Abstract
Background.
Potential disparities in health care utilization were examined using overnight hospitalization data from the University of Alabama at Birmingham Study of Aging, a longitudinal investigation of a stratified sample of Medicare beneficiaries.
Methods.
Racial differences in self-reported surgical and nonsurgical overnight hospital admissions were examined using Cox proportional hazards models. Andersen’s Behavioral Model provided the conceptual framework to identify other potential predictors of admission.
Results.
Nine hundred and forty-two participants, 50.1% African American, provided data at baseline and at least one follow-up assessment (mean age = 75.3 years, range: 65–106). African Americans were less likely to utilize surgical admissions compared with Caucasians in a bivariate model (hazard ratio = 0.63, 95% confidence interval = 0.41–0.98). This effect was not significant after controlling for demographics and self-reported physical health. Additional bivariate predictors of surgical admission were intact mental status, having private insurance, and higher education. African Americans were less likely to utilize nonsurgical admissions in both bivariate (hazard ratio = 0.74, 95% confidence interval = 0.59–0.93) and covariate-adjusted models (hazard ratio = 0.64, 95% confidence interval = 0.50–0.84). This effect was significantly stronger for men than for women, with African American men only 0.50 times as likely as Caucasian men to report a nonsurgical admission. Other bivariate predictors of nonsurgical admission were increased age, poor physical health, negative psychological characteristics, higher levels of social support, and low perceived discrimination.
Conclusion.
Underutilization of services has been linked to increased mortality in African Americans. Modifications in mutable domains associated with service utilization such as perceived discrimination, social support, and having private insurance may be beneficial.
Keywords: Health care utilization, Health disparities, Minority aging, Hospital admission, Older adults
OLDER adults in the United States who are members of minority populations have an increased risk for negative health outcomes. This risk increases when the additive effect of low socioeconomic status is considered (1–3). Identification of disparities between the health outcomes of ethnic minorities compared with the Caucasian majority is a current focus of research (3). One important source of racial differences in health may be the disproportionate use of certain kinds of health services by minority groups. Underutilization of services by African Americans has been identified when studying several disease areas and has been linked to higher rates of mortality for African Americans (3,4). These findings have been mixed depending on the use of a national or local sample, the type of service utilization, and how it is measured.
Miller and associates (5) found that older African Americans were less likely to have an overnight hospital stay using data from the 1984 Supplement of Aging and the 1984 National Long-Term Care Survey, but there was no racial difference when examining data from the 1987 National Medical Care Expenditure Survey. An analysis of data from the National Health and Nutrition Examination Study revealed that that African American and Caucasian adults were hospitalized at similar rates in early adulthood, but African Americans were less likely to be hospitalized later in life (6). A delay in treatment-seeking behaviors in African Americans is a potential factor that may contribute to worse longitudinal outcomes.
Andersen (7) has reviewed the factors that might affect one’s likelihood to utilize health services. A portion of his behavioral model conceptualizes use of health services to be a function of individual determinants that are an individual’s characteristics that predispose him or her to use a particular service, social and environmental factors that enable or deter use, and one’s illness level or need for care. It was determined that need had the largest association with overnight hospitalization in previous investigations when compared with predisposing and enabling factors (8).
In the current investigation utilizing data from the University of Alabama at Birmingham Study of Aging, the primary objective was to examine the relationships between race and use of surgical and nonsurgical overnight hospital admissions in a sample of African American and Caucasian Medicare beneficiaries. Andersen’s Behavioral Model was used to identify additional measures (predisposing and enabling factors as well as illness level or need) predictive of overnight hospital admission.
METHODS
Participants
The University of Alabama at Birmingham Study of Aging, conducted at the University of Alabama at Birmingham, is a longitudinal observational study designed to examine racial differences in patterns of mobility, to examine short-term and long-term predictors of mobility limitation for African Americans and Caucasians, and to determine if mobility limitations predict subsequent nursing home placement and death. A stratified random sample of community dwelling adults aged 65 years and older was selected from a list of Medicare beneficiaries from five counties in central Alabama. The University of Alabama at Birmingham Study of Aging oversampled African Americans, males, and rural residents to provide a balanced sample in terms of race, gender, and urban–rural residence, with all individuals possessing some form of health care coverage. A total sample of 1,000 participants, 50% Caucasians, 50% African Americans, 51% rural, and 50% female, were recruited. Initial data were collected during an in-home assessment (1999–2001), and follow-up data were collected every 6 months via telephone interview. Data through the 48-month follow-up telephone interview are included in the present investigation. All procedures were approved by the Institutional Review Board of the University of Alabama at Birmingham.
Measures
Prospective overnight hospital admission.—
During the longitudinal follow-up telephone interviews, participants were asked, “In the last six months, have you been hospitalized overnight?” If so, the date and reason for each overnight hospitalization were recorded. The hospitalizations were later categorized as major surgical admissions or nonsurgical admissions. Surgical overnight hospital admissions included the following surgeries: cardiac, thoracic, gastrointestinal, orthopedic, vascular, and urologic. All other overnight hospital admissions including procedures such as colonoscopy and angioplasty were defined as nonsurgical (9). Participants reported dates for 1–3 admissions at each follow-up interview, and the time to the first occurrence was analyzed. If multiple events were reported, the date of the earliest event was used.
Predisposing characteristics.—
Demographic factors.—
The baseline questionnaire collected self-reported data on demographics, including age, gender, ethnicity, and marital status. Marital status was analyzed as married versus not married (widowed, separated, divorced, and never married).
Mini-Mental State Examination.—
The Mini-Mental State Examination is a brief and objective screening measure of cognitive impairment that has been proven to be valid and reliable across clinical, epidemiological, and community survey studies. The higher the score from 0 to 30, the less cognitively impaired the individual (10).
Depressive symptoms.—
Depression was assessed using the Geriatric Depression Scale—Short Form (SF), a 15-item self-report questionnaire designed to measure common symptoms of depression (11). Using a yes/no format, the respondents were asked if they had experienced the symptom in the past week. The scale has a range of 0 to 15, with higher scores on the questionnaire suggestive of clinical depression.
Anxiety.—
Anxiety was assessed using the Arthritis Impact Measurement Scale—Anxiety Subscale (12). The Arthritis Impact Measurement Scale is a self-report questionnaire that contains nine subscales, addressing physical, mental, and social health. The Arthritis Impact Measurement Scale has also previously been used in nonarthritic populations (13). The anxiety subscale consists of five items scored on a scale of 1 (always) to 5 (never). The items were totaled for an overall anxiety score ranging from 5–25. The lower scores corresponded to increased anxiety.
Enabling resources.—
Personal/family resources (education and health insurance) as well as social support were assessed. Education was recorded and ranged from 6 (sixth grade education or less) to 17 (graduate or professional degree). Private insurance was coded as 0 for individuals who reported no private insurance in addition to Medicare and 1 for those with private insurance.
Social support.—
Social support was assessed at baseline with four questions modified from the Arthritis Impact Measurement Scale. Individuals were asked: (a) How often did you feel that your family or friends would be around if you needed assistance, (b) were sensitive to your personal needs, (c) were interested in helping you solve problems, and (d) understood how getting older has affected you? Response options ranged from 0 (never) to 4 (always). Responses were summed to achieve a total score that ranged from 0 to 16, with higher scores representing more social support.
Urban versus rural residence.—
Urban versus rural community status was categorized by using geocoding. Once a latitude–longitude coordinate is assigned, the address can be displayed on a map or used in a spatial search to locate the nearest medical facilities or linked to census data to track population density. Individuals with missing data for this measure (N = 3) were categorized as living in an urban versus rural community based on the county they lived in.
Perceived discrimination.—
Participants were asked, “Over your lifetime, how often have you experienced discrimination because of your race or skin color?” Responses options included never (0), occasionally (1), often (2), very often (3), and always (4).
Illness level or need.—
SF-12.—
The SF-12 provides a global measure of health. The SF-12 physical component scale score was standardized to have a mean of 50 and a SD of 10 in the adult U.S. population (14). Similarly, the SF-12 produces a mental component scale score. Both component scores were examined.
Activities of daily living.—
Activities of daily living assessed the individual’s ability to perform five self-care tasks, including eating, using the toilet, dressing, transferring, and bathing. Participants were asked if they had difficulty performing each task. Scores on this measure were a count of the tasks the participant reported having difficulty performing (15).
Short Physical Performance Battery.—
Timed tests of balance, walking, and the ability to rise from a chair were used to measure lower extremity function (16,17). Persons were ranked by standards set by Guralnik and associates (17); a person unable to perform a given task was assigned a score of 0 for that task and 4 represented the highest level of performance. The composite score, calculated as the sum of the three rankings, ranged from 0 to 12, with higher scores indicating better performance. The internal consistency of the scale for the entire University of Alabama at Birmingham Study of Aging sample, as assessed by Cronbach alpha, was .76 (18).
Statistical Analyses
All analyses were performed using the SAS 9.1 software package (19). Racial differences on study variables at baseline were examined using t tests for continuous variables and chi-square independence tests for nominal variables. Complete date information was provided for 540 of the 578 hospitalization events. For 26 hospitalization events, only the month and year were recorded, and the 15th day of that month was analyzed as the date of that event in the analyses. If a participant reported a hospitalization but did not provide a date (N = 12), the midpoint between the current assessment and the previous assessment was imputed as the date of the hospitalization. A time-to-event analysis was conducted using Cox Proportional hazards models to examine the bivariate effects of study variables on time to the first overnight hospital admission (20,21). If no admission occurred, time to the event was censored. For individuals who died, the death date was used as the censoring point. For individuals who survived throughout the follow-up period without overnight hospitalization, the date of last follow-up interview was used as the censoring date.
Additional covariate-adjusted models were conducted to assess the effects of race on time to hospital admission. These models examined race as a predictor of hospital admission and statistically controlled for age, gender, education, marital status, urban versus rural residence, and physical health. A Race × Gender interaction was also assessed to determine if the effect of race on hospital admission rates depended on an individual’s gender. For significant interactions, vectors were used to compare African American females, African American males, and Caucasian females to the reference group, Caucasian males, to examine the nature of the significant interaction.
RESULTS
Participants
A total of 942 participants were eligible for this analysis. The mean age of these participants was 75.3 (SD = 6.7; range: 65–106). African Americans were significantly older, less likely to be married, had lower Mini-Mental State Examination scores, and reported higher levels of anxiety than Caucasians. African Americans were also less likely to have private insurance, had fewer years of education, less social support, reported worse physical and mental health, and were more likely to report perceived discrimination compared with their Caucasian counterparts (Table 1). Ninety-six percent of participants reported having a doctor whom they see for their normal health care.
Table 1.
Descriptive Statistics for University of Alabama at Birmingham Study of Aging Variables at Baseline
| Variable | African American (n = 472) | Caucasian (n = 470) | p Value |
| Age, M (SD) | 75.8 (7.2) | 74.9 (6.3) | .0119 |
| Female gender, n (%) | 240 (50.8) | 238 (50.6) | .9488 |
| Rural, n (%) | 235 (49.8) | 235 (50.0) | .9482 |
| Married, n (%) | 189 (40.0) | 294 (62.5) | <.0001 |
| PCS, M (SD) | 38.81 (12.4) | 41.16 (13.2) | .0050 |
| MMSE, M (SD) | 23.09 (5.1) | 27.16 (3.2) | <.0001 |
| Depressive symptoms, M (SD) | 2.4 (2.3) | 2.2 (2.3) | .1543 |
| Anxiety, M (SD) | 19.2 (4.2) | 19.8 (4.0) | .0204 |
| MCS, M (SD) | 52.8 (9.91) | 54.3 (9.3) | .0180 |
| Education, M (SD) | 9.2 (3.2) | 12.1 (2.7) | <.0001 |
| Private insurance, n (%) | 141 (29.9) | 317 (67.4) | <.0001 |
| Social support score, M (SD) | 13.7 (3.3) | 14.2 (2.7) | .0170 |
| Racial discrimination, M (SD) | 1.1 (1.2) | 0.1 (0.4) | <.0001 |
| ADL limitations, M (SD) | 0.9 (1.3) | 0.7 (1.1) | .0195 |
| SPPB composite score, M (SD) | 5.9 (3.2) | 7.8 (3.0) | <.0001 |
Notes: ADL = activities of daily living; MCS = the SF-12 mental component scale; MMSE = Mini-Mental State Examination; PCS = the SF-12 physical component scale; SPPB = Short Physical Performance Battery.
Surgical Overnight Hospital Admissions
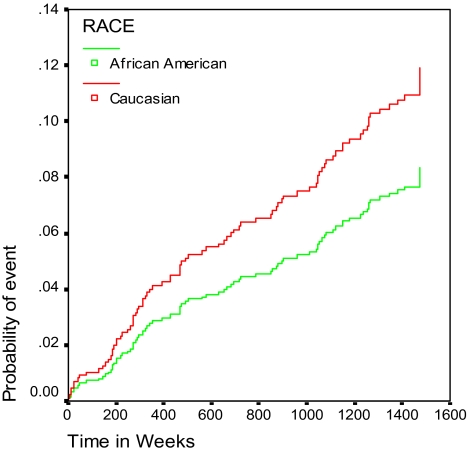
The number of surgical admissions ranged from 0 to 2, with 85 participants (9.0%) reporting at least one admission. Bivariate analyses revealed that the African Americans were less likely to report a surgical admission than Caucasians (hazard ratio = 0.63, 95% confidence interval = 0.41–0.98). Lower physical component scale, higher Mini-Mental State Examination, having private insurance, and more activities of daily living limitations were each predictive of a higher rate of surgical admission. There was also a trend for more education being associated with a higher rate of surgical admission (Table 2). Although the main effect of race was no longer significant in the covariate-adjusted model, African Americans were only 0.69 times as likely to utilize a surgical admission when compared with Caucasians at any given time (hazard ratio = 0.69, 95% confidence interval = 0.42–1.13; Figure 1). The Race × Gender interaction was nonsignificant.
Table 2.
Univariate Cox Proportional Hazard Ratios for the Effect of Each Predictor on Time to Surgical Overnight Hospital Admission
| Predictors | Hazard Ratio (95% Confidence Interval) | p Value |
| Demographics | ||
| Race (African American vs Caucasian) | 0.633 (0.409–0.979) | .0398 |
| Age | 0.986 (0.954–1.019) | .4088 |
| Gender (female vs male) | 0.853 (0.558–1.306) | .4652 |
| Married (yes vs no) | 0.950 (0.621–1.454) | .8133 |
| Residence (rural vs urban) | 1.047 (0.684–1.602) | .8323 |
| Neuropsychological characteristics | ||
| MMSE | 1.121 (1.050–1.197) | .0007 |
| Depressive symptoms | 1.029 (0.942–1.125) | .5236 |
| Anxiety | 0.969 (0.922–1.018) | .2119 |
| MCS | 0.998 (0.976–1.020) | .8445 |
| Personal/family resources | ||
| Education | 1.065 (0.998–1.137) | .0588 |
| Private insurance (yes vs no) | 1.960 (1.256–3.058) | .0030 |
| Social support and social structure | ||
| Social support score | 0.963 (0.903–1.027) | .2561 |
| Perceived discrimination | 0.974 (0.788–1.205) | .8104 |
| Need | ||
| PCS | 0.981 (0.966–0.997) | .0228 |
| ADL limitations | 1.193 (1.030–1.382) | .0188 |
| SPPB composite score | 0.976 (0.914–1.041) | .4619 |
Notes: ADL = activities of daily living; MCS = the SF-12 mental component scale; MMSE = Mini-Mental State Examination; PCS = the SF-12 physical component scale; SPPB = Short Physical Performance Battery.
Figure 1.
Racial difference in rates of overnight surgical admission.
Nonsurgical Overnight Hospital Admissions
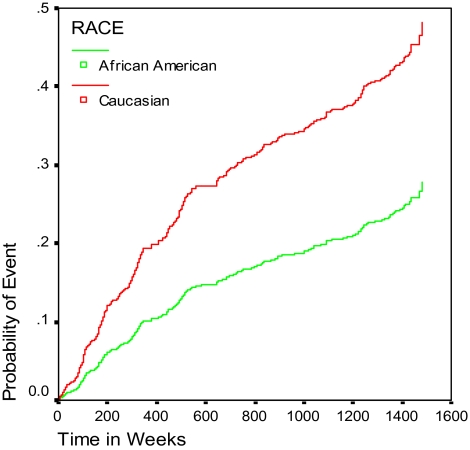
The number of nonsurgical admissions ranged from 0 to 7, with 315 participants (33.4%) reporting at least one. Bivariate Cox proportional hazards models revealed that African Americans were also less likely to utilize nonsurgical admissions, (hazard ratio = 0.74, 95% confidence interval = 0.59-0.93). Older age, lower physical component scale, more depressive symptoms and anxiety, lower mental component scale, more social support, reporting less racial discrimination, more activities of daily living limitations, and poor performance on the Short Physical Performance Battery were predictive of a higher rate of utilization of nonsurgical admissions (p’s < .05; Table 3).
Table 3.
Univariate Cox Proportional Hazard Ratios for the Effect of Each Predictor on Time to Nonsurgical Overnight Hospital Admission
| Predictors | Hazard Ratio (95% Confidence Interval) | p Value |
| Demographics | ||
| Race (African American vs Caucasian) | 0.742 (0.594–0.927) | .0085 |
| Age | 1.029 (1.013–1.045) | .0004 |
| Gender (female vs male) | 0.952 (0.763–1.187) | .6614 |
| Married (yes vs no) | 0.856 (0.686–1.068) | .1686 |
| Residence (rural vs urban) | 0.991 (0.794–1.236) | .9341 |
| Neuropsychological characteristics | ||
| MMSE | 1.005 (0.981–1.029) | .6898 |
| Depressive symptoms | 1.089 (1.042–1.138) | .0002 |
| Anxiety | 0.956 (0.931–0.981) | .0007 |
| MCS | 0.982 (0.971–0.992) | .0007 |
| Personal/family resources | ||
| Education | 1.000 (0.967–1.034) | 1.0000 |
| Private insurance (yes vs no) | 1.168 (0.936–1.457) | .1689 |
| Social support and social structure | ||
| Social support score | 1.044 (1.003–1.087) | .0371 |
| Perceived discrimination | 0.876 (0.779–0.985) | .0267 |
| Need | ||
| PCS | 0.970 (0.962–0.978) | <.0001 |
| ADL limitations | 1.194 (1.104–1.291) | <.0001 |
| SPPB composite score | 0.919 (0.890–0.949) | <.0001 |
Notes: ADL = activities of daily living; MCS = the SF-12 mental component scale; MMSE = Mini-Mental State Examination; PCS = the SF-12 physical component scale; SPPB = Short Physical Performance Battery.
The disparity in utilization of nonsurgical admissions widened in the covariate-adjusted model, with African Americans being only 0.64 times as likely to utilize a nonsurgical admission at any given time when compared with Caucasians (hazard ratio = 0.64, 95% confidence interval = 0.50–0.84; Figure 2). The Race × Gender interaction was found to be significant, p = .0275. Each race–gender group reported a significantly lower rate of nonsurgical admission than the referent Caucasian male group (p’s < .02). The largest difference was between African American men and Caucasian men, with African American men only 0.50 times as likely to reporting a nonsurgical admission at any given time.
Figure 2.
Racial difference in rates of overnight nonsurgical admission.
Discussion
African Americans reported lower utilization rates for both major surgical and nonsurgical overnight hospital admissions compared with their Caucasian counterparts. Race was a significant predictor of surgical overnight hospital admission when other factors were not included in the model. However, the covariate-adjusted effect of race was not significant, perhaps due to the small percentage of participants reporting the outcome and/or the number of predictors in the model. These findings are consistent with research examining surgery for specific conditions (22,23). Data from the 1990 U.S. Census, the National Center for Health Statistics, and the Centers for Medicare and Medicaid Services found racial differences in surgical procedures to treat heart disease (cardiac catheterization, coronary artery bypass graft, and percutaneous transluminal coronary angioplasty), with African Americans less likely to undergo these procedures.
Predictors of Service Utilization
Predisposing characteristics.—
Individuals suffering from mental problems have been found to be less likely to engage in preventive behaviors compared with older adults without mental health problems (24). These finding were supported by the results of this investigation. Individuals with higher Mini-Mental State Examination scores, which represent better cognitive functioning, were more likely to utilize surgical overnight hospital admissions. Poorer mental health, measured by depressive symptoms, anxiety, and the mental component scale, were predictive of higher rates of nonsurgical admission. These results advocate the need for medical personnel to address mental health issues with their patients, particularly because of previously observed links between psychological characteristics and physical health (25).
Enabling resources.—
This investigation revealed a link between perceived discrimination and a lower rate of nonsurgical admission. Perceived discrimination is important to consider relative to the health and well-being of older minority adults; literature indicates that discrimination may have a negative impact on the mental and physical health of African Americans (26–30). Specifically, an individual’s perception of discrimination represents a stressful life experience that can have an adverse impact on health. Although the lifetime experience of discrimination cannot be changed, delayed treatment seeking could potentially be decreased at the individual level with programs targeted at making the individual feel more comfortable with their physician and the health care environment. Overcoming the barriers presented by the perception of discrimination could decrease the utilization disparities between African American and Caucasian older adults.
Although all participants were Medicare beneficiaries, individuals with private insurance in addition to their Medicare coverage were found to have a higher rate of surgical admission. Private insurance results in lower hospital copayments, better coverage of the costs of physicians’ services, and better coverage of the costs of medications (31). In addition to reducing out-of-pocket expenses, private insurance also provides the opportunity to select from a larger network of physicians. Therefore, individuals with limited resources and no access to private insurance might continue to show disparities in utilization.
Social support was found to be predictive of a higher rate of utilizing nonsurgical hospital admission. This result was consistent with the findings of Penning (32) where high levels of instrumental support from members of the support network were associated with more hospitalizations within the past year in a sample of adults 60 years of age and older residing in Canada.
Illness level or need.—
Poor physical performance measured by the Short Physical Performance Battery was predictive of a higher rate of nonsurgical admission. A low physical component scale score and more activities of daily living limitations were predictive of both surgical and nonsurgical overnight hospital admission. Although need in African Americans might have been greater, there was lack of corresponding service utilization.
Limitations of the Current Investigation
The current findings were derived from self-reported hospital admissions data. Previous work comparing self-report data to administrative data has shown that participant reports underestimate the actual services utilized (33,34). Additionally, sample size constraints prevented an analysis of the predictors for specific reasons for admission. Investigation of individuals with a particular disease profile might have resulted in a different set of predictors. Time since diagnosis would be another indication of participants’ willingness to seek treatment, another important factor in Anderson’s model. Hospitalizations are unlike ambulatory care visits or use of preventive procedures such as mammography or flu shots in that they are more affected by a patient’s health maintenance behaviors. Previous research hypothesizes that minorities may have personal preferences toward care seeking that differ from Caucasians (35,36). This pathway could not be assessed utilizing data from the University of Alabama at Birmingham Study of Aging as the primary focus of the study was mobility, and measures that assess preferences toward care seeking and undergoing surgical procedures were not assessed.
Conclusions
Andersen’s model was effective in identifying measures predictive of health care utilization, which has been linked to physical health outcomes in older adults. Andersen suggests intervening on measures that have high mutability, the extent to which a given component can actually be altered to influence the distribution of health services (8). The results of this investigation suggest that reductions of racial differences in domains that enable or deter service utilization such as social support, perceived discrimination, and having private insurance may lead to a minimization of delayed treatment seeking in older African American Medicare beneficiaries. Additional longitudinal studies building on these findings are needed to examine the multiple dimensions that lead to health disparities. Specifically, studies aimed to examine additional predictors of service utilizations such as individual differences in care seeking and physician preferences and determine if racial differences in service utilization lead to negative outcomes.
FUNDING
This work was supported by the National Institute on Aging at the National Institutes of Health (R01 AG015062 and 3P30AG031054-02S1).
References
- 1.Williams D, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 2.Thorpe RJ, Kasper J, Szanton S, Frick K, Fried L, Simonsick E. Relationship of race and poverty to lower extremity function and decline: findings from the Women’s Health and Aging Study. Soc Sci Med. 2008;66:811–821. doi: 10.1016/j.socscimed.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine; 2002. [PubMed] [Google Scholar]
- 4.Jang Y, Giyeon K, Chiriboga DA. Health, health care utilization, and satisfaction with service: barriers and facilitators for older Korean Americans. J Am Geriatr Soc. 2005;53:1613–1617. doi: 10.1111/j.1532-5415.2005.53518.x. [DOI] [PubMed] [Google Scholar]
- 5.Miller B, Campbell RT, Furner S, Kaufman JE, Li M, Muramatsu N, et al. Use of medical care by African American and White older persons: comparative analysis of three national data sets. J Gerontol B Soc Sci. 1997;52B(6):S325–S335. doi: 10.1093/geronb/52b.6.s325. [DOI] [PubMed] [Google Scholar]
- 6.Ferraro KF, Thorpe RJ, McCabe GP, Kelley-Moore JA, Jiang Z. The color of hospitalization over the adult life course: cumulative disadvantage in Black and White? J Gerontol B Soc Sci. 2006;61B(6):S299–S306. doi: 10.1093/geronb/61.6.s299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter. J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 8.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83:1–28. [PubMed] [Google Scholar]
- 9.Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150:372–378. doi: 10.7326/0003-4819-150-6-200903170-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 11.Yesavage JA, Brink TL, Rose TL, Adey M. The geriatric depression rating scale: comparison with other self-report and psychiatric rating scales. In: Crook T, Ferris SH, Bartus R, editors. Assessment in Geriatric Psychopharmacology. New Canaan, CT: Mark Powley Associates; 1983. pp. 153–165. [Google Scholar]
- 12.Meenan RF, Gertman PM, Mason JH. Measuring health status in arthritis: the arthritis impact measurement scale. Arthritis Rheum. 1980;23:146–152. doi: 10.1002/art.1780230203. [DOI] [PubMed] [Google Scholar]
- 13.Anderson JJ, Firschein HE, Meenan RF. Sensitivity of a health status measure to short-term clinical changes in arthritis. Arthritis Rheum. 1989;32:844–850. [PubMed] [Google Scholar]
- 14.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston MA: Health Institute, New England Medical Center; 1995. [Google Scholar]
- 15.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 16.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 17.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J Gerontol A Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peel C, Baker PS, Roth DL, Brown CJ, Bodner EV, Allman RM. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85:1008–1019. [PubMed] [Google Scholar]
- 19.SAS. SAS Version 9. SAS Institute Inc. Cary, NC: SAS Institute Publishing; 2002. [Google Scholar]
- 20.Hosmer DW, Jr, Lemeshow S. Applied Survival Analysis: Regression Modeling of Time to Event Data. New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 21.Allison PD. Survival Analysis Using SAS: A Practical Guide. Cary, NC: SAS Institute; 1995. [Google Scholar]
- 22.Eggers PW, Greenberg LG. Racial and ethnic differences in hospitalization rates among aged Medicare beneficiaries, 1998. Health Care Financ Rev. 2000;21:1–15. [PMC free article] [PubMed] [Google Scholar]
- 23.Steel N, Clark A, Lang IA, Wallace RB, Melzer D. Racial disparities in receipt of hip and knee joint replacements are not explained by need: the Health and Retirement Study 1998–2004. J Gerontol A Biol Sci Med Sci. 2008;63:629–634. doi: 10.1093/gerona/63.6.629. [DOI] [PubMed] [Google Scholar]
- 24.Burns BJ, Wagner HR, Gaynes BN, Wells KB, Schulberg HC. General medical and specialty medical health service use for major depression. Int J Psychiatry Med. 2000;30:127–143. doi: 10.2190/TLXJ-YXLX-F4YA-6PHA. [DOI] [PubMed] [Google Scholar]
- 25.Kim HFS, Braun U, Kunik ME. Anxiety and depression in mentally ill older adults. J Clin Geropsychology. 2001;7(2):117–130. [Google Scholar]
- 26.Kessler RC, Mickleson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 27.Williams DR, Neighbors HW, Jackson J. Racial/ethnic discrimination and health: Findings from community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKenzie K. Racism and health. BMJ. 2003;326:65–66. doi: 10.1136/bmj.326.7380.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford, UK: Oxford University Press; 2000. pp. 36–75. [Google Scholar]
- 30.Lewis TT, Barnes LL, Bienias JL, Lackland DT, Evans DA, Mendes de Leon CF. Perceived discrimination and blood pressure in older African American and White adults. J Gerontol A Biol Sci Med Sci. 2009;64A(9):1002–1008. doi: 10.1093/gerona/glp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miles S, Parker K. Men, women, and health insurance. N Engl J Med. 1997;336:218–221. doi: 10.1056/NEJM199701163360312. [DOI] [PubMed] [Google Scholar]
- 32.Penning MJ. Health, social support, and the utilization of health services among older adults. J Gerontol B Soc Sci. 1995;50B(5):S330–S339. doi: 10.1093/geronb/50b.5.s330. [DOI] [PubMed] [Google Scholar]
- 33.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ. Comparison of self-reported and medical health care utilization measures. J Clin Epidemiol. 1996;49:989–995. doi: 10.1016/0895-4356(96)00143-6. [DOI] [PubMed] [Google Scholar]
- 34.Wallihan DB, Stump TE, Callahan CM. Accuracy of self-reported health services use and patterns of care among urban older adults. Med Care. 1999;37:662–670. doi: 10.1097/00005650-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O’Malley K, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication. J Gen Intern Med. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ibrahim SA, Zhang A, Mercer MB, Baughman M, Kwoh CK. Inner city African American elder patients’ perceptions and preferences for the care of chronic knee and hip pain: findings from focus groups. Gerontol A Biol Sci Med Sci. 2004;59A(12):1318–1322. doi: 10.1093/gerona/59.12.1318. [DOI] [PubMed] [Google Scholar]