Abstract
Purpose
To describe the clinical characteristics of idiopathic juxtafoveal telangiectasis (IJT) in Koreans.
Methods
Medical records of 16 patients with IJT were analyzed during the period from 1997 to 2009. Diagnosis was based on biomicrosopic and fluorescein angiographic findings and the group was determined according to the Gass and Blodi classification.
Results
We analyzed eight patients in group 1A (50%), two in group 1B (12.5%), and six in group 2A (37.5%). Diverse treatment modalities, such as macular laser photocoagulation, photodynamic therapy, intravitreal antiangiogenic agent, and steroid injection, were applied for macular edema in nine eyes; however, only two eyes showed visual improvement.
Conclusions
In this case series, group 1A was the most common. For macular edema related to IJT, current treatment strategies had no consistent effect.
Keywords: Idiopathic Juxtafoveal Retinal Telangiectasia, Intravitreal Injection, Macular edema, Photochemotherapy
In 1982, Gass and Oyakawa [1] defined idiopathic juxtafoveal telangiectasis (IJT) as a unilateral or bilateral developmental retinal vascular abnormality associated with incompetence and ectasia of foveal and parafoveal capillaries. Classification and staging of IJT was based on clinical and fluorescein angiographic findings. This classification was later updated by Gass and Blodi [2]. The pathophysiology of IJT is still unknown, although the cause of visual loss in IJT is associated with macular edema [1,2]. Several treatment modalities such as laser photocoagulation [3,4], photodynamic therapy (PDT) [5,6], and intravitreal injection of triamcinolone acetonide [7,8] or bevacizumab [9-12] have been tested for the treatment of macular edema in IJT. To date, only one study has investigated IJT in Korean patients: Chang et al. [3] reported that the group 1B subtype was the most common and that argon laser photocoagulation was an effective treatment for macular edema in IJT. In this study, we identified the clinical characteristics of IJT in Koreans.
Materials and Methods
We reviewed the medical records of 16 IJT patients (22 affected eyes) presenting to the Samsung Medical Center between 1997 and 2009. Patients with secondary juxtafoveal telangiectasis caused by retinal venous obstruction, irradiation, and intraocular inflammation were excluded from this study. All patients provided a detailed medical and ocular history and underwent a complete eye examination including slit-lamp biomicroscopy, fundus photography, and fluorescein angiography. Clinical features analyzed included age at diagnosis, gender, laterality, best corrected visual acuity (BCVA), systemic disease, type of treatment, and classification of the disease according to Gass and Blodi [2] (Table 1).
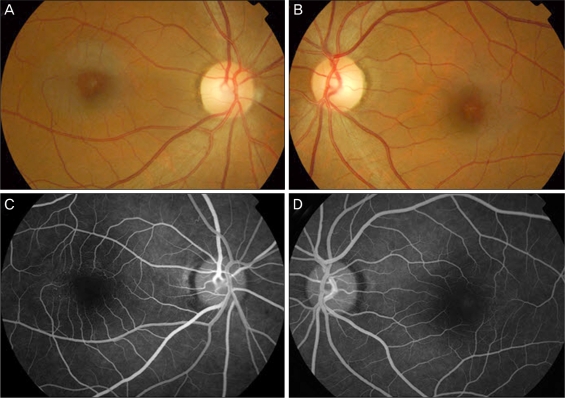
Table 1.
Demographic and clinical information for 16 patients with idiopathic juxtafoveal retinal telangiectasis
VApre = visual acuity before treatment; VApost = visual acuity after treatment; LP = laser photocoagulation; DM = diabetes mellitus; HTN = hypertension; IVB = intravitreal bevacizumab injection; IVTA = intravitreal triamcinolone acetonide; PDT = photodynamic therapy.
Results
Of the 16 study patients, eight had group 1A disease, two had group 1B, and six had group 2A.
Group 1A
Eight patients (six males and two females) were classified as group 1A. Patients ranged in age from 11 to 66 years (mean, 48.6 years) at presentation. Disease was unilateral in all cases, involving three right eyes and five left eyes. Two patients had diabetes mellitus. One had diabetes mellitus and hypertension. Six of the eight patients (75%) were treated for macular edema and were followed for 3 to 62 months (mean, 16.6 months). Two patients were treated by laser photocoagulation to the area of capillary leakage and the rest were treated by intravitreal bevacizumab and laser photocoagulation. However, at the last examination, visual acuity had improved in only one patient (case 9), visual acuity remained unchanged in three, and had worsened in two (Table 1).
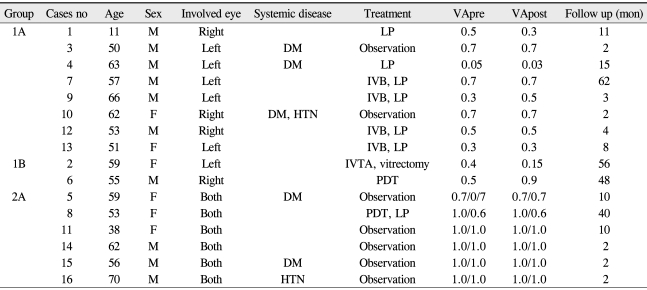
The patient corresponding to case 12 was a 53-year-old man who presented with a complaint of decreased vision in his right eye 1 year previously. The BCVA in the right eye was 20 / 40. Fundus examination of the right eye showed significant macular edema and circinate exudates. Fundus fluorescein angiography revealed parafoveal telangiectasis. Optical coherence tomography (OCT) demonstrated cystoid macular edema. He received two intravitreal bevacizumab injections (1.25 mg in 0.05 mL) and one laser photocoagulation treatment. Three months later, visual acuity of his left eye remained unchanged and the macular edema in the right eye was not improved, as confirmed by OCT (Fig. 1).
Fig. 1.
Group 1A idiopathic juxtafoveal retinal telangiectasis (case 12). (A) Color fundus photography of the left eye on presentation showed a lipid exudate with aneurysm-like capillaries in its center. (B) Fluorescein angiography of the left eye on presentation showed telangiectasis and microaneurysm. (C) Optical coherence tomography of the left eye on presentation indicates macular edema with foveolar detachment. (D) Macular edema showed no improvement 3 months after a repeat intravitreal bevacizumab treatment and focal laser photocoagulation.
Group 1B
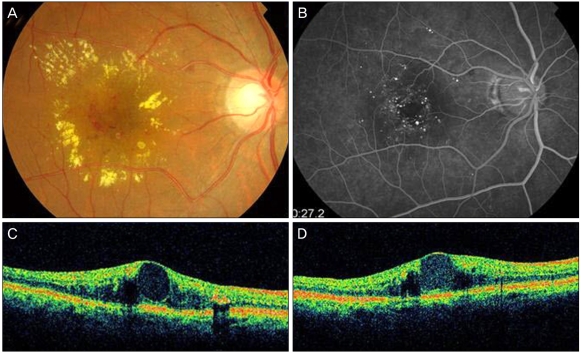
Two patients (one male and one female) were classified as group 1B. The patients were 55 and 59 years old at presentation and both had undergone treatment for macular edema (Table 1). In one patient (case 2), macular edema resolved after additional intravitreal trimacinolone acetonide (IVTA) injection; however, there was subsequent recurrence and the patient underwent vitrectomy. The other patient (case 6) was treated with PDT, and visual improvement and resolution of macular edema was achieved (Fig. 2).
Fig. 2.
Group 1B idiopathic juxtafoveal retinal telangiectasis (case 6). (A) Color fundus photography of the right eye on presentation. (B) Fluorescein angiography of the right eye on presentation showed focal juxtafoveal telangiectasis. (C) Optical coherence tomography of the right eye on presentation. Images demonstrated a foveal cystoid and intraretinal edema. (D) The macular edema resolved after photodynamic treatment.
Group 2A
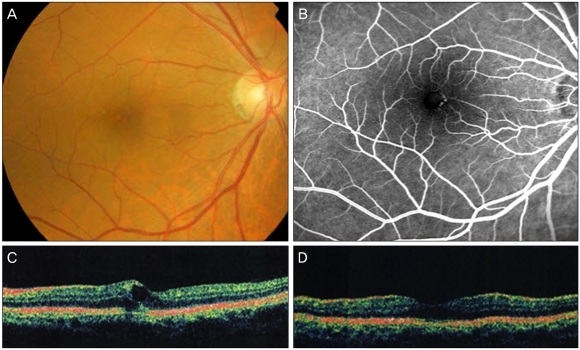
Six patients (four males and two females) were classified as group 2A. Patients ranged in age from 38 to 70 years (mean, 55.1 years) at presentation. Two patients had diabetes mellitus and one had systemic hypertension. Among them, one eye (case 8) was treated for macular edema with laser photocoagulation and PDT (Table 1). The visual acuity remained unchanged. The remaining five patients did not receive treatment (Fig. 3).
Fig. 3.
Group 2A idiopathic juxtafoveal retinal telangiectasis (case 10) (A,B) Color fundus photography of both eyes on presentation showed slight graying of the perifoveal retina and lipid exudates in the right eye. (C,D) Fluorescein angiography of both eyes on presentation showed telangiectatic change in the temporal macular lesion.
Discussion
IJT is an uncommon retinal disorder characterized by incompetent and dilated retinal capillaries in the foveal and parafoveal region. IJT was first described by Gass in 1968 [13]. According to a revised classification [2], group 1A is unilateral congenital parafoveolar telangiectasis. This class is characterized by prominent telangiectatic retinal capillaries that typically involve the temporal half of the macula for 2 disc diameters (DD) or greater and are usually associated with varying amounts of yellowish exudate. More than 90% of patients with group 1A disease are males, with an average age of 39 years, and more than 90% are unilateral cases. In our study, 75% of the patients were male with a mean age of 48.6 years and all were unilateral. Decreased visual acuity was most commonly caused by macular edema, which was present in 6 of 8 patients. Tripathi and Ashton [14] suggested that the cause of telangiectasis in group 1A is a functional or structural breakdown of the blood-retinal barrier (vascular endothelial) with consequent mural disorganization and formation of aneurysms or telangiectasis. Group 1B patients also show male predilection and unilaterality. Lesions are visible, exudative, and focal juxtafoveolar telangiectasis with a small focal area of incompetent capillaries next to the foveal avascular zone. We observed these lesions in only two of our study patients.
Group 2A is characterized by bilaterality, and occult and nonexudative acquired parafoveolar telangiectasis that is often located temporal to the fovea, with a more or less symmetric appearance in both eyes. There is no gender predilection and 95% of patients have bilateral involvement at initial presentation. In our series, the median age was 55.1 years, which was similar to the mean age of 55 years in the Gass-Blodi series, and men were more frequently affected than woman (66.7%).
Group 2B is juvenile occult familial IJT. Group 3A represents occlusive IJT with visual loss, minimal exudation, and extensive occlusion of the juxtafoveal capillary network in both eyes. Group 3B is occlusive IJT associated with central nervous system vasculopathy.
In prior studies, the most common subtype was group 2A, followed by group 1A [2,15-17]. In a previous report on Korean patients, Chang et al. [3] reported that group 1B was the most common, whereas group 1A was most the common subtype in our study. These differences can be attributed to different classifications. Chang et al. [3] added the classification that there is no lipid exudation in group 1B even if telangiectatic retinal capillaries involved the macula for 2DD or greater. However, Gass and Blodi [2] proposed that group 1B is a mild form of the disease seen in group 1A patients, and Yannuzzi et al. [17] considered that group 1B progresses to a more extensive disease with time and therefore group 1A and 1B should be merged by omitting the distinctions based on two clock hours of involvement in the juxtafoveal area. In the results of Chang et al. [3] and our study, group 1 disease was more common than group 2 among Korean IJT patients, in contrast to findings of the largest two previous series [2,17]. This difference may be partly due to limitations of our study. The significance of our study was limited by the small number of cases and the possibility that there were many asymptomatic patients who did not visit hospital. In recent large-scaled epidemiological studies [18,19], the prevalence of macular telangiectasis type 2 was higher than previously believed because early cases, which are usually asymptomatic, go undetected.
Diabetes mellitus has been reported as a risk factor for IJT [20]. One report also described a high incidence of impaired glucose tolerance in these patients [21]. Although we had five patients with diabetes mellitus at the time of presentation, it was difficult to prove or disprove a correlation between diabetes and IJT.
The cause of vision loss in patients with IJT is macular edema and hard exudates in group 1, and foveal atrophy or choroidal neovascularization in group 2 [2,16,17]. Therapeutic options for IJT are limited. Macular laser photocoagulation has been proposed for all forms of IJT by several authors; however, it was reported that treatment was helpful only for group 1 but not for group 2, and success was confined to cases in which the ectatic vessels were not close to the foveal center [2,4]. A few case reports support the use of PDT for IJT with macular edema or choroidal neovascularization [5,6]. Two cases in our study were treated by PDT: one was group 1B IJT with macular edema and the other was group 2A IJT with subretinal neovascularization. At the last follow up, macular edema was improved in the former and subretinal neovascularization remained quiescent in the latter. Several recent case studies have demonstrated the safety and potential benefits of intravitreal anti-angiogenic [10,11,22,23] and steroid drugs [7,8], providing new possibilities for the stabilization of vessel walls and reduction of fluid leakage and edema.
In this study, nine eyes with macular edema underwent treatment; six eyes in group 1A, two in group 1B, and one in group 2A. Macular edema showed improvement in eight of the nine eyes, whereas visual acuity increased in only two eyes; one in group 1B that underwent PDT (case 6) and one in group 1A that was refractory to laser photocoagulation and underwent additional intravitreal bevacizumab injection therapy (case 9). Five eyes did not show visual improvement and two eyes presented with aggravated vision. Four cases of macular edema in group 1A IJT were refractory to laser photocoagulation and were treated with intravitreal injection of bevacizumab. None of them showed improvement of visual acuity (Table 1). In the study of Gass and Blodi [2], there were only five patients in group 1B and the prognosis for these patients was favorable. Only one of them was treated by laser photocoagulation because of a decline in visual acuity, which returned to 20 / 20 after treatment. In contrast, both group 1B patients in our study were treated because visual acuities decreased below 20 / 40. The patient who was treated with IVTA developed cataract after treatment. Although the patient had cataract surgery, there was recurrence of macular edema. The patient underwent vitrectomy and laser photocoagulation; however, the visual acuity worsened because of vascularized retinal scars.
In summary, in our study, group 1A IJT was the most common, followed by group 2A. Macular edema was the most common cause of decreased vision in IJT; however, no treatment modality showed consistent efficacy. Further investigation is obviously required to improve the treatment of macular edema in IJT patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gass JD, Oyakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Arch Ophthalmol. 1982;100:769–780. doi: 10.1001/archopht.1982.01030030773010. [DOI] [PubMed] [Google Scholar]
- 2.Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and follow-up study. Ophthalmology. 1993;100:1536–1546. [PubMed] [Google Scholar]
- 3.Chang YI, Lee JG, Kim TW, Lee EK. The Clinical manifestations and treatments of parafoveal telangiectasis. J Korean Ophthalmol Soc. 2004;45:576–584. [Google Scholar]
- 4.Park DW, Schatz H, McDonald HR, Johnson RN. Grid laser photocoagulation for macular edema in bilateral juxtafoveal telangiectasis. Ophthalmology. 1997;104:1838–1846. doi: 10.1016/s0161-6420(97)30019-0. [DOI] [PubMed] [Google Scholar]
- 5.Kotoula MG, Chatzoulis DZ, Karabatsas CH, et al. Resolution of macular edema in idiopathic juxtafoveal telangiectasis using PDT. Ophthalmic Surg Lasers Imaging. 2009;40:65–67. doi: 10.3928/15428877-20090101-10. [DOI] [PubMed] [Google Scholar]
- 6.Smithen LM, Spaide RF. Photodynamic therapy and intravitreal triamcinolone for a subretinal neovascularization in bilateral idiopathic juxtafoveal telangiectasis. Am J Ophthalmol. 2004;138:884–885. doi: 10.1016/j.ajo.2004.05.073. [DOI] [PubMed] [Google Scholar]
- 7.Alldredge CD, Garretson BR. Intravitreal triamcinolone for the treatment of idiopathic juxtafoveal telangiectasis. Retina. 2003;23:113–116. doi: 10.1097/00006982-200302000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Wu L, Evans T, Arevalo JF, et al. Long-term effect of intravitreal triamcinolone in the nonproliferative stage of type II idiopathic parafoveal telangiectasia. Retina. 2008;28:314–319. doi: 10.1097/IAE.0b013e31814cf03e. [DOI] [PubMed] [Google Scholar]
- 9.Charbel Issa P, Holz FG, Scholl HP. Findings in fluorescein angiography and optical coherence tomography after intravitreal bevacizumab in type 2 idiopathic macular telangiectasia. Ophthalmology. 2007;114:1736–1742. doi: 10.1016/j.ophtha.2007.03.079. [DOI] [PubMed] [Google Scholar]
- 10.Kovach JL, Rosenfeld PJ. Bevacizumab (avastin) therapy for idiopathic macular telangiectasia type II. Retina. 2009;29:27–32. doi: 10.1097/IAE.0b013e31818ba9de. [DOI] [PubMed] [Google Scholar]
- 11.Maia OO, Jr, Bonanomi MT, Takahashi WY, et al. Intravitreal bevacizumab for foveal detachment in idiopathic perifoveal telangiectasia. Am J Ophthalmol. 2007;144:296–299. doi: 10.1016/j.ajo.2007.03.059. [DOI] [PubMed] [Google Scholar]
- 12.Moon SJ, Berger AS, Tolentino MJ, Misch DM. Intravitreal bevacizumab for macular edema from idiopathic juxtafoveal retinal telangiectasis. Ophthalmic Surg Lasers Imaging. 2007;38:164–166. doi: 10.3928/15428877-20070301-15. [DOI] [PubMed] [Google Scholar]
- 13.Gass JD. A fluorescein angiographic study of macular dysfunction secondary to retinal vascular disease. V. Retinal telangiectasis. Arch Ophthalmol. 1968;80:592–605. doi: 10.1001/archopht.1968.00980050594005. [DOI] [PubMed] [Google Scholar]
- 14.Tripathi R, Ashton N. Electron microscopical study of Coat's disease. Br J Ophthalmol. 1971;55:289–301. doi: 10.1136/bjo.55.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abujamra S, Bonanomi MT, Cresta FB, et al. Idiopathic juxtafoveolar retinal telangiectasis: clinical pattern in 19 cases. Ophthalmologica. 2000;214:406–411. doi: 10.1159/000027534. [DOI] [PubMed] [Google Scholar]
- 16.Watzke RC, Klein ML, Folk JC, et al. Long-term juxtafoveal retinal telangiectasia. Retina. 2005;25:727–735. doi: 10.1097/00006982-200509000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Yannuzzi LA, Bardal AM, Freund KB, et al. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124:450–460. doi: 10.1001/archopht.124.4.450. [DOI] [PubMed] [Google Scholar]
- 18.Aung KZ, Wickremasinghe SS, Makeyeva G, et al. The prevalence estimates of macular telangiectasia type 2: the Melbourne Collaborative Cohort Study. Retina. 2010;30:473–478. doi: 10.1097/IAE.0b013e3181bd2c71. [DOI] [PubMed] [Google Scholar]
- 19.Klein R, Blodi BA, Meuer SM, et al. The prevalence of macular telangiectasia type 2 in the Beaver Dam eye study. Am J Ophthalmol. 2010;150:55–62.e2. doi: 10.1016/j.ajo.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chew EY, Murphy RP, Newsome DA, Fine SL. Parafoveal telangiectasis and diabetic retinopathy. Arch Ophthalmol. 1986;104:71–75. doi: 10.1001/archopht.1986.01050130081025. [DOI] [PubMed] [Google Scholar]
- 21.Millay RH, Klein ML, Handelman IL, Watzke RC. Abnormal glucose metabolism and parafoveal telangiectasia. Am J Ophthalmol. 1986;102:363–370. doi: 10.1016/0002-9394(86)90012-7. [DOI] [PubMed] [Google Scholar]
- 22.Charbel Issa P, Finger RP, Holz FG, Scholl HP. Eighteen-month follow-up of intravitreal bevacizumab in type 2 idiopathic macular telangiectasia. Br J Ophthalmol. 2008;92:941–945. doi: 10.1136/bjo.2007.129627. [DOI] [PubMed] [Google Scholar]
- 23.Gamulescu MA, Walter A, Sachs H, Helbig H. Bevacizumab in the treatment of idiopathic macular telangiectasia. Graefes Arch Clin Exp Ophthalmol. 2008;246:1189–1193. doi: 10.1007/s00417-008-0795-6. [DOI] [PubMed] [Google Scholar]