This report expands the literature showing that robotic-assisted removal of mediastinal masses or cysts can be a safe and effective technique in the management of intrathoracic disease.
Keywords: Duplication cysts, robotic surgery, thoracoscopy, VATS
Abstract
Esophageal duplication cysts are infrequent anomalies of the gastrointestinal tract that are predominantly found in children. The conventional surgical approach for removal of these cysts is an open surgery one with a posterolateral thoracotomy incision. However, more recently, these cysts have been excised via video-assisted thoracoscopic surgery (VATS). In this article, we present 2 pediatric patients treated with successful excision of an esophageal duplication cyst via robotic-assisted thoracoscopic surgery (RATS) using the da Vinci surgical system. With robotic technology, precise dissection and complete resection of the thoracic mass was achieved without violating the esophageal mucosa. There were no complications, and the patients did not require placement of a postoperative chest tube. Pathological examination of the mass was consistent with an esophageal (foregut) duplication cyst in both cases.
INTRODUCTION
Duplication cysts of the alimentary tract are infrequent anomalies that can affect any portion of the gastrointestinal tract.1 The reported incidence of gastrointestinal duplication cysts is 1:100 000, with approximately 70% to 75% of the cases affecting children.2–4 The most common location for these cysts is the ileum with the esophagus being the second most prevalent site.1–4 Clinical presentation of patients with esophageal duplication cysts is varied. In children, esophageal cysts become symptomatic in 80% of cases while most adults with esophageal cysts are asymptomatic.2,5–9 The most common complaints of symptomatic patients are dysphagia, epigastric discomfort, and retrosternal pain.10–11 Once diagnosed, the definitive treatment for esophageal cysts is surgical excision. Most cysts are resected due to active symptoms. However, cysts that are incidentally found and asymptomatic are surgically resected to prevent potential complications from untreated duplication cysts.2,10,12 Potential complications include cyst rupture, infection, and bleeding.2,10,12 In addition, in rare cases, malignant transformation of the cysts can occur.1,2 Furthermore, definitive diagnosis of esophageal duplication cysts is made via pathological examination of a surgical specimen.1,12 While open surgical resection via posterolateral thoracotomy is the conventional approach for removal of esophageal duplication cysts, video-assisted thoracoscopic surgery (VATS) has become a viable alternative approach for the esophageal cyst excision.12 This report describes the successful excision of an esophageal duplication cyst in 2 pediatric patients using robotic-assisted thoracoscopic surgery (RATS) with the da Vinci surgical system (Surgical intuitive, Mountain View, CA).
CASE REPORTS
Case 1
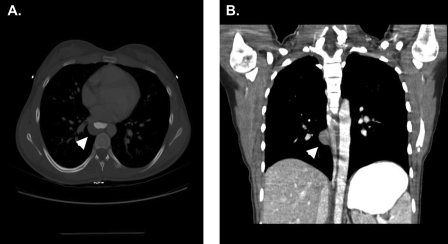
A 12-year-old Caucasian female was brought in by her parents for evaluation of new onset shortness of breath. A CT scan of the chest with contrast was performed, and a mediastinal mass was found. The mass measured 2cm x 1.5cm in size and was located in the posterolateral aspect of the mid thoracic esophagus on the right (Figure 1A, 1B). The radiographic appearance of the mass was consistent with a cystic lesion, likely an esophageal or bronchogenic duplication cyst. The patient was scheduled to undergo surgical resection.
Figure 1.
CT scan of the chest showing the presence of a mass on the posterolateral aspect of the esophagus on the right. A. Transverse view. B. Coronal view.
Case 2
A 15-year-old Caucasian male with a history of spina-bifida, hydrocephalus, VP shunt, and a 1-week history of back pain was evaluated with a CT of the thorax/spine, which revealed a 2cm x 2cm retrocaval right-sided thoracic mass determined to be solid based on CT criteria. At that time, his parent's had reported several diaphoretic spells. Differential diagnosis included carcinoid tumor, neuroblastoma, and duplication cyst. Serotonin levels were normal and markers for neuroblastoma were negative. Surgery was scheduled for resection of the mass.
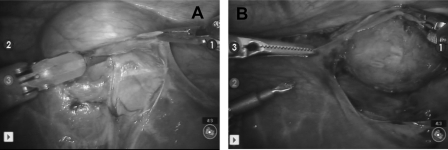
Both patients were treated with robotic-assisted thoracoscopic resection. The technique used for both is described here. After general anesthesia and intubation with a double lumen tube, the patients were placed in the left lateral decubitus position with the right side of the chest up. An 8-mm da Vinci port used for the 3-dimensional 8-mm camera was placed at the level of the sixth intercostal space, at the mid axillary line. A total of 3 additional 8-mm trocars were inserted under direct thoracoscopic guidance, one in the right upper chest behind the scapula and 2 in the right lower chest at the level of the mid axillary line. Once all trocars were in adequate position, the da Vinci camera was docked, followed by sequential docking of each of the 3 instrument robotic arms. By using a combination of da Vinci instruments including a small electrocautery spatula, DeBakey dissector, and Cartier grasper, the cyst was mobilized in each case. The duplication cyst was found to be approximately 2cm x 3cm and covered by a layer of pleura, which was divided. Subsequently, the cyst was mobilized away from the pulmonary vein. In both cases, the cyst was in very close relationship to the thoracic esophagus and appeared to share a common wall. The cyst was mobilized carefully with sharp and blunt dissection away from the esophagus by dividing some of the muscle fibers of the esophageal wall without entering the mucosa (Figure 2). No further surgical manipulations were necessary to enucleate the cysts. In one case, the mucosa was exposed slightly but not injured, and the lumen of the esophagus was not entered; hence, we did not believe it was necessary to test the esophagus for perforation via endoscopy. The posterior and anterior branches of the vagus nerve were identified and dissected away from this lesion with complete preservation of the vagus. Complete resection of the cyst was achieved in both cases. In one case, the cyst was removed intact. However, in the second case, the cyst was ruptured due to a small extravasation identified at the time of the procedure. As a result, the pleural cavity was copiously irrigated and aspirated. The estimated blood loss was <5cc, and no chest tube placement was necessary. Complete re-expansion of the lung was achieved after evacuation of the pneumothorax with a ravenel drainage tube placed through one of the trocar sites and removed at the conclusion of the procedure.
Figure 2.
Intraoperative appearance of esophageal duplication cyst.
Postoperatively, no complications occurred. Both patients experienced minimal pain, and were mobilized/ambulating and eating a normal diet by postoperative day 1. One patient was discharged home on postoperative day 1, and the second one was discharged on postoperative day 2. Pathological examination of the excised specimens confirmed the diagnosis of an esophageal (foregut) duplication cyst.
DISCUSSION
For an esophageal cyst to be classified as duplication, it must meet the following criteria: (1)The cyst must be within or attached to the esophageal wall, (2) it must be covered by 2 muscle layers, (3) and the lining must be squamous, columnar, cuboidal, pseudostratified, or ciliated epithelium.10 Clinical presentation varies, with the most common presenting symptoms being dysphagia, epigastric discomfort, and retrosternal pain.10–12 In our cases, the patients presented with new onset shortness of breath and chest pain. Preoperative diagnosis of an esophageal cyst can be made by standard radiological techniques like CT scans and endoscopic ultrasound.13–16 In one of our cases, the CT scan was somewhat misleading, because it suggested the presence of a solid posterior mediastinal lesion. However, at the time of surgery, the lesion was found to be cystic, as would be expected with a duplication cyst. Surgical excision is the definitive treatment for esophageal cysts. In addition, surgical excision is also required for definitive diagnosis via pathological examination of the resected specimen. Open surgical resection via posterolateral thoracotomy incision has been considered the best surgical approach for the excision of the cysts. However, video-assisted thoracoscopic surgery (VATS) has recently become a viable surgical option for the excision of duplication cysts.12 Compared with the open approach, VATS reduces postoperative pain, leads to earlier recovery and hospital discharge, and has a better cosmetic outcome.12,17 Most recently, some have advocated the use of robotic technology for surgical resection of such lesions. Robotic-assisted thoracoscopic (RATS) surgery is becoming more widely accepted and used.18–20 Compared with VATS, RATS has a few advantages: (1)superior visualization of the surgical field, (2) greater range of motion with multi-articulated instruments, and (3) more precise movements with tremor filtration and motion scaling.18 In this article, we present 2 pediatric patients who underwent successful surgical resection of esophageal duplication cysts via RATS using the da Vinci surgical system. As previously reported,18–20 we had no operative complications but did have excellent postoperative outcomes including decreased pain and early patient discharge.
CONCLUSION
This article expands the current literature on the use of robotic surgery for the removal of mediastinal masses or cysts, such as esophageal (foregut) duplication cysts. Additionally, it provides further supportive evidence for the use of robotic surgery as a safe and effective surgical technique in the management of intrathoracic pathology.
Contributor Information
Patrick Chidi Obasi, Division of Pediatric Surgery, Medical University of South Carolina, Charleston, South Carolina, USA..
Andre Hebra, Division of Pediatric Surgery, Medical University of South Carolina, Charleston, South Carolina, USA..
Juan Carlos Varela, Medical Scientist Training Program, Medical University of South Carolina, Charleston, South Carolina, USA..
References:
- 1. Hebra A. Alimentary tract duplications. Surgical Directives: Pediatirc Surgery. Lippincott Williams and Wilkins; Philadelphia, PA: 2002 [Google Scholar]
- 2. Ringley C, Bochkarev V, Oleynikov D. Esophageal duplication cyst–a guest case in robotic and computer-assisted surgery from the university of Nebraska Medical Center. Medscape General Medicine. 2006;8(4):25. [PMC free article] [PubMed] [Google Scholar]
- 3. Banner KB, Helft S, Kadam J, Miah A, Kaushik N. An unusual cause of dysphagia in a young woman: esophageal duplication cyst. Gastintest Endosc. 2008;68(4):793–795 [DOI] [PubMed] [Google Scholar]
- 4. Will U, Meyer F, Bosseckert H. Successful endoscopic treatment of an esophageal duplication cyst. Scan J Gastroenterol. 2005;40(8):995–999 [DOI] [PubMed] [Google Scholar]
- 5. Gerle RD, Jaretski A, Ashley CA, Berne AS. Congenital bronchopulmonary foregut malformation. Pulmonary sequestration communicating with the gastrointestinal tract. N Engl J Med. 1968;278(26):1413–1419 [DOI] [PubMed] [Google Scholar]
- 6. Sundaramoothi T, Behranwala AA, Codispoti M, Mankad P. Asymptomatic Congenital oesophageal cyst infiltrating the lung: An unusual complication. Eur J Cardiothorac Surg. 2000;18:117–119 [DOI] [PubMed] [Google Scholar]
- 7. Diaz de Liano A, Ciga MA, Trujillo R, Aizcorbe M, Cobo F, Oteiza F. Congenital esophageal cysts—two cases in adult patients. Hepatogastroenteroogy. 1999;46(28):2405–2408 [PubMed] [Google Scholar]
- 8. Cioffi U, Bonavina L, De Simone M, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest. 1998;113:1492–1496 [DOI] [PubMed] [Google Scholar]
- 9. Versleine MW, Drenth JP, Nagengast FM. A case of esophageal duplication cyst with a 13-year follow-up period. Endoscopy. 2005;37:870–872 [DOI] [PubMed] [Google Scholar]
- 10. Singh K, Saxena A, Narasimha K, Singh M, Suri S. Esophageal duplication cyst: An unusual case of respiratory distress in infants. Pediatr Emerg Care. 2005;21(12):854–856 [DOI] [PubMed] [Google Scholar]
- 11. Anderson MC, Silberman WW, Shields TW. Duplications of the alimentary tract in the adult. Arch Surg. 1962;85:94–108 [DOI] [PubMed] [Google Scholar]
- 12. Kang CU, Cho DG, Cho KD, Jo MS. Thoracoscopic stapled resection of multiple esophageal duplication cysts with different pathological findings. Eur J Cardiothorac Surg. 2008;34:216–218 [DOI] [PubMed] [Google Scholar]
- 13. Noguchi T, Hashimoto T, Takeno S, Wada S, Tohara K, Uchida Y. Laparoscopic resection of esophageal duplication cyst in an adult. Dis Esophagus. 2003;16:148–150 [DOI] [PubMed] [Google Scholar]
- 14. Sirivella S, Ford WB, Zikria EA, Miller WH, Samadani SR, Sullivan ME. Foregut cysts of the mediastinum. Results in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg. 1985;90(5):776–782 [PubMed] [Google Scholar]
- 15. Bhutani MS, Hoffman BJ, Reed C. Endosonographic diagnosis of an esophageal duplication cyst. Endsocopy. 1996;28(4):396–397 [DOI] [PubMed] [Google Scholar]
- 16. Van Dam J, Rice TW, Sivak MV. Endoscopic ultrasonography and endoscopically guided needle aspiration for the diagnosis of upper gastrointestinal tract foregut cysts. Am J Gastroenterol. 1992;87(6):762–765 [PubMed] [Google Scholar]
- 17. Hazelrigg SR, Landreneau RJ, Mack MJ, Acuff TE. Thoracoscopic resection of mediastinal cysts, Ann Thorac Surg. 1993;56(3):659–660 [DOI] [PubMed] [Google Scholar]
- 18. Bodnes J, Zitt M, Ott H, et al. Robotic-assisted thoracoscopic surgery (RATS) for benign and malignant esophageal tumors. Ann Thorac Surg. 2005;80:1202–1206 [DOI] [PubMed] [Google Scholar]
- 19. Melfi F, Menconi GF, Mariani M, Angeletti CA. early experience with robotic technology for thoracoscopic surgery. Eur J Cardiothorac Surg. 2002;21:864–868 [DOI] [PubMed] [Google Scholar]
- 20. Bodner J, Wykypiel H, Wetscher G, Schmid T. First experiences with the da Vinci operating robot in thoracic surgery. Eur J Cardiothorac Surg 2004;25:844–851 [DOI] [PubMed] [Google Scholar]