mortality rates for people aged 45 years and older, 1900–1984
| Age group | 1900–1939 era
|
1940–1954 era
|
1955–1969 era
|
1970–1984 era
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality declinea | P-valueb | P-valuec | Mortality declinea | P-valueb | P-valuec | Mortality declinea | P-valueb | P-valuec | Mortality declinea | P-valueb | P-valuec | |
| All-cause mortality | ||||||||||||
| 45–54 | 938 | NA | NA | 1917 | 0.00 | NA | 104 | 0.00 | NA | 1506 | 0.00 | NA |
| 55–64 | 1336 | NA | 0.00 | 2908 | 0.00 | 0.00 | 666 | 0.00 | 0.01 | 2854 | 0.00 | 0.00 |
| 65–74 | 2074 | NA | 0.00 | 6365 | 0.00 | 0.86 | 1494 | 0.00 | 0.93 | 5487 | 0.00 | 0.06 |
| ≥75 | 2611 | NA | 0.00 | 15 699 | 0.00 | 0.25 | 3506 | 0.00 | 0.56 | 10 341 | 0.04 | 0.00 |
| Log (all-cause mortality) | ||||||||||||
| 45–54 | 0.72 | NA | NA | 2.09 | 0.00 | NA | 0.14 | 0.00 | NA | 2.42 | 0.00 | NA |
| 55–64 | 0.53 | NA | 0.00 | 1.47 | 0.00 | 0.00 | 0.39 | 0.00 | 0.01 | 1.96 | 0.00 | 0.00 |
| 65–74 | 0.40 | NA | 0.21 | 1.49 | 0.00 | 0.00 | 0.40 | 0.00 | 0.06 | 1.72 | 0.00 | 0.00 |
| ≥75 | 0.19 | NA | 0.24 | 1.37 | 0.00 | 0.00 | 0.34 | 0.00 | 0.06 | 1.15 | 0.00 | 0.00 |
| Non-infectious disease mortality | ||||||||||||
| 45–54 | 380 | NA | NA | 1068 | 0.00 | NA | 911 | 0.00 | NA | 1413 | 0.00 | NA |
| 55–64 | 553 | NA | 0.00 | 1807 | 0.00 | 0.01 | 519 | 0.01 | 0.01 | 2681 | 0.00 | 0.00 |
| 65–74 | 681 | NA | 0.00 | 4800 | 0.00 | 0.11 | 1347 | 0.00 | 0.06 | 5144 | 0.00 | 0.09 |
| ≥75 | 320 | NA | 0.00 | 11718 | 0.00 | 0.33 | 3841 | 0.00 | 0.86 | 9937 | 0.01 | 0.00 |
| Log (non-infectious disease mortality) | ||||||||||||
| 45–54 | 0.38 | NA | NA | 1.29 | 0.00 | NA | 0.01 | 0.00 | NA | 2.31 | 0.00 | NA |
| 55–64 | 0.26 | NA | 0.00 | 0.98 | 0.00 | 0.00 | 0.31 | 0.01 | 0.01 | 1.87 | 0.00 | 0.00 |
| 65–74 | 0.15 | NA | 0.00 | 1.19 | 0.00 | 0.86 | 0.37 | 0.00 | 0.93 | 1.65 | 0.00 | 0.06 |
| ≥75 | 0.03 | NA | 0.00 | 1.09 | 0.00 | 0.25 | 0.39 | 0.00 | 0.56 | 1.15 | 0.00 | 0.00 |
For untransformed mortality data (All Cause and Non-infectious Disease), values represent average annual absolute decline in mortality; for log transformations, values can be interpreted as an annual per cent decline in mortality.
Era-to-era comparison within age groups.
Age grouping to age grouping comparisons within era.
The annual percent declines within eras, however, are inconsistent across younger and older age groups. We would expect to find the era-to-era comparisons to more clearly demonstrate differences in mortality declines across age groups than within era comparisons. For example, the dramatic decline in cardiovascular disease mortality in the 1970s and 1980s was most pronounced in the younger age groups and may account for larger mortality declines in these age groups during this era.38,39 Similarly, there are undeniably a host of unmeasured factors affecting mortality among the age cohorts born in the last half of the nineteenth century particularly affecting mortality in the 1900–1930 era.
The era-to-era comparisons clearly indicate that average absolute mortality declines (and the annual percent declines) were experienced within all age groups. The magnitude of these declines is, however, greater for the 1970–1984 period compared to the 1955–1969 period, as well as the 1940–1954 period compared to the 1900–1939 period. These patterns of differences between eras largely held for both absolute declines in mortality rates, as well as annual percent declines and support our hypotheses.
Summary and Discussion
Taken together, we believe these data largely support our hypothesis that improvements in socioeconomic status via the Social Security program have had a beneficial impact on the health of the elderly in the United States. Our most convincing test showed that non-infectious disease mortality declined throughout the first 80 years of the twentieth century. The deceleration of mortality observed in the first crucial period beginning 1940 was substantially more pronounced for those aged 65 years and older than for the younger groups. As non-infectious disease mortality accounted for more than 90 per cent of the decline in all-cause mortality, it is clear that the difference in deceleration of the non-infectious disease mortality between the older and younger age groups across the relevant eras is large enough to admit explanation by a factor specifically affecting the elderly, that is, Social Security.
Unadjusted comparisons of age groups and parallelisms among time series cannot exclude alternative explanations because the data are also consistent with other interpretations of the changing nature of and access to medical care. Specifically the period from 1940 to 1955 was also one in which the use of antibiotics in the treatment of infectious disease emerged and grew in clinical medicine, and the period 1971 to 1985 saw the growth of Medicare and improvement in the treatment and prevention of life-threatening chronic diseases, especially heart disease.35,40 Limited availability of aggregate data makes it difficult to estimate empirically the relative importance of these changes in medical care versus the introduction and then indexing of Social Security cash benefits. It should be noted that we find significant effects in mortality decline even before the introduction of Medicare.
With our data we were however able to estimate rates of declines in various causes of death to approximate the impact of antibiotics, the effects of which should be seen almost entirely in changing rates of infectious disease among all age groups. Consistent with the patterns we originally hypothesized and tested, non-infectious disease mortality rates declined throughout the 1900s in both the young and elderly age strata, but the rates of decline for the elderly were in almost all instances higher than those for the younger age groups. To determine whether the income effect of Social Security truly exists as an independent phenomenon when other confounding effects like antibiotic use or medical technology are adequately controlled awaits further research.
Caveats exist with respect to our analyses beyond antibiotic use. We could not distinguish between income levels of beneficiaries within each era. It is likely that the beneficial impact of Social Security on health could be correlated with the proportion of total income the benefit represents. We also cannot distinguish between the significance of access to medical care versus income effects on other co-factors of mortality, including psychosocial, economic, and environmental conditions of life that may be mitigated via improved nutrition and housing, reductions of psychosocial (especially financial) stress, and increased resources for adapting to stress and threats to health.5,24 Similarly, both the decline in smoking rates and the civil rights movement have been shown to have had salutary impacts on population health beginning in the 1960s.35,41 These distinctions could well strengthen our results in key population subgroups and gain significance as the political debate on universal health coverage continues and as researchers investigate the correlation between other social and economic factors on improving population health.
Overall, we believe that the data we have examined are consistent with the hypothesis that Social Security improved the health of the elderly by improving living conditions and increasing access to medical care. Social Security’s role in alleviating the burden of poverty for millions of Americans and its potential link to improved health status among the elderly should add a cautionary note to policymakers as they are poised to radically alter the future of Social Security for generations to come.
Acknowledgments
Support for this article was provided, in part, by a RWJF Investigator Award in Health Policy Research (Arno) from the Robert Wood Johnson Foundation, Princeton, New Jersey and by grant P60-MD0005-03 from the National Institute on Minority Health and Health Disparities (Arno, Schechter). Special thanks to Nancy Sohler for her preliminary assistance with the analysis and to Robert G. Hughes, David Mechanic, Al Tarlov, Lynn Rogut, and Hal Strelnick for their support and encouragement.
References
- 1.Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 2.Marmot M, Wilkinson RG. Social Determinants of Health. 2. Oxford: UK Oxford University Press; 2006. [Google Scholar]
- 3.Lantz PM, House JS, Lepkowski LM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality. Journal of the American Medical Association. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 4.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. New England Journal of Medicine. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 5.Balan-Cohen A. The effect of income on elderly mortality: Evidence from the Old Age Assistance Program in the United States. American Economic Association Conference Papers; 2009. [accessed 1 January 2009.]. http://www.aeaweb.org/assa/2009/author_papers.php?author_ID=6557. [Google Scholar]
- 6.Herd P, Schoeni RF, House JS. Upstream solutions: Does the supplemental security income program reduce disability in the elderly? The Milbank Quarterly. 2008;86:5–45. doi: 10.1111/j.1468-0009.2007.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connor J, Rodgers A, Priest P. Randomized studies of income supplementation: A lost opportunity to assess health outcomes. Journal of Epidemiology and Community Health. 1999;53:725–730. doi: 10.1136/jech.53.11.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Englehardt GV, Gruber J. Working Paper 10466. Cambridge MA: National Bureau of Economic Research; 2004. Social Security and the Evolution of Elderly Poverty. [Google Scholar]
- 9.Romig K. Social Security Reform: Possible Effects on the Elderly Poor and Mitigation Options. Congressional Research Service Report to Congress; 2008. [accessed 6 January 2011.]. www.globalaging.org/elderrights/us/2008/socreform.pdf. [Google Scholar]
- 10.National Commission on Fiscal Responsibility and Reform. [accessed 18 December 2010.];The Moment of Truth: Report of the National Commission on Fiscal Responsibility and Reform. 2010 December 1; http://www.fiscalcommission.gov/news/moment-truth-report-national-commission-fiscal-responsibility-and-reform.
- 11. [accessed 12 July 2010.];H.R.4529: Roadmap for America’s Future Act of 2010. http://www.govtrack.us/congress/bill.xpd?bill=h111-4529.
- 12.Wright JD, Devine JA. Poverty among the elderly. Journal of Long-Term Home Health Care. 1995;13(1):5–16. [PubMed] [Google Scholar]
- 13.Radner DB. Incomes of the elderly and nonelderly, 1967–92. Social Security Bulletin. 1995;58(4):82–101. [PubMed] [Google Scholar]
- 14.Ross CM, Danziger S, Smolensky E. Interpreting changes in the economic status of the elderly, 1949–1979. Contemporary Policy Issues. 1987;5(2):98–112. doi: 10.1111/j.1465-7287.1987.tb00259.x. [DOI] [PubMed] [Google Scholar]
- 15.DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2008. Washington DC: Government Printing Office; 2009. U.S. Census Bureau, Current Population Reports; pp. 60–236. [Google Scholar]
- 16.Kollman G. Summary of Major Changes in the Social Security Cash Benefits Program: 1935–1996. Congressional Research Service Report to Congress; 1996. [accessed 5 January 2011.]. http://www.ssa.gov/history/pdf/crs9436.pdf. [Google Scholar]
- 17.Shearon M. Economic status of the aged. Social Security Bulletin. 1938;1(1):5–17. [PubMed] [Google Scholar]
- 18.Upp M. A look at the economic status of the aged then and now. Social Security Bulletin. 1982;45(3):16–22. [PubMed] [Google Scholar]
- 19.Social Security Administration. Annual statistical supplement, 2008 to the Social Security Bulletin. Office of Policy, Office of Research, Evaluation and Statistics; 2008. SSA Publication No. 13–11700. [Google Scholar]
- 20.Social Security Administration. Office of retirement and disability policy. [accessed 10 July 2010.];Income of the Aged Chartbook 2008. 2008 http://www.socialsecurity.gov/policy/docs/chartbooks/income_aged/2008/iac08.html#definitions.
- 21.Social Security Administration. [accessed 22 December 2010.];Defined Contribution Pension Plans and the Supplemental Security Income Program. 2006 Policy Brief No. 2006-01 http://www.ssa.gov/policy/docs/policybriefs/pb2006-01.pdf.
- 22.Purcell P. Older Workers: Employment and Retirement Trends. Congressional Research Service Report to Congress; 2009. [accessed 6 January 2011.]. http://digitalcommons.ilr.cornell.edu/key_workplace/655. [Google Scholar]
- 23.U.S. Census Bureau. Current Population Reports, Series P-50, No. 2. 1945. Current Population Survey. [Google Scholar]
- 24.Robert SA, House JS. Socioeconomic status and health over the life course. In: Abeles RP, Gift HC, Ory MG, editors. Aging and Quality of Life. New York: Springer-Verlag; 1994. pp. 253–274. [Google Scholar]
- 25.Beckett M. Converging health inequalities in later life: An artifact of mortality selection? Journal of Health and Social Behavior. 2000;41(1):106–119. [PubMed] [Google Scholar]
- 26.Behrman JC, Sickles R, Taubman P. Causes, Correlates and Consequences of Death among Older Adults: Some Methodological Approaches and Substantive Analyses. Boston, MA: Kluwer Academic Publishers; 1998. pp. 109–129. [Google Scholar]
- 27.Snyder S, Evans W. The effect of income on mortality: Evidence from the social security notch. Review of Economics and Statistics. 2006;88(3):482–495. [Google Scholar]
- 28.Handwerker EW. Unpublished doctoral dissertation. University of California; Berkeley: 2007. Empirical essays in the economics of aging. [Google Scholar]
- 29.Case A. Does money protect health status? Evidence from South African pensions. In: Wise DA, editor. Perspectives on the Economics of Aging. Chicago, IL: University of Chicago Press; 2004. pp. 287–312. [Google Scholar]
- 30.Jensen RT, Richter K. The health implications of social security failure: Evidence from the Russian pension crisis. Journal of Public Economics. 2003;88:209–236. [Google Scholar]
- 31.Feng J, He L, Sato H. Public Pension and Household Saving: Evidence from China. Bank of Finland, Institute for Economies in Transition; 2009. BOTIT Discussion Papers, No 2009/02. [Google Scholar]
- 32.Norström T, Palme J. Public pension institutions and old-age mortality in a comparative perspective. International Journal of Social Welfare. 2010;19:s121–s130. [Google Scholar]
- 33.Andersson K, Petzold MG, Sonesson C, Lonnroth K, Carlsten A. Do policy changes in the pharmaceutical reimbursement schedule affect drug expenditures? Interrupted time series analysis of cost, volume and cost per volume trends in Sweden 1986–2002. Health Policy. 2006;79(2–3):231–243. doi: 10.1016/j.healthpol.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 34.French B, Heagerty PJ. Analysis of longitudinal data to evaluate a policy change. Statistics in Medicine. 2008;27(24):5005–5025. doi: 10.1002/sim.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cutler D, Meara E. Changes in the age distribution of mortality over the 20th century. In: Wise DA, editor. Perspectives on the Economics of Aging. Chicago, IL: University of Chicago Press; 2004. pp. 333–366. [Google Scholar]
- 36.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. Journal of the American Medical Association. 1999;281:61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 37.Manning WG, Mullahy J. Estimating log models: To transform or not to transform? Journal of Health Economics. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 38.CDC. Achievements in public health, 1900–1999: Decline in deaths from heart disease and stroke: United States, 1900–1999. MMWR. 1999;48:649–656. [PubMed] [Google Scholar]
- 39.National Center for Health Statistics. Chartbook for the conference on the decline in coronary heart disease mortality. U.S. Department of Health, Education, and Welfare; 1978. [accessed 12 December 2010.]. www.cdc.gov/nchs/data/misc/corltrtacc.pdf. [Google Scholar]
- 40.Card D, Dobkin C, Maestas N. Does Medicare save lives? The Quarterly Journal of Economics. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaplan GA, Ranjit N, Burgard SA. Lifting gates, lengthening lives: Did civil rights policies improve the health of African American women in the 1960s and 1970s? In: Schoeni RF, House JS, Kaplan GA, Pollack H, editors. Making Americans Healthier. New York: Russell Sage Foundation; 2008. pp. 145–169. [Google Scholar]