A laparoscopic approach is recommended for the complication of prolapsed sigmoid colon epiploica after total laparoscopic hysterectomy.
Keywords: Total laparoscopic hysterectomy, Sigmoid colon, Prolapse
Abstract
Prolapsed epiploica of the sigmoid colon through the vaginal cuff is a rare finding that has never been reported after total laparoscopic hysterectomy. We encountered a case of prolapsed epiploica of the sigmoid colon in a 40-year-old female, 4 months status after total laparoscopic hysterectomy. Diagnostic laparoscopy demonstrated prolapsed epiploica of the sigmoid colon through a dehisced vaginal cuff.
INTRODUCTION
Vaginal cuff dehiscence and evisceration of abdominal contents after hysterectomy is a rare complication that was first described in the early 1900s.1 The incidence ranges from 0.03% to 0.3% after abdominal or vaginal hysterectomy. This number has recently been reported to be approaching 5% after total laparoscopic or robotic-assisted hysterectomy.2–4 Herein, we report the first known case of prolapsed epiploica of the sigmoid colon after total laparoscopic hysterectomy.
CASE REPORT
A 40-year-old woman, gravida 4, para 3, underwent total laparoscopic hysterectomy for a symptomatic fibroid uterus. The procedure was performed in the usual fashion as described by Sokol et al.5 Colpotomy was performed utilizing the Harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH) and the KOH Colpotimizer (Cooper Surgical, Trumbull, CT). Electrocautory was not used during the colpotomy. The vaginal cuff was closed with interrupted figure-of-eight stitches of delayed absorbable sutures on CT-1 needles. The knots were secured extracorporeally. The procedure was uncomplicated with an uneventful postoperative course. The patient was discharged after a 23-hour observation.
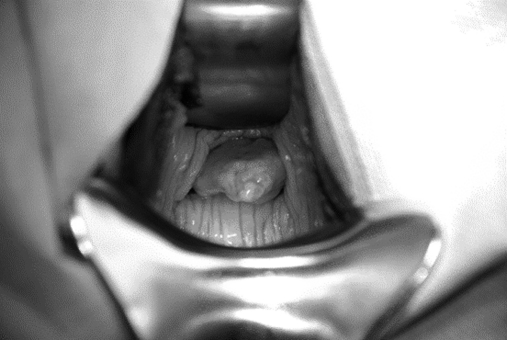
Four months postoperatively, the patient presented as an outpatient complaining of diffuse abdominal discomfort, postcoital bleeding, and vaginal discharge. On physical examination, the abdomen was benign. Speculum examination revealed a 3cm×3cm soft tissue mass, firm and globular, protruding from the vaginal apex consistent with prolapsed viscera. Upon obtaining further history, the patient reported resuming sexual activity 2 weeks postoperatively. She was scheduled to undergo a diagnostic laparoscopy the following day. Intraoperatively, a moderate amount of dense adhesions of the small and large bowel to the vaginal cuff was noted. Sharp enterolysis was carried out laparoscopically to obtain visualization of the vaginal cuff. A soft tissue mass, deemed to be prolapsed epiploica of the sigmoid colon, was subsequently reduced from the vaginal cuff (Figure 1). The cuff appeared completely dehisced. No signs of cuff cellulitis or pelvic infection were noted. Inspection of the bowel revealed no evidence of ischemia or serosal injury. The Harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH) was used to transect the fatty appendage from the sigmoid colon. The vaginal cuff was reapproximated laparoscopically with interrupted figure-of-eight stitches by using 2-0 polydioxanone suture (Ethicon, Somerville, NJ). The patient's recovery was uncomplicated, and she was discharged on postoperative day 2. The final pathology revealed “fat pad” of the large intestine with acute inflammation.
Figure 1.
Epiploica originating from the sigmoid colon prolapsed through vaginal cuff.
DISCUSSION
Nezhat et al6 described the first cases of small bowel evisceration after total laparoscopic hysterectomy in 1996. Small bowel remains the most common organ, with the ileum being the most common segment of the small bowel, to eviscerate through the vaginal cuff.1 Prolapse cases involving the omentum, colon, and fallopian tube have also been described after hysterectomy.1,7 We present the first known case of prolapsed epiploica of the sigmoid colon through the vaginal cuff after total laparoscopic hysterectomy. The only other case of prolapsed epiploica after hysterectomy was described by Lane in 1965,8 which involved appendiceal epiploica in a 73-year-old patient, 6 years after concurrent vaginal hysterectomy and repeat enterocele repair.
Compared with abdominal and vaginal approaches, laparoscopic hysterectomy appears to have an increased incidence of cuff dehiscence. The contributing factors to cuff dehiscence are thought to be thermal tissue damage during colpotomy, suboptimal cuff closure, and early resumption of intercourse.3,4,6,7 Recent reports seem to suggest that robotic-assisted hysterectomy may share a similarly increased risk of cuff dehiscence,2,9 which further underscores the possible role of thermal tissue necrosis and devascularization in this complication, as monopolar electrocautory is the main energy modality used during colpotomy in the robotic approach. In this case, we believe early resumption of intercourse was a significant contributing factor to the cuff dehiscence along with ultrasonic-induced tissue damage of the Harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH).
CONCLUSION
Prolapse of the epiploica of the sigmoid colon is a rare and potential complication of total laparoscopic hysterectomy. A laparoscopic approach may be successfully used in the management of such a complication. As encountered in this case, visceral prolapse through the vaginal cuff does not always present acutely after laparoscopic hysterectomy. Gynecologic surgeons performing laparoscopic hysterectomy should be intimately familiar with different clinical scenarios in which such complications can present. In addition, in-depth knowledge of possible causes of cuff dehiscence in laparoscopic hysterectomy is a prerequisite to prevention and accurate diagnosis of such complications. This is especially important as laparoscopic hysterectomy continues to sideline conventional hysterectomy via the abdominal route.
Contributor Information
Reza Askari, Department of Gynecology-Obstetrics, University at Buffalo, The State University of New York Buffalo, New York, USA..
Samadh F. Ravangard, Department of Gynecology-Obstetrics, University at Buffalo, The State University of New York Buffalo, New York, USA..
Ali Ghomi, Department of Obstetrics and Gynecology, Sisters of Charity Hospital, Buffalo, New York, USA..
References:
- 1. Ramirez PT, Klemer DP. Vaginal evisceration after hysterectomy: a literature review. Obstet Gynecol Survey. 2002;57:462–467 [DOI] [PubMed] [Google Scholar]
- 2. Kho RM, Akl M, Cornella JL, et al. Incidence and characteristics of patients with vaginal cuff dehiscence after robotic procedures. Obstet Gynecol. 2009;114:231–235 [DOI] [PubMed] [Google Scholar]
- 3. Agdi M, Al-Ghafri W, Antolin R, et al. Vaginal vault dehiscence after hysterectomy. J Minim Invasive Gynecol. 2009;16:313–317 [DOI] [PubMed] [Google Scholar]
- 4. Hur HC, Guido RS, Mansuria SM, et al. Incidence and patient characteristics of vaginal cuff dehiscence after different modes of hysterectomies. J Minim Invasive Gynecol. 2007;14:311–317 [DOI] [PubMed] [Google Scholar]
- 5. Sokol AI, Green IC. Laparoscopic hysterectomy. Clin Obstet Gynecol. 2009;52:304–312 [DOI] [PubMed] [Google Scholar]
- 6. Nezhat CH, Nezhat F, Seidman DS, et al. Vaginal vault evisceration after total laparoscopic hysterectomy. Obstet Gynecol. 1996;87:868–870 [PubMed] [Google Scholar]
- 7. Caceres A, McCarus SD. Fallopian tube prolapse after total laparoscopic hysterectomy. Obstet Gynecol. 2008;112(2 Part 2):494–495 [DOI] [PubMed] [Google Scholar]
- 8. Lane D. Strangulated appendix epiploica presenting per vaginam. Med J Aust. 1965;2:712. [DOI] [PubMed] [Google Scholar]
- 9. Robinson BL, Liao JB, Adams SF, et al. Vaginal cuff dehiscence after robotic total laparoscopic hysterectomy. Obstet Gynecol. 2009;114:369–371 [DOI] [PMC free article] [PubMed] [Google Scholar]