Postpartum ovarian vein thrombosis carries a significant risk of morbidity and mortality if not recognized early and managed appropriately.
Keywords: Ovarian vein, Thrombosis, Puerperium
Abstract
Background:
Ovarian vein thrombosis (OVT) is a rare but potentially serious postpartum complication, which occurs in 0.05% to 0.18% of pregnancies and is diagnosed on the right side in 80% to 90% of the cases.
Case Report:
A 32-year-old woman presented at 15 days postpartum to our emergency department with severe abdominal pain, fever, and abdominal distension. Abdominal examination revealed right lower quadrant pain with rebound tenderness. The plain abdominal radiography evidenced a diffuse fecal stasis; abdominal ultrasound showed the presence of free fluid in the Douglas’ pouch and between small bowel loops. Diagnosis of acute appendicitis was made. The patient immediately underwent explorative laparoscopy; at surgery, a woody tumoration consistent with right ovarian vein thrombosis was found. Laparoscopic ultrasound confirmed the diagnosis. Anticoagulation therapy and antibiotics were instituted. CT-scan confirmed the presence of thrombosis up to the vena cava. The patient was discharged on postoperative day 4. At 1-month follow-up, she remained stable and symptom free.
Discussion:
Even though postpartum ovarian vein thrombosis is rare, recognition and treatment is needed to institute adequate therapy and avoid potential serious sequelae. The diagnosis can be established by ultrasound, CT scan, and MRI examinations, although, as in the case described, the limitation of ultrasound includes obscuration of the gonadic vein by overlying bowel gas.
Conclusion:
OVT should be considered in any woman in the postpartum period with lower abdominal pain, fever, and leucocytosis.
INTRODUCTION
Ovarian vein thrombosis is a rare but potentially serious disorder associated with a variety of pelvic conditions, most notably, recent childbirth, but also pelvic inflammatory disease, gynecological surgery, and malignancies.1 Recognition and treatment of this condition is needed to avoid the morbidity and the mortality related both to the thrombosis and to any associated infection or sepsis. Ovarian vein thrombosis occurs in 0.02% to 0.18% of pregnancies. Eighty percent to 90% occur in the right side. This is believed to be due, in part, to the dextrotorsion of the enlarging uterus that commonly occurs during pregnancy, which causes compression of the right ovarian vein and right ureter as they cross the pelvic rim.2 The usual clinical features of postpartum ovarian vein thrombosis (POVT) includes pelvic or flank pain, or both, fever during the 15 days after delivery, and right-sided palpable mass.3 Ultrasound can provide a quick and inexpensive initial examination. Color Doppler evaluation is a helpful tool for the assessment of blood flow in the imaged vessels.4 Hence, correct identification is of crucial importance when we are faced with a postpartum patient with lower quadrant pain and fever.
CASE REPORT
A 32-year-old woman presented at 15 days postpartum to our emergency department with severe, stabbing abdominal pain, fever (up to 39°C) and abdominal distension. There was no associated vaginal bleeding, nausea, or vomiting. She had a spontaneous vaginal delivery of a live full-term male; the immediate postpartum period was unremarkable. Her past clinical history was negative. Abdominal examination revealed right lower quadrant pain associated with rebound tenderness. Plain abdominal X-ray evidenced a diffuse fecal stasis; ultrasonography showed the presence of free fluid into Douglas’ pouch and between small bowel loops. Investigations showed a white blood cell count of 14.4×109/L and hemoglobin of 12g/dL. The rest of the laboratory investigations were within normal values. A diagnosis of acute appendicitis was suspected. The patient underwent exploratory laparoscopy; 3 port sites were used. A pseudotumor aspect of the right ovarian vein was discovered (Figure 1). The appendix and the left ovary and gonadic vein were absolutely normal. Suspecting a POVT, laparoscopic ultrasound was immediately performed. A complete right ovarian vein thrombosis extending up to the vena cava was discovered; Doppler interrogation demonstrated the absence of flow (Figure 2). After that, abdominal CT scan demonstrated an enlarged right ovarian vein with central hypodensity, representing a complete thrombosis, extending up to the vena cava, 3cm below the right renal vein (Figure 3, 4). The patient was treated with intravenous heparin for 5 days, combining oral anticoagulants in the form of warfarin. Antibiotic therapy with ceftriaxone (2g/day) was also administered. She made a good recovery and was discharged from the hospital after 15 days. At 2-month follow-up, the patient remained stable and symptom free.
Figure 1.
Laparoscopic exploration highlights the presence of a woody tumoration at the level of right ovarian vein.
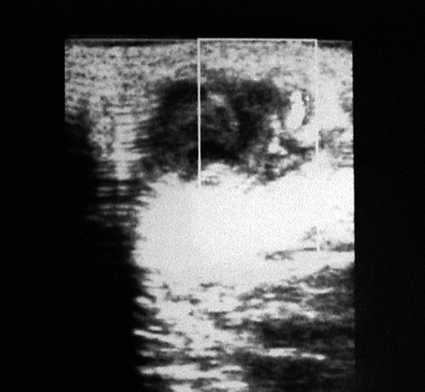
Figure 2.
Laparoscopic cross-section ultrasound image shows the presence of a tubular anechoic-to-hypoechoic structure, with absence of flow on Doppler US interrogation.
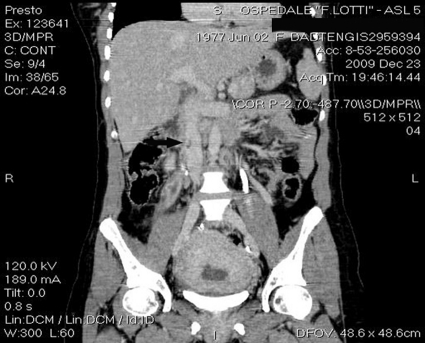
Figure 3.
CT coronal demonstrates an enlarged ovarian vein with central hypodensity, representing thrombosis (arrow).
Figure 4.
CT coronal shows the extension of the thrombus up to the vena cava (arrow).
DISCUSSION
Postpartum ovarian vein thrombosis is an uncommon disease, with a reported incidence from 1:600 to 1:2000 deliveries. POVT is characterized by lower abdominal or flank pain, fever, and leucocytosis. A total of 80% to 90% of cases involve the right ovarian vein. The pathophysiology of ovarian vein thrombosis and septic pelvic thrombophlebitis are ascribed to Virchow's triad of vessel wall injury, venous stasis, and hypercoagulability. An increased risk of thrombosis in pregnancy and puerperium is known. Women are 5 times more likely to suffer from a thromboembolic event when they are pregnant. Compression of the inferior vena cava by the uterus and hormonal changes underlie the thrombus formation in the deep veins of the lower limbs and pelvis.5 However, changes in fibinolysis and coagulation during pregnancy are possibly the most important factors. There is a decrease in blood flow velocity immediately after delivery. Simons et al6 reported an anterograde flow in the right ovarian vein along with a retrograde flow in the left ovarian vein immediately after delivery. In addition, the right ovarian vein is also longer than the left ovarian vein and has many valves within its length, which could increase the risk of thrombosis because these valves might act as a nidus for thrombus formation.7 Other conditions that are associated with hypercoagulability, such as recent surgery, Crohn's disease, or malignancy, could increase the patient's risk for ovarian vein thrombosis.8 Salomon et al9 performed a prospective study on the incidence and risk factors for POVT in 13 women over 4 years. The authors noted that the risk for maternal POVT is increased by cesarean delivery of twins.
POVT typically presents with symptoms suggestive of acute appendicitis, and in most cases, patients undergo exploratory laparoscopy.10 Eighty percent of patients present with pyrexia. Lower quadrant pain and flank pain with associated nausea are common. A mass may be palpable in the right iliac fossa. The differential diagnosis of POVT includes septic pelvic thrombophlebitis, pyelonephritis, urinary tract infection, adnexal torsion, intestinal volvulus, puerperal endometritis, and tubo-ovarian abscess. The diagnosis is made on the clinical features described above. When POVT is suspected, the initial investigation should be an ultrasound examination, which may confirm the diagnosis. However, ultrasound examination is operator-dependent and, as in the case described, is frequently limited by overlying bowel gas. CT scan or MRI can provide better and more reliable visualization of the vascular system. Coronal images are useful in evaluating the extent of a thrombus. Indeed, the severity of POVT is related to the extension of thrombus to the vena cava with an increased risk of pulmonary embolism, which occurs in 13% of cases. A thick-walled, enlarged ovarian vein with rim enhancement and central hypodensity are considered the main CT imaging findings of POVT.11 Hence, in cases of suspected POVT, a spiral CT scan or MRI should be requested even in the presence of a negative ultrasound.12 This careful approach should avoid what happened in the case described, in which a clinical diagnosis of acute appendicitis was suspected, but laparoscopic diagnosis revealed an unexpected ovarian vein thrombosis. Diagnosis and treatment should both be noninvasive. Once the diagnosis is considered, the appropriate investigations can be ordered, and other surgical procedures avoided. Anticoagulants and antibiotics are the mainstay of treatment. Broad-spectrum antibiotic treatment should be initiated immediately, as should intravenous heparin; once thrombolysis has begun, warfarin is introduced and continued for 3 months to 4 months.13 Some authors suggest the use of low molecular weight heparin in uncomplicated cases of POVT; however, there is no uniform agreement regarding the type, dosage, or length of anticoagulation.14
CONCLUSION
Our experience proves that early recognition of this condition is of paramount importance, and even though postpartum ovarian vein thrombosis is infrequently reported, this entity carries a risk of significant morbidity and mortality if inadequately treated. Early recognition is of paramount importance, and any woman who presents in the postpartum period with unexplained lower abdominal pain, fever, and leucocytosis should be evaluated by ultrasound or CT scan to make the right diagnosis and avoid potential serious complications.
Contributor Information
Giancarlo Basili, Health Unit 5 Pisa, Pontedera Hospital, General Surgery Unit, Pontedera, Italy..
Nicola Romano, Health Unit 5 Pisa, Pontedera Hospital, General Surgery Unit, Pontedera, Italy..
Marco Bimbi, Health Unit 5 Pisa, Pontedera Hospital, Department of Emergency Radiology, Pontedera, Italy..
Luca Lorenzetti, Health Unit 5 Pisa, Pontedera Hospital, General Surgery Unit, Pontedera, Italy..
Dario Pietrasanta, Health Unit 5 Pisa, Pontedera Hospital, General Surgery Unit, Pontedera, Italy..
Orlando Goletti, Health Unit 5 Pisa, Pontedera Hospital, General Surgery Unit, Pontedera, Italy..
References:
- 1. Ortin X, Ugarriza A, Espax RM, et al. Postpartum ovarian vein thrombosis. Thromb Haemost. 2005;93:1004–1005 [PubMed] [Google Scholar]
- 2. Dunnihoo DR, Gallaspy JW, Wise RB, Otterson WN. Post-partum ovarian vein thrombophlebitis: a review. Obstet Gynecol Surv. 1991;46:415–427 [DOI] [PubMed] [Google Scholar]
- 3. Sinha D, Yasmin H, Samra JS. Postpartum inferior vena cava and ovarian vein thrombosis – a case report and literature review. J Obstet Gynaecol. 2005;25:312–313 [DOI] [PubMed] [Google Scholar]
- 4. Baran GW, Frisch KM. Duplex Doppler evaluation of puerperal ovarian vein thrombosis. Am J Roentgenol. 1987;149:321–322 [DOI] [PubMed] [Google Scholar]
- 5. Calderwood CJ, Jamienson R, Greer IA. Gestational related changes in the deep venous system of the lower limb on light reflection rheography in pregnancy and the puerperium. Clin Radiol. 2007;62:1174–1179 [DOI] [PubMed] [Google Scholar]
- 6. Simons GR, Piwnica-Worms DR, Goldhaber SZ. Ovarian vein thrombosis. Am Heart J. 1993;126:641–647 [DOI] [PubMed] [Google Scholar]
- 7. Savander SJ, Otero RR, Savander BL. Puerperal ovarian vein thrombosis: evaluation with CT, US, and MR imaging. Radiology. 1988;167:637–639 [DOI] [PubMed] [Google Scholar]
- 8. Salomon O, Apter S, Shaham D, et al. Risk factors associated with postpartum ovarian vein thrombosis. Thromb Haemost. 1999;82:1015–1019 [PubMed] [Google Scholar]
- 9. Salomon O, Dulitzky M, Apter S. New observations in postpartum ovarian vein thrombosis: experience of a single center. Blood Coagul Fibrunolsys. 2010;21:16–19 [DOI] [PubMed] [Google Scholar]
- 10. Johnson A, Wietfeldt ED, Dhevan V, Hassan I. Right lower quadrant pain and postpartum ovarian vein thrombosis. Uncommon but not forgotten. Arch Gynecol Obstet. 2010;281:261–263 [DOI] [PubMed] [Google Scholar]
- 11. Quane LK, Kidney DD, Cohen AJ. Unusual causes of ovarian vein thrombosis as revealed by CT and sonography. AJR Am J Roentgenol. 1998;171:487–490 [DOI] [PubMed] [Google Scholar]
- 12. Twickler DM, Setiawan AT, Evans RS, et al. Imaging of puerperal septic thrombophlebitis: prospective comparison of MR imaging, CT, and sonography. AJR Am J Roentgenol. 1997;169:1039–1043 [DOI] [PubMed] [Google Scholar]
- 13. Själander A, Jansson JH, Bergqvist D, Eriksson H, Carlberg B, Svensson P. Efficacy and safety of anticoagulant prophylaxis to prevent venous thromboembolism in acutely ill medical inpatients: a meta-analysis. J Intern Med. 2008;263:52–60 [DOI] [PubMed] [Google Scholar]
- 14. Al-Toma A, Heggelman BG, Kramer MH. Postpartum ovarian vein thrombosis: report of a case and review of literature. Neth J Med. 2003;61:334–336 [PubMed] [Google Scholar]