A retroperitoneal laparoscopic approach was found to be useful for treating primary retroperitoneal tumors located below the level of the renal vessels.
Keywords: Retroperitoneal inflammatory pseudotumor, Retroperitoneoscopic surgery in supine position
Abstract
Background:
Inflammatory pseudotumors were mostly encountered in the lung. Retroperitoneal inflammatory pseudotumors are relatively rare. Although laparoscopic surgery with a modified flank position is widely performed for retroperitoneal tumors, we placed the patient in the supine position to maintain the normal anatomical view of the retroperitoneal space. We report a case of retroperitoneal inflammatory pseudotumor extracted via retroperitoneoscopic surgery in the supine position.
Methods and Results:
A 53-year-old man presented with back pain and frequent urination. Ultrasonographic examination revealed a solid tumor above the urinary bladder. This tumor was diagnosed as a primary retroperitoneal tumor by computed tomography, magnetic resonance imaging, and angiography. The retroperitoneoscopic procedure was adopted to remove this tumor. Histopathologic examination revealed an inflammatory pseudotumor. There was no evidence of recurrence 5 years after surgery.
Conclusions:
The diagnosis of the inflammatory pseudotumor is rarely made before histologic examination. Only pathologic examination allows the correct diagnosis. Consequently, most patients undergo surgical treatment. A recurrence rate of 25% has been reported for inflammatory pseudotumors. Thus, radical resection is needed. The retroperitoneal laparoscopic approach with the patient in the supine position is useful for surgically treating these primary retroperitoneal tumors located below the level of the renal vessels.
INTRODUCTION
Inflammatory pseudotumors occur in many anatomic sites, especially in the lung. The cause of inflammatory pseudotumors has yet to be determined.1 Because it is difficult to diagnosis using radiographic methods, surgery is the usual strategy for treating these tumors.1 Retroperitoneal inflammatory pseudotumors are relatively rare.1,2 We report a case of retroperitoneal inflammatory pseudotumor extracted via retroperitoneoscopic surgery with the patient in the supine position.
CASE REPORT
A 53-year-old man presented to our institution with back pain and frequent urination. Physical examinations showed neither swollen superficial lymph nodes nor tumors on palpation. However, abdominal ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) revealed a tumor 49mm in diameter above the urinary bladder. Furthermore, an abdominal angiography showed an artery feeding to the tumor from the right common iliac artery (Figure 1). Because peripheral blood tests including tumor markers, hormonal investigation, chest CT, and a digestive examination showed no pathological findings, this tumor was diagnosed as a primary retroperitoneal tumor. The retroperitoneoscopic procedure was adopted to remove this tumor. The patient was placed in a dorsal supine position while under general anesthesia. The common iliac arteries and inferior vena cava were exposed by developing the retroperitoneal space with 3 ports inserted at the right lower abdomen (Figure 2). Slightly adhered to the peritoneum and the right lumbar splanchnic nerves, the tumor was removed without injury to either of them. The operative time was 163 minutes, and the estimated blood loss was minimal. The weight of the tumor was 30g. Macroscopically, the tumor was well encapsulated. The tumor was composed of inflammatory cells consisting of lymphocytes, muscular fibroblastic cells, and fibroblastic cells (Figure 3). Neither nuclear atypia nor dysplasia was found. Consequently, this tumor was diagnosed as an inflammatory pseudotumor. The postoperative course was uneventful. The patient did not experience ejaculatory dysfunction. There was no evidence of recurrence 5 years after surgery.
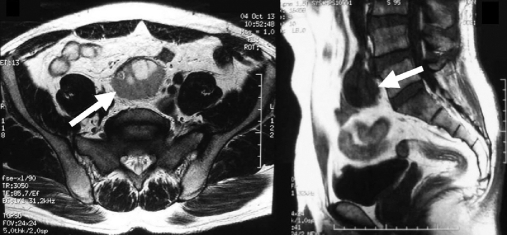
Figure 1.
MRI revealed low signal intensity on unenhanced T1-weighted images (A), while high intensity on unenhanced T2-weighted images showed a well-defined mass (B).
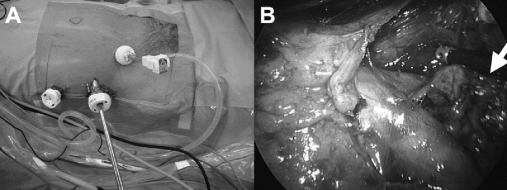
Figure 2.
Three ports were inserted at the right lower abdomen (A). Prior to removal of the tumor, great vessels including the vena cava and bilateral common iliac artery were exposed (B).
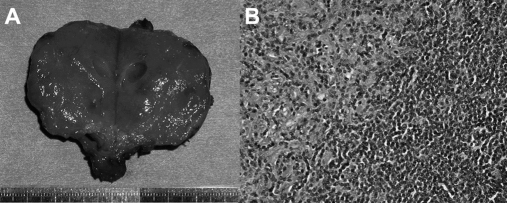
Figure 3.
The tumor was well capsulated macroscopically (A). Microscopically, the tumor was composed of diffuse proliferation lymphocytes without nuclear atypia, as well as myofibroblast cells and fibroblast cells (B).
DISCUSSION
Extrapulmonary inflammatory pseudotumors account for 5% of inflammatory pseudotumors. Coffen et al1 reported a clinicopathologic study of 84 cases of extrapulmonary inflammatory pseudotumors. The initial radiographic examinations suggested the presence of malignant lesions showing the vascular enhancement, the areas of necrosis or hemorrhage, or the involvement of the adjacent structures. The diagnosis was rarely made prior to histologic examination; only pathologic examination allowed the correct diagnosis. Consequently, most patients undergo surgical treatment.2 Although the prognosis for inflammatory pseudotumors was usually excellent, a recurrence rate of 25% has been reported for inflammatory pseudotumors. Furthermore, the transformation of these tumors into undifferentiated sarcomatoid proliferation has also been reported in some cases. The proximity to vital structures is an important factor, because complete resection is a very promising curative procedure for the treatment of these tumors.3–7 In the present case, the retroperitoneal laparoscopic procedure to extract the tumor was performed with the patient in the supine position, because this tumor could be clearly differentiated from adjacent organs by CT and MR imaging. Hara et al8 noted that the retroperitoneal space was easily developed by applying pneumatic pressure during laparoscopic retroperitoneal lymph node dissection with the patient in the supine position, thereby exposing the great vessels including the vena cava, the abdominal aorta, the common iliac veins, and the common iliac arteries.
CONCLUSION
The retroperitoneal laparoscopic approach with the patient in the supine position is useful for surgically treating these primary retroperitoneal tumors located below the level of the renal vessels.
References:
- 1. Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995;19:859–872 [DOI] [PubMed] [Google Scholar]
- 2. Kovach SJ, Fischer AC, Katzman PJ, et al. Inflammatory myofibroblastic tumors. J Surg Oncol. 2006;94:385–391 [DOI] [PubMed] [Google Scholar]
- 3. Johnston SJ, Beaver BL, Sun CC, Luddy RE, Schwartz AD. Inflammatory pseudotumor of the retroperitoneum. Md Med J. 1991;40:787–790 [PubMed] [Google Scholar]
- 4. Gignoux B, Chappuis J, Carlioz P. Inflammatory pseudotumor of the retroperitoneum in a child. Pediatr Surg Int. 1997;12:443–445 [DOI] [PubMed] [Google Scholar]
- 5. Coffin CM, Dehner LP, Meis-Kindblom JM. Inflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and related lesions: an historical review with differential diagnostic considerations. Semin Diagn Pathol. 1998;15:102–110 [PubMed] [Google Scholar]
- 6. Hartyanszky IL, Kadar K, Hubay M. Rapid recurrence of an inflammatory myofibroblastic tumor in the right ventricular outflow tract. Cardiol Young. 2000;10:271–274 [DOI] [PubMed] [Google Scholar]
- 7. Emley TE, Cain MP, Faught PR, Davis MM. Ureteropelvic junction obstruction due to inflammatory pseudotumor masquerading as hydronephrosis because of a neuropathic bladder in a child with myelomeningocele. Urology. 2001;58:105. [DOI] [PubMed] [Google Scholar]
- 8. Hara I, Kawabata G, Yamada Y, Tanaka K, Kamidono S. Extraperitoneal laparoscopic retroperitoneal lymph node dissection in supine position after chemotherapy for advanced testicular carcinoma. Int J Urol. 2004;11:934–939 [DOI] [PubMed] [Google Scholar]