Abstract
In a mass casualty situation due to chemical, biological, radiological, or nuclear (CBRN) event, triage is absolutely required for categorizing the casualties in accordance with medical care priorities. Dealing with a CBRN event always starts at the local level. Even before the detection and analysis of agents can be undertaken, zoning, triage, decontamination, and treatment should be initiated promptly. While applying the triage system, the available medical resources and maximal utilization of medical assets should be taken into consideration by experienced triage officers who are most familiar with the natural course of the injury presented and have detailed information on medical assets. There are several triage systems that can be applied to CBRN casualties. With no one standardized system globally or nationally available, it is important for deploying a triage and decontamination system which is easy to follow and flexible to the available medical resources, casualty number, and severity of injury.
Keywords: Chemical, biological, radiological, or nuclear event, casualty, treatment
When a chemical, biological, radiological, or nuclear (CBRN) event occurs, life or death often is determined within the first few minutes of its onset. The threat of CBRN terrorism shows that we must be prepared for these threats at all levels. The medical knowledge and expertise of CBRN responders can make a critical difference in CBRN disasters with respect to the mortality, morbidity, and social consequences.[2]
In 1984, the release of toxic methylisocyanate gas had occurred suddenly and without warning from the union carbide plant in Bhopal, the capital city of Madhya Pradesh. This was one of the world's worst industrial disasters which occurred in the early morning hours of December 3, 1984 in India. This disaster had created thousands of casualties thereby overwhelming local, health and medical resources.[3] The complexity of the Bhopal crisis was underscored by the severe mortality and morbidity as well as its occurrence in a developing nation that had little experience in dealing with chemical disasters. The disaster exposed serious deficiencies in preparedness and major problems of coordination.[4,5] In that catastrophic situation, however, an appropriate triage may have helped in the better utilization of the available medical resources to meet the needs. Despite this knowledge, specific expertise, education, and training of CBRN responders working in the field of hazardous materials (hazmat) are not well organized probably due to the lack of standardization, availability of necessary protocols, training programs, and international standards.[6–10]
Chemical, Biological, Radiological, or Nuclear Challenge
CBRN emergency can occur as a result of industrial disaster, occupational exposure, natural catastrophe, warfare, or acts of terrorism.[3] CBRN incidents present different challenges for all responders, necessitating the rapid decontamination and treatment of a significant numbers of casualties while taking critical measures to ensure the well-being of the personnel managing the incident.
The detection is part of a triplet of actions: (1) detection, (2) identification, and (3) monitoring following a CBRN incidence. The non-expert responder can use simple, pre-tuned devices for detection, such as an explosion danger meter, to detect the presence of a gas that could explode. Other pre-tuned devices available include a dose-rate meter, which can be used to detect the presence of nuclear agents. The ability of devices to detect all CBRN agents is an illusion. Therefore, it is essential to identify which variables should be detected and organize accordingly the Personal Protective Equipment (PPE), Chemical, Biological and Radiological Detection, Identification and Monitoring Equipment (for personnel, boundary monitoring and analysis).[11]
Decontamination Considerations
Some CBRN situations may require unique application of decontamination principles, procedures, and methods. These considerations should take into account command, control, communications, and planning capabilities required for decontamination of strategically significant areas/terrain or facilities, to include standing up/deactivating a task force, selecting and defining joint decontamination operations sites, and establishing the manning allocation of initial headquarters required by decontamination operation missions.
Patient decontamination reduces the threat of contamination-related injury to health service support (HSS) personnel and patients. Patient decontamination will have to be accomplished as the operation and patient load allows. Under most CBRN circumstances, delaying treatment or stabilization of the patient for decontamination should not put the patient at additional risk. Trained and qualified triage personnel should determine priority of treatment and decontamination. In addition, the various decision-making activities related to decontamination must be executed in a flexible and impromptu manner, depending on the victim's general state, the physical nature of the agent (gas, aerosol, droplet, splash, liquid, powder, etc.), the decontamination capabilities of the community, as well as the season, weather conditions, and other factors.[12]
The principles of decontamination are:
-
a)
decontaminate as soon as possible;
-
b)
decontaminate by priority;
-
c)
decontaminate only what is necessary;
-
d)
decontaminate as far forward as possible.
Responding to a Chemical, Biological, Radiological, or Nuclear Event
After a CBRN event, hospitals and emergency departments may have only enough resources available for patients who present relatively early after an event. Resource-allocation decisions will need to be made until additional resources become available. This means that some patients will receive treatment and others will not. The only option is to make hard resource-allocation decisions with appropriate field triage.[13]
Scene management
The scene should be isolated to mitigate consequences. Effective scene management is required to control access to and from the incident scene, control movement of contaminated victims, provide safe working methods for responders, and contain the release of any substances.
Once first responders approach and arrive at the scene, the following actions will need to be initiated:
-
a)
approach scene with caution and upwind;
-
b)
carry out scene assessment;
-
c)
establish incident command (each responding agency);
-
d)
recognize signs and indicators of CBRN incidents;
-
e)
determine whether CBRN or hazardous material incident;
-
f)
estimate the number of casualties/victims;
-
g)
estimate resource requirements;
-
h)
carry out primary triage, decontamination, secondary triage, medical care, and transport; and
-
i)
consider specialist advice/resource requirements
CBRN casualty management zones
A CBRN incident site will have three areas. Especially when responding to a chemical accident, one of the first things responders should do is to establish a clean treatment area, at least 300 yards upwind of the contaminated area. The clean treatment area is referred to as the cold zone, while the contaminated area is called the hot zone. Separating the hot and cold zones is the warm zone where decontamination occurs. The warm zone should be several hundred yards upwind from the contamination and at least 50 yards from the cold zone. All responders must leave the hot zone via specially designated pathways into the warm zone where they will be decontaminated.[14,15]
The hot line separating the hot zone from the cold zone is an arbitrarily established line that demarcates the area of liquid-agent contamination from an area that is liquid-agent free. Once established, it should be clearly marked using engineer tape or another marker to insure that liquid contamination or a person with potential liquid contamination does not cross into the clean area. This might necessitate the use of concertina wire or armed guards. The only entrance to the clean treatment area is through the decontamination stations.
When the medical facility is set up in a clean area (no liquid contamination), the ground behind the hot line is clean except the holding area for contaminated casualties waiting to be evacuated and the routes traversed by the contaminated evacuation vehicles; these should be far to the side of the contaminated triage and treatment areas. In other circumstances, the clean treatment area will be an oasis surrounded by the hot line.
No medical care is provided during this time or during the time spent waiting to begin the decontamination process. Therefore, before leaving the emergency care area, the patient must be stabilized to an extent that his condition will not deteriorate during this time. In a contaminated environment, emergency care is given by personnel in the highest level of mission-oriented protective posture, whose capabilities are limited by their protective gear. After receiving emergency care, a casualty must go through the decontamination station before receiving more definitive care in a clean environment. Decontamination takes 10–20 minutes.[16]
Personal protective equipment
All responders must take appropriate measures to protect themselves before entering the contaminated area. Use of PPE[17] to protect airway, skin, and eyes is an indispensable component of emergency response. Limitations to the use of PPE are restriction of physical activity, dehydration, heat-related illness, and psychological effect. To avoid this, emergency personnel should be trained to use PPE appropriately.
Level A PPE denotes fully encapsulated suit, with over-gloves and overboots integrated into the suit. Respiratory protection is a self-contained breathing apparatus. Level Aprotection is required for entry into an unknown hazardous environment.
Level B PPE denotes a hooded suit, double gloves, overboots, and a self-contained breathing apparatus, and may be used for decontamination procedures for an unknown substance and for entry into hot zones where the agent is not caustic.
Level C PPE is similar to Level B, but uses an air-purifying respirator instead of a self-contained breathing apparatus. Level C PPE can be used only after the hazardous substance has been identified, and upon verification of adequate oxygen in the environment.
Hazard monitoring strategies
Monitoring the time of the staff in PPE triaging is important. The time when each team member is completely donned in his or her PPE is written on the back of his or her PPE suit. This gives the safety officers and other team members an opportunity to help identify times for changing out staff. Time limitations for staff to be in PPE performing triage or decontamination depend on or may change due to the level of PPE, weather conditions, and/or response of staff to the stress level of the event.
Each team is responsible for monitoring the condition of their fellow team member. This allows the team to identify when one member may be having physical problems not necessarily related to the time in PPE. By observing the eyes of the team member in PPE, one can identify the onset of problems and the need to request a replacement triage team.
Mass Casualty Triage
In a mass casualty incident response, several organizations may be augmented by extraordinary measures in order to maintain an effective, suitable, and sustainable emergency response. By definition, such events have the potential to rapidly overwhelm – or threaten to exceed – the local capacity available to respond, even with the implementation of major incident plans.[18]
Saving lives is the top priority of all responding agencies. Contamination of victims/casualties must be considered as part of the initial assessment for a CBRN event. Effective methods for rescue, decontamination, and medical treatment must be provided. The provision of timely warnings and/or evacuation of the public, where appropriate, must be initiated, which may also contribute to saving lives by reducing the risk of exposure.
In most mass casualty situations, the number of patients and the severity of their injuries exceed the capability of the facility and staff, and patients sustaining major injuries who have the greatest chance of survival with the least expenditure of time, equipment, supplies, and personnel must be managed first. Triage is the most important mission of any disaster medical response, regardless of the nature of the mass casualty incident. The basic concept of conventional triage is to do the greatest good for the individual patient. The objective of disaster triage (field triage) is to do the greatest good for the greatest number of people.
Origin of triage
Triage comes from the French verb “trier”, which means “to sort”. It evolved, perhaps as early as Napoleon's time, as a technique for assigning priorities for treatment of the injured when resources were limited. The principle of triage implies making the most efficient use of available resources.
Why triage?
There are three major reasons why triage is beneficial in the disaster response.[19]
-
a)
Triage separates out those who need rapid medical care to save life or limb.
-
b)
By separating out the minor injuries, triage reduces the urgent burden on medical facilities and organizations. On average, only 10–15% of disaster casualties are serious enough to require overnight hospitalization.
-
c)
By providing for the equitable and rational distribution of casualties among the available hospitals, triage reduces the burden on each to a manageable level, often even to “non-disaster” levels.
CBRN Casualties Triage
The medical management of casualties resulting from exposure to biological agents, toxins, chemical agents or radiation will require appropriate assessment and categorization. Triaging for decontamination in such patients may be necessary to move the casualties quickly and safely into the health care system. The casualties can be initially triaged into ambulatory and nonambulatory groups. Ambulatory casualties most often are classified as minor or delayed. However, even these casualties triaged as minor or delayed must be observed for worsening signs and symptoms. Immediately, decontaminating procedures have to be initiated for casualties who were closest to the point of chemical release, those with liquid contamination, and those who have severe signs or symptoms of chemical injury or severe conventional injuries. Victims may be classified as expectant when they have serious signs and symptoms after initial therapy or are unresponsive to antidotes. During suspected radiation hazard, responders should be provided rapid biological (ionizing radiation) dose estimating devices for the use in medical triage and diagnosis of potentially exposed casualties. Rapid assessment of potentially exposed individuals will reduce short- and long-term health effects. But during a biological attack, the first indication of a problem may be delayed with the appearance of casualties in which medical personnel are unable to differentiate natural disease epidemics from overt or covert enemy attacks. An exception to this aspect would be an attack with biological toxin(s) that might create an immediate and dramatic mass casualty situation. Onset of illness following exposure to toxic agents may range from few minutes to as long as 3 weeks. Some potential biological agents are transmissible among humans and may spread fast after the initial attack may become an important triage planning consideration.[19]
It is also important to move casualties triaged as unsalvageable/Expired/Black Tag,to a site that is not observed readily by the public or other casualties. The deceased have to be kept at this site until law enforcement officers have acquired available evidence and the living casualties have been moved into the health care facility after decontamination. Deceased casualties require a thorough decontamination before they are moved to the morgue or they are ready for release.[20]
Triage zones
In CBRN mass casualty incident, the site should be divided into zones/sectors and, in addition to the appointment of an overall triage officer, triage officers should be appointed for each of the identified zone. Field medical triage must be conducted at three levels:
-
1)
On-site triage (Level 1)
-
2)
Medical triage (Level 2)
-
3)
Evacuation triage (Level 3)
On-site triage hot zone (Level 1)
This is a rapid categorization of victims with potentially severe injuries needing immediate medical care “where they are lying” or at a triage site. Personnel are typically first responders from the local population or local emergency medical personnel. Patients are characterized as “acute” or “non-acute”. Simplified color coding may be done if resources permit:
acute = red; non-acute = green.
During the initial response phase, first responders can use the START protocol for the Primary Triage. “START” stands for Simple Triage and Rapid Treatment. The START protocol is intended to provide a simple technique to be used in conducting Primary Triage by the first rescuers arriving on scene. This will assist in quickly identifying those patients in need of immediate treatment and transportation. Triage takes priority over emergency treatment. All victims will need to be tagged. Emergency care administered by START teams is restricted to opening airways, controlling severe hemorrhage, and elevating patient's feet. Casualties will be tagged according to the seriousness of their conditions and placed into one of the following categories:[21]
-
a)
Immediate (critical) = red tag = Ventilations present after positioning the airway or ventilations are over 30 per minute or capillary refill greater than 2 seconds or no radial pulse or cannot follow simple command.
-
b)
Delayed (urgent) = yellow tag = Any patient not in the immediate or minor categories. These patients are generally non-ambulatory.
-
c)
Minor (ambulatory) = green tag = Any patient requiring medical attention who is not immediate or delayed and who is able to walk.
-
d)
Deceased (expired) = black tag = No ventilations present after the airway is opened.
Medical triage cold zone (Level 2)
Rapid categorization of victims at a casualty site by the most experienced medical personnel available to identify the level of medical care is needed. Personnel assigned to the treatment areas will perform a secondary exam and complete any required information on the triage tag. Emergency personnel are not required to follow the START protocol during secondary and subsequent triage. “The greatest good for the greatest number of people” has to be kept in mind. Knowledge of the medical consequences of various injuries (e.g., burn, blast, or crush injuries or exposure to chemical, biological, or nuclear weapons) is critical. Color coding may be used: Casualties who require immediate life-saving interventions (airway, breathing, circulation): Urgent. Casualties who do not require immediate life-saving interventions and for whom treatment can be delayed: Delayed. Casualties who are not expected to survive due to the severity of injuries complicated by the conditions and lack of resources: Expectant/Deceased. Individuals who require minimal or no medical care: Minor.[22]
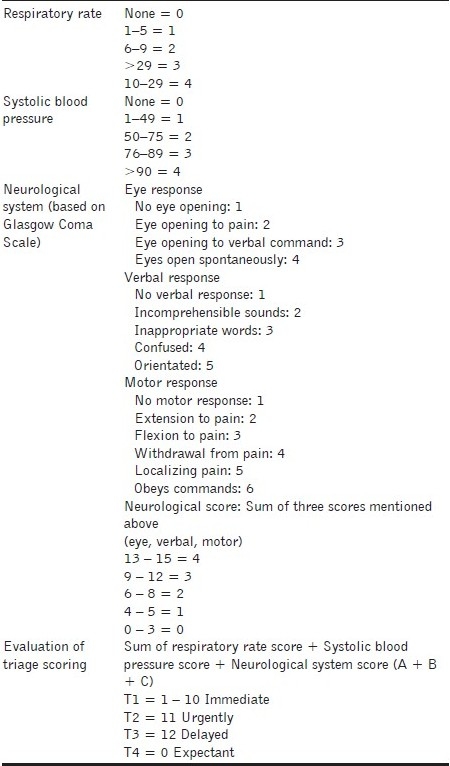
While applying triage, evaluation of signs and symptoms of chemical casualties is as significant as existing medical care possibilities such as medical assets and treatment facilities. It is difficult to standardize which signs and symptoms belong to which triage category. First of all, respiratory and circulatory findings are the most important criteria for such a determination. Respiration rate, systolic blood pressure, or pulse rate are also reported that have to be scored in accordance with degree of severity. Applying this triage system is apparently highly practical, but on the other hand, it seems time consuming for mass casualties who are in need of urgent medical care and first aid [Table 1].[22]
Table 1.
Another triage system proposed by NBC health care providers that may be used in the medical management of chemical casualties[1,22]
Radiological attack concerns
Effects of a radiological dispersion device (RDD), also known as a “dirty bomb,” would produce injuries from heat, force of the explosion, debris, and radiological dust. A dirty bomb consists of radioactive material attached to a conventional bomb. Upon confirming the initial fatalities after an explosion, the future radiation can be determined. This will be dependent upon the grade of radioactive material and the amount that has been released.[19]
The health risks of exposure to radioactive material are dependent upon several factors: the amount of radiation received, known as the dose, and the length of time over which the dose is received. Radiation generally penetrates the body when exposed to beta particles and gamma rays. Beta particles can be a hazard to both bare skin and eyes by causing burns. If ingested or inhaled, damage to internal organs will occur in its victims. Gamma radiation travels hundreds of meters in open air and penetrates most objects. Gamma rays penetrate tissue farther than do beta or alpha particles. Gamma rays can cause death. Alpha particles do not damage living tissue when outside the body; however, when alpha emitting atoms are inhaled or swallowed, they especially are damaging because they transfer relatively large amounts of ionizing energy to living cells. Damage to internal organs will occur in these victims.
First responders are reminded to utilize time, distance, and shielding (TDS) in order to reduce or eliminate the exposure of radiation. Emergency managers must enforce this safety measure with their personnel upon their arrival to the scene. Another possible threat in responding to a dirty bomb incident is the issue of a secondary explosive device against first responders
The “RTR” system (comprising Radiation-specific TRiage, TReatment, TRansport sites) is designed to support medical care following a nuclear incident. Its purpose is to characterize, organize, and efficiently deploy appropriate material and personnel assets as close as physically possible to various categories of victims, while preserving the safety of responders. The RTR system is not a medical triage system for individual patients. After an incident is characterized and safe perimeters are established, RTR sites should be determined in real-time, which are based on the extent of destruction, environmental factors, residual radiation, available infrastructure, and transportation routes. Such RTR sites are divided into three types depending on their physical/situational relationship to the incident. The RTR1 sites are near the epicenter with residual radiation and include victims with blast injuries and other major traumatic injuries including radiation exposure; RTR2 sites are situated in relationship to the plume with varying amounts of residual radiation present, with most victims being ambulatory; and RTR3 sites are collection and transport sites with minimal or no radiation present or exposure risk and a victim population with a potential variety of injuries or radiation exposures.[18]
Biological attack concerns
Decontamination of personnel and equipment after a biological warfare attack is a lesser concern than after a chemical warfare attack because most biological warfare agents are not dermally active (the trichothecene mycotoxins are an exception). Still, decontamination remains an effective way to decrease the spread of infection from potential secondary aerosolization. Three basic methods of decontamination are physical removal, chemical deactivation, and biological deactivation of the agent. Biological deactivation has not been developed to the point of being practical.
Chemical attack concerns
CBRN mass casualty situations are normally chaotic. Victims are in various stages of pain and distress [Table 2]. Casualties may have single or multiple injuries, or may have conventional injuries which are complicated by CBRN exposure (such as in a toxic spill or nuclear power plant accident). Casualties will range in age from infants to geriatric patients. Parents and loved ones may not want to be separated from the victim, even to permit the provision of medical care. Severity of medical conditions will vary from relatively minor injuries to severe, life-threatening trauma. Medical care provided may be complicated due to pre-existing medical conditions (disease, injury, or disability). New casualties will be arriving before the patients already on hand are treated. There may be personnel who are just dazed and wandering throughout the area disrupting operations. There may be uninjured persons looking for a family member, friend, or coworker; their search may be disruptive to the ongoing medical operation.[1,23]
Table 2.
A summary of physical characteristics of nerve and blister agents exposures in a triage procedure[24]
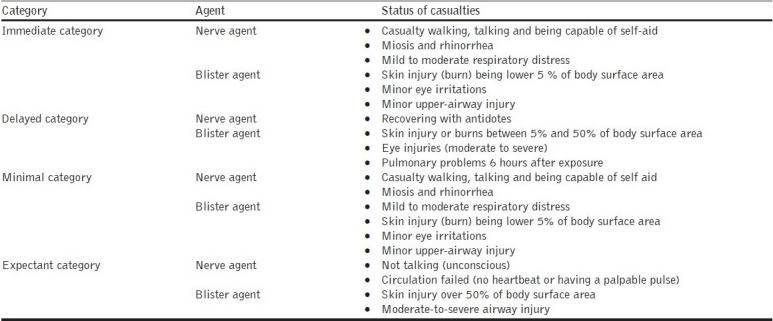
Chemicals are usually introduced into the body by inhalation, absorption, ingestion, or inoculation. They can be rapidly acting and have immediate or delayed effects [Table 2]. Only a few chemical agents have effective antidotes and the most important life-saving procedure available is to extract the casualty to a safe environment. Immediate administration of specific antidotes can, for some agents, be life-saving (e.g., atropine, oximes, and anticonvulsants in the case of nerve agents). Care of casualties exposed to chemical hazards requires rapid transfer to a safe atmosphere, appropriate antidotes, and attention to the ABCs of trauma care prior to and during decontamination.
It should be emphasized once again that triage be performed at every echelon of medical care, preferably several times, because the health status of some chemical casualties categorized as “delayed” may change within a short time and develop unanticipated life-threatening conditions like severe bleeding. Demand to medical goods for chemical casualties may exceed beyond the current resources. Delaying medical care for casualties who are categorized into “delayed” group may not change or affect adversely the outcome of progress. Therefore, taking basic life support measures for this triage category and then providing the discharge to treatment centers can be beneficial for other chemical casualties with severe injuries in immediate category to improve the survival rate.[14]
Monitoring litter decontamination area
There are two stations in this area, the clothing removal station and the skin decontamination station. At the clothing removal station (litter), two people work together, one on each side of the litter, to (in order) decontaminate the mask and hood, remove the hood (but leave mask in place), decontaminate the casualty's mask and area around the mask, remove the field medical card, remove gross contamination from the casualty's protective garment, cut and remove the protective garment jacket, cut and remove the protective garment trousers, remove outer gloves, remove the overboots and boots, remove inner clothing and underwear (in the same order and using the same procedures as with the protective garments), and check for contamination. At this time, the nude patient is transferred to the skin decontamination litter using a three-person roll lift.[25]
During clothing removal, the aidman removes tourniquets after placing a new one an inch or so higher and cuts away bandages and irrigates wounds (replacing the bandage only if bleeding recurs). He also thoroughly decontaminates splints, but does not remove them. On the skin decontamination litter, spot decontamination (only) is done on areas of potential contamination. These include the neck, lower face, and wrists, and also on areas under breaks in the protective ensemble, including around wound sites. After final monitoring for contamination, the casualty is carried on the litter to the shuffle pit and there is moved to a clean litter provided by a team from the clean side of the hot line. The mask is removed further upwind, at the entrance to the clean treatment area.
Monitoring the ambulatory decontamination area
A member of the decontamination team might help the walking patient or walking patients might help each other to remove their garments. The steps in this procedure are to drop the load bearing equipment, decontaminate and remove the hood, decontaminate the mask and surrounding skin, place the field medical card in a plastic bag, remove all gross contamination from the overgarment, remove the overgarment jacket, remove the rubber gloves, remove the overboots, remove overgarment trousers, remove cotton glove liners, check the battledress uniform (BDU) or any other garment and surrounding skin for contamination (and decontaminate any spots of contamination found), and lift the mask (while the casualty has his breath held and eyes closed), wipe the face, and replace, seal, and clear the mask. During this procedure, the medic will change tourniquets and remove bandages as described in the previous section. The casualty, dressed in his BDUs (including mask), thoroughly dusts his boots as he proceeds through the shuffle pit (the hot line) to the clean treatment area. The mask is removed further upwind, at the entrance to the clean treatment area. If because of the nature of his wounds his BDU is removed, the casualty becomes a litter patient.[25]
Evacuation triage-loading zone (Level 3)
Level 3 triage assigns priorities to disaster victims for transfer to medical facilities. The goal is appropriate evacuation (by land or air) of victims according to the severity of injury and available resources. Same medical personnel as in Level 2 triage. Evacuation can be useful in a disaster. There are several indications for evacuation in a disaster:
-
a)
to decompress the disaster area;
-
b)
to improve care for most critical casualties by removal to off-site medical facilities; and
-
c)
to provide specialized care for specific casualties, such as those with burns and crush injuries
There are also several reasons to delay or defer evacuation of some casualties. These include:
-
a)
contaminated casualties;
-
b)
casualties with transmissible diseases; and
-
c)
unstable casualties
The following types of information the triage officer must have will absolutely facilitate the procedures [Table 3].
Table 3.
Information for the triage officer[1]

Comparing mass casualty triage systems
Several primary and secondary triage tools have been developed, including START, JumpSTART (pediatrics), Care Flight Triage, Triage Sieve, Sort, Assess, Life Saving Interventions, Treatment and/or Transport (SALT) Secondary Assessment of Victim Endpoint (SAVE) Move, Assess, Sort, Send (MASS) Sacco Triage Method (STM), and Pediatric Triage Tape [Figure 1]. Id-me! (I – Immediate, D – Delayed, M – Minimum, E – Expectant) is a simple mnemonic for sorting patients during triage of mass casualties, and it is used effectively in the SALT Triage model. Evidence to support the use of one triage algorithm over another is limited, and the development of effective triage protocols is an important research priority. The most widely recognized mass casualty triage algorithms in use today are not evidence-based, and no studies directly address these issues in the mass casualty setting. Furthermore, no studies have evaluated existing mass casualty triage algorithms regarding ease of use, reliability, and validity, when biological, chemical, or radiological agents are introduced. Currently, the lack of a standardized mass casualty triage system that is well validated, reliable, and uniformly accepted, and it remains an important gap.[26]
Figure 1.
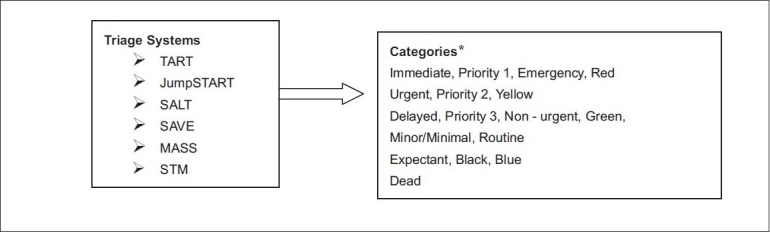
Triage systems sort patients into categories
*Note: This is a representative but not complete list of the kinds of categories used in various triage systems; each bullet lists the approximate equivalent categories used by various systems; see each system for the exact meaning of the categories used in that system; systems typically have four or five categories, some named by color only; the category “Dead” does not appear in all systems; these systems and categories were created typically for trauma triage or critical care assessments, not specifically incidents involving radiation or trauma plus radiation
All accepted methods of triage are based on the principles of the START plan,[27] and all are subject to under- and over-triage.[28] An undertriage rate of 5% is considered acceptable;[29] anything higher may lead to unnecessary morbidity and mortality in severely injured but potentially salvageable patients. An overtriage rate of about 50% is acceptable[30] to minimize the number of patients who are undertriaged.
One of the practical triaging of patients is categorizing into one of three groups: (1) immediate care, (2) delayed care, and (3) unsalvageable. Numbers, colors, or symbols may be used to denote the different triage categories. For example, red (priority 1) tags are attached to patients allocated to the immediate-care group, yellow tags (priority 2) to the delayed-care group, and black tags to unsalvageable patients. In Israel, they have added the blue tag to identify children and a gray one to identify patients with a combined injury (induced, for example, by chemical and conventional weapons). Some teams prefer a site-based categorization.[31]
No matter what the method is, the signs need to be appropriate and clear. According to Simon Ward working in Guys’ and St. Thomas Hospital, chemical casualties are categorized into three priority (P) groups.[32]
-
a)
P1: Those who require resuscitation during decontamination in a stretcher facility
-
b)
P2: Those whose treatment may be delayed until decontamination ends in a stretcher facility
-
c)
P3: Those who have minor injuries and may walk spontaneously.
Categories of triage commonly accepted to be used in casualties injured with weapons of mass destruction:
-
a)
T1 Immediate: Casualties who require life saving care within a short time
-
b)
T2 Delayed: Casualties who require hospitalization and prolonged surgery
-
c)
T3 Minimal: Casualties who have minor injuries
-
d)
T4 Expectant: Casualties who would not survive with optimal medical care
Triage tags
Triage tags are commonly used for large-scale disasters but their small size makes it difficult to read the information they contain or to write new information on tags while wearing protective gear. Also, paper tags are not suitable for wet decontamination. In Israel, plastic triage tags are used in instances of chemical exposure. These plastic tags are like bingo cards, and information can be recorded by punching holes in them using a finger. Some hospitals in Japan have developed paper hospital triage tags that have a space for recording NBC contamination and decontamination information, and a system using colored ribbons also for triage has been reported.
Direct, visible, red marking on the victim's body is a good way to achieve this. It is also simple and less expensive. The use of plastic triage tags, currently employed in Israel for chemical exposures, has been suggested to be a simpler but a more expensive system. The system using triage ribbons probably takes longer and is more difficult considering the practical difficulties of tying ribbons while wearing thick butyl rubber gloves. Other options include the use of color tape or Velcro bands or the Simple Triage and Rapid Decontamination of Mass Casualties with Colored Clothes Pegs (STARDOMCCP). Color tapes also would need to be cut and Velcro bands would be more expensive than CCPs.[12]
Medical Emergency Triage Tags (METTAG) have historically been used worldwide in MCIs ranging from automobile and aircraft accidents involving several victims, to large-scale terrorism incidents. With rising concerns of how to effectively handle triage situations involving hazmat, terrorism, and possible use of weapons of mass destruction, the need for an alternative triage tag has emerged.
The CB-100 triage tag was designed to meet the needs of the first responders to the growing complexities and dangers of the modern triage environment. Constructed of the same high-density water-resistant synthetic paper and printed using the same special thermal printing process as the Original MT-137,the front of the CB-100 has all of the key information fields needed to quickly note the triage patient's status and to fill in additional patient assessment and tracking information as time permits. The back of the CB-100 provides room for additional notes about the patient, if needed. Each section of the CB-100 has a unique barcode serial number for tracking and monitoring the victim's triage process. The CB-100 can be used with standard triage systems like the START method or with the A-E Triage System that is specifically designed to handle hazmat and terrorist incidents.[33]
Monitoring After CBRN Response
Once the event has ended and the patients are within the health care system, the process of returning to normal function begins. Scientifically and logistically, this can be the most difficult aspect of the incident. Numerous areas, equipment, vehicles, and other items may be left contaminated. Identifying the contaminating chemical or chemicals, the preferred methods for decontamination, the chemical's persistency on various surfaces, and the chemical's effect on water and food sources requires considerable review and expertise.[20]
The decontamination area must be cleaned, and contaminated clothing and equipment used during the decontamination process must be cleaned or disposed of appropriately. Final disposition of contaminated articles is in accordance with previously established arrangements and the overall community hazardous waste plan.
Patients’ valuables are an important issue. During the patient decontamination process, rings, watches, wallets, purses, and other items such as hearing aids are removed and placed in marked plastic bags. A security person may be the most appropriate person to ensure that these items are stored in a secure manner. To avoid legal difficulties, follow chain-of-custody procedures to ensure that these valuables are not disturbed. As soon as it is practical, check these items for contamination and clean them as necessary for return to their owners.
Conclusion
The “Ideal” Triage Tool should have the ability to process many victims with accuracy by the first responders responding to the scene while patients are triaged in the field and hazmat handles decontamination in the field. It should also be simple, objective, based on physiological parameters, easy to remember, easy to use, and evidence-based. No patient group should receive special consideration based on emotion or other parameter. Even with limited data, the sickest patients should be shifted with Emergency Medical Services (EMS) already sorted and tagged, decontaminated, partially treated with hospitals “only” needing to care for them.
But what really happens following a CBRN incident in the scene is usually in a “Chaotic” phase for 15–30 minutes. There will be no emergency medical response, no scene leader, victims requiring different levels of triage and decontamination cannot be easily and quickly identified. The coding employed for triage may not be easily understood by first responders, they may be hindered by their protective gear. The transition from triage to decontamination may not be smooth, hampering the efficiency of decontamination. Around 80% or more of minimally injured casualties may self-transport to the closest medical facilities, with no triage, decontamination, or medical intervention.
Disaster triage occurs at various points along the continuum of care and is classified accordingly. Triage involves decisions related to allocating critical care resources. Currently standard triage protocols are lacking. Effective triage requires significant planning and an infrastructure that can support the process during a disaster. A strong ethical framework is necessary to guide the development and implementation of a triage protocol.
The above mentioned procedures for triage and decontamination are merely guidelines. Both triage and decontamination should be conducted in a flexible manner depending on the medical resources available, patient counts, and distribution of severity. Thus, the future research should be directed at triage as a necessity, and the development of a practical, universal, triage algorithm that incorporates requirements for decontamination or special precautions for infectious agents would facilitate a more organized mass casualty medical response during a CBRN incident.[27,34]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kenar L, Eryιlmaz M. Evaluations on Triage Applications for Chemical Casualties in Chemically Contaminated Area. JAEM. 2009;8:42. [Google Scholar]
- 2.Van der Woude I, de Cock JS, Bierens JJ, Christiaanse JC. TAP CBRN Preparedness: Knowledge, training, and networks. Prehosp Disaster Med. 2008;23:s65–9. doi: 10.1017/s1049023x00021270. [DOI] [PubMed] [Google Scholar]
- 3.Chakravorty N, Jain RK, Agarwal RC. Bhopal Gas Tragedy - Preparedness and Management of Chemical Disaster. Ind J Trauma Anaesth Crit Care. 2007;8:566–72. [Google Scholar]
- 4.Ember LR. FBI takes lead in developing counterterrorism effort. Chem Eng News. 1996;4:10–6. [Google Scholar]
- 5.Department of Defense, Department of Energy. Joint Report to Congress: Preparedness and Response to a Nuclear, Radiological, Biological, or Chemical Terrorist Attack. Washington DC: Department of Defense, Department of Energy; 1996. [Google Scholar]
- 6.Niska RW, Burt CW. Bioterrorism and mass casualty preparedness in hospitals: United States, 2003. Adv Data. 2005;364:1–14. [PubMed] [Google Scholar]
- 7.Jasper E, Miller M, Sweeney B, Berg D, Feuer E, Reganato D. Preparedness of hospitals to respond to a radiological terrorism event as assessed by a fullscale exercise. J Public Health Manag Pract. 2005;11:s11–6. doi: 10.1097/00124784-200511001-00003. [DOI] [PubMed] [Google Scholar]
- 8.Ciraulo DL, Frykberg ER, Feliciano DV, Knuth TE, Richart CM, Westmoreland CD, et al. A survey assessment of the level of preparedness for domestic terrorism and mass casualty incidents among Eastern Association for the Surgery of Trauma members. J Trauma. 2004;56:10339. doi: 10.1097/01.ta.0000127771.06138.7d. [DOI] [PubMed] [Google Scholar]
- 9.Treat KN, Williams JM, Furbee PM, Manley WG, Russell FK, Stamper CD., Jr Hospital preparedness for weapons of mass destruction incidents: An initial assessment. Ann Emerg Med. 2001;38:562–5. doi: 10.1067/mem.2001.118009. [DOI] [PubMed] [Google Scholar]
- 10.Young CF, Persell DJ. Biological, chemical, and nuclear terrorism readiness: Major concerns and preparedness of future nurses. Disaster Manag Response. 2004;2:109–14. doi: 10.1016/j.dmr.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 11.van der Woude I, de Cock JS, Bierens JJ, Christiaanse JC. TAP CBRN preparedness: Knowledge, Training and Networks. [Last accessed on 2010 Jun 19];Prehosp Disaster Med. 2008 23:s65–9. doi: 10.1017/s1049023x00021270. Available from: http://pdm.medicine.wisc.edu . [DOI] [PubMed] [Google Scholar]
- 12.Okumura T, Kondo H, Nagayama H, Makino T, Yoshioka T, Yamamoto Y. Simple triage and rapid decontamination of mass casualties with the colored clothes pegs (STARDOM-CCP) system against chemical releases. Prehosp Disaster Med. 2007;22:233–6. doi: 10.1017/s1049023x00004738. [DOI] [PubMed] [Google Scholar]
- 13.Iserson KV, Sanders AB, Mathieu D. Ethics in Emergency Medicine. 2nd ed. Tucson, AZ: Galen Press, Ltd; 1995. [Google Scholar]
- 14.Briggs Susan M, Cronin Michael. The ABCs of Disaster Medical Response Manual for Providers 2nd ed. International Trauma and Disaster Institute. [Cited in 2010]. Available from: http://www.hospitalesseguros.crid or cr/pdf/abc_2nd_edition.pdf .
- 15.Frederick R. Management of Chemical Warfare Agent Casualties: A Handbook for Emergency Medical Services. Bel Air, MD: HB Publishing; 1995. [Cited in 2007]. Available from: http://www.ijtacc.org/Feb . [Google Scholar]
- 16.Brigadier General Russ Zajtchuk, Ronald F. Bellamy Specialty. In: Sidell FR, Takafuji ET, Franz DR, editors. Medical aspects of Chemical and Biological Warfare. Textbook of Military Medicine. Vol. 3. Washington, DC: The Office of The Surgeon General at TMM Publications; 1989. pp. 351–9. [Google Scholar]
- 17.Varela J. Hazardous Materials Handbook for Emergency Responders. New York: Van Nostrand Reinhold; 1996. [Google Scholar]
- 18.Mass Casualties Incidents. A Framework for Planning NHS Scotland Strategic Guidance for NHS Boards in Scotland. 2009 May [Google Scholar]
- 19.Hrdina CM, Coleman CN, Bogucki S, Bader JL, Hayhurst RE, Forsha JD, et al. The “RTR” medical response system for nuclear and radiological mass-casualty incidents: A functional TRiage-TReatment-TRansport medical response model. Prehosp Disaster Med. 2009;24:167–78. doi: 10.1017/s1049023x00006774. [DOI] [PubMed] [Google Scholar]
- 20.Gum Robert M. Robert M Gum CBRNE - Chemical Warfare Mass Casualty Management. [Updated on 2009 Jan 27]; Available from: http://www.emedicine.medscape.com . [Google Scholar]
- 21.EMS Response for a Mass Casualty. Kootenai County M.C.I.Plan Protocol #108. 2006 Mar 31; [Google Scholar]
- 22.James MR. Triage: Principles and Pressures. Eur J Trauma Emerg Surg. 2008;34:427–32. doi: 10.1007/s00068-008-8804-3. [DOI] [PubMed] [Google Scholar]
- 23.Appendix J. Mass Casualty Situations. J-1. FM 8-42. www.cdmha.org/toolkit/cdmha-rltk .
- 24.Russ Zajtchuk, Ronald F. Bellamy Specialty. In: Sidell FR, Takafuji ET, Franz DR, editors. Medical aspects of Chemical and Biological Warfare. Textbook of Military Medicine. Vol. 3. Washington, DC: The Office of The Surgeon General at TMM Publications; 1989. pp. 337–49. [Google Scholar]
- 25.Casualty Management. Medical Management of Casualties Handbook. 3rd ed. [last accessed on 1999 Aug]. Available from: http://www.fas.org/nuke/guide/usa/doctrine/army .
- 26.Jenkins JL, McCarthy ML, Sauer LM, Green GB, Stuart S, Thomas TL, et al. Mass-casualty triage: Time for an evidence-based approach. Prehosp Disaster Med. 2008;23:3–8. doi: 10.1017/s1049023x00005471. [DOI] [PubMed] [Google Scholar]
- 27.Meirav Mor, Yehezkel Waisman. Triage principles in Multiple Casualty Situations Involving Children. The Israeli Experience. pp. 1–19. www.pemdatabase.org/files/triage.pdf .
- 28.Kennedy K, Aghababian RV, Gans L, Lewis CP. Triage: Techniques and applications in decision-making. Ann Emerg Med. 1996;28:136–44. doi: 10.1016/s0196-0644(96)70053-7. [DOI] [PubMed] [Google Scholar]
- 29.Wesson DE, Scorpio R. Field triage: Help or hindrance? Can J Surg. 1992;35:19–21. [PubMed] [Google Scholar]
- 30.American College of Surgeons Committee on Trauma. Field categorization of trauma victims. Bull Am Coll Surg. 1986;71:17–21. [Google Scholar]
- 31.Meirav Mor, Yehezkel Waisman. Triage principles in Multiple Casualty Situations Involving Children - The Israeli Experience. [Last accessed on 2010 Jun 19]; Available from: http:// www.pemdatabase.org/files/triage.pdf . [Google Scholar]
- 32.Ward S, Murray V. Principles of the pre-hospital management of chemicals incidents. Prehospital Immediate Care. [Last accessed on 2010 Jun 19]. Available from: http://www.journalagent.com .
- 33.James M. Ryan Triage.Principles and Pressures European Journal of Trauma and Emergency Surgery Focus on Disaster Medicine. Eur J Trauma Emerg Surg. 2008;34:427–32. doi: 10.1007/s00068-008-8804-3. [DOI] [PubMed] [Google Scholar]
- 34.Tom Carey. DECON and CBRNE treatment of the masses: Can we be that ready? [Last acceesed on 2010 Mar 28]. Available from: http//www.tom@theklaxon.com .


