Abstract
Atopic asthma is a chronic disease of the airways that has taken on epidemic proportions in the industrialized world. The increase in asthma rates has been linked epidemiologically to the rapid disappearance of Helicobacter pylori, a bacterial pathogen that persistently colonizes the human stomach, from Western societies. In this study, we have utilized mouse models of allergic airway disease induced by ovalbumin or house dust mite allergen to experimentally examine a possible inverse correlation between H. pylori and asthma. H. pylori infection efficiently protected mice from airway hyperresponsiveness, tissue inflammation, and goblet cell metaplasia, which are hallmarks of asthma, and prevented allergen-induced pulmonary and bronchoalveolar infiltration with eosinophils, Th2 cells, and Th17 cells. Protection against asthma was most robust in mice infected neonatally and was abrogated by antibiotic eradication of H. pylori. Asthma protection was further associated with impaired maturation of lung-infiltrating dendritic cells and the accumulation of highly suppressive Tregs in the lungs. Systemic Treg depletion abolished asthma protection; conversely, the adoptive transfer of purified Treg populations was sufficient to transfer protection from infected donor mice to uninfected recipients. Our results thus provide experimental evidence for a beneficial effect of H. pylori colonization on the development of allergen-induced asthma.
Introduction
Atopic asthma is characterized by lung inflammation, airway hyperresponsiveness, and airway obstruction (1). The pulmonary infiltrates of asthmatic patients consist of eosinophils, mast cells, and activated Th2 and Th17 cells, which orchestrate allergen-specific immune responses (2). In recent decades, the incidence of asthma and associated allergic diseases has increased to epidemic proportions in developed countries, especially among children (3). The growing prevalence of asthma has been attributed to pollution and tobacco smoke (3) and to a lack of infectious stimuli arising from modern sanitary practices and the widespread use of antibiotics (4). The “hygiene hypothesis” postulates that early exposure to microbial antigens is essential for the normal maturation of the immune system and the prevention of allergic diseases (4); it was recently revisited by Blaser and Falkow (5), who propose that the loss of our ancestral indigenous microbiota, rather than a general decline in arbitrary childhood infections, is causally associated with the asthma epidemic. In experimental models of asthma, infection with microorganisms possessing strong immunomodulatory properties has been negatively associated with allergic airway disease (6, 7).
Several epidemiological studies have reported an inverse correlation between asthma incidence and chronic infection with the human gastric pathogen Helicobacter pylori (8–11), the causative agent of gastric ulcers, gastric lymphoma, and gastric adenocarcinoma. This association was strongest in young individuals with early-life asthma onset (9) and depended in part on the H. pylori virulence determinant CagA (8, 10). We have recently introduced a CagA+ H. pylori infection model that recapitulates the gastric preneoplastic histopathology of a subset of H. pylori–infected patients (12). In this model, mice that are experimentally infected during the neonatal period develop H. pylori–specific immunological tolerance and are protected against gastric immunopathology resulting from CagA+ infection in adults (12). Here, we have utilized models of allergic airway inflammation and hyperresponsiveness to examine a possible inverse association between H. pylori infection and asthma.
Results and Discussion
Experimental infection with H. pylori protects against allergic airway disease.
To experimentally test the effects of H. pylori on OVA-induced allergic airway disease, C57BL/6 mice were infected with H. pylori at either 6 days or 6 weeks of age (i.e., as neonates or adults), sensitized with alum-adjuvanted OVA, and challenged with aerosolized OVA 4 weeks later to induce asthma-like symptoms. Infection with H. pylori significantly reduced airway hyperresponsiveness as evidenced by decreased airway resistance following methacholine challenge (Figure 1A) and alleviated the peribronchiolar and perivascular inflammation and goblet cell metaplasia that are hallmarks of asthma (Figure 1, B and C). The infiltration of immune cells into the bronchoalveolar lavage fluid (BALF) as well as the increase of eosinophils and concomitant relative decrease of alveolar macrophages in BALF was largely prevented in infected mice (Figure 1, D–F). Finally, the secretion of IL-5 into the BALF and the pulmonary infiltration of Th2 and Th17 cells as detected by flow cytometric analysis of lung single cell preparations were diminished in infected animals (Figure 1G and Supplemental Figure 1; supplemental material available online with this article; doi: 10.1172/JCI45041DS1). Most indicators of asthma were more strongly reduced in neonatally infected than in adult-infected mice (Figure 1, A–G), suggesting a continuum of protection that is inversely correlated with age at the time of infection. Interestingly, antibiotic eradication therapy resulting in efficient killing of the bacteria after the sensitization phase of our protocol abrogated asthma protection (Figure 1, A–G). To rule out that asthma protection in infected mice is due to their defect in generating a primary allergen-specific immune response, we compared OVA-specific responses in infected and uninfected mice. All mice generated similar OVA-specific IgE titers and splenocyte recall responses (Supplemental Figure 2), indicating that the infection status does not affect the primary responses to allergen. To verify our results in another model of allergic airway disease, we alternatively utilized house dust mite (HDM) allergen for sensitization and intranasal challenge. HDM-sensitized/challenged mice showed robust airway responses similar to those of OVA-treated mice (Figure 1, H-M). As observed in the OVA model, neonatally infected mice were protected against HDM-induced airway hyperresponsiveness as assessed by methacholine challenge (Figure 1H) and exhibited significantly less peribronchiolar and perivascular inflammation and goblet cell metaplasia than uninfected controls (Figure 1, I and J). Their bronchoalveolar inflammation, eosinophilia, and IL-5 and IL-13 secretion were clearly reduced (Figure 1, K–M). Mice infected as adults did not benefit from H. pylori in the HDM model (Figure 1, H–M). In conclusion, we show here that infection with H. pylori, especially early in life, is protective against asthma in mouse models of the disease.
Figure 1. Experimentally induced asthma is alleviated by H. pylori infection.
Mice were orally infected as neonates (iN) or adults (iA) with H. pylori and sensitized with alum-adjuvanted OVA (A–G) or HDM (H–M) 4 and 6 weeks after infection along with an uninfected (uninf) group. 1 group of neonatally infected mice received antibiotic therapy between the first and second allergen doses. 2 weeks after the second sensitization, all mice (including a mock-sensitized control group [PBS]) were exposed to 3 consecutive daily doses of aerosolized OVA or intranasal HDM. (A, H) Airway hyperresponsiveness in response to increasing doses of methacholine and the highest dose of 100 mg/ml, respectively (upper and lower panels in A). (B, C, I, and J) Tissue inflammation and goblet cell metaplasia as assessed on H&E- and PAS-stained tissue sections. Representative micrographs are shown in B and I; inflammation and PAS scores are shown in C and J. Original magnification, ×100 (H&E); ×400 (PAS). (D and K) Total cells contained in 1 ml of BALF. (E) Relative representation of the indicated cell types in BALF. (F and L) Absolute numbers of eosinophils in 1 ml of BALF. (G and M) IL-5 and/or IL-13 secretion as assessed by cytometric bead array. *P < 0.05 and **P < 0.01 in comparison with uninfected, but allergen-treated, controls. All group data of methacholine measurements are presented as mean ± SEM. Total cell and eosinophil counts in BALF are presented for individual mice, with horizontal bars indicating group medians. Inflammation scores and PAS+ cells are represented by box and whisker plots, with horizontal bars representing medians and whisker ends indicating minimal and maximal values. Cytokine measurements and PCR results are presented as group mean ± SD.
H. pylori–mediated asthma protection is associated with increased pulmonary Treg infiltration and impaired DC maturation.
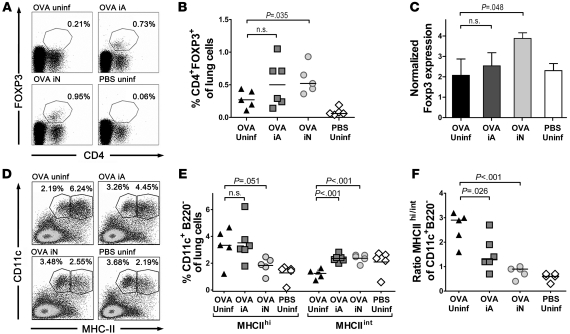
Multiple recent studies have highlighted a functional role of CD4+FoxP3+ Tregs in controlling allergic Th2 cell responses (13). To examine a role of Tregs in H. pylori–mediated asthma protection, we first assessed pulmonary FoxP3+ Treg infiltration in the OVA-induced asthma model. Neonatally infected mice exhibited higher numbers of pulmonary CD4+FoxP3+ Tregs than uninfected mice, whereas adult-infected mice showed an intermediate phenotype (Figure 2, A–C). Immunomagnetic isolation of pulmonary CD4+CD25+ Tregs from neonatally infected, OVA-challenged mice revealed that this Treg population has strong suppressive activity ex vivo (Supplemental Figure 3). Another characteristic feature of neonatally infected mice was their pulmonary infiltration by semimature DCs with low to intermediate MHCII expression, which are believed to induce peripheral T cell tolerance (14); in contrast, mature MHCIIhi DCs constituted the predominant DC population in asthmatic lungs of uninfected or adult-infected animals (Figure 2, D and E). Consequently, the MHCIIhi/ MHCIIint ratio was higher in the latter groups (Figure 2F). These results suggest a causal relationship between H. pylori–mediated asthma protection and lung infiltration by “tolerogenic” immune cell populations such as Tregs and semimature DCs.
Figure 2. Tregs and semimature DCs accumulate in the lungs of neonatally infected mice.
Groups of mice treated as described in Figure 1 were analyzed with respect to lung infiltration by FoxP3+ Tregs and CD11c+B220– DCs. (A and B) Representative scatter plots and quantification of CD4+FoxP3+ cells in lung preparations of 4–6 mice per group; percentages in A denote the fraction of CD4+FoxP3+ cells of all lung cells. (C) foxP3 expression of the mice shown in B, normalized to GAPDH. (D and E) Representative scatter plots and quantification of CD11c+B220– DCs expressing high and intermediate levels of MHCII; percentages in D denote the fractions of MHCIIhi and MHCIIint cells of all CD11c+B220– lung DCs. (F) Ratios of MHCIIhi/MHCIIint DCs as calculated per mouse. All group data of methacholine measurements are presented as mean ± SEM. Total cell and eosinophil counts in BALF are presented for individual mice, with horizontal bars indicating group medians. Inflammation scores and PAS+ cells are represented by box and whisker plots, with horizontal bars representing medians and whisker ends indicating minimal and maximal values. Cytokine measurements and PCR results are presented as group mean ± SD.
Asthma protection conferred by H. pylori infection is mediated by Tregs.
Two recent epidemiological studies have revealed an inverse association of asthma with seropositivity for the H. pylori immunodominant antigen CagA, implying that infection with CagA+ H. pylori strains is particularly beneficial with regard to asthma prevention (8, 10). The H. pylori strain used here harbors a cagA gene as well as the type IV secretion system (T4SS) required for CagA delivery to host cells (12). To determine whether CagA delivery is required for asthma protection, we first verified that H. pylori reisolates retain their ability to deliver CagA in vitro after prolonged coexistence with their murine hosts (Supplemental Figure 4A). We then infected neonatal mice with either wild-type H. pylori or an isogenic mutant lacking an essential component of the T4SS (ΔCagE). H. pylori ΔCagE–infected animals were protected at least as well as wild-type infected mice from OVA-induced asthma as determined by assessment of airway resistance, histopathology, and airway eosinophilia (Supplemental Figure 4, B–F), indicating that CagA delivery is not a prerequisite for asthma protection in this model.
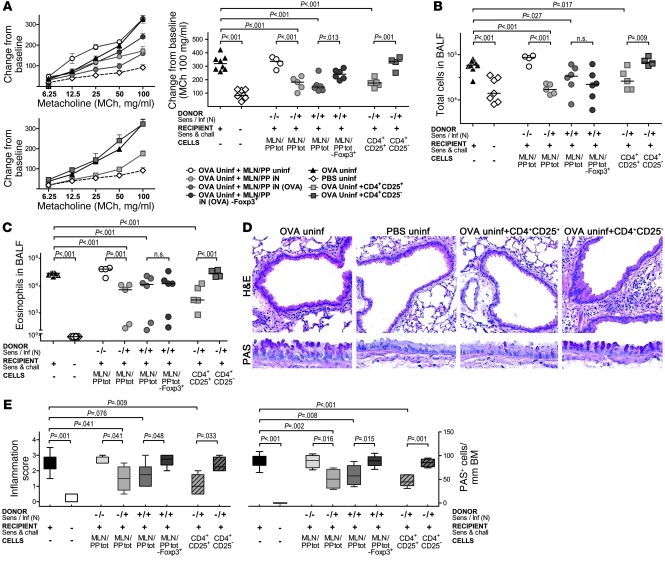
To determine whether the protection conferred by neonatal H. pylori infection depends on Tregs, we depleted Tregs by anti-CD25 mAb treatment during OVA challenge. This treatment was sufficient to largely abrogate protection (Supplemental Figure 4, B–F). We next tested to determine whether asthma protection can be adoptively transferred from infected donors to uninfected recipients using specific immune cell populations. We isolated mesenteric lymph node and Peyer patch (MLN/PP) cell populations from mice that had been infected as neonates and/or had been sensitized with OVA and systemically depleted of Tregs. Asthma protection was successfully conferred by adoptive transfer of 1 × 107 MLN/PP cells from neonatally infected, but not uninfected, donors as determined by methacholine challenge, histopathological analysis, and quantification of bronchoalveolar infiltration, eosinophilia, and IL-5 production; prior exposure of the donors to OVA was not a prerequisite for protection (Figure 3, A–E, and Supplemental Figure 5). In contrast, prior depletion of Tregs in the infected donors reduced protection (Figure 3, A–E). In line with this result, as few as 2.5 × 105 adoptively transferred, immunomagnetically purified, MLN/PP-derived CD4+CD25+ Tregs, but not CD4+CD25– conventional T cells, were sufficient to confer protection (Figure 3, A–E).
Figure 3. Asthma protection is conferred by Tregs.
Groups of mice were sensitized with OVA or PBS only prior to intravenously receiving unsorted (total [tot]) MLN/PP populations isolated from uninfected or neonatally infected and/or OVA-sensitized or Treg-depleted (–FoxP3+) donors. Tregs were depleted in foxP3-EGFP-DTR–transgenic donors by a single dose of diphtheria toxin 1 day prior to cell isolation; Treg-proficient donors were nontransgenic littermates. Additional recipients received 2.5 × 105 immunomagnetically isolated, MLN/PP-derived CD4+CD25+ Tregs or CD4+CD25– T cells (>85% purity each) from neonatally infected donors. All recipients as well as control groups were nebulized with OVA on days 2, 3, and 4 after adoptive transfer and sacrificed 2 days later. (A) Airway hyperresponsiveness in response to increasing doses of inhaled methacholine and the highest dose of 100 mg/ml, respectively. (B and C) Total cells and eosinophils contained in 1 ml of BALF. (D and E) Tissue inflammation and goblet cell metaplasia as assessed on H&E- and PAS-stained tissue sections. Micrographs of representative T cell recipients and controls are shown in D; inflammation and PAS scores are shown in E for all mice. Original magnification: ×100 (H&E); ×400 (PAS). All group data of methacholine measurements are presented as mean ± SEM. Total cell and eosinophil counts in BALF are presented for individual mice, with horizontal bars indicating group medians. Inflammation scores and PAS+ cells are represented by box and whisker plots, with horizontal bars representing medians and whisker ends indicating minimal and maximal values. Cytokine measurements and PCR results are presented as group mean ± SD.
In summary, we conclude that H. pylori prevents allergic airway disease in preclinical models; we attribute protection against asthma to the immunomodulatory properties of H. pylori based on the following observations. Protection is particularly evident in neonatally infected mice, which develop H. pylori–specific immunological tolerance mediated by long-lived, inducible Tregs (12). Tregs with suppressive activity accumulate in the lungs of neonatally infected, protected mice. Their depletion abrogates protection, and the adoptive transfer of purified Tregs alone is sufficient to confer protection. Based on our finding of semimature DC infiltration into the lungs of protected mice, we speculate that neonatally induced Tregs retain lung-infiltrating DCs in a semimature state. An analogous mechanism was proposed recently by Onishi et al., who found that FoxP3+ Tregs form aggregates on DCs, actively downregulate their costimulatory molecules, and impair the DCs’ ability to activate antigen-specific T cells (15).
Several viral and parasitic pathogens, including influenza viruses and helminths, have been implicated in protection against asthma and allergy (6, 7, 16); additional observations point to H. pylori as a plausible causative agent in asthma protection. First, H. pylori is rapidly disappearing from human populations; its disappearance is evident as a birth cohort effect, with fewer than 10% of children still harboring H. pylori in industrialized countries compared with the historic 70%–90% (17). The decline in H. pylori infection rates has preceded a rise in the prevalence of asthma and other atopic diseases in developed countries (3). Numerous case-control and cross-sectional studies have reported an inverse association of H. pylori infection with asthma, allergic rhinitis, and atopic dermatitis, especially in young individuals with early-onset disease (reviewed in ref. 11). H. pylori–infected children are known to preferentially launch Treg responses to the pathogen (18), which may account for the particularly beneficial effects of H. pylori in this population. In conclusion, our model of H. pylori–mediated asthma protection provides experimental support for the “disappearing microbiota” hypothesis (5), which postulates that the asthma and allergy epidemic of modern societies is a direct consequence of the disappearance of our ancestral indigenous microflora, which included H. pylori.
Methods
Animal experimentation.
C57BL/6 mice (Charles River) were orally infected with H. pylori PMSS1 or an isogenic CagE-deficient mutant (12). Infections and antibiotic therapy were performed as described (12). Mice were sensitized by i.p. injection of 20 μg OVA (Sigma-Aldrich) or 20 μg HDM allergen (Dermatophagoides pteronyssinus; Greer Laboratories) emulsified in 2.25 mg aluminum hydroxide (Alum Imject; Pierce) at 4 and 6 weeks after infection OVA-sensitized mice were challenged with 1% aerosolized OVA using an ultrasonic nebulizer (NE-U17; Omron) for 20 minutes daily on days 31, 32, and 33 after initial sensitization. HDM-sensitized animals were anesthetized on days 31, 32, and 33 by i.p. injection of ketamine/Rompun (Ketamine-Ratiopharm/Rompun 2%) and received 25 μg HDM allergen in 50 μl PBS intranasally. Airway resistance measurements were performed on anesthetized, intubated, and mechanically ventilated mice (flexiVent; Scireq) in response to increasing doses of inhaled methacholine (19). In vivo depletion of Tregs was achieved by 3 i.p. injections of 100 μg of anti-CD25 antibody (clone PC61) or by administration of diphtheria toxin to foxP3-EGFP-DTR–transgenic mice as described (12). MLN/PP single cell preparations and immunomagnetic cell sorting of CD4+CD25+ cells were performed as described (12). All animal experimentation was approved by the Zurich Cantonal Veterinary Office (Zurich, Switzerland).
BAL, histopathology, lung single cell preparation, flow cytometry, and real-time RT-PCR.
Lungs were lavaged via the trachea with 1 ml PBS. BALF cells were counted using Trypan blue dye exclusion. Differential cell counts of macrophages, lymphocytes, neutrophils, and eosinophils were performed on cytocentrifuged preparations stained with the Microscopy Hemacolor-Set (Merck). Cytokines in BALF were quantified by cytometric bead array (BD). Lungs were dissected, enzymatically digested with 0.5 mg/ml collagenase type IA (Sigma-Aldrich), and pushed through a 70-μm nylon cell strainer. The antibodies were anti-CD4 (clone H129.19), anti–I-Ab (clone AF6-120.1), anti-B220 (RA3-6B2), anti-CD11c (clone HL3), anti–IL-5 (clone TRFK5; all BD Biosciences — Pharmingen), anti-Foxp3 (FJK-16s), and anti–IL-17A (TC11-18H10.1, both eBioscience). Lungs were fixed by inflation and immersion in 10% formalin and embedded in paraffin. Tissue sections were stained with H&E and periodic acid-Schiff and examined in blinded fashion on a BX40 Olympus microscope. Peribronchial inflammation was scored on a scale from 0 to 4. PAS-positive goblet cells were quantified per 1 mm of basement membrane. FoxP3 real-time RT-PCR was performed as described previously (12).
Statistics.
All statistical analysis was performed using Graph Pad prism 5.0 software. The significance of categorical and numerical differences was calculated by Mann-Whitney and 2-tailed Student’s t test, respectively. P < 0.05 was considered significant.
Supplementary Material
Acknowledgments
This study was funded by grants from Swiss National Science Foundation and the Zurich University Research Priority Program — Systems Biology to A. Müller. Additional funding was obtained from Deutsches Forschungsgemeinschaft (DFG) (Ta 275/4-1 and Ta 275/5-1) and the Research Center for Immunology of the University of Mainz (to C. Taube).
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2011;121(8):3088–3093. doi:10.1172/JCI45041.
References
- 1.Busse WW, Lemanske RF., Jr Asthma. N Engl J Med. 2001;344(5):350–362. doi: 10.1056/NEJM200102013440507. [DOI] [PubMed] [Google Scholar]
- 2.Wakashin H, et al. IL-23 and Th17 cells enhance Th2-cell-mediated eosinophilic airway inflammation in mice. Am J Respir Crit Care Med. 2008;178(10):1023–1032. doi: 10.1164/rccm.200801-086OC. [DOI] [PubMed] [Google Scholar]
- 3.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 4.Strachan DP. Hay fever, hygiene, and household size. Bmj. 1989;299(6710):1259–1260. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blaser MJ, Falkow S. What are the consequences of the disappearing human microbiota? Nat Rev Microbiol. 2009;7(12):887–894. doi: 10.1038/nrmicro2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kitagaki K, Businga TR, Racila D, Elliott DE, Weinstock JV, Kline JN. Intestinal helminths protect in a murine model of asthma. J Immunol. 2006;177(3):1628–1635. doi: 10.4049/jimmunol.177.3.1628. [DOI] [PubMed] [Google Scholar]
- 7.Wilson MS, Taylor MD, Balic A, Finney CA, Lamb JR, Maizels RM. Suppression of allergic airway inflammation by helminth-induced regulatory T cells. J Exp Med. 2005;202(9):1199–1212. doi: 10.1084/jem.20042572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Blaser MJ. Inverse associations of Helicobacter pylori with asthma and allergy. Arch Intern Med. 2007;167(8):821–827. doi: 10.1001/archinte.167.8.821. [DOI] [PubMed] [Google Scholar]
- 9.Chen Y, Blaser MJ. Helicobacter pylori colonization is inversely associated with childhood asthma. J Infect Dis. 2008;198(4):553–560. doi: 10.1086/590158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reibman J, et al. Asthma is inversely associated with Helicobacter pylori status in an urban population. PLoS One. 2008;3(12):e4060. doi: 10.1371/journal.pone.0004060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blaser MJ, Chen Y, Reibman J. Does Helicobacter pylori protect against asthma and allergy? Gut. 2008;57(5):561–567. doi: 10.1136/gut.2007.133462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arnold I, et al. Tolerance rather than immunity protects from Helicobacter pylori -induced gastric preneoplasia. Gastroenterology. 2011;140(1):199–209. doi: 10.1053/j.gastro.2010.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson DS. Regulatory T cells and asthma. Clin Exp Allergy. 2009;39(9):1314–1323. doi: 10.1111/j.1365-2222.2009.03301.x. [DOI] [PubMed] [Google Scholar]
- 14.Steinman RM, et al. Dendritic cell function in vivo during the steady state: a role in peripheral tolerance. Ann N Y Acad Sci. 2003;987:15–25. doi: 10.1111/j.1749-6632.2003.tb06029.x. [DOI] [PubMed] [Google Scholar]
- 15.Onishi Y, Fehervari Z, Yamaguchi T, Sakaguchi S. Foxp3+ natural regulatory T cells preferentially form aggregates on dendritic cells in vitro and actively inhibit their maturation. Proc Natl Acad Sci U S A. 2008;105(29):10113–10118. doi: 10.1073/pnas.0711106105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang YJ, et al. Influenza infection in suckling mice expands an NKT cell subset that protects against airway hyperreactivity. J Clin Invest. 2011;121(1):57–69. doi: 10.1172/JCI44845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banatvala N, Mayo K, Megraud F, Jennings R, Deeks JJ, Feldman RA. The cohort effect and Helicobacter pylori. J Infect Dis. 1993;168(1):219–221. doi: 10.1093/infdis/168.1.219. [DOI] [PubMed] [Google Scholar]
- 18.Harris PR, et al. Helicobacter pylori gastritis in children is associated with a regulatory T-cell response. Gastroenterology. 2008;134(2):491–499. doi: 10.1053/j.gastro.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Reuter S, et al. Mast cell-derived tumour necrosis factor is essential for allergic airway disease. Eur Respir J. 2008;31(4):773–782. doi: 10.1183/09031936.00058907. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.